Abstract
Purpose of Review
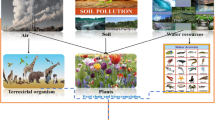
Exposure to inorganic arsenic (iAs) via drinking water represents a significant global public health threat with chronic exposure associated with cancer, skin lesions, neurological impairment, and cardiovascular diseases. Particularly susceptible populations include the developing fetus and young children. This review summarizes some of the critical studies of the long-term health effects and underlying biological mechanisms related to developmental exposure to arsenic. It also highlights the complex factors, such as the sex of the exposed individual, that contribute to susceptibility to the later life health effects of iAs.
Recent Findings
Studies in animal models, as well as human population-based studies, have established that prenatal and early life iAs exposures are associated with long-term effects, and many of these effects display sexually dimorphic responses. As an underlying molecular basis, recent epidemiologic and toxicologic studies have demonstrated that changes to the epigenome may play a key mechanistic role underlying many of the iAs-associated health outcomes.
Summary
Developmental exposure to iAs results in early and later life health effects. Mechanisms underlying these outcomes are likely complex, and include disrupted key biological pathways with ties to the epigenome. This highlights the importance of continued research, particularly in animal models, to elucidate the important underpinnings (e.g., timing of exposure, metabolism, dose) of these complex health outcomes and to identify the biological mechanisms underlying sexual dimorphism in iAs-associated diseases. Future research should investigate preventative strategies for the protection from the detrimental health endpoints associated with early life exposure to iAs. Such strategies could include potential interventions focused on dietary supplementation for example the adoption of a folate-rich diet.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Guidelines for Drinking-Water Quality, Fourth Edition. World Health Organization, 2011. http://apps.who.int/iris/bitstream/10665/44584/1/9789241548151_eng.pdf. Accessed 3 Aug 2017.
Naujokas MF, Anderson B, Ahsan H, Aposhian HV, Graziano JH, Thompson C, et al. The broad scope of health effects from chronic arsenic exposure: update on a worldwide public health problem. Environ Health Perspect. 2013;121(3):295–302. https://doi.org/10.1289/ehp.1205875.
Sanders AP, Messier KP, Shehee M, Rudo K, Serre ML, Fry RC. Arsenic in North Carolina: public health implications. Environ Int. 2012;38(1):10–6. https://doi.org/10.1016/j.envint.2011.08.005.
Baris D, Waddell R, Beane Freeman LE, Schwenn M, Colt JS, Ayotte JD, Ward MH, Nuckols J, Schned A, Jackson B, Clerkin C, Rothman N, Moore le, Taylor A, Robinson G, Hosain GMM, Armenti KR, McCoy R, Samanic C, Hoover RN, Fraumeni JF, Johnson A, Karagas MR, Silverman DT Elevated bladder cancer in northern New England: the role of drinking water and arsenic. J Natl Cancer Inst 2016;108(9). https://doi.org/10.1093/jnci/djw099.
Steinmaus C, Yuan Y, Bates MN, Smith AH. Case-control study of bladder cancer and drinking water arsenic in the western United States. Am J Epidemiol. 2003;158(12):1193–201. https://doi.org/10.1093/aje/kwg281.
Concha G, Vogler G, Lezcano D, Nermell B, Vahter M. Exposure to inorganic arsenic metabolites during early human development. Toxicol Sci. 1998;44(2):185–90. https://doi.org/10.1006/toxs.1998.2486.
Vahter M. Effects of arsenic on maternal and fetal health. Annu Rev Nutr. 2009;29(1):381–99. https://doi.org/10.1146/annurev-nutr-080508-141102.
Vahter M. Health effects of early life exposure to arsenic. Basic Clin Pharmacol Toxicol. 2008;102(2):204–11. https://doi.org/10.1111/j.1742-7843.2007.00168.x.
Farzan SF, Li Z, Korrick SA, Spiegelman D, Enelow R, Nadeau K, et al. Infant infections and respiratory symptoms in relation to in utero arsenic exposure in a U.S. cohort. Environ Health Perspect. 2016;124(6):840–7. https://doi.org/10.1289/ehp.1409282.
Recio-Vega R, Gonzalez-Cortes T, Olivas-Calderon E, Lantz RC, Gandolfi AJ, Gonzalez-De Alba C. In utero and early childhood exposure to arsenic decreases lung function in children. J Appl Toxicol. 2015;35(4):358–66. https://doi.org/10.1002/jat.3023.
Smith AH, Marshall G, Liaw J, Yuan Y, Ferreccio C, Steinmaus C. Mortality in young adults following in utero and childhood exposure to arsenic in drinking water. Environ Health Perspect. 2012;120(11):1527–31. https://doi.org/10.1289/ehp.1104867.
Yuan Y, Marshall G, Ferreccio C, Steinmaus C, Selvin S, Liaw J, et al. Acute myocardial infarction mortality in comparison with lung and bladder cancer mortality in arsenic-exposed region II of Chile from 1950 to 2000. Am J Epidemiol. 2007;166(12):1381–91. https://doi.org/10.1093/aje/kwm238.
Raqib R, Ahmed S, Sultana R, Wagatsuma Y, Mondal D, Hoque AM, et al. Effects of in utero arsenic exposure on child immunity and morbidity in rural Bangladesh. Toxicol Lett. 2009;185(3):197–202. https://doi.org/10.1016/j.toxlet.2009.01.001.
von Ehrenstein OS, Poddar S, Yuan Y, Mazumder DG, Eskenazi B, Basu A, et al. Children’s intellectual function in relation to arsenic exposure. Epidemiology. 2007;18(1):44–51. https://doi.org/10.1097/01.ede.0000248900.65613.a9.
Davis MA, Mackenzie TA, Cottingham KL, Gilbert-Diamond D, Punshon T, Karagas MR. Rice consumption and urinary arsenic concentrations in U.S. children. Environ Health Perspect. 2012;120(10):1418–24. https://doi.org/10.1289/ehp.1205014.
Jackson BP, Taylor VF, Karagas MR, Punshon T, Cottingham KL. Arsenic, organic foods, and brown rice syrup. Environ Health Perspect. 2012;120(5):623–6. https://doi.org/10.1289/ehp.1104619.
Karagas MR, Punshon T, Sayarath V, Jackson BP, Folt CL, Cottingham KL. Association of rice and rice-product consumption with arsenic exposure early in life. JAMA Pediatr. 2016;170(6):609–16. https://doi.org/10.1001/jamapediatrics.2016.0120.
•• Quansah R, Armah FA, Essumang DK, Luginaah I, Clarke E, Marfoh K, et al. Association of arsenic with adverse pregnancy outcomes/infant mortality: a systematic review and meta-analysis. Environ Health Perspect. 2015;123(5):412–21. https://doi.org/10.1289/ehp.1307894. Provides a concise systematic review of reproductive/birth outcomes and perinatal health associated with iAs exposure.
El-Baz MAH, El-Deeb TS, El-Noweihi AM, Mohany KM, Shaaban OM, Abbas AM. Environmental factors and apoptotic indices in patients with intrauterine growth retardation: a nested case-control study. Environ Toxicol Pharmacol. 2015;39(2):589–96. https://doi.org/10.1016/j.etap.2015.01.009.
Peng S, Liu L, Zhang X, Heinrich J, Zhang J, Schramm KW, et al. A nested case-control study indicating heavy metal residues in meconium associate with maternal gestational diabetes mellitus risk. Environ Health. 2015;14(1):19. https://doi.org/10.1186/s12940-015-0004-0.
Hopenhayn-Rich C, Browning SR, Hertz-Picciotto I, Ferreccio C, Peralta C, Gibb H. Chronic arsenic exposure and risk of infant mortality in two areas of Chile. Environ Health Perspect. 2000;108(7):667–73. https://doi.org/10.1289/ehp.00108667.
Gelmann ER, Gurzau E, Gurzau A, Goessler W, Kunrath J, Yeckel CW, et al. A pilot study: the importance of inter-individual differences in inorganic arsenic metabolism for birth weight outcome. Environ Toxicol Pharmacol. 2013;36(3):1266–75. https://doi.org/10.1016/j.etap.2013.10.006.
Laine JE, Bailey KA, Rubio-Andrade M, Olshan AF, Smeester L, Drobna Z, et al. Maternal arsenic exposure, arsenic methylation efficiency, and birth outcomes in the Biomarkers of Exposure to ARsenic (BEAR) pregnancy cohort in Mexico. Environ Health Perspect. 2015;123(2):186–92. https://doi.org/10.1289/ehp.1307476.
Rahman A, Vahter M, Smith AH, Nermell B, Yunus M, El Arifeen S, et al. Arsenic exposure during pregnancy and size at birth: a prospective cohort study in Bangladesh. Am J Epidemiol. 2009;169(3):304–12. https://doi.org/10.1093/aje/kwn332.
Gilbert-Diamond D, Emond JA, Baker ER, Korrick SA, Karagas MR. Relation between arsenic exposure and birth outcomes in a cohort of mothers and their newborns from New Hampshire. Environ Health Perspect. 2016;124(8):1299–307. https://doi.org/10.1289/ehp.1510065.
Davis MA, Higgins J, Li Z, Gilbert-Diamond D, Baker ER, Das A, et al. Preliminary analysis of in utero low-level arsenic exposure and fetal growth using biometric measurements extracted from fetal ultrasound reports. Environ Health. 2015;14(1):1–11. https://doi.org/10.1186/1476-069x-14-12.
Newcombe R, Milne BJ, Caspi A, Poulton R, Moffitt TE. Birthweight predicts IQ: fact or artefact? Twin Res Hum Genet. 2007;10(4):581–6. https://doi.org/10.1375/twin.10.4.581.
Gale CR, O'Callaghan FJ, Bredow M, Martyn CN. The influence of head growth in fetal life, infancy, and childhood on intelligence at the ages of 4 and 8 years. Pediatrics. 2006;118(4):1486–92. https://doi.org/10.1542/peds.2005-2629.
Dakeishi M, Murata K, Grandjean P. Long-term consequences of arsenic poisoning during infancy due to contaminated milk powder. Environ Health. 2006;5(1):31. https://doi.org/10.1186/1476-069x-5-31.
Yorifuji T, Kato T, Ohta H, Bellinger DC, Matsuoka K, Grandjean P. Neurological and neuropsychological functions in adults with a history of developmental arsenic poisoning from contaminated milk powder. Neurotoxicol Teratol. 2016;53:75–80. https://doi.org/10.1016/j.ntt.2015.12.001.
Wasserman GA, Liu X, Parvez F, Factor-Litvak P, Ahsan H, Levy D, et al. Arsenic and manganese exposure and children’s intellectual function. Neurotoxicology. 2011;32(4):450–7. https://doi.org/10.1016/j.neuro.2011.03.009.
Rosado JL, Ronquillo D, Kordas K, Rojas O, Alatorre J, Lopez P, et al. Arsenic exposure and cognitive performance in Mexican schoolchildren. Environ Health Perspect. 2007;115(9):1371–5. https://doi.org/10.1289/ehp.9961.
Hsieh RL, Huang YL, Shiue HS, Huang SR, Lin MI, Mu SC, et al. Arsenic methylation capacity and developmental delay in preschool children in Taiwan. Int J Hyg Environ Health. 2014;217(6):678–86. https://doi.org/10.1016/j.ijheh.2014.02.004.
Wasserman GA, Liu X, Loiacono NJ, Kline J, Factor-Litvak P, van Geen A, et al. A cross-sectional study of well water arsenic and child IQ in Maine schoolchildren. Environ Health. 2014;13(1):23. https://doi.org/10.1186/1476-069x-13-23.
Hamadani JD, Tofail F, Nermell B, Gardner R, Shiraji S, Bottai M, et al. Critical windows of exposure for arsenic-associated impairment of cognitive function in pre-school girls and boys: a population-based cohort study. Int J Epidemiol. 2011;40(6):1593–604. https://doi.org/10.1093/ije/dyr176.
Hamadani JD, SM G-MG, Tofail F, Nermell B, Fangstrom B, Huda SN, et al. Pre- and postnatal arsenic exposure and child development at 18 months of age: a cohort study in rural Bangladesh. Int J Epidemiol. 2010;39(5):1206–16. https://doi.org/10.1093/ije/dyp369.
Andrew AS, Jewell DA, Mason RA, Whitfield ML, Moore JH, Karagas MR. Drinking-water arsenic exposure modulates gene expression in human lymphocytes from a U.S. population. Environ Health Perspect. 2008;116(4):524–31. https://doi.org/10.1289/ehp.10861.
Biswas R, Ghosh P, Banerjee N, Das JK, Sau T, Banerjee A, et al. Analysis of T-cell proliferation and cytokine secretion in the individuals exposed to arsenic. Hum Exp Toxicol. 2008;27(5):381–6. https://doi.org/10.1177/0960327108094607.
Dangleben NL, Skibola CF, Smith MT. Arsenic immunotoxicity: a review. Environ Health. 2013;12(1):73. https://doi.org/10.1186/1476-069X-12-73.
Smith AH, Yunus M, Khan AF, Ercumen A, Yuan Y, Smith MH, et al. Chronic respiratory symptoms in children following in utero and early life exposure to arsenic in drinking water in Bangladesh. Int J Epidemiol. 2013;42(4):1077–86. https://doi.org/10.1093/ije/dyt120.
Rahman A, Vahter M, Ekstrom EC, Persson LA. Arsenic exposure in pregnancy increases the risk of lower respiratory tract infection and diarrhea during infancy in Bangladesh. Environ Health Perspect. 2011;119(5):719–24. https://doi.org/10.1289/ehp.1002265.
Farzan SF, Korrick S, Li Z, Enelow R, Gandolfi AJ, Madan J, et al. In utero arsenic exposure and infant infection in a United States cohort: a prospective study. Environ Res. 2013;126:24–30. https://doi.org/10.1016/j.envres.2013.05.001.
Ahmed S, Akhtar E, Roy A, von Ehrenstein OS, Vahter M, Wagatsuma Y, et al. Arsenic exposure alters lung function and airway inflammation in children: a cohort study in rural Bangladesh. Environ Int. 2017;101:108–16. https://doi.org/10.1016/j.envint.2017.01.014.
Dauphine DC, Ferreccio C, Guntur S, Yuan Y, Hammond SK, Balmes J, et al. Lung function in adults following in utero and childhood exposure to arsenic in drinking water: preliminary findings. Int Arch Occup Environ Health. 2011;84(6):591–600. https://doi.org/10.1007/s00420-010-0591-6.
Fry RC, Navasumrit P, Valiathan C, Svensson JP, Hogan BJ, Luo M, et al. Activation of inflammation/NF-kappaB signaling in infants born to arsenic-exposed mothers. PLoS Genet. 2007;3(11):e207. https://doi.org/10.1371/journal.pgen.0030207.
Rager JE, Bailey KA, Smeester L, Miller SK, Parker JS, Laine JE, et al. Prenatal arsenic exposure and the epigenome: altered microRNAs associated with innate and adaptive immune signaling in newborn cord blood. Environ Mol Mutagen. 2014;55(3):196–208. https://doi.org/10.1002/em.21842.
Ahmed S, Ahsan KB, Kippler M, Mily A, Wagatsuma Y, Hoque AM, et al. In utero arsenic exposure is associated with impaired thymic function in newborns possibly via oxidative stress and apoptosis. Toxicol Sci. 2012;129(2):305–14. https://doi.org/10.1093/toxsci/kfs202.
Soto-Pena GA, Luna AL, Acosta-Saavedra L, Conde P, Lopez-Carrillo L, Cebrian ME, et al. Assessment of lymphocyte subpopulations and cytokine secretion in children exposed to arsenic. FASEB J. 2006;20(6):779–81. https://doi.org/10.1096/fj.05-4860fje.
Ahmed S, Moore SE, Kippler M, Gardner R, Hawlader MD, Wagatsuma Y, et al. Arsenic exposure and cell-mediated immunity in pre-school children in rural Bangladesh. Toxicol Sci. 2014;141(1):166–75. https://doi.org/10.1093/toxsci/kfu113.
Smeester L, Bommarito PA, Martin EM, Recio-Vega R, Gonzalez-Cortes T, Olivas-Calderon E, et al. Chronic early childhood exposure to arsenic is associated with a TNF-mediated proteomic signaling response. Environ Toxicol Pharmacol. 2017;52:183–7. https://doi.org/10.1016/j.etap.2017.04.007.
Chen Y, Graziano JH, Parvez F, Liu M, Slavkovich V, Kalra T, et al. Arsenic exposure from drinking water and mortality from cardiovascular disease in Bangladesh: prospective cohort study. BMJ. 2011;342(may05 2):d2431. https://doi.org/10.1136/bmj.d2431.
Moon KA, Guallar E, Umans JG, Devereux RB, Best LG, Francesconi KA, et al. Association between exposure to low to moderate arsenic levels and incident cardiovascular disease. A prospective cohort study. Ann Intern Med. 2013;159(10):649–59. https://doi.org/10.7326/0003-4819-159-10-201311190-00719.
Chen CJ, Chiou HY, Chiang MH, Lin LJ, Tai TY. Dose-response relationship between I schemic heart disease mortality and long-term arsenic exposure. Arterioscler Thromb Vasc Biol. 1996;16(4):504–10. https://doi.org/10.1161/01.ATV.16.4.504.
Rahman M, Tondel M, Ahmad SA, Chowdhury IA, Faruquee MH, Axelson O. Hypertension and arsenic exposure in Bangladesh. Hypertension. 1999;33(1):74–8. https://doi.org/10.1161/01.HYP.33.1.74.
Rosenberg HG. Systemic arterial disease with myocardial infarction. Report on two infants. Circulation. 1973;47(2):270–5. https://doi.org/10.1161/01.CIR.47.2.270.
Systemic RHG. Arterial disease and chronic arsenicism in infants. Arch Pathol. 1974;97(6):360–5.
Rahman M, Sohel N, Yunus M, Chowdhury ME, Hore SK, Zaman K, et al. Increased childhood mortality and arsenic in drinking water in MATLAB, Bangladesh: a population-based cohort study. PLoS One. 2013;8(1):e55014. https://doi.org/10.1371/journal.pone.0055014.
Hawkesworth S, Wagatsuma Y, Kippler M, Fulford AJ, Arifeen SE, Persson LA, et al. Early exposure to toxic metals has a limited effect on blood pressure or kidney function in later childhood, rural Bangladesh. Int J Epidemiol. 2013;42(1):176–85. https://doi.org/10.1093/ije/dys215.
Osorio-Yáñez C, Ayllon-Vergara JC, Aguilar-Madrid G, Arreola-Mendoza L, Hernández-Castellanos E, Barrera-Hernández A, et al. Carotid intima-media thickness and plasma asymmetric dimethylarginine in Mexican children exposed to inorganic arsenic. Environ Health Perspect. 2013;121(9):1090–6. https://doi.org/10.1289/ehp.1205994.
Farzan SF, Brickley EB, Li Z, Gilbert-Diamond D, Gossai A, Chen Y, et al. Maternal and infant inflammatory markers in relation to prenatal arsenic exposure in a U.S. pregnancy cohort. Environ Res. 2017;156:426–33. https://doi.org/10.1016/j.envres.2017.03.056.
Liaw J, Marshall G, Yuan Y, Ferreccio C, Steinmaus C, Smith AH. Increased childhood liver cancer mortality and arsenic in drinking water in northern Chile. Cancer Epidemiol Biomark Prev. 2008;17(8):1982–7. https://doi.org/10.1158/1055-9965.epi-07-2816.
Smith AH, Marshall G, Yuan Y, Ferreccio C, Liaw J, von Ehrenstein O, et al. Increased mortality from lung cancer and bronchiectasis in young adults after exposure to arsenic in utero and in early childhood. Environ Health Perspect. 2006;114(8):1293–6. https://doi.org/10.1289/ehp.8832.
Wang JP, Qi L, Moore MR, Ng JC. A review of animal models for the study of arsenic carcinogenesis. Toxicol Lett. 2002;133(1):17–31. https://doi.org/10.1016/S0378-4274(02)00086-3.
Waalkes MP, Ward JM, Liu J, Diwan BA. Transplacental carcinogenicity of inorganic arsenic in the drinking water: induction of hepatic, ovarian, pulmonary, and adrenal tumors in mice. Toxicol Appl Pharmacol. 2003;186(1):7–17. https://doi.org/10.1016/S0041-008X(02)00022-4.
Tokar EJ, Diwan BA, Ward JM, Delker DA, Waalkes MP. Carcinogenic effects of “whole-life” exposure to inorganic arsenic in CD1 mice. Toxicol Sci. 2011;119(1):73–83. https://doi.org/10.1093/toxsci/kfq315.
Waalkes MP, Ward JM, Diwan BA. Induction of tumors of the liver, lung, ovary and adrenal in adult mice after brief maternal gestational exposure to inorganic arsenic: promotional effects of postnatal phorbol ester exposure on hepatic and pulmonary, but not dermal cancers. Carcinogenesis. 2004;25(1):133–41. https://doi.org/10.1093/carcin/bgg181.
Liu J, Xie Y, Cooper R, Ducharme DM, Tennant R, Diwan BA, et al. Transplacental exposure to inorganic arsenic at a hepatocarcinogenic dose induces fetal gene expression changes in mice indicative of aberrant estrogen signaling and disrupted steroid metabolism. Toxicol Appl Pharmacol. 2007;220(3):284–91. https://doi.org/10.1016/j.taap.2007.01.018.
Tseng C-H. Arsenic methylation, urinary arsenic metabolites and human diseases: current perspective. J Environ Sci Health, Part C. 2007;25(1):1–22. https://doi.org/10.1080/10590500701201695.
Tokar EJ, Diwan BA, Thomas DJ, Waalkes MP. Tumors and proliferative lesions in adult offspring after maternal exposure to methylarsonous acid during gestation in CD1 mice. Arch Toxicol. 2012;86(6):975–82. https://doi.org/10.1007/s00204-012-0820-8.
Waalkes MP, Qu W, Tokar EJ, Kissling GE, Dixon D. Lung tumors in mice induced by “whole-life” inorganic arsenic exposure at human-relevant doses. Arch Toxicol. 2014;88(8):1619–29. https://doi.org/10.1007/s00204-014-1305-8.
Waalkes MP, Liu J, Diwan BA. Transplacental arsenic carcinogenesis in mice. Toxicol Appl Pharmacol. 2007;222(3):271–80. https://doi.org/10.1016/j.taap.2006.12.034.
Xie Y, Liu J, Benbrahim-Tallaa L, Ward JM, Logsdon D, Diwan BA, et al. Aberrant DNA methylation and gene expression in livers of newborn mice transplacentally exposed to a hepatocarcinogenic dose of inorganic arsenic. Toxicology. 2007;236(1–2):7–15. https://doi.org/10.1016/j.tox.2007.03.021.
Sullivan JP, Minna JD, Shay JW. Evidence for self-renewing lung cancer stem cells and their implications in tumor initiation, progression, and targeted therapy. Cancer Metastasis Rev. 2010;29(1):61–72. https://doi.org/10.1007/s10555-010-9216-5.
Wicha MS, Liu S, Dontu G. Cancer stem cells: an old idea—a paradigm shift. Cancer Res. 2006;66(4):1883–90; discussion 95-6. https://doi.org/10.1158/0008-5472.CAN-05-3153.
Kangsamaksin T, Park HJ, Trempus CS, Morris RJ. A perspective on murine keratinocyte stem cells as targets of chemically induced skin cancer. Mol Carcinog. 2007;46(8):579–84. https://doi.org/10.1002/mc.20355.
Sun Y, Tokar EJ, Waalkes MP. Overabundance of putative cancer stem cells in human skin keratinocyte cells malignantly transformed by arsenic. Toxicol Sci: Off J Soc Toxicol. 2012;125(1):20–9. https://doi.org/10.1093/toxsci/kfr282.
Chang Q, Chen B, Thakur C, Lu Y, Chen F. Arsenic-induced sub-lethal stress reprograms human bronchial epithelial cells to CD61 cancer stem cells. Oncotarget. 2014;5(5):1290–303. https://doi.org/10.18632/oncotarget.1789.
Waalkes MP, Liu J, Germolec DR, Trempus CS, Cannon RE, Tokar EJ, et al. Arsenic exposure in utero exacerbates skin cancer response in adulthood with contemporaneous distortion of tumor stem cell dynamics. Cancer Res. 2008;68(20):8278–85. https://doi.org/10.1158/0008-5472.can-08-2099.
States JC, Singh AV, Knudsen TB, Rouchka EC, Ngalame NO, Arteel GE, et al. Prenatal arsenic exposure alters gene expression in the adult liver to a proinflammatory state contributing to accelerated atherosclerosis. PLoS One. 2012;7(6):e38713. https://doi.org/10.1371/journal.pone.0038713.
Aung KH, Kyi-Tha-Thu C, Sano K, Nakamura K, Tanoue A, Nohara K, et al. Prenatal exposure to arsenic impairs behavioral flexibility and cortical structure in mice. Front Neurosci. 2016;10:137. https://doi.org/10.3389/fnins.2016.00137.
Gutierrez-Torres DS, Gonzalez-Horta C, Del Razo LM, Infante-Ramirez R, Ramos-Martinez E, Levario-Carrillo M, et al. Prenatal exposure to sodium Arsenite alters placental glucose 1, 3, and 4 transporters in BALB/c mice. Biomed Res Int. 2015;2015:175025. https://doi.org/10.1155/2015/175025.
•• Rodriguez KF, Ungewitter EK, Crespo-Mejias Y, Liu C, Nicol B, Kissling GE, et al. Effects of in utero exposure to arsenic during the second half of gestation on reproductive end points and metabolic parameters in female CD-1 mice. Environ Health Perspect. 2016;124(3):336–43. https://doi.org/10.1289/ehp.1509703. This study illustrates that even at the WHO recommended limit of 10ppb for arsenic in drinking water, prenatal iAs exposure is associated with late onset adverse outcomes.
Lantz RC, Chau B, Sarihan P, Witten ML, Pivniouk VI, Chen GJ. In utero and postnatal exposure to arsenic alters pulmonary structure and function. Toxicol Appl Pharmacol. 2009;235(1):105–13. https://doi.org/10.1016/j.taap.2008.11.012.
Waalkes MP, Liu J, Chen H, Xie Y, Achanzar WE, Zhou Y-S, et al. Estrogen signaling in livers of male mice with hepatocellular carcinoma induced by exposure to arsenic in utero. J Natl Cancer Inst. 2004;96(6):466–74. https://doi.org/10.1093/jnci/djh070.
Ahmed S, Mahabbat-e Khoda S, Rekha RS, Gardner RM, Ameer SS, Moore S, et al. Arsenic-associated oxidative stress, inflammation, and immune disruption in human placenta and cord blood. Environ Health Perspect. 2011;119(2):258–64. https://doi.org/10.1289/ehp.1002086.
Bailey KA, Laine J, Rager JE, Sebastian E, Olshan A, Smeester L, et al. Prenatal arsenic exposure and shifts in the newborn proteome: interindividual differences in tumor necrosis factor (TNF)-responsive signaling. Toxicol Sci: Off J Soc Toxicol. 2014;139(2):328–37. https://doi.org/10.1093/toxsci/kfu053.
Kile ML, Houseman EA, Baccarelli AA, Quamruzzaman Q, Rahman M, Mostofa G, et al. Effect of prenatal arsenic exposure on DNA methylation and leukocyte subpopulations in cord blood. Epigenetics. 2014;9(5):774–82. https://doi.org/10.4161/epi.28153.
Rojas D, Rager JE, Smeester L, Bailey KA, Drobná Z, Rubio-Andrade M, et al. Prenatal arsenic exposure and the epigenome: identifying sites of 5-methylcytosine alterations that predict functional changes in gene expression in newborn cord blood and subsequent birth outcomes. Toxicol Sci. 2015;143(1):97–106. https://doi.org/10.1093/toxsci/kfu210.
Sanders AP, Smeester L, Rojas D, DeBussycher T, Wu MC, Wright FA, et al. Cadmium exposure and the epigenome: exposure-associated patterns of DNA methylation in leukocytes from mother-baby pairs. Epigenetics. 2014;9(2):212–21. https://doi.org/10.4161/epi.26798.
Horikoshi M, Yaghootkar H, Mook-Kanamori DO, Sovio U, Taal HR, Hennig BJ, et al. New loci associated with birth weight identify genetic links between intrauterine growth and adult height and metabolism. Nat Genet. 2013;45(1):76–82. https://doi.org/10.1038/ng.2477.
St-Pierre J, Hivert M-F, Perron P, Poirier P, Guay S-P, Brisson D, et al. IGF2 DNA methylation is a modulator of newborn’s fetal growth and development. Epigenetics. 2012;7(10):1125–32. https://doi.org/10.4161/epi.21855.
• Martin E, Smeester L, Bommarito PA, Grace MR, Boggess K, Kuban K, et al. Sexual epigenetic dimorphism in the human placenta: implications for susceptibility during the prenatal period. Epigenomics. 2017;9(3):267–78. https://doi.org/10.2217/epi-2016-0132. This study highlights sexually-dimorphic epigenetic patterns in the placenta that likely influence the response to toxic substances such as inorganic arsenic.
Silveira PP, Portella AK, Goldani MZ, Barbieri MA. Developmental origins of health and disease (DOHaD). J pediatr. 2007;83(6):494–504. https://doi.org/10.2223/JPED.1728.
Vickers M. Early life nutrition, epigenetics and programming of later life disease. Nutrients. 2014;6(6):2165–78. https://doi.org/10.3390/nu6062165.
Vanhees K, Vonhogen IG, van Schooten FJ, Godschalk RW. You are what you eat, and so are your children: the impact of micronutrients on the epigenetic programming of offspring. Cell Mol life Sci: CMLS. 2014;71(2):271–85. https://doi.org/10.1007/s00018-013-1427-9.
Acknowledgements
This work was supported by grants from the National Institute of Environmental Health Sciences (R01ES019315 and P42ES005948). We would like to thank Caroline Brock Reed for her assistance with Fig. 1.
Author information
Authors and Affiliations
Ethics declarations
Conflict of Interest
Lisa Smeester and Rebecca C. Fry declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Mechanisms of Toxicity
Rights and permissions
About this article
Cite this article
Smeester, L., Fry, R.C. Long-Term Health Effects and Underlying Biological Mechanisms of Developmental Exposure to Arsenic. Curr Envir Health Rpt 5, 134–144 (2018). https://doi.org/10.1007/s40572-018-0184-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40572-018-0184-1