Abstract
Background
Dynapenic abdominal obesity (DAO) (i.e., impairment in muscle strength and high waist circumference) is gaining interest, as it is associated with several important adverse health outcomes. However, the association between DAO and multimorbidity is largely unclear. Thus, the aim of the present study was to investigate the association between DAO at baseline and new onset multimorbidity over ten years of follow-up.
Methods
People participating in the English Longitudinal Study of Ageing were included. DAO was defined as waist circumference > 102 cm in men and > 88 cm in women, and a concomitant presence of dynapenia (handgrip strength defined as < 27 kg for men and < 16 kg for women). Multimorbidity was defined as having two or more chronic conditions. The association between DAO and incident multimorbidity was assessed using a multivariable logistic regression analysis, reporting the data as odds ratios (ORs) and their 95% confidence intervals (CIs).
Results
Overall, 3302 participants (mean age: 63.4 years, males: 50.3%) without multimorbidity at baseline were followed-up for ten years. After adjusting for several variables, compared to participants without dynapenia nor abdominal obesity, the presence of abdominal obesity (OR = 1.505; 95%CI: 1.272–1.780; p < 0.0001) and DAO (OR = 1.671; 95%CI: 1.201–2.325; p = 0.002) significantly increased the risk of multimorbidity. Compared to no dynapenia nor abdominal obesity, DAO was associated with significantly higher risk for arthritis and diabetes.
Conclusions
DAO was significantly associated with a higher risk of incident multimorbidity, over 10 years of follow-up. The results of our study suggest that addressing DAO can potentially decrease risk for multimorbidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-communicable diseases (NCDs) are now responsible for almost all global deaths [1]. It is largely known that NCDs are most common in older adults, and a substantial increase in NCDs burden is expected due to the rapid ageing population [2]. In this context, the presence of two or more chronic conditions is commonly called multimorbidity [3]. Multimorbidity is an important risk factor for several adverse health outcomes such as lower quality of life [4], increased health-care utilization [5], dementia[6], and ultimately higher risk of premature mortality [7].
In recent years, there has been increasing interest in dynapenic abdominal obesity (DAO) (i.e., impairment in muscle strength and high waist circumference)[8] as a clinical risk concept since this specific condition has been observed to be associated with several important adverse health outcomes including falls [9, 10], metabolic alterations [11], disability [12], and premature death [13], similarly to multimorbidity. Literature indicates that DAO may increase the risk for chronic diseases and consequently multimorbidity as weak muscle strength has been found to be associated with an unfavorable inflammatory profile (e.g., higher levels of C-reactive proteins and fibrinogen) [14], while the metabolic risk associated with obesity is more strongly associated with central rather than peripheral fat distribution [15]. Therefore, it is possible for people with DAO to be at particularly high risk for multimorbidity, but there are currently no longitudinal studies on this topic, that can better elucidate the potential role of DAO as a risk factor for multimorbidity.
Given this background, the aim of the present study was to investigate the association between DAO at baseline and new onset multimorbidity over 10 years of follow-up in a large representative sample of the English older adult population, while also exploring the association between DAO and single incident chronic medical conditions.
Materials and methods
Study population
This study is based on data from six waves (from wave 2 to wave 7) of the English Longitudinal Study of Ageing (ELSA). The ELSA study is a prospective and nationally representative cohort of men and women living in England [16]. Wave 2 (baseline survey) was conducted between 2004 and 2005, and wave 7 between 2014 and 2015. Other waves took place every two years between these dates. The ELSA was approved by the London Multicenter Research Ethics Committee (MREC/01/2/91). Informed consent was obtained from all participants.
DAO (exposure variable)
Dynapenia was defined using the criteria proposed by the revised European consensus on the definition and diagnosis of sarcopenia [17], i.e., having weak handgrip strength defined as < 27 kg for men and < 16 kg for women (using the average value of three handgrip measurements of the dominant hand) [17]. We used mean values instead of maximum, owing to previous literature showing a good agreement between these two parameters and that in the ELSA study mean values of handgrip strength are usually employed. [18,19,20] Abdominal obesity was defined using the traditional cut-offs of 102 cm in men, 88 cm in women [21]. All respondents were eligible to have their waist and hip measurements taken, unless they were chairbound or had a colostomy or ileostomy. The waist circumference was evaluated twice; if the second measurement differed from the first by 3 cm or more, the nurse was given an error message and took a third measurement. The measurement of the waist was made with the participant standing. DAO was then defined as the combination of these two entities.
Multimorbidity (outcome)
Information on the presence of medical conditions was collected by self-report on doctor diagnosed high blood pressure, diabetes, cancer, lung disease, heart conditions, stroke, psychiatric conditions, arthritis, asthma, high cholesterol levels, cataracts, Parkinson’s disease, hip fracture, Alzheimer’s disease, and other dementias. The total number of chronic conditions was then summed and multimorbidity was defined as ≥ 2 chronic conditions, in line with previously used definitions [22,23,24]. The presence of multimorbidity was ascertained at the baseline (wave 2) and then at wave 3, 4, 5, 6, and 7.
Covariates
The selection of covariates was based on their previously reported associations with the exposure (DAO) and outcome (multimorbidity) [25] and included the following: age (in years, as continuous variable); sex; years of education (considered as a continuous variable); ethnicity (whites vs. non-whites); marital status (categorized as married, partnered, separated, divorced, widowed, never married); smoking status (ever vs. never); alcohol drinking (categorized as yes or no); physical activity level categorized as sedentary, low, moderate or high according to a question about the frequency with which they did moderate exercise in the previous week (e.g., gardening, cleaning the car, walking at a moderate pace, dancing, floor or stretching exercise).
Statistical analyses
The data were weighted using the person-level longitudinal weight, core sample, wave 2 (http://www.ifs.org.uk/ELSA). Means and standard deviations (SD) were used to describe quantitative measures, while percentages and counts were used for categorical variables. Characteristics of the study participants at baseline were compared according to the presence of multimorbidity during follow-up, using Chi-squared or Fisher exact tests for categorical variables, and independent T-test for continuous variables.
The analyses were restricted to those who did not have multimorbidity at baseline to better evaluate the prospective risk of this condition among people initially free of multimorbidity. The association between the exposure variable at baseline (categorized as no dynapenia nor abdominal obesity [reference], only dynapenia, only abdominal obesity, and DAO) and incident multimorbidity was assessed using univariable and multivariable logistic regression analysis and reported as odds ratios (OR) and 95% confidence intervals (95% CI). The multivariable analysis adjusted for age, sex, alcohol drinking, educational level, ethnicity, marital status, smoking status, physical activity level, and presence of one chronic condition at baseline. The covariates used for analysis were initially chosen based on the previous literature. These variables were included in the final model if they were significantly different between people with and without multimorbidity during the follow-up in univariate analyses, using a conservative p-value of < 0.10. We also explored the association between DAO and incident single conditions, adjusted for all covariates, after removing the participants with that specific condition at baseline.
All statistical tests were two-tailed, and a p-value < 0.05 was considered statistically significant. All analyses were performed using SPSS 26.0 version software.
Results
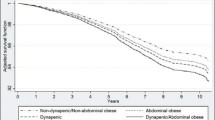
Figure 1 shows the inclusion flow-chart for this study. At the baseline evaluation (wave 2), 9432 participants were initially considered. We subsequently removed 1922 participants since no data regarding dynapenia were available, 220 had no data regarding waist circumference, and 3685 already had two or more medical conditions at the baseline. Moreover, for 303 participants, no data regarding incident multimorbidity were available, finally leaving 3302 eligible participants for the analysis on DAO and multimorbidity.
The 3302 participants had a mean age of 63.4 ± SD 8.9 years (range: 52–90), with an approximately equal distribution of males and females (50.3%, male). During the 10-year follow-up, 1810 (55.0% of the initial population) developed multimorbidity and these people were significantly older, less educated, more frequently smokers, and less likely to consume alcohol than those without multimorbidity. Moreover, incident multimorbidity (vs. no incident multimorbidity) was associated with a lower prevalence at baseline of high physical activity level (Table 1). Among the conditions considered at the baseline, a higher prevalence of high blood pressure, diabetes, lung and heart diseases, and arthritis was observed in people with multimorbidity compared to those without. Finally, a higher prevalence of dynapenia, abdominal obesity, and DAO was observed in participants with incident multimorbidity compared to those without this condition during follow-up (Table 1).
Table 2 shows the association between dynapenia, abdominal obesity, and DAO at baseline and multimorbidity during follow-up. Compared to participants without dynapenia and abdominal obesity, participants with only dynapenia did not report any significant risk of multimorbidity during follow-up (p = 0.806), whilst the presence of abdominal obesity (OR = 1.505; 95%CI: 1.272–1.780; p < 0.0001) and DAO (OR = 1.671; 95%CI: 1.201–2.325; p = 0.002) significantly increased the risk of multimorbidity. Other risk factors which were significantly associated with incident multimorbidity were older age, female sex, fewer years in education, and those separated (versus married) (Table 2).
Table 3 shows the association between dynapenia, abdominal obesity, or DAO, at baseline and single medical conditions during follow-up. Compared to people without dynapenia or abdominal obesity, the presence of only dynapenia significantly increased the risk of diabetes (OR = 2.44; 95%CI: 1.21–4.91; P = 0.001), whilst the presence of only abdominal obesity increased the risk of high blood pressure (OR = 1.43; 95%CI: 1.15–1.78; P = 0.001), diabetes (OR = 4.56; 95%CI: 2.99–6.95; P < 0.0001), arthritis (OR = 1.48; 95%CI: 1.18–1.86; P = 0.001), and high cholesterol levels (OR = 1.24; 95%CI: 1.03–1-49; P = 0.02). DAO increased the risk of diabetes (OR = 5.87; 95%CI: 3.13–11.03; P < 0.0001) and arthritis (OR = 1.92; 95%CI: 1.27–2.92; P = 0.002) (Table 3).
Discussion
In this large nationally representative sample of UK adults, we found that the presence of abdominal obesity and DAO significantly increased the risk of multimorbidity over ten years of follow-up. DAO was significantly associated with incident multimorbidity, whilst dynapenia was not. Moreover, DAO further increases the risk of multimorbidity during the follow-up when compared to the presence of only abdominal obesity. In terms of the individual chronic conditions, compared to no dynapenia nor abdominal obesity, DAO was associated with significantly higher risk for arthritis and diabetes. To the best of the authors’ knowledge, this is the first study, with a prospective design, on the association between DAO and multimorbidity.
A first relevant epidemiological finding of our study is that approximately half of the population included at baseline had two or more medical conditions and were therefore excluded from our analyses. Considering that the mean age of the participants included in our study was approximately 63 years, we can consider that a consistent number of young-old people are already comorbid indicating a population that is in poorer health than expected [26]. Moreover, our study showed that during the follow-up period of 10 years, a large proportion of the population became multimorbid, reinforcing the importance of studies that can identify risk factors for this condition, such as DAO, which is potentially reversible. Several mechanisms can explain the association between DAO and incident multimorbidity. First, DAO is characterized by dynapenia and central adiposity, and both these conditions are associated with higher serum inflammatory markers [14, 27]. In this regard, cross-sectional studies have found a significant association between inflammatory markers and sarcopenia or dynapenia [28]. Some inflammatory cytokines, such as interleukin (IL)-6 or tumor necrosis factor (TNF)-α, seem to increase skeletal muscle breakdown, slow protein synthesis, and inhibit plasma concentrations of insulin-like growth factors that could impair muscle anabolic processes [29, 30]. Moreover, the presence of central adiposity could further impair the immune response [31], and adipose tissue is now considered an endocrine organ that can produce and secrete several inflammatory molecules [32]. Dysregulation of inflammatory responses can lead to the development of several physical medical conditions by affecting immunity, for example. [33]
Regarding DAO and individual chronic conditions, we found a positive and significant association between DAO with arthritis and diabetes, during ten years of follow-up. The association between DAO and higher risk of arthritis may be mainly explained by central adiposity. Indeed, in the present study central obesity alone was also associated with a higher risk of arthritis and obesity per se is a well-known risk factor for arthritis [34]. Moreover, the link between DAO and diabetes is also likely mainly driven by central obesity. It is known that abdominal obesity increases the risk of diabetes via changes in function of adipose tissue, specifically, increased release of free fatty acids and abnormalities in adipokine secretion resulting in insulin resistance [35]. Furthermore, abdominal obesity is associated with a higher insulin resistance level, a key marker of diabetes [36]. Our study showed that dynapenia at baseline was also associated with a higher risk of diabetes, confirming other findings indicating a significant association between sarcopenia and diabetes, independently from obesity, which could be explained by increases in insulin resistance level [37].
We believe that our epidemiological findings could have relevant clinical implications since they suggest that interventions to manage DAO could potentially prevent multimorbidity. In this regard, while pharmacological interventions are still not available, physical activity and nutrition interventions could be most appropriate [38]. For example, resistance training could be particularly important since this kind of intervention could decrease body fat mass and at the same time increase muscle strength, and muscle performance [39]. Of importance, our study indicated that low physical activity level is another independent risk factor for incident multimorbidity during the follow-up period. Similarly, nutritional interventions are of importance to reach an adequate weight loss and therefore improve inflammation and insulin resistance [40]. However, since hypocaloric diets may lead to a loss in muscle mass, the combination of physical activity in DAO is of importance.
The findings of our study must be interpreted in light of the study’s limitations. First, most of the study variables, including those regarding multimorbidity were self-reported and this could introduce recall bias, however, for several medical conditions in the ELSA study, a good agreement between self-reported and medical records have been observed [41]. However, other studies have reported that a large variability may exist with a low agreement between medical records and self-reported information. However, self-reported medical data may be sufficient for ruling out history of a particular condition [42]. Second, while our list of chronic conditions probably included most important conditions that occur in late life, it is possible for the results to have differed with a list of different chronic conditions. Third, the population was largely Caucasian, since the waist circumference cut-off is ethnic-specific, incident MM may differ in other populations. Therefore, studies from other ethnic groups are needed which may or may not reinforce the present findings. Finally, some relevant risk factors, such as the use of medications, owing to data not being available, were not included in the present analyses and could modify the association that we found in our study.
In conclusion, in the present study including a large representative sample of middle-aged and older UK adults, DAO was significantly associated with a higher risk of incident multimorbidity, compared to no dynapenia nor abdominal obesity, over ten years of follow-up. Interventions to prevent or manage DAO may also aid in the prevention of (multiple) chronic conditions that are typical of DAO such as arthritis and diabetes, usually associated with a poor quality of life. Future intervention studies are, however, needed before concrete recommendations can be made.
Data availability
The original contributions presented in the study are included in the article; further inquiries can be directed to the corresponding author.
References
Hunter DJ, Reddy KS (2013) Noncommunicable diseases. N Engl J Med 369:1336–1343
Habib SH, Saha S (2010) Burden of non-communicable disease: global overview. Diabetes Metab Syndr 4:41–47
Kernick D, Chew-Graham CA, O’Flynn N (2017) Clinical assessment and management of multimorbidity: NICE guideline. Br J Gen Pract 67:235–236
Fortin M, Lapointe L, Hudon C et al (2004) Multimorbidity and quality of life in primary care: a systematic review. Health Qual Life Outcomes 2:51
Lehnert T, Heider D, Leicht H et al (2011) Review: health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev 68:387–420
Grande G, Marengoni A, Vetrano DL et al (2021) Multimorbidity burden and dementia risk in older adults: the role of inflammation and genetics. Alzheimers Dement 17:768–776
Gallo JJ, Hwang S, Joo JH et al (2016) Multimorbidity, depression, and mortality in primary care: randomized clinical trial of an evidence-based depression care management program on mortality risk. J Gen Intern Med 31:380–386
de Oliveira MR, de Oliveira DC, Ramírez PC et al (2021) Dynapenia, abdominal obesity or both: which accelerates the gait speed decline most? Age Ageing 50:1616–1625
de Oliveira MR, Santos JLF, Perracini MR et al (2019) Abdominal obesity, dynapenia and dynapenic-abdominal obesity as factors associated with falls. Braz J Phys Ther 23:497–505
Veronese N, Koyanagi A, Soysal P et al (2023) Dynapenic abdominal obesity and susceptibility to fall a prospective analysis of the osteoarthritis initiative. Front Nutr. https://doi.org/10.3389/fnut.2023.1153399
Sénéchal M, Dionne IJ, Brochu M (2012) Dynapenic abdominal obesity and metabolic risk factors in adults 50 years of age and older. J Aging Health 24:812–826
Alexandre TdS, Scholes S, Santos JLF et al (2019) Dynapenic abdominal obesity as a risk factor for worse trajectories of ADL disability among older adults: the ELSA cohort study. J Gerontol: Series A 74:1112–1118
Rossi AP, Fantin F, Caliari C et al (2016) Dynapenic abdominal obesity as predictor of mortality and disability worsening in older adults: a 10-year prospective study. Clin Nutr 35:199–204
Bano G, Trevisan C, Carraro S et al (2017) Inflammation and sarcopenia: a systematic review and meta-analysis. Maturitas 96:10–15
Shen W, Punyanitya M, Chen J et al (2006) Waist circumference correlates with metabolic syndrome indicators better than percentage fat. Obesity 14:727–736
Steptoe A, Breeze E, Banks J et al (2013) Cohort profile: the English longitudinal study of ageing. Int J Epidemiol 42:1640–1648
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31
de Almeida MR, de Souza VF, do Rosario TC et al (2022) Agreement between maximum and mean handgrip strength measurements in cancer patients. PLoS ONE 17:e0270631
Veronese N, Koyanagi A, Barbagallo M et al (2023) Pain increases the risk for sarcopenia in community dwelling adults results from the English longitudinal study of ageing. J Gerontol: Series A. https://doi.org/10.1093/gerona/glad062
Spexoto MCB, Ramírez PC, de Oliveira MR et al (2022) European working group on sarcopenia in older people 2010 (EWGSOP1) and 2019 (EWGSOP2) criteria or slowness: which is the best predictor of mortality risk in older adults? Age Ageing 51:afac164
Grundy SM, Brewer HB Jr, Cleeman JI et al (2004) Definition of metabolic syndrome: report of the national heart, lung, and blood institute/American heart association conference on scientific issues related to definition. Circulation 109:433–438
van den Akker M, Buntinx F, Knottnerus JA (1996) Comorbidity or multimorbidity: what’s in a name? a review of literature. Eur J Gen Pract 2:65–70
Veronese N, Smith L, Cereda E et al (2021) Multimorbidity increases the risk for sarcopenia onset: longitudinal analyses from the English longitudinal study of ageing. Exp Gerontol 156:111624
Barbagallo M, Smith L, Koyanagi A et al (2023) Multimorbidity increased the risk of urinary incontinence in community-dwelling adults: results from the English longitudinal study on ageing. Maturitas. https://doi.org/10.1016/j.maturitas.2022.12.007
Ramírez PC, de Oliveira DC, de Oliveira MR et al (2023) Is dynapenic abdominal obesity a risk factor for cardiovascular mortality? A competing risk analysis. Age Ageing 52:afac301
Veronese N, Noale M, Sinclair A et al (2022) Risk of progression to diabetes and mortality in older people with prediabetes: the English longitudinal study on ageing. Age Ageing 51:afab222
Hermsdorff HHM, Zulet MÁ, Puchau B et al (2011) Central adiposity rather than total adiposity measurements are specifically involved in the inflammatory status from healthy young adults. Inflammation 34:161–170
Taaffe DR, Harris TB, Ferrucci L et al (2000) Cross-sectional and prospective relationships of interleukin-6 and C-reactive protein with physical performance in elderly persons: MacArthur studies of successful aging. J Gerontol A Biol Sci Med Sci 55:M709–M715
Charters Y, Grimble RF (1989) Effect of recombinant human tumour necrosis factor α on protein synthesis in liver, skeletal muscle and skin of rats. Biochem J 258:493–497
García-Martínez C, López-Soriano FJ, Argilés JM (1993) Acute treatment with tumour necrosis factor-α induces changes in protein metabolism in rat skeletal muscle. Mol Cell Biochem 125:11–18
De Heredia FP, Gómez-Martínez S, Marcos A (2012) Obesity, inflammation and the immune system. Proc Nutr Soc 71:332–338
Liu D, Li Q, Dong J et al (2019) The association between normal BMI with central adiposity and proinflammatory potential immunoglobulin GN-glycosylation. Diabetes, Metab Syndr Obes: Targ Ther. https://doi.org/10.2147/DMSO.S216318
Zhong J, Shi G (2019) Regulation of inflammation in chronic disease. Frontiers Media SA, p 737
Magliano M (2008) Obesity and arthritis. Menopause. International 14:149–154
Westphal SA (2008) Obesity, abdominal obesity, and insulin resistance. Clin Cornerstone 9:23–31
Kahn SE, Hull RL, Utzschneider KM (2006) Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 444:840–846
Veronese N, Pizzol D, Demurtas J et al (2019) Association between sarcopenia and diabetes: a systematic review and meta-analysis of observational studies. Eur Geriatr Med. https://doi.org/10.1007/s41999-019-00216-x
Yoshimura Y, Wakabayashi H, Yamada M et al (2017) Interventions for treating sarcopenia a systematic review and meta-analysis of randomized controlled studies. J Am Med Dir Associ 18:553–553
Chen N, He X, Feng Y et al (2021) Effects of resistance training in healthy older people with sarcopenia: a systematic review and meta-analysis of randomized controlled trials. Eur Rev Aging Phys Act 18:1–19
Tobias DK, Chen M, Manson JE et al (2015) Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 3:968–979
Kriegsman DM, Penninx BW, Van Eijk JTM et al (1996) Self-reports and general practitioner information on the presence of chronic diseases in community dwelling elderly: a study on the accuracy of patients’ self-reports and on determinants of inaccuracy. J Clin Epidemiol 49:1407–1417
Smith B, Chu LK, Smith TC et al (2008) Challenges of self-reported medical conditions and electronic medical records among members of a large military cohort. BMC Med Res Methodol 8:1–10
Acknowledgements
The ELSA was developed by a team of researchers based at University College London, the National Centre for Social Research and the Institute for Fiscal Studies. The data were collected by the National Centre for Social Research. The funding was provided by the National Institute of Aging in the USA, and a consortium of UK government departments coordinated by the Office for National Statistics. The developers and funders of the ELSA and the UK Data Archive do not bear any responsibility for the analyses or interpretations presented here. J. W. is supported by the Centre for the Development and Evaluation of Complex Interventions for Public Health Improvement, a UKCRC Public Health Research: Centre of Excellence. Funding from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council (ESRC RES-590-28-0005), Medical Research Council (MR/KO232331/1), the Welsh Assembly Government and the Wellcome Trust (WT087640MA), under the auspices of the UK Clinical Research Collaboration, and the contribution is gratefully acknowledged. M. K. is supported by the UK Medical Research Council (K013351), the Academy of Finland and the US National Institutes of Health (R01HL036310 and R01AG034454) and by a professorial fellowship from the Economic and Social Research Council. G. D. B. is a member of the University of Edinburgh Centre for Cognitive Ageing and Cognitive Epidemiology, part of the cross-council Lifelong Health and Wellbeing Initiative (G0700704/84698).
Funding
Open access funding provided by Università degli Studi di Palermo within the CRUI-CARE Agreement. None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Human and animal rights
The ELSA study was approved by the London Multicenter Research Ethics Committee (MREC/01/2/91).
Consent to participate
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Veronese, N., Koyanagi, A., Soysal, P. et al. Dynapenic abdominal obesity and incident multimorbidity: findings from the English longitudinal study on ageing. Aging Clin Exp Res 35, 1671–1678 (2023). https://doi.org/10.1007/s40520-023-02455-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02455-2