Abstract
Introduction
To improve kidney transplant allocation equitability, a new Kidney Allocation System (KAS) was implemented December 4, 2014. The purpose of this study was to determine if the impact of KAS on peri-operative outcomes differed by recipient race/ethnicity.
Methods
This was a time series analysis using data aggregated in monthly intervals from October 2012 through September 2015 using the University HealthSystem Consortium (UHC). This includes national data aggregated at the center level of all US kidney transplant centers that participate in the UHC (416 centers). Segmented regression with interaction terms was used to determine the impact of KAS on outcomes and differences by race/ethnicity.
Results
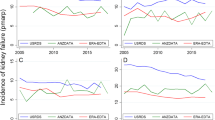
A total of 28,809 deceased donor kidney transplants were included with 25 months of pre-KAS data and 10 months of post-KAS data. After KAS implementation, the estimated transplant rate per month decreased significantly for Caucasians by 17.6 cases per month (p = 0.0001), and increased significantly for AAs by 37.8 (p = 0.0001), Hispanics by 16.3 (p = 0.0001), and other races by 8.2 cases per month (p = 0.0001). Delayed graft function, 7- and 14-day readmissions significantly increased after KAS, which did not differ by race. Hispanics saw a 7.7% decrease in ICU admissions after KAS, which differed as compared to other racial/ethnic cohorts (p = 0.0026). Costs of kidney transplantation increased significantly after KAS in all groups except Hispanics. Mortality, length of stay, in-hospital complications, and 30-day readmissions were not significantly impacted by KAS, also not differing by race/ethnicity.
Conclusion
KAS had substantial impact on transplant rates by race/ethnicity. KAS also led to increased costs, readmissions, and delayed graft function (DGF) across all racial/ethnic groups. The impact of KAS on ICU cases solely within Hispanics requires further investigation into potential etiologies.






Similar content being viewed by others
References
Organ Procurement and Transplantation Network. OPTN: Organ Procurement and Transplantation Network-OPTN. https://optn.transplant.hrsa.gov/. Accessed August 30, 2017.
Bray RA, Brannon P, Breitenbach C, et al. The new OPTN kidney allocation policy: potential for inequitable access among highly sensitized patients. Am J Transplant. 2014;15(1):284–5. https://doi.org/10.1111/ajt.13061.
Gebel HM, Kasiske BL, Gustafson SK, Pyke J, Shteyn E, Israni AK, et al. Allocating deceased donor kidneys to candidates with high panel-reactive antibodies. Clin J Am Soc Nephrol. 2016;11(3):505–11. https://doi.org/10.2215/cjn.07720715.
Formica RN, Friedewald JJ, Aeder M. Changing the kidney allocation system: a 20-year history. Curr Transplant Rep. 2016;3(1):39–44. https://doi.org/10.1007/s40472-016-0093-x.
Ladin K, Hanto DW. Rational rationing or discrimination: balancing equity and efficiency considerations in kidney allocation. Am J Transplant. 2011;11(11):2317–21. https://doi.org/10.1111/j.1600-6143.2011.03726.x.
Lefell MS, Zachary AA. The national impact of the 1995 changes to the UNOS renal allocation system. Clin Transpl. 1999;13(4):287–95. https://doi.org/10.1034/j.1399-0012.1999.130402.x.
Neylan JF, Sayegh MH, Coffman TM, Danovitch GM, Krensky AM, Strom TB, et al. The allocation of cadaver kidneys for transplantation in the United States: consensus and controversy. ASN transplant advisory group American Society of Nephrology. J Am Soc Nephrol. 1999;10(10):2237–43.
Sass DA, Doyle AM. Liver and kidney transplantation. Med Clin N Am. 2016;100(3):435–48. ISSN 0025-7125, https://doi.org/10.1016/j.mcna.2015.12.001
Smith JM, Biggins SW, Haselby DG, Kim WR, Wedd J, Lamb K, et al. Kidney, pancreas and liver allocation and distribution in the United States. Am J Transplant. 2012;12(12):3191–212. https://doi.org/10.1111/j.1600-6143.2012.04259.x.
Friedewald JJ, Samana CJ, Kasiske BL, Israni AK, Stewart D, Cherikh W, et al. The kidney allocation system. Surg Clin N Am. 2013;93(6):1395–406. https://doi.org/10.1016/j.suc.2013.08.007.
Chopra B, Sureshkumar KK. Changing organ allocation policy for kidney transplantation in the United States. World J Transplant. 2015;5(2):38–43. https://doi.org/10.5500/wjt.v5.i2.38.
Stewart DE, Kucheryavaya AY, Klassen DK, Turgeon NA, Formica RN, Aeder MI. Changes in deceased donor kidney transplantation one year after KAS implementation. Am J Transplant. 2016;16(6):1834–47. https://doi.org/10.1111/ajt.13770.
Melanson TA, Hockenberry JM, Plantinga L, Basu M, Pastan S, Mohan S, et al. New kidney allocation system associated with increased rates of transplants among black and Hispanic patients. Health Aff. 2017;36(6):1078–85. https://doi.org/10.1377/hlthaff.2016.1625.
Taber DJ, Mcgillicuddy JW, Bratton CF, Lin A, Chavin KD, Baliga PK. The concept of a composite perioperative quality index in kidney transplantation. J Am Coll Surg. 2014;218(4):588–97. https://doi.org/10.1016/j.jamcollsurg.2013.12.018.
Taber DJ, DuBay D, McGillicuddy JW, Nadig S, Bratton CF, Chavin KD, et al. Impact of the new kidney allocation system on perioperative outcomes and costs in kidney transplantation. J Am Coll Surg. 2017;224(4):585–92. https://doi.org/10.1016/j.jamcollsurg.2016.12.009.
Saunders MR, Lee H, Alexander GC, Tak HJ, Thistlethwaite JR, Ross LF. Racial disparities in reaching the renal transplant waitlist: is geography as important as race? Clin Transpl. 2015;29(6):531–8. https://doi.org/10.1111/ctr.12547.
Tambur AR, Haarberg KMK, Friedewald JJ, Leventhal JR, Cusick MF, Jaramillo A, et al. Unintended consequences of the new National Kidney Allocation Policy in the United States. Am J Transplant. 2015;15(9):2465–9. https://doi.org/10.1111/ajt.13381.
Cho PS, Saidi RF, Cutie CJ, Ko DSC. Competitive market analysis of transplant centers and discrepancy of wait-listing of recipients for kidney transplantation. Int J Organ Transplant Med. 2015;6(4):141–9.
Filiopoulos V, Boletis JN. Renal transplantation with expanded criteria donors: which is the optimal immunosuppression? World J Transplant. 2016;6(1):103. https://doi.org/10.5500/wjt.v6.il.103.
Israni AK, Salkowski N, Gustafson S, Snyder JJ, Friedewald JJ, Formica RN, et al. New National Allocation Policy for deceased donor kidneys in the United States and possible effect on patient outcomes. J Am Soc Nephrol. 2014;25(8):1842–8. https://doi.org/10.1681/asn.2013070784.
Acknowledgements
Medical University of South Carolina Department of Surgery and Medical University of South Carolina College of Medicine Alumni Association were acknowledged. This research was supported through grants from the National Institute of Diabetes and Digestive and Kidney Diseases under Award Numbers K23DK099440 and T35DK007431.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sanchez, D., Dubay, D., Prabhakar, B. et al. Evolving Trends in Racial Disparities for Peri-Operative Outcomes with the New Kidney Allocation System (KAS) Implementation. J. Racial and Ethnic Health Disparities 5, 1171–1179 (2018). https://doi.org/10.1007/s40615-018-0464-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-018-0464-3