Abstract
Background
Racial disparities in guideline-directed medical therapy (GDMT) for heart failure with reduced ejection fraction (HFrEF) have not been fully documented in a community setting.
Methods
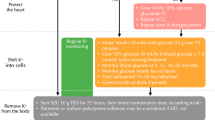
In the ARIC Surveillance Study (2005–2014), we examined racial differences in GDMT at discharge, its temporal trends, and the prognostic impact among individuals with hospitalized HFrEF, using weighted regression models to account for sampling design. Optimal GDMT was defined as beta blockers (BB), mineralocorticoid receptor antagonist (MRA) and ACE inhibitors (ACEI) or angiotensin II receptor blockers (ARB). Acceptable GDMT included either one of BB, MRA, ACEI/ARB or hydralazine plus nitrates (H-N).
Results
Of 16,455 (unweighted n = 3,669) HFrEF cases, 47% were Black. Only ~ 10% were discharged with optimal GDMT with higher proportion in Black than White individuals (11.1% vs. 8.6%, p < 0.001). BB use was > 80% in both racial groups while Black individuals were more likely to receive ACEI/ARB (62.0% vs. 54.6%) and MRA (18.0% vs. 13.8%) than Whites, with a similar pattern for H-N (21.8% vs. 10.1%). There was a trend of decreasing use of optimal GDMT in both groups, with significant decline of ACEI/ARB use in Whites (− 2.8% p < 0.01) but increasing H-N use in both groups (+ 6.5% and + 9.2%, p < 0.01). Only ACEI/ARB and BB were associated with lower 1-year mortality.
Conclusions
Optimal GDMT was prescribed in only ~ 10% of HFrEF patients at discharge but was more so in Black than White individuals. ACEI/ARB use declined in Whites while H-N use increased in both races. GDMT utilization, particularly ACEI/ARB, should be improved in Black and Whites individuals with HFrEF.




Similar content being viewed by others
Data availability
ARIC data is available through the NHLBI BioLINCC (https://biolincc.nhlbi.nih.gov/home/) or the ARIC Data Coordinating Center at the University of North Carolina (details can be found at https://sites.cscc.unc.edu/aric/distribution-agreements).
Code Availability
Custom code is available upon request.
Abbreviations
- ACEI:
-
Angiotensin-converting-enzyme inhibitor
- AF:
-
Atrial fibrillation or flutter
- ARB:
-
Angiotensin-receptor blocker
- ARIC:
-
Atherosclerosis Risk in Communities Study
- BB:
-
Beta blocker
- BMI:
-
Body mass index
- CHD:
-
Coronary heart disease
- CKD:
-
Chronic kidney disease
- HF:
-
Heart failure
- HFrEF:
-
Heart failure with reduced ejection fraction
- H-N:
-
Hydralazine nitrate
- HR:
-
Heart rate
- GDMT:
-
Guideline-directed medical therapy
- MMCC:
-
Morbidity and mortality
- MRA:
-
Mineralocorticoid receptor antagonist
- LVEF:
-
Left ventricular ejection fraction
- SBP:
-
Systolic blood pressure
- IABP:
-
Intra-aortic balloon pump
- LVAD:
-
Left ventricular assist device
- eGFR:
-
Estimated glomerular filtration rate
References
Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev. 2017;3(1):7–11.
Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67–492.
Chang PP, Wruck LM, Shahar E, et al. Trends in hospitalizations and survival of acute decompensated heart failure in four US communities (2005–2014): the Atherosclerosis Risk in Communities (ARIC) Study Community Surveillance. Circulation 2018.
Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136(6):e137–61.
Barker WH, Mullooly JP, Getchell W. Changing incidence and survival for heart failure in a well-defined older population, 1970–1974 and 1990–1994. Circulation. 2006;113(6):799–805.
Glynn P, Lloyd-Jones DM, Feinstein MJ, Carnethon M, Khan SS. Disparities in cardiovascular mortality related to heart failure in the United States. J Am Coll Cardiol. 2019;73(18):2354–5.
Bibbins-Domingo K, Pletcher MJ, Lin F, et al. Racial differences in incident heart failure among young adults. N Engl J Med. 2009;360(12):1179–90.
Bahrami H, Kronmal R, Bluemke DA, et al. Differences in the incidence of congestive heart failure by ethnicity: the multi-ethnic study of atherosclerosis. Arch Intern Med. 2008;168(19):2138–45.
Kalogeropoulos A, Georgiopoulou V, Kritchevsky SB, et al. Epidemiology of incident heart failure in a contemporary elderly cohort: the health, aging, and body composition study. Arch Intern Med. 2009;169(7):708–15.
Huffman MD, Berry JD, Ning H, et al. Lifetime risk for heart failure among white and black Americans: cardiovascular lifetime risk pooling project. J Am Coll Cardiol. 2013;61(14):1510–7.
Mathews L, Han D, Evans MK, Zonderman AB, Ndumele CE, Crews DC. Prevalence of guideline-directed medical therapy for cardiovascular disease among Baltimore City adults in the Healthy Aging in Neighborhoods of Diversity Across the Life Span (HANDLS) Study. J Racial Ethn Health Disparities 2021.
Angraal S, Khera R, Wang Y, et al. Sex and race differences in the utilization and outcomes of coronary artery bypass grafting among medicare beneficiaries, 1999–2014. J Am Heart Assoc. 2018 7(14).
Ayanian JZ, Udvarhelyi IS, Gatsonis CA, Pashos CL, Epstein AM. Racial differences in the use of revascularization procedures after coronary angiography. JAMA. 1993;269(20):2642–6.
Bertoni AG, Goonan KL, Bonds DE, Whitt MC, Goff DC Jr, Brancati FL. Racial and ethnic disparities in cardiac catheterization for acute myocardial infarction in the United States, 1995–2001. J Natl Med Assoc. 2005;97(3):317–23.
Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116(15):1653–62.
Aragam KG, Dai D, Neely ML, et al. Gaps in referral to cardiac rehabilitation of patients undergoing percutaneous coronary intervention in the United States. J Am Coll Cardiol. 2015;65(19):2079–88.
Ritchey MD, Maresh S, McNeely J, et al. Tracking cardiac rehabilitation participation and completion among Medicare beneficiaries to inform the efforts of a national initiative. Circ Cardiovasc Qual Outcomes. 2020;13(1):e005902.
Eberly LA, Richterman A, Beckett AG, et al. Identification of racial inequities in access to specialized inpatient heart failure care at an academic medical center. Circ Heart Fail. 2019;12(11):e006214.
Hunt SA, Abraham WT, Chin MH, et al. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005;112(12):e154-235.
Rassi AN, Cavender MA, Fonarow GC, et al. Temporal trends and predictors in the use of aldosterone antagonists post-acute myocardial infarction. J Am Coll Cardiol. 2013;61(1):35–40.
Parameswaran AC, Tang WH, Francis GS, Gupta R, Young JB. Why do patients fail to receive beta-blockers for chronic heart failure over time? A “real-world” single-center, 2-year follow-up experience of beta-blocker therapy in patients with chronic heart failure. Am Heart J. 2005;149(5):921–6.
Patel P, White DL, Deswal A. Translation of clinical trial results into practice: temporal patterns of beta-blocker utilization for heart failure at hospital discharge and during ambulatory follow-up. Am Heart J. 2007;153(4):515–22.
Curtis LH, Mi X, Qualls LG, et al. Transitional adherence and persistence in the use of aldosterone antagonist therapy in patients with heart failure. Am Heart J. 2013;165(6):979-986 e971.
Fonarow GC, Albert NM, Curtis AB, et al. Improving evidence-based care for heart failure in outpatient cardiology practices: primary results of the Registry to Improve the Use of Evidence-Based Heart Failure Therapies in the Outpatient Setting (IMPROVE HF). Circulation. 2010;122(6):585–96.
Khazanie P, Liang L, Curtis LH, et al. Clinical effectiveness of hydralazine-isosorbide dinitrate therapy in patients with heart failure and reduced ejection fraction: findings from the Get With The Guidelines-Heart Failure Registry. Circ Heart Fail. 2016;9(2):e002444.
Greene SJ, Fonarow GC, DeVore AD, et al. Titration of medical therapy for heart failure with reduced ejection fraction. J Am Coll Cardiol. 2019;73(19):2365–83.
Greene SJ, Butler J, Albert NM, et al. Medical therapy for heart failure with reduced ejection fraction: the CHAMP-HF Registry. J Am Coll Cardiol. 2018;72(4):351–66.
Allen LA, Fonarow GC, Liang L, et al. Medication initiation burden required to comply with heart failure guideline recommendations and hospital quality measures. Circulation. 2015;132(14):1347–53.
Dickson VV, Knafl GJ, Wald J, Riegel B. Racial differences in clinical treatment and self-care behaviors of adults with chronic heart failure. J Am Heart Assoc. 2015 4(4).
Yancy CW, Abraham WT, Albert NM, et al. Quality of care of and outcomes for African Americans hospitalized with heart failure: findings from the OPTIMIZE-HF (Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure) registry. J Am Coll Cardiol. 2008;51(17):1675–84.
Hernandez AF, Fonarow GC, Liang L, et al. Sex and racial differences in the use of implantable cardioverter-defibrillators among patients hospitalized with heart failure. JAMA. 2007;298(13):1525–32.
Steinberg BA, Zhao X, Heidenreich PA, et al. Trends in patients hospitalized with heart failure and preserved left ventricular ejection fraction: prevalence, therapies, and outcomes. Circulation. 2012;126(1):65–75.
Komajda M, Anker SD, Cowie MR, et al. Physicians’ adherence to guideline-recommended medications in heart failure with reduced ejection fraction: data from the QUALIFY global survey. Eur J Heart Fail. 2016;18(5):514–22.
Surveillance of Heart Failure Manual of Operations Manual 3A [Manual]. 2009;Version 2.0. http://www.cscc.unc.edu/aric/visit/Surveillance_Procedures_-_Heart_Failure.6_3a.pdf. Accessed 06/26/19. Accessed Apr 14, 2020.
White AD, Folsom AR, Chambless LE, et al. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) Study: methods and initial two years’ experience. J Clin Epidemiol. 1996;49(2):223–33.
Wojcik NC, Huebner WW, Jorgensen G. Strategies for using the National Death Index and the Social Security Administration for death ascertainment in large occupational cohort mortality studies. Am J Epidemiol. 2010;172(4):469–77.
Cowper DC, Kubal JD, Maynard C, Hynes DM. A primer and comparative review of major US mortality databases. Ann Epidemiol. 2002;12(7):462–8.
Cochran WG. Sampling Techniques, vol. 3rd. John Wiley and Sonds: Edition. Harvard University; 1977.
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55.
Lunceford JK, Davidian M. Stratification and weighting via the propensity score in estimation of causal treatment effects: a comparative study. Stat Med. 2004;23(19):2937–60.
Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661–79.
Austin PC, Stuart EA. The performance of inverse probability of treatment weighting and full matching on the propensity score in the presence of model misspecification when estimating the effect of treatment on survival outcomes. Stat Methods Med Res. 2017;26(4):1654–70.
Cummings P. Estimating adjusted risk ratios for matched and unmatched data: an update. Stand Genomic Sci. 2011;11(2):290–8.
O’Brien EC, Rose KM, Suchindran CM, et al. Medication, reperfusion therapy and survival in a community-based setting of hospitalised myocardial infarction. Heart. 2013;99(11):767–73.
Dugoff EH, Schuler M, Stuart EA. Generalizing observational study results: applying propensity score methods to complex surveys. Health Serv Res. 2014;49(1):284–303.
Skinner J, Chandra A, Staiger D, Lee J, McClellan M. Mortality after acute myocardial infarction in hospitals that disproportionately treat black patients. Circulation. 2005;112(17):2634–41.
Gilstrap LG, Fonarow GC, Desai AS, et al. Initiation, continuation, or withdrawal of angiotensin-converting enzyme inhibitors/angiotensin receptor blockers and outcomes in patients hospitalized with heart failure with reduced ejection fraction. J Am Heart Assoc. 2017 6(2).
Margolis J, Gerber RA, Roberts C, Gheorghiade M. Adherence to aldosterone-blocking agents in patients with heart failure. Am J Ther. 2010;17(5):446–54.
Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. The New England Journal of Medicine. 1999;341(10):709–17.
Cohn JN, Tognoni G, Valsartan Heart Failure Trial I. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345(23):1667–75.
Packer M, Fowler MB, Roecker EB, et al. Effect of carvedilol on the morbidity of patients with severe chronic heart failure: results of the carvedilol prospective randomized cumulative survival (COPERNICUS) study. Circulation. 2002;106(17):2194–9.
Taylor AL, Ziesche S, Yancy C, et al. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med. 2004;351(20):2049–57.
McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371(11):993–1004.
Yusuf S, Pitt B, Davis CE, Hood WB, Cohn JN. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991;325(5):293–302.
Juurlink DN, Mamdani MM, Lee DS, et al. Rates of hyperkalemia after publication of the Randomized Aldactone Evaluation Study. N Engl J Med. 2004;351(6):543–51.
Zannad F, McMurray JJ, Krum H, et al. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. 2011;364(1):11–21.
Cohn JN, Johnson G, Ziesche S, et al. A comparison of enalapril with hydralazine-isosorbide dinitrate in the treatment of chronic congestive heart failure. N Engl J Med. 1991;325(5):303–10.
Cohn JN, Archibald DG, Ziesche S, et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure. Results of a Veterans Administration Cooperative Study. N Engl J Med. 1986;314(24):1547–52.
American Academy of Family P, American Academy of H, Palliative M, et al. ACCF/AHA/AMA-PCPI 2011 performance measures for adults with heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures and the American Medical Association-Physician Consortium for Performance Improvement. J Am Coll Cardiol 2012;59(20):1812–1832.
Kao DP, Trinkley KE, Lin CT. Heart failure management innovation enabled by electronic health records. JACC Heart failure. 2020;8(3):223–33.
Acknowledgements
The Atherosclerosis Risk in Communities study has been funded in whole or in part with Federal funds from the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services, under Contract nos. (HHSN268201700001I, HHSN268201700002I, HHSN268201700003I, HHSN268201700005I, HHSN268201700004I). The authors thank the staff and participants of the ARIC study for their important contributions.
Funding
Dr. Mathews was supported by Diversity Supplement under ARIC Contract Grant Number Contract HHSN268201700002I/ 75N92019F00074- from the National Heart, Lung, and Blood Institute, National Institutes of Health. Dr. Punjabi was supported by National Institute of Health Grant no. HL146709.
Author information
Authors and Affiliations
Contributions
Lena Mathews: conceptualization, methodology, formal analysis, writing—original draft; Ning Ding: formal analysis; Yingying Sang: formal analysis; Laura R. Loehr: conceptualization, methodology; Jung-Im Shin: conceptualization, methodology; Naresh M. Punjabi: conceptualization, methodology; Alain G. Bertoni: conceptualization, methodology; Deidra C. Crews: conceptualization, methodology; Wayne D. Rosamond: conceptualization, methodology; Josef Coresh: conceptualization, methodology; Chiadi E. Ndumele: conceptualization, methodology, writing—original draft, supervision; Kunihiro Matsushita: conceptualization, methodology, writing—original draft, supervision; Patricia P. Chang: conceptualization, methodology, writing—original draft, supervision.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Participating Institutions.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mathews, L., Ding, N., Sang, Y. et al. Racial Differences in Trends and Prognosis of Guideline-Directed Medical Therapy for Heart Failure with Reduced Ejection Fraction: the Atherosclerosis Risk in Communities (ARIC) Surveillance Study. J. Racial and Ethnic Health Disparities 10, 118–129 (2023). https://doi.org/10.1007/s40615-021-01202-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-021-01202-5