Abstract
Background
Incontinence and hip fractures are common in older people, especially women, and associated with multiple adverse effects. Incontinence is a risk factor for falls.
Aims
We aimed to investigate the prevalence of urinary (UI) and double incontinence (DI, concurrent UI and faecal incontinence), and to identify factors associated with UI and DI 6 months post-fracture.
Methods
A prospective real-life cohort study was conducted consisting of 910 women aged ≥ 65 who were treated for their first hip fracture in Seinäjoki Central Hospital, Finland, between May 2008 and April 2018. Continence status was elicited at baseline and 6 months postoperatively at our geriatric outpatient clinic where all participants underwent a multidisciplinary comprehensive geriatric assessment (CGA) consisting of an evaluation of cognition, nutrition, mood, mobility, and functional ability.
Results
At baseline, 47% of the patients were continent, 45% had UI and 8% had DI, and at follow up, 38%, 52%, and 11%, respectively. The mean age of the patients was 82.7 ± 6.8. Both UI and DI were associated with functional disability and other factors related to frailty. The associations were particularly prominent for patients with DI who also had the worst performance in the domains of CGA. We identified several modifiable risk factors: depressive mood (odds ratio [OR] 1.81; 95% confidence interval [CI] 1.16–2.84) and constipation (OR 1.48, 95% CI 1.02–2.13) associated with UI and, late removal of urinary catheter (OR 2.33, 95% CI 1.31–4.14), impaired mobility (OR 2.08, 95% CI 1.05–4.15), and poor nutrition (OR 2.31, 95% CI 1.11–4.79) associated with DI.
Conclusions
This study demonstrates a high prevalence of UI and DI in older women with hip fracture and modifiable risk factors, which should be targeted in orthogeriatric management and secondary falls prevention. Patients with DI were found to be an especially vulnerable group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary incontinence (UI), defined as any reported involuntary loss of urine [1], has long been recognized as a geriatric syndrome associated with adverse patient outcomes, such as functional decline, decreased quality of life, depression, institutionalization, and mortality. UI is more common in women than in men, and prevalence increases with advancing age. Nearly 40% of women older than 60 years and nearly 80% of women residing in long-term care have UI. Despite high prevalence, UI remains under-reported and poorly managed [2,3,4].
Double incontinence (DI) is defined as the concurrent UI and faecal incontinence (FI) [5]. DI, the most severe form of pelvic floor dysfunction, is associated with greater decline in quality of life than UI or FI in isolation. As with UI, DI is more common among women and associated with advancing age. Risk factors for DI include high comorbidity, frailty, depression, and limited mobility. The prevalence of DI in community-dwelling adults has ranged between 2.5 and 14.5% in prior studies. In a large cross-sectional study of over 64,000 community-dwelling older women, the prevalence of DI was 7% [6,7,8]. The prevalence of DI is higher and estimated around 33–65% in patients residing in long-term care and, it becomes more common with increasing time after admission. DI is associated with UI, functional and cognitive deficits, comorbidities, and advancing age in these patients [9, 10].
UI is known to be associated with falls in older adults, especially women, and both are associated with frailty. Frailty is a multidimensional syndrome defined as diminished physiologic reserve and function with increased vulnerability to minor stressors and risk for adverse health outcomes [11,12,13,14]. UI is twice as common among frail older adults as compared to the robust, and underlying causes of incontinence in this group are diverse and often related to factors outside the urinary tract; namely, functional and cognitive decline, comorbidity, and polypharmacy [15].
Research on the connection between DI and falls or frailty is scarce. In one study of older community-dwelling Brazilian women, falls experienced during the previous year were found to be a risk factor for incident DI [16]. Moreover, FI has been associated with falls [17] and mortality after a hip-fracture in older adults [18]. Therefore, our hypothesis is that DI is associated with poor outcomes after a hip fracture.
The aim of this study was to investigate the prevalence and factors associated with UI and DI among older women with hip fracture. Moreover, we sought to examine associated factors separately for UI and DI, since we assumed that the DI group represented the frailest of the study population.
Methods
Study population
The study population comprised 1675 consecutive women aged ≥ 65 years who were treated for their first hip fracture in Seinäjoki Central Hospital, Finland, between May 2008 and April 2018. Seinäjoki Central Hospital is the only hospital providing acute surgical care in the Hospital district of Southern Ostrobothnia, which has a population of approximately 200,000. The patients were discharged from the acute hospital into primary care hospitals for rehabilitation after a median length of stay of 5 days (interquartile range [IQR] of 2–8 days). The only exclusion criteria in this study were pathologic and periprosthetic fractures. All the patients regardless of cognitive state, morbidity or functional ability or living arrangements were invited to participate.
Data collection
The baseline data was collected during hospitalization by a trained geriatric nurse interviewing the patients or their representatives, and from patient medical records. In addition, follow-up data was collected at the outpatient clinic during the CGA visit in a median time of 6 months (IQR 4–6 months). The CGA was performed by a multidisciplinary team lead by a geriatrician or a trainee in geriatric medicine under her supervision. A geriatric nurse carried out the assessment of the domains with the selected tools. Both the patient and his or her next of kin or caregiver were invited. A physiotherapist’s examination preceded the geriatric assessment. Informed consent was obtained from all the patients or their representatives (legal guardian or next of kin). The study was approved by the Ethics Committee of the Hospital District of Southern Ostrobothnia.
Variables and definitions
During the initial perioperative interview, continence status before the fracture was elicited from the patients or their representatives. UI was defined as any reported involuntary loss of urine, and FI as any reported involuntary loss of faeces, respectively. Patients with both symptoms were deemed to have DI. Data on demographics, number of prescribed medications, diagnosis of cognitive disorder (yes or no), mobility, and living arrangements were collected. Independent mobility was defined as being able to ambulate independently without personal assistance. Living in an institution was defined as residing in a primary care hospital or a long-term care facility (LTCF) providing 24-h care.
The preoperative American Society of Anaesthesiologists (ASA) risk scores were used to assess general health at baseline. There are five classes: (1) healthy person, (2) mild systemic disease, (3) severe systemic disease, (4) severe systemic disease that is a constant threat of life, and (5) a moribund person who is not expected to survive without an operation [19]. Nutritional status was assessed using Mini Nutritional Assessment Short Form (MNA-SF) [20] both during hospitalization and at follow up. For the purposes of our study, poor nutrition was defined as being at risk for malnutrition or being malnourished according to the MNA-SF. Fracture type and the removal or non-removal of urine catheter (UC) before discharge from the acute hospital care were extracted from the medical records. Categorization of the baseline variables is shown in Table 1.
At the outpatient clinic, different domains of the CGA were assessed using standardized and well-known measures [21]. Cognitive function was measured with the Mini Mental State Examination (MMSE) [22], depressive mood with the 15-item Geriatric Depression Scale (GDS-15) [23], and Instrumental Activities of Daily Living (IADL) by Lawton and Brody [24]. Continence status, constipation, and new falls after the fracture were elicited during the interview. The physiotherapist’s assessment of the patient’s physical performance included the Timed up and go-test (TUG) assessing mobility, balance, and risk of falls [25], the Elderly Mobility Scale (EMS) which represents patient’s mobility and ability to perform basic ADL (activities of daily living) [26], and grip strength as a measure of muscle strength. Grip strength was measured in the stronger hand with a Jamar dynamometer and defined as weakened if less than 16 kg [27]. The categorization of the variables used at the outpatient clinic is shown in Table 2.
Statistical analysis
Distributions of the baseline characteristics between the patients who were continent and those who had UI or DI are shown in Table 1. Distributions of the outpatient domains between the respective groups are presented Table 2. Groupwise comparisons were performed using the Pearson’s Chi2 test or Fisher’s exact test.
Age- and multivariable-adjusted multinomial logistic regression analyses with odds ratios (OR) and 95% confidence intervals (CI) were conducted to examine the associations of both the baseline variables and outpatient domains with UI and DI at follow up using the continent group as a reference. IBM SPSS Statistics version 25.0 for Windows software (SPSS Inc. Chicago, Illinois) was used for statistical analyses. All tests were two-sided, and p values < 0.05 were considered statistically significant.
Results
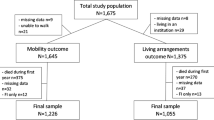
A total of 1675 participants were included in this study. The flow chart related to participant selection is shown in Fig. 1, whereas the participant characteristics are presented in Tables 1 and 2. The few patients (n = 31) with FI only were excluded from the final sample. The mean age of the patients was 82.7 ± 6.8. At baseline, 25% of the patients had a cognitive disorder, 22% lived in an institution, 33% had poor nutrition, and 37% could not ambulate independently.
Out of the 910 patients, 431 (47%) were continent, 406 (45%) had UI and 73 (8%) had DI at baseline, and at follow up, 343 (38%), 469 (52%) and 98 (11%), respectively. During the follow-up period, the continence status improved in 113 (12%) and deteriorated in 216 (24%) of the patients (Fig. 1).
In the age-adjusted univariate analyses, UI at follow up was associated with the following baseline variables: age over 80, ≥ 10 regular medications per day, diagnosis of cognitive disorder, non-independent mobility, living in an institution, poor nutrition, late removal of UC and previous UI or DI. In age-adjusted univariate analyses, DI at follow up was associated with the baseline variables including age between 80 and 89, ASA score higher than 2, ≥ 4 regular medications per day, diagnosis of cognitive disorder, non-independent mobility, poor nutrition, late removal of UC, and previous UI or DI (Table A1). Except for grip strength, all the domains of the CGA assessed at the outpatient clinic, observed constipation and new falls after fracture were significantly associated with both UI and DI at follow up in the age-adjusted univariate analyses (Table A2).
In the multivariable models of the baseline variables, UI at the follow-up visit was independently associated with age over 90, previous diagnosis of cognitive disorder and pre-fracture UI or DI while an independent association was observed between UI and difficulties in IADL, depressive mood, abnormal EMS, and self-reported constipation in the outpatient CGA. The respective results of the multivariable-adjusted analyses for associations with DI at follow up were non-independent mobility, living in an institution, late removal of UC and previous UI or DI at baseline, as well as difficulties in IADL, abnormal EMS, and poor nutrition observed in the outpatient CGA (Tables 3 and 4).
Discussion
UI and DI were common in this large cohort study of older women with hip fracture. Both UI and DI were associated with functional disability and other factors related to frailty. The associations were particularly prominent for patients with DI. Moreover, patients with DI performed more poorly in the domains of CGA at follow up as compared to the patients with UI or without either condition suggesting that patients with DI represent a frailer patient population than those with UI alone. We identified several potentially modifiable risk factors, namely depressive mood and constipation associated with UI and, late removal of UC, impaired mobility, and poor nutrition associated with DI.
Half of the surviving patients had UI while every tenth patient had DI at the end of follow up. Our results were in line with previous studies on hip fracture patients [28, 29]. However, DI was slightly more common in our study than in the previous studies on community-dwelling adults [6, 8] emphasizing the older and frailer population in our study.
At 6 months post-fracture, the continence status had deteriorated in every fourth patient. According to a previous study, hospital-acquired UI affects up to 21% of women suffering a hip fracture [30]. Advancing age, severe functional disability, and cognitive impairment have been shown to be major risk factors for developing UI and FI during hospitalization [31].
One of the main findings of our study is the association between incontinence and functional disability and reduced mobility. In the multivariable analyses, patients with difficulties in IADL in the outpatient CGA were almost twice more likely to report UI and six times more likely to report DI while patients with difficulties in basic ADL and mobility according to the EMS scores were twice as likely to report UI and five times more likely to report DI, respectively. Furthermore, the patients with non-independent mobility at baseline had a twofold risk for DI at follow up. Similar associations have been described in prior studies for UI and for DI in a long-term care setting [9, 10, 32].
As observed in our earlier study, nutritional status deteriorated in a significant proportion of the patients during the follow up [33]. In the multivariable model, poor nutrition observed at follow up was independently associated with DI. This is not surprising as a high rate of malnutrition associated with impaired mobility and muscle strength among older hip fracture patients has been observed before, suggesting a connection between protein-energy malnutrition and sarcopenia [33]. In the present study, no significant association between decreased grip strength and UI or DI was observed. Reduced statistical power due to a large proportion of missing data in this domain may have influenced the result. Our study utilized MNA-SF only in the evaluation of nutritional status, but it has also been introduced as a screening tool for frailty with a similar cutoff value [34]. Hence, the high prevalence of poor nutrition probably also reflects a high rate of frailty in our study population.
Advancing age and cognitive disorders are well known risk factors for both UI and DI [6, 10, 32, 35]. We observed an association with age over 90 and UI, as well as diagnosis of cognitive disorder and UI. However, similar associations with DI were not observed. The limited sample of individuals with DI might partly explain the lack of association with age and cognitive disorder in these patients.
In accordance with previous observations [9, 10], patients living in a LTCF were over 2.5 times more likely to report DI at follow up as compared to those who lived at home. Pre-facture incontinence was a strong risk factor for both UI and DI at follow up in our study. DI is frequently known to precede UI in isolation [9, 10].
Depressive mood was equally common in patients with UI and DI, with one in five being affected in both groups. Depressed patients were twice as likely to report UI at follow up. In the age-adjusted univariate analysis there was also an association with DI, but it ceased to be significant in the final model. Both UI [36] and DI [6, 8] have been shown to be associated with depression in older women. Depression is a risk factor for hip fractures [37], and patients recovering from a hip fracture are at high risk of developing depression [38]. Moreover, prevalence of depression has been found to be higher in incontinent fracture patients compared to the continent patients with a fracture [29]. Screening and management of depression is an important part of CGA in older women suffering a hip fracture, since its management can positively affect the rehabilitation process, and possibly the prognosis of concurrent incontinence; thus, improving overall quality of life.
Constipation was very common in our study cohort, affecting nearly half of those with UI and 40% of those with DI. Constipation was associated with a 1.5-fold risk of UI at follow up. Constipation is a common health condition among older people with a reported prevalence of up to 50% in community-dwelling and up to 70% in populations living in LTCFs. Underlying causes are often multifactorial and related to reduced mobility, decreased liquid intake and nutrition, as well as comorbidities and polypharmacy [39]. Constipation is a known risk factor for both UI and FI [9, 39, 40]. This highlights the importance of early mobilization and sufficient nutrition and hydration of the hip fracture patients. If constipation nonetheless develops, it should be managed effectively.
The relationship with UI and falls is multidimensional, and both are indicators of frailty [11,12,13,14]. Women experience falls more often than men [41]. The risk of falls has been observed to correlate with the severity of UI [17], and DI has been associated with falls as well [16]. In our study, there was a connection with new falls after fracture in age-adjusted analysis for both UI and DI, but the association ceased to be significant in the multivariable-adjusted analyses, although the result was not far from being statistically significant for DI. The association of DI and falls warrants further studies with larger study populations.
Late removal of UC was independently associated with DI at follow up in the multivariable model and the association was nearly statistically significant for UI. The use of UCs in hospitalized older patients is widespread and often inappropriate. The use of UC increases the risk of iatrogenic urinary tract infection, which can lead to more serious complications, including bacteraemia, delirium, and death [28, 42,43,44]. Older women and surgical patients are at a highest risk of inappropriate UC use and thus, for adverse outcomes [42]. Prolonged use of UC or diapers during hospitalization have been shown to predict incident UI [43], and worse recovery after a hip fracture [45]. Conversely, prompt removal of UC has been shown to decrease the risk of mortality [46] and protect from decline in mobility and the need for more supported living arrangements [47] after a hip fracture.
International guidelines recommend avoiding routine UC use with surgical patients and removing the UC within 24 h postoperatively to minimize adverse effects [44]. Notably, the frailest patients with the highest risk of adverse outcomes had the highest prevalence of prolonged UC use in our study. Prompt removal of a UC postoperatively is vital in preventing complications and promoting recovery among frail hip fracture patients.
Overall, all the associations mentioned above denote underlying frailty and suggest that individuals with DI were frailer than those with UI. The connection between frailty and UI is well known [15, 48]. Associations between UI and functional disability, impaired mobility, malnutrition and cognitive impairments have also been previously demonstrated in a study of older fragility fracture patients [29]. However, there is a paucity of literature regarding DI and frailty, especially among community-dwelling adults. Our study confirms the strong association of DI with frailty in older women with hip fracture.
Importantly, frailty is believed to be at least a partially reversible condition [48]. Since hip fracture patients are generally very frail and at risk of developing incontinence, and on the other hand patients with incontinence are more prone to falls [49], a multidisciplinary treatment approach with the aim of improving patient’s mobility and nutrition might improve overall prognosis of these patients.
To our knowledge, this is the first real-world study to investigate the prevalence and associated factors of both UI and DI in a cohort of older women with hip fracture. Furthermore, our study was large and prospective in design. The outpatient CGA included well-known and standardized instruments. In addition, cognitive disorder or living in a LTCF were not among the exclusion criteria, which is an important factor in the generalizability of our findings in this patient group.
There are several limitations which should be considered when interpreting our results. Firstly, the incontinence symptoms were assessed using simple questions rather than more detailed questionnaires, or other diagnostic tools. Secondly, most of the domains of the CGA were examined only in the follow up. Thirdly, the exact duration of UC use was not known. Finally, the follow-up data was only available for 54% of the original study population. The patients who had died before follow up or could not attend the outpatient clinic were most likely the frailest and in the poorest health, which introduces the possibility of a selection bias where the prevalence of UI and especially DI is underestimated.
Conclusions and implications
We demonstrated a high prevalence of UI and DI in older women with hip fracture in this large real-world prospective study. Both UI and DI were associated with multiple functional impairments and modifiable risk factors such as constipation, depressive mood, poor nutrition, and prolonged UC use, all of which should be targeted in orthogeriatric management and secondary falls prevention. Increased clinical awareness of incontinence and its consequences and complications in older frail hip fracture patients is paramount.
References
Ancona CD, Hamid R, Schizas A et al (2019) The International Continence Society ( ICS ) report on the terminology for adult male lower urinary tract and pelvic floor symptoms and dysfunction. Neurourol Urodyn 38:433–477. https://doi.org/10.1002/nau.23897
Lukacz ES, Santiago-Lastra Y, Albo ME et al (2017) Urinary incontinence in women a review. JAMA 318:1592–1604. https://doi.org/10.1001/jama.2017.12137
Gibson W, Wagg A (2014) New horizons: urinary incontinence in older people. Age Ageing 43:157–163. https://doi.org/10.1093/ageing/aft214
John G, Bardini C, Combescure C et al (2016) Urinary incontinence as a predictor of death: a systematic review and meta-analysis. PLoS ONE 11:e0158992. https://doi.org/10.1371/journal.pone.0158992
Sultan AH, Monga A, Lee J et al (2017) An International Urogynecological Association ( IUGA )/ International Continence Society ( ICS ) Joint Report on the Terminology for Female Anorectal Dysfunction. Neurourol Urodyn 36:10–34. https://doi.org/10.1002/nau.23055
Wu JM, Matthews CA, Vaughan CP et al (2015) Urinary, fecal, and dual incontinence in older U.S. adults. J Am Geriatr Soc 63:947–953. https://doi.org/10.1111/jgs.13385
Matthews CA (2014) Risk factors for urinary, fecal, or double incontinence in women. Curr Opin Obstet Gynecol 26:393–397. https://doi.org/10.1097/GCO.0000000000000094
Matthews CA, Whitehead WE, Townsend MK et al (2013) Risk factors for urinary, fecal, or dual incontinence in the nurses’ health study. Obstet Gynecol 122:539–545. https://doi.org/10.1097/AOG.0b013e31829efbff
Musa MK, Saga S, Blekken LE et al (2019) The prevalence, incidence, and correlates of fecal incontinence among older people residing in care homes: a systematic review. J Am Med Dir Assoc 20:956-962.e8. https://doi.org/10.1016/j.jamda.2019.03.033
Bliss DZ, Gurvich OV, Eberly LE et al (2018) Time to and predictors of dual incontinence in older nursing home admissions. Neurourol Urodyn 37:229–236. https://doi.org/10.1002/nau
Moon S, Chung HS, Yu JM et al (2020) Impact of urinary incontinence on falls in the older population: 2017 national survey of older Koreans. Arch Gerontol Geriatr 90:104158. https://doi.org/10.1016/j.archger.2020.10415
Chiarelli PE, Mackenzie LA, Osmotherly PG (2009) Urinary incontinence is associated with an increase in falls: a systematic review. Aust J Physiother 55:89–95. https://doi.org/10.1016/S0004-9514(09)70038-8
Chong E, Chan M, Lim WS et al (2018) Frailty predicts incident urinary incontinence among hospitalized older adults—a 1-Year Prospective Cohort Study. J Am Med Dir Assoc 19:422–427. https://doi.org/10.1016/j.jamda.2017.12.103
Fried LP, Tangen CM, Walston J et al (2001) Frailty in older adults: evidence for a phenotype. J Gerontol Ser A Biol Sci Med Sci 56:146–157. https://doi.org/10.1093/gerona/56.3.m146
Veronese N, Soysal P, Stubbs B et al (2018) Association between urinary incontinence and frailty: a systematic review and meta-analysis. Eur Geriatr Med 9:571–578. https://doi.org/10.1007/s41999-018-0102-y
Yuaso DR, Santos JLF, Castro RA et al (2018) Female double incontinence: prevalence, incidence, and risk factors from the SABE (Health, Wellbeing and Aging) study. Int Urogynecol J 29:265–272. https://doi.org/10.1007/s00192-017-3365-9
Schluter PJ, Askew DA, Jamieson HA et al (2020) Urinary and fecal incontinence are independently associated with falls risk among older women and men with complex needs: a National Population Study. Neurourol Urodyn 39:945–953. https://doi.org/10.1002/nau.24266
Guzon-Illescas O, Perez Fernandez E, Crespí Villarias N et al (2019) Mortality after osteoporotic hip fracture: Incidence, trends, and associated factors. J Orthop Surg Res 14:203. https://doi.org/10.1186/s13018-019-1226-6
Sankar A, Johnson SR, Beattie WS et al (2014) Reliability of the American Society of Anesthesiologists physical status scale in clinical practice. Br J Anaesth 113:424–432. https://doi.org/10.1093/bja/aeu100
Rubenstein LZ, Harker JO, Salvà A et al (2001) Screening for undernutrition in geriatric practice: Developing the Short-Form Mini-Nutritional Assessment (MNA-SF). Journals Gerontol Ser A Biol Sci Med Sci 56:366–372. https://doi.org/10.1093/gerona/56.6.M366
Nuotio M, Luukkaala T (2016) Factors associated with changes in mobility and living arrangements in a comprehensive geriatric outpatient assessment after hip fracture. Disabil Rehabil 38:1125–1133. https://doi.org/10.3109/09638288.2015.1074728
Folstein MF, Folstein SE, Mchugh PR (1975) Mini-mental State. A practical method for grading the cognitive state of patients of the clinician. J Psychiatr Res 12:189–198. https://doi.org/10.1016/0022-3956(75)90026-6
Brown LM, Schinka JA (2005) Development of initial validation of a 15-item informant version of the Geriatric Depression Scale. Int J Geriatr Psychiatry 20:911–918. https://doi.org/10.1002/gps.1375
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186
Viccaro LJ, Perera S, Studenski SA (2011) Is timed up and go better than gait speed in predicting health, function, and falls in older adults? J Am Geriatr Soc 59:887–892. https://doi.org/10.1111/j.1532-5415.2011.03336.x
Smith R (1994) Validation and reliability of the elderly mobility scale. Physiotherapy 80:744–747. https://doi.org/10.1016/S0031-9406(10)60612-8
Alley DE, Shardell MD, Peters KW et al (2014) Grip strength cutpoints for the identification of clinically relevant weakness. J Gerontol Ser A Biol Sci Med Sci 69:559–566. https://doi.org/10.1093/gerona/glu011
Sørbye LW, Grue EV (2013) Hip fracture and urinary incontinence—use of indwelling catheter postsurgery. Scand J Caring Sci 27:632–642. https://doi.org/10.1111/j.14716712.2012.01075.x
Gosch M, Talasz H, Nicholas JA et al (2015) Urinary incontinence and poor functional status in fragility fracture patients: an underrecognized and underappreciated association. Arch Orthop Trauma Surg 135:59–67. https://doi.org/10.1007/s00402-014-2113-6
Palmer MH, Baumgarten M, Langenberg P et al (2002) Risk factors for hospital-acquired incontinence in elderly female hip fracture patients. Journals Gerontol Ser A Biol Sci Med Sci 57:M672–M677. https://doi.org/10.1093/gerona/57.10.M672
Mecocci P, Von Strauss E, Cherubini A et al (2005) Cognitive impairment is the major risk factor for development of geriatric syndromes during hospitalization: results from the GIFA study. Dement Geriatr Cogn Disord 20:262–269. https://doi.org/10.1159/000087440
Gibson W, Ii TJ, Markland A et al (2021) Incontinence in frail elderly persons: report of the 6th International Consultation on Incontinence. Neurourol Urodyn 40:38–54. https://doi.org/10.1002/nau.24549
Helminen H, Luukkaala T, Saarnio J et al (2017) ScienceDirect Changes in nutritional status and associated factors in a geriatric post-hip fracture assessment. Eur Geriatr Med 8:134–139. https://doi.org/10.1016/j.eurger.2017.02.002
Soysal P, Veronese N, Arik F et al (2019) Mini nutritional assessment scale-short form can be useful for frailty screening in older adults. Clin Interv Aging 14:693–699. https://doi.org/10.2147/CIA.S196770
Stenzelius K, Mattiasson A, Hallberg IR et al (2004) Symptoms of urinary and faecal incontinence among men and women 75+ in relations to health complaints and quality of life. Neurourol Urodyn 23:211–222. https://doi.org/10.1002/nau.20030
Lim YM, Lee SR, Choi EJ et al (2018) Urinary incontinence is strongly associated with depression in middle-aged and older Korean women: data from the Korean longitudinal study of ageing. Eur J Obstet Gynecol Reprod Biol 220:69–73. https://doi.org/10.1016/j.ejogrb.2017.11.017
Shi TT, Min M, Zhang Y et al (2019) Depression and risk of hip fracture: a systematic review and meta-analysis of cohort studies. Osteoporos Int 30:1157–1165. https://doi.org/10.1007/s00198-019-04951-6
Lenze EJ, Munin ÃMC, Skidmore ER et al (2007) Onset of depression in elderly persons after hip fracture: implications for prevention and early intervention of late-life depression. J Am Geriatr Soc 55:81–86. https://doi.org/10.1111/j.1532-5415.2006.01017.x
De Giorgio R, Ruggeri E, Stanghellini V et al (2015) Chronic constipation in the elderly: a primer for the gastroenterologist. BMC Gastroenterol 15:130. https://doi.org/10.1186/s12876-015-0366-3
Lian W, Li F, Huang H et al (2019) Constipation and risk of urinary incontinence in women: a meta-analysis. Int Urogynecol J 30:1629–1634. https://doi.org/10.1007/s00192-019-03941-w
Gale CR, Cooper C, Sayer AA (2016) Prevalence and risk factors for falls in older men and women: the English longitudinal study of ageing. Age Ageing 45:789–794. https://doi.org/10.1093/ageing/afw129
Hu F, Yang D, Huang C et al (2015) Inappropriate use of urinary catheters among hospitalized elderly patients: clinician awareness is key. Geriatr Gerontol Int 15:1235–1241. https://doi.org/10.1111/ggi.12431
Zisberg A, Gary S, Gur-yaish N et al (2011) In-hospital use of continence aids and New-Onset urinary incontinence in adults aged 70 and older. J Am Geriatr Soc 59:1099–1104. https://doi.org/10.1111/j.1532-5415.2011.03413.x
Gould CV, Umscheid CA, Agarwal RK et al (2010) Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol 31:319–326. https://doi.org/10.1086/651091
Morri M, Chiari P, Forni C et al (2018) What factors are associated with the recovery of autonomy after a hip fracture? A Prospective, Multicentric Cohort Study. Arch Phys Med Rehabil 99:893–899. https://doi.org/10.1016/j.apmr.2018.01.021
Pajulammi HM, Luukkaala TH, Pihlajamäki HK et al (2016) Decreased glomerular filtration rate estimated by 2009 CKD-EPI equation predicts mortality in older hip fracture population. Injury 47:1536–1542. https://doi.org/10.1016/j.injury.2016.04.028
Pajulammi HM, Pihlajamäki HK, Luukkaala TH et al (2015) Pre- and perioperative predictors of changes in mobility and living arrangements after hip fracture—a population-based study. Arch Gerontol Geriatr 61:182–189. https://doi.org/10.1016/j.archger.2015.05.007
Suskind AM (2017) Frailty and lower urinary tract symptoms. Curr Urol Rep 18:67. https://doi.org/10.1007/s11934-017-0720-9
Gibson W, Hunter KF, Camicioli R et al (2018) The association between lower urinary tract symptoms and falls: forming a theoretical model for a research agenda. Neurourol Urodyn 37:501–509. https://doi.org/10.1002/nau.23295
Acknowledgements
Ms Kaisu Haanpää, RN, is gratefully acknowledged for her expert collecting and saving of the data.
Funding
Open Access funding provided by University of Turku (UTU) including Turku University Central Hospital. This work was supported by Research Fund of the Hospital District of Southern Ostrobothnia (VTR111) and the State Research Financing of Seinäjoki Central Hospital (VTR233).
Author information
Authors and Affiliations
Contributions
Study concept and design: AHB, MN, SAN, TL. Acquisition of data: MN, MK. Analysis and interpretation of data: AHB, TL, MN, SAN. Drafting of the manuscript: AHB, MN. Critical revision of the manuscript for important intellectual content: AHB, MN, SAN, TL, MK.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
The study design was approved by the Ethics Committee of the Hospital District of Southern Ostrobothnia. The study complies with the ethical standards of the Declaration of Helsinki and its later amendments.
Statement on human rights
All procedures performed in our study were in accordance with the ethical standards of the Ethics Committee of the Hospital District of Southern Ostrobothnia and with the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all the participants or their representatives.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hellman-Bronstein, A.T., Luukkaala, T.H., Ala-Nissilä, S.S. et al. Factors associated with urinary and double incontinence in a geriatric post-hip fracture assessment in older women. Aging Clin Exp Res 34, 1407–1418 (2022). https://doi.org/10.1007/s40520-021-02046-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-021-02046-z