Abstract
Objectives
This systematic review aimed to compare the weight change in people with or without binge eating who underwent various weight loss treatments.
Methods
We searched for studies in PubMed, American Psychological Association, and Embase from inception to January 2022. The studies selected included assessment of binge eating and body weight before and after weight loss treatment in people of any age. The meta-analyses were conducted using Comprehensive Meta-Analysis (CMA). We used Egger’s regression test, the funnel plot, and the Trim and Fill test to assess the risk of publication bias.
Results
Thirty-four studies were included in the systematic review, with a total of 10.184 participants. The included studies were divided into three categories according to types of weight loss treatments, namely, (1) bariatric surgery; (2) pharmacotherapy isolated or combined with behavioral interventions; and (3) behavioral and/or nutritional interventions. The meta-analyses showed no significant difference in weight loss between people with or without binge eating engaged in weight loss treatments, with an overall effect size of − 0.117 (95% CI − 0.405 to 0.171; P = 0.426).
Conclusions
Our findings showed no difference in weight loss in people with or without pre-treatment binge eating who received various weight loss treatments. Weight loss treatments should not be withheld on the basis that they will not be effective in people with pre-treatment binge eating, albeit their safety and longer term impacts are unclear.
Level of evidence: Level I, at least one properly designed randomized controlled trials; systematic reviews and meta-analyses; experimental studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a global public health concern [1]. People with obesity are at an elevated risk of weight-related health complications, such as diabetes, cardiovascular diseases, hypertension, metabolic syndrome, and fatty liver [2, 3]. In addition, some people with obesity also experience recurrent binge eating episodes [3]. Binge eating is defined as the ingestion of an excessive amount of food in a given period, typically within 2 h while feeling a sense loss of control over food intake during the episode [4]. Previous studies showed that a significant proportion of people with obesity experience binge eating episodes [5,6,7]. For instance, in Latin America, 16–52% of people with obesity seeking weight loss treatments had recurrent binge eating episodes [8]. In Spain, 87% of people with binge eating disorder (BED) had obesity [9], and in Finland, 56% of women with BED had overweight or obesity [10]. Moreover, the prevalence of people with obesity and comorbid binge eating has increased 7.3-fold in South Australia from 1995 to 2015 [11].
The relationship between obesity and binge eating is complex as binge eating can be a cause and a consequence of obesity [12]. Nonetheless, people with obesity and comorbid binge eating generally seek weight loss treatments rather than therapies for eating disorders [13, 14]. For instance, a systematic review found that 30–73% of people with obesity and comorbid eating disorders sought weight loss treatments [13], and another study showed that 59% of people with BED seek treatments for problems with weight [14]. In addition, a study that investigated the prevalence of BED, bulimia nervosa (BN) and recurrent binge eating in a middle-income country found that only 42.4% of people with BED sought treatment [15]. From those, 35.3% contacted a dietitian and only 25.9% sought a mental health professional (i.e., psychologist or a psychiatrist) [15]. Furthermore, previous studies found that there is a low probability that people with obesity and comorbid eating disorders receive specialized therapies for their eating disorder [16, 17]. This means that people with obesity and comorbid recurrent binge eating are mostly accessing to weight loss treatments rather than eating disorder treatments. This can be problematic, because (1) people with obesity and comorbid binge eating are thereby not accessing therapies to address their eating disorder behaviors; and (2) recurrent binge eating may potentially hinder weight loss outcomes in obesity treatments.
Previous studies showed contrasting findings regarding whether binge eating can hinder weight loss in people with obesity [18,19,20,21,22,23,24,25]. Some studies found that binge eating hinders weight loss outcomes in people with obesity [18, 19], while other studies showed that people with or without binge eating can lose weight similarly when they receive a variety of weight loss treatments [18,19,20,21,22,23]. Studies with meta-analyses also found contrasting results regarding weight loss outcomes in people with or without binge eating. A matched-study meta-analysis showed that post-treatment weight loss was poorer in people with BED compared to those without BED (1.3 kg versus 10.5 kg, respectively) [26]. Nonetheless, this matched-study meta-analysis did not investigate all the available literature in the field as it evaluated the moderating influence of binge eating on weight loss treatments that were matched to control key background variables [26]. For instance, in that matched-study meta-analysis, studies that investigated the effects of weight loss treatments in people with BED—but did not include a sample of people without BED—were matched with a sample of people without BED from another similar study [26]. In contrast, a systematic review with meta-analysis showed that pre-surgery binge eating had minimal or no effect on weight loss outcomes after bariatric surgery [21]. However, that systematic review with meta-analysis included only studies that examined weight loss in people with or without binge eating who underwent bariatric surgery, and excluded studies with other types of weight loss treatments [21].
Overall, it is not clear whether binge eating hinders weight loss outcomes in people with overweight or obesity who received weight loss treatments that are routinely implemented in clinics and hospitals. Thus, it is important to further investigate whether binge eating is associated with poor weight loss outcomes. This investigation is needed, because—if people with overweight or obesity and comorbid binge eating have poorer weight loss outcomes compared to those without binge eating—they may potentially benefit from therapies to reduce their eating disorder psychopathology and associated binge eating prior to initiating weight loss treatments. However, if weight loss is similar in people with or without binge eating, those with obesity and comorbid binge eating can potentially benefit from treatments that address weight management and eating disorder behaviors simultaneously [27]. This systematic review aims to compare changes in body weight in people with or without pre-treatment binge eating who received varied types of weight loss treatments.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement, updated in 2020, provided the framework for this review [28].
Information sources
In our systematic review we searched for eligible studies in three databases, namely, PubMed, American Psychological Association (APA), and Embase.
Search strategy
Our systematic review with meta-analyses were conducted using the following population, intervention, control, and outcome (PICO) [29] framework. The population included people with overweight or obesity and pre-treatment binge eating. The intervention comprised various weight loss treatments. The control group consisted of people with overweight or obesity but without pre-treatment binge eating. The outcome of this study was the change in body weight after a weight loss treatment.
The search terms used in each database were described below. The following search terms were used in the PubMed database: (binge eating OR binge eating disorder* OR BED) AND (weight loss* OR weight reduction*) AND (obes* OR overweight OR BMI OR body mass index), with filters for “clinical study”, “clinical trial”, “controlled clinical trial”, “randomized clinical trial”. The following search terms were used in the APA database: (binge eating OR binge eating disorder) AND (“obesity” OR overweight) AND (weight loss OR weigh reduction). The following search terms were used in the Embase database: (binge eating disorder OR binge eating) AND (obesity OR overweight) AND (body weight loss) with the filters “controlled clinical trial” and “randomized clinical trial”. An initial search was conducted in March 17th 2020 and a second search was conducted in January 21st 2022 to update our results.
Selection process
The publications were inserted in EndNote, where duplicates were removed. Next, the studies were included in the software Rayyan, where the authors (IL, FQdL, TG) independently screened them according to eligibility criteria, initially by reading the titles and abstracts, and next by reading the full texts. Additional studies were included by active search of the reference lists of studies that met eligibility criteria.
Eligibility criteria
We included studies that (1) assessed binge eating prior to weight loss treatments; (2) assessed body weight at pre- and post-treatment in people with overweight or obesity that were enrolled in a weight loss treatment; and (3) reported assessments of body weight in 2 or more groups of people with different levels of binge eating (e.g., subthreshold binge eating, moderate binge eating, severe binge eating, BED). Our primary outcome measure was change in body weight from baseline to the last assessment of each study. We did not include any restrictions on treatment settings/characteristics, language, date of publication, and participants’ age or sex.
We excluded studies with the following characteristics: (1) studies with animals; (2) studies that examined correlations between binge eating and weight loss but did not compare weight change in people with or without binge eating; (3) studies that included only people with recurrent binge eating or only people without binge eating; and (4) studies that did not assess pre- and post-treatment body weight in groups of people with different levels of binge eating.
Data collection process
We extracted the following data from eligible studies: (1) characteristics of weight loss treatments; (2) sample characteristics (e.g., levels of binge eating prior to treatment, age, sex); (3) measures used to assess binge eating; and (4) body weight at baseline, end of treatment, and follow-up assessments. Data from the eligible studies were extracted by IL and checked for accuracy by FQdL.
Data processing and meta-analyses
To conduct the meta-analyses, we compared body weight change and standard deviations (SD) of the change in weight from baseline to the end of treatment or last follow-up assessment in groups of people with or without pre-treatment binge eating and with overweight or obesity. Seven studies identified in our systematic review were eligible for a meta-analysis but did not report changes in body weight and SD of the change in weight from baseline assessment to the end of treatment or last follow-up assessment. For these studies, we employed an imputation method delineated in the Cochrane Handbook [30] to determine the SD of change in weight from baseline to the end of treatment or last follow-up assessment. The following procedure was used to include the 7 abovementioned studies in a meta-analysis:
We used data from the studies that reported change in body weight and SD of the change in weight from the baseline assessment to the end of treatment or last follow-up assessment to calculate the mean correlation. We used the formulas below to calculate the mean correlation (first formula) and SD of change in weight (second formula):
Corr is the correlation coefficient; SDbaseline is the standard deviation of ‘baseline’ means; SDfinal is the standard deviation of “final” mean; SDchange is the standard deviation of the change between timepoints.
To minimize risk of bias, we employed the following three methods. First, some studies compared treatment effects in groups with varying levels of binge eating, such as no binge eating; moderate binge eating; and severe binge eating. To address this, we analyzed only the most extreme comparisons (i.e., no binge eating versus severe binge eating, rather than moderate binge eating versus severe binge eating). Second, the studies had different follow-up periods, so we analyzed the last assessment reported in each study. In addition, we performed two sub-group analyses based on the period of the last follow-up assessment: (a) short term (last follow-up assessment conducted less than 12 months/52.14 weeks after treatment commencement) and (b) long term (last assessment conducted at 12 months/52.14 weeks or more after treatment commencement). Third, when studies used multiple types of weight loss treatment, such as cognitive behavior therapy and behavior weight loss therapy, we analyzed each treatment independently in our meta-analyses.
We excluded from the meta-analyses studies that did not provide data that enabled the calculation of the SD of the change in body weight from pre-treatment to the end of treatment or last follow-up assessment. Studies with the following characteristics were excluded: (1) studies that did not report sample sizes in the pre-treatment phase and at the end of treatment or last follow-up assessment and (2) studies that did not report SD or standard error (SE) or did not specify whether data were reported in SD or SE. To facilitate the analyses, we converted the measurement of time to a common unit (i.e., weeks). In addition, we converted SE into SD from all the data reported in the studies. Body weight data that was reported in lb was converted to kg. However, some studies reported body weight outcomes in other units (e.g., BMI or % weight change) that could not be converted.
Study risk of bias assessment
The quality of the studies was assessed by two authors (IS and FQdL) using criteria adapted from a checklist for the assessment of the methodological quality of randomized and non-randomized studies of health care interventions [31]. Publications were assessed on the clarity of information provided about the hypothesis or aim, outcomes, participants characteristics, main findings, attrition rates, method of randomization, allocation concealment, validity and reliability of outcome measures, blinding of participants and assessors, sample power calculation and selective outcome bias (i.e., whether or not researchers appeared to selectively report their findings). Attrition < 30% was considered acceptable. Bias was defined as the practice of reporting completers only for interventions, where attrition was > 30%. Each publication included in this systematic review was classified under each of these criteria as ‘yes’, ‘no’, ‘unclear’ or ‘not applicable’ (e.g., measures that were applicable only to randomized controlled trials), as shown in Table 2.
Synthesis methods and certainty assessments
The meta-analyses were conducted using Comprehensive Meta-Analysis (CMA) version 3.3.070. We calculated the mean effect size and the true effect size in 95% confidence intervals. We used CMA add-on (i.e., CMA Prediction Intervals) to calculate prediction intervals. We assumed that the studies included in the meta-analyses were heterogeneous (e.g., due to differences in participants characteristics and types of weight loss treatment) and used Q statistic (variance of the observed effect sizes), and I2 and Tau statistics to assess heterogeneity among studies in each meta-analysis. We conducted sensitivity analyses by removing one study at a time from each meta-analysis to investigate whether the results would change from the overall result.
Reporting bias assessment
We used the Egger’s regression test, the funnel plot and Trim and Fill test to assess the risk of publication bias. A cumulative analysis was also conducted to assess small study effects among the studies included in each meta-analysis.
Results
Study selection
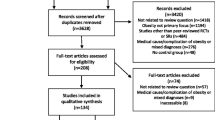
As shown in Fig. 1, we found 2883 publications with our search strategy. Five hundred fifty-two of these publications were duplicated, 2145 were excluded after screening titles and abstracts, and 55 were read in full. From those, 19 were included and 15 additional publications were added from reference lists of the eligible studies. In total, 34 studies were included. These studies included a total of 10.184 participants and were published from 1990 to 2021.
Flow chart of the systematic review search. We excluded from the meta-analyses studies that (1) did not report sample sizes in the pre-treatment phase and at the last assessment; (2) did not report SD or standard error (SE) or did not specify whether data were reported in SD or SE; and (3) studies that did not provide data that enabled the calculation of the SD of the change in body weight from pre-treatment to the end of treatment or last follow-up assessment
Study characteristics
Study characteristics are described in Table 1. The samples size of the studies ranged from 38 to 4901 participants. Twenty-seven studies included male and female participants, and 7 studies included only female participants. Most studies (32 out of 34) included adults, 1 study included only adolescents, and 1 study included only children. The period of post-treatment assessments ranged from 10 weeks (i.e., end of treatment) to 313 weeks (i.e., extended follow-up assessment). Fourteen of the studies had a short-term follow-up period (i.e., < 12 months) and 20 studies had a long-term follow-up period (i.e., ≥ 12 months) (see Table 1).
The included studies were divided into 3 categories according to types of weight loss treatments: (1) bariatric surgery; (2) pharmacotherapy isolated or combined with behavioral interventions; and (3) behavioral and/or nutritional interventions. We found 12 studies with bariatric surgery [32,33,34,35,36,37,38,39,40,41,42,43], 7 studies with pharmacotherapy isolated or combined with behavioral interventions [44,45,46,47,48,49,50], and 15 studies with behavioral and/or nutritional interventions [51,52,53,54,55,56,57,58,59,60,61,62,63,64,65] (Table 2).
Results of syntheses
Seventeen out of the 34 included studies reported data that was suitable for a meta-analysis, and we conducted 6 meta-analyses in total. The remaining 17 studies did not report data in a format that was suitable for a meta-analysis and were assessed qualitatively.
Overall weight change in people with or without binge eating who received any type of weight loss treatments
One of our meta-analyses compared weight change in people with or without binge eating who received any type of weight loss treatment. This meta-analysis included the outcome of 21 weight loss treatments, that were reported in 17 studies, with a total of 3017 participants. This meta-analysis showed no significant difference in weight loss between people with or without binge eating, with an overall effect size (standardized mean difference, SMD) of − 0.117 (95% confident interval [CI] 0–0.405 to 0.171; P = 0.426), which is considered small by Cohen’s [66] definition. The studies in this meta-analysis showed heterogeneity. Heterogeneity was calculated by Tau2 (variance of true effect size) with a value of 0.345, and Tau (standard deviation of the true effect sizes) was 0.588 which is considered high, and I2 of 82.6. The prediction interval (PI) was − 1.38 to 1.15 (Fig. 2), which means that in 95% of all populations the true effect size would fall in this range.
Our subgroup analysis showed no statistically significant differences in body weight between people with or without binge eating at short (< 12 months) versus long (≥ 12 months) follow-up assessments following any type of weight loss treatment, with an overall effect size of − 0.118 (CI of − 0.419 to 0.184; P = 0.44). However, we found significant heterogeneity (see Table 3).
Assessment of weight change in people with or without binge eating in specific types of weight loss treatments
We also examined changes in body weight in people with or without binge eating in three sub-group analysis in our meta-analyses categorized by the type of weight loss treatment (i.e., bariatric surgery; pharmacotherapy isolated or combined with behavioral interventions; behavioral and/or nutritional interventions) (Fig. 3). We assumed a common among-study variance component across subgroups (pool within-group estimates of tau-squared) and combined the subgroups using random effects to yield an overall effect. The results of our meta-analyses showed that people without binge eating prior to bariatric surgery lost significantly more body weight compared to those with binge eating prior to bariatric surgery (SMD = − 0.538; CI = − 1.066 to − 0.010; P = 0.046). However, significant heterogeneity was observed between the studies (P value = 0.000), with a prediction interval (PI) from − 1.87 to 0.79. This precludes us from making a definitive conclusion regarding the superiority of bariatric surgery induced greater weight loss in people without binge eating compared to those with pre-treatment binge eating. When investigating the effect of pharmacotherapy isolated or combined with behavior interventions on weight loss, our results showed no difference in weight loss in people with or without pre-treatment binge eating (SMD = − 0.434; CI = − 0.216 to 1.084; P = 0.191). We did not find evidence of heterogeneity in this meta-analysis. Finally, our meta-analysis investigating the effect of behavioral and/or nutritional interventions on weight loss found no difference in weight loss in people with or without pre-treatment binge eating (SMD = − 0.084; CI = − 0.478 to − 0.310; P = 0.675). We did not find evidence of heterogeneity in this meta-analysis. In addition, our assessment of reporting bias assessment did not show any effect on our results.
Forest plot by intervention subgroup and general. The first diamond (from the top-down) refers to behavioral and/or nutritional interventions, the second diamond refers to pharmacotherapy isolated or combined with behavior interventions, and the third diamond refers to weight loss surgery. The last diamond refers to all treatments combined
Studies that were not included in a meta-analysis, because data format was not suitable for a meta-analysis
Weight loss in people with or without binge eating who underwent weight loss surgery
Six studies assessed weight loss in people with or without pre-treatment binge eating who underwent bariatric surgery. Two of these studies found that people with binge eating lost significantly less weight in comparison with those without binge eating [33, 41] and four of these studies did not find significant differences in weight loss in people with or without binge eating [34, 36, 38, 43].
Weight loss in people with or without binge eating who received pharmacotherapy isolated or combined with behavior interventions
Three studies [44, 46, 47] assessed weight loss in people with or without pre-treatment binge eating who received pharmacotherapy isolated or combined with behavioral interventions. These studies did not find significant differences in weight loss in people with or without binge eating [44, 46, 47].
Weight loss in people with or without binge eating who received behavioral and/or nutritional interventions
Eight studies [51, 56,57,58, 60, 61, 63, 64] assessed weight loss in people with or without pre-treatment binge eating who received behavioral and/or nutritional interventions. Two of these studies found that people with binge eating lost significantly less weight in comparison with those without binge eating [60, 61], and 1 study showed that people with binge eating lost significantly more weight than people without binge eating [63]. However, most studies (i.e., 5 out of 8) did not find significant differences in weight loss between people with or without pre-treatment binge eating who received behavioral and/or nutritional interventions [51, 56,57,58, 64].
Discussion
The aim of this systematic review with meta-analyses was to compare changes in body weight in people with or without pre-treatment binge eating who received a variety of weight loss treatments. Overall, the meta-analyses found no differences in weight loss—between people with or without pre-treatment binge eating—at the end of treatment or last follow-up assessment reported in each study. There were also no differences in weight loss observed in sub-group analyses for different types of weight loss treatments or follow-up periods. While we found a difference in weight loss between people with or without pre-treatment binge eating in the studies of bariatric surgery, we were unable to conclude that there is a difference in weight loss due to high level of heterogeneity present. Furthermore, our qualitative analysis of studies that were not included in a meta-analysis (i.e., studies that did not report data in a format that was suitable for a meta-analysis) also showed no difference in weight loss in people with or without pre-treatment binge eating.
Our findings are in line with the results of a previous systematic review with meta-analysis that found no difference in weight loss between people with or without binge eating who underwent bariatric surgery [21]. In addition, our systematic review with meta-analyses expands the knowledge in this field as we found no difference in weight loss between people with or without binge eating who received other weight loss treatments (i.e., pharmacotherapy isolated or combined with behavior interventions; behavioral and/or nutritional interventions). Our findings contrasted with the findings of a matched-study meta-analysis that showed that people with pre-treatment BED lost significantly less weight compared to people without pre-treatment BED in a variety of weight loss treatments [26]. However, the method of that matched-study meta-analysis differs from our systematic review with meta-analyses [26]. For instance, as we mentioned in the Introduction, that matched-study meta-analysis did not comprehensively search the literature for all published studies that examined the effects of weight loss treatments in people with or without binge eating [26]. Moreover, that matched-study meta-analysis included only studies that were published until 2004, while our systematic review with meta-analyses included studies that were published until 2022 [26].
A potential explanation for our finding of similar weight loss in people with or without pre-treatment binge eating is that some weight loss treatments can potentially induce greater control over eating behavior. For example, some studies included in our systematic review showed that binge eating reduced once people received weight loss treatments [33, 37, 43,44,45, 47, 50, 52, 53, 55, 57, 60, 64]. Similarly, a randomized trial that was not included in our review showed that people with binge eating who received a dietary intervention reduced binge eating, uncontrolled eating, and emotional eating [67]. In addition, a longitudinal study showed that loss of control over eating and BED reduced 1 year after bariatric surgery (albeit loss of control over eating and BED resumed in the following years) [68]. Finally, a systematic review with meta-analysis found reductions in eating disorder symptoms, binge eating severity, and binge eating episodes in people with overweight or obesity who received behavior weight management interventions [69]. Overall, these studies suggest that weight loss interventions conducted under clinical supervision can potentially assist people in reducing binge eating at least during the treatment phase.
In conclusion, our systematic review with meta-analyses found no difference in weight loss in people with or without binge eating who received a variety of weight loss treatments. Thus, it is unlikely that pre-treatment binge eating will impede weight loss outcomes in people with overweight or obesity who received clinically supervised weight loss interventions. Notwithstanding that people with or without binge eating can reduce body weight similarly, psychological assessments of people with obesity seeking weight loss treatments can be useful to identify those who may benefit from eating disorder therapies.
Strengths and limits
Our systematic review with meta-analyses has several strengths and limitations. A notable strength is that [28]. Our review was comprehensive, as it included varied types of weight loss treatments or combinations of treatments, and samples of males and females of different age groups. We also performed sub-group analyses (e.g., based on different treatment categories, or length of the last assessment) and conducted a qualitative analysis of studies that were not included in a meta-analysis, allowing us to gain a comprehensive understanding of weight change in individuals with or without pre-treatment binge eating who underwent various weight loss interventions. Our systematic review with meta-analyses was limited in that the risk of bias assessment showed that some of the included studies had a low-quality regarding method of randomization, allocation concealment, blind participants and assessors, and sample power calculation, which lowers the strength of data reported in these studies. In addition, this review was limited in that there were differences in the methods used to classify the occurrence of binge eating in the included studies. Some of the studies included participants that met full criteria for BED, while other studies included participants with subthreshold BED, or participants only with loss of control over eating. This is relevant as more extreme comparisons (e.g., people with BED versus people without binge eating) can potentially show significantly greater differences in weight loss [26]. Second, we did not examine the effects of weight loss treatments on binge eating behaviors. This is an important consideration, because the occurrence or absence of binge eating episodes during a weight loss treatment can potentially interfere with weight loss outcomes. For example, a previous study found that people with pre-treatment binge eating that stopped binge eating once they received an intensive lifetime intervention were just as successful to lose weight as people without binge eating [20]. In addition, most studies included in our systematic review did not assess whether participants engaged in other eating disorder behaviors (e.g., compulsive exercise, self-induced vomiting, or abuse of laxatives/diuretics) that can potentially influence weight loss outcomes. It is noteworthy that we did not investigate the safety of weight loss treatments on mental health of people with overweight or obesity and recurrent binge eating and the risk of transitioning to a restrictive eating disorder, such as atypical anorexia [70]. Even though behavior weight management interventions do not increase eating disorder behaviors in most adults, a small proportion of people (0–6.5%) can be at risk of experiencing eating disorder symptoms during or after behavior weight loss treatments [69]. Thus, in any event eating disorder therapies following updated guidelines should be provided to people with a high body weight and comorbid binge eating seeking weight loss treatments [71]. Finally, it should be noted that the differential weight loss in people with or without binge eating derives mostly from sub-analyses of the studies included in our review.
What is already known about this subject?
Previous studies showed contrasting findings on whether pre-treatment binge eating can hinder weight loss in people who received obesity treatments.
What do we now know as a result of this study that we did not know before?
Our systematic review with meta-analyses found no difference in weight loss in people with or without pre-treatment binge eating who received varied types of weight loss treatments. Weight loss treatments should not be withheld on the basis that they will not be effective in people with pre-treatment binge eating. However, further research is needed to investigate the safety and long-term impacts of weight loss treatments in people with recurrent binge eating.
Data availability
Not applicable.
References
Peralta M et al (2018) Prevalence and trends of overweight and obesity in older adults from 10 European countries from 2005 to 2013. Scand J Public Health 46(5):522–529
Barber JA et al (2015) Medication use and metabolic syndrome among overweight/obese patients with and without binge-eating disorder in a primary care sample. Prim Care Companion CNS Disord 17(5):27470
Blüher M (2019) Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol 15:288–297
Association, A.P. (2013) Diagnostic and statistical manual of mental disorders, 5th edn. Association A.P., Washington, DC
McCuen-Wurst C, Ruggieri M, Allison KC (2018) Disordered eating and obesity: associations between binge-eating disorder, night-eating syndrome, and weight-related comorbidities. Ann N Y Acad Sci 1411(1):96–105
Hay P, Girosi F, Mond J (2015) Prevalence and sociodemographic correlates of DSM-5 eating disorders in the Australian population. J Eat Disord 3:19
Bianciardi E et al (2019) Prevalence of Food Addiction and Binge Eating in an Italian sample of bariatric surgery candidates and overweight/obese patients seeking low-energy-diet therapy. Riv Psichiatr 54(3):127–130
Palavras MA et al (2011) A review of Latin American studies on binge eating disorder. Braz J Psychiatry 33(Suppl 1):S81-108
Villarejo C et al (2012) Lifetime obesity in patients with eating disorders: increasing prevalence, clinical and personality correlates. Eur Eat Disord Rev 20(3):250–254
Keski-Rahkonen A, Mustelin L (2016) Epidemiology of eating disorders in Europe: prevalence, incidence, comorbidity, course, consequences, and risk factors. Curr Opin Psychiatry 29(6):340–345
da Luz FQ et al (2017) Prevalence of obesity and comorbid eating disorder behaviors in South Australia from 1995 to 2015. Int J Obes (Lond) 41(7):1148–1153
Černelič-Bizjak M (2022) Predictors of binge eating: Relevance of BMI, emocional eating and sensivity to environmental food cues. Nutr Food Sci 52:171–180
Hart LM et al (2011) Unmet need for treatment in the eating disorders: a systematic review of eating disorder specific treatment seeking among community cases. Clin Psychol Rev 31(5):727–735
Cachelin FM, Striegel-Moore RH (2006) Help seeking and barriers to treatment in a community sample of Mexican American and European American women with eating disorders. Int J Eat Disord 39(2):154–161
Appolinario JC et al (2022) Correlates and impact of DSM-5 binge eating disorder, bulimia nervosa and recurrent binge eating: a representative population survey in a middle-income country. Soc Psychiatry Psychiatr Epidemiol 57(7):1491–1503
Mond JM et al (2009) Women with bulimic eating disorders: When do they receive treatment for an eating problem? J Consult Clin Psychol 77(5):835–844
Mond JM et al (2009) Comparing the health burden of eating-disordered behavior and overweight in women. J Womens Health (Larchmt) 18(7):1081–1089
Wilfley DE et al (2002) A randomized comparison of group cognitive-behavioral therapy and group interpersonal psychotherapy for the treatment of overweight individuals with binge-eating disorder. Arch Gen Psychiatry 59(8):713–721
Devlin MJ et al (2005) Cognitive behavioral therapy and fluoxetine as adjuncts to group behavioral therapy for binge eating disorder. Research 13(6):1077–1088
Gorin AA et al (2008) Binge eating and weight loss outcomes in overweight and obese individuals with type 2 diabetes: results from the Look AHEAD trial. Arch Gen Psychiatry 65(12):1447–1455
Kops NL et al (2021) Preoperative binge eating and weight loss after bariatric surgery: a systematic review and meta-analysis. Obes Surg 31(3):1239–1248
Fujioka K et al (2008) Evaluating preoperative weight loss, binge eating disorder, and sexual abuse history on Roux-en-Y gastric bypass outcome. Surg Obes Relat Dis 4(2):137–143
Abiles V et al (2013) Effectiveness of cognitive-behavioral therapy in morbidity obese candidates for bariatric surgery with and without binge eating disorder. Nutr Hosp 28(5):1523–1529
Barnes RD et al (2014) A randomized controlled trial comparing scalable weight loss treatments in primary care. Obesity 22(12):2508–2516
Barnes RD et al (2018) Examining motivational interviewing plus nutrition psychoeducation for weight loss in primary care. J Psychosom Res 104:101–107
Blaine B, Rodman J (2007) Responses to weight loss treatment among obese individuals with and without BED: a matched-study meta-analysis. Eat Weight Disord 12(2):54–60
Palavras MA et al (2021) Integrated weight loss and cognitive behavioural therapy (CBT) for the treatment of recurrent binge eating and high body mass index: a randomized controlled trial. Eat Weight Disord 26(1):249–262
Page MJ et al (2021) Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. J Clin Epidemiol 134:103–112
Sackett D et al (1997) How to practice and teach evidence based medicine. Churchill Livingstone
Higgins J, Deeks J, Altman D (2011) Chapter 16: special topics in statistics. In: Deeks J (ed) Cochrane handbook for systematic reviews of interventions version 5.1.0 (updated March 2011). The Cochrane Collaboration
Downs SH, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52(6):377–384
Alger-Mayer S et al (2009) Preoperative binge eating status and gastric bypass surgery: a long-term outcome study. Surgery 19(2):139–145
Chao AM et al (2016) Binge-eating disorder and the outcome of bariatric surgery in a prospective, observational study: two-year results. Obesity (Silver Spring) 24(11):2327–2333
Colles SL, Dixon JB, O’Brien PE (2008) Grazing and loss of control related to eating: two high-risk factors following bariatric surgery. Obesity (Silver Spring) 16(3):615–622
Green AE et al (2004) Psychosocial outcome of gastric bypass surgery for patients with and without binge eating. Obes Surg 14(7):975–985
Nikiforova I et al (2019) Analysis of the association between eating behaviors and weight loss after laparoscopic sleeve gastrectomy. Obes Facts 12(6):618–631
Wadden TA et al (2011) Binge eating disorder and the outcome of bariatric surgery at one year: a prospective, observational study. Obesity (Silver Spring) 19(6):1220–1228
Bocchieri-Ricciardi LE et al (2006) Pre-surgery binge eating status: effect on eating behavior and weight outcome after gastric bypass. Obes Surg 16(9):1198–1204
Kops NL et al (2020) Binge eating scores pre-bariatric surgery and subsequent weight loss: a prospective, 5 years follow-up study. Clin Nutr ESPEN 38:146–152
Puglisi F et al (2007) Intragastric balloon and binge eating. Obes Surg 17(4):504–509
Sallet PC et al (2007) Eating behavior as a prognostic factor for weight loss after gastric bypass. Obes Surg 17(4):445–451
Susmallian S et al (2017) Do pre-surgery eating habits affect weight loss one year following a sleeve gastrectomy? Clin Nutr ESPEN 19:5
Ben-Porat T et al (2021) Food addiction and binge eating during one year following sleeve gastrectomy: prevalence and implications for postoperative outcomes. Obes Surg 31(2):603–611
Alger SA et al (1999) Beneficial effects of pharmacotherapy on weight loss, depressive symptoms, and eating patterns in obese binge eaters and non-binge eaters. Obes Res 7(5):469–476
Bauer C, Fischer A, Keller U (2006) Effect of sibutramine and of cognitive-behavioural weight loss therapy in obesity and subclinical binge eating disorder. Diabetes Metab 8(3):289–295
de Zwaan M, Nutzinger DO, Schoenbeck G (1992) Binge eating in overweight women. Compr Psychiatry 33(4):256–261
Marcus MD et al (1990) A double-blind, placebo-controlled trial of fluoxetine plus behavior modification in the treatment of obese binge-eaters and non-binge-eaters. Am J Psychiatry 147(7):876–881
Grilo CM, White MA (2013) Orlistat with behavioral weight loss for obesity with versus without binge eating disorder: Randomized placebo-controlled trial at a community mental health center serving educationally and economically disadvantaged Latino/as. Behav Res Ther 51(3):167–175
Grilo CM et al (2021) Physical activity changes during behavioral weight loss treatment by Latinx patients with obesity with and without binge eating disorder. Obesity (Silver Spring) 29(12):2026–2034
Carbone EA et al (2021) An open-label trial on the efficacy and tolerability of naltrexone/bupropion SR for treating altered eating behaviours and weight loss in binge eating disorder. Eat Weight Disord 26(3):779–788
Delinsky SS, Latner JD, Wilson GT (2006) Binge eating and weight loss in a self-help behavior modification program. Obesity (Silver Spring) 14(7):1244–1249
Porzelius LK, Houston C, Smith M, Arfken C, Fisher E Jr (1995) Comparison of a standard behavioral weight loss treatment and a binge eating weight loss treatment. Behav Ther 26:119–134
Nauta H et al (2000) A comparison between a cognitive and a behavioral treatment for obese binge eaters and obese non-binge eaters. Behav Ther 31(3):441–461
Balantekin KN et al (2017) Patterns of eating disorder pathology are associated with weight change in family-based behavioral obesity treatment. Obesity (Silver Spring) 25(12):2115–2122
Bishop-Gilyard CT et al (2011) Weight reduction in obese adolescents with and without binge eating. Obesity 19(5):982–987
LaPorte DJ (1992) Treatment response in obese binge eaters: preliminary results using a very low calorie diet (VLCD) and behavior therapy. Addict Behav 17(3):247–257
Raymond NC et al (2002) Effect of a very low calorie diet on the diagnostic category of individuals with binge eating disorder. Int J Eat Disord 31(1):49–56
Telch CF, Agras WS (1993) The effects of a very low calorie diet on binge eating. Behav Ther 24(2):177–193
Björkman S et al (2020) Nocturnal eating but not binge eating disorder is related to less 12 months’ weight loss in men and women with severe obesity: a retrospective cohort study. Clin Obes 10:1–9
Chao AM et al (2017) Binge eating and weight loss outcomes in individuals with type 2 diabetes: 4-year results from the look AHEAD study. Obesity (Silver Spring) 25(11):1830–1837
Masheb RM et al (2015) High-frequency binge eating predicts weight gain among veterans receiving behavioral weight loss treatments. Obesity (Silver Spring) 23(1):54–61
Wadden TA, Foster GD, Letizia KA (1992) Response of obese binge eaters to treatment by behavior therapy combined with very low calorie diet. J Consult Clin Psychol 60(5):808–811
Gladis MM et al (1998) Behavioral treatment of obese binge eaters: do they need different care? J Psychosom Res 44(3–4):375–384
Tseng MC et al (2004) Response of Taiwanese obese binge eaters to a hospital-based weight reduction program. J Psychosom Res 57(3):279–285
Yanovski SZ et al (1994) Binge eating disorder affects outcome of comprehensive very-low-calorie diet treatment. Obes Res 2(3):205–212
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. L. Erlbaum Associates, Hillsdale
Mason C et al (2019) Eating behaviors and weight loss outcomes in a 12-month randomized trial of diet and/or exercise intervention in postmenopausal women. Int J Behav Nutr Phys Activity 16(1):1–11
Smith KE et al (2019) Loss of control eating and binge eating in the 7 years following bariatric surgery. Obes Surg 29(6):1773–1780
Jebeile H et al (2023) Eating disorder risk during behavioral weight management in adults with overweight or obesity: a systematic review with meta-analysis. Obes Rev 24:e13561
Watson C, Riazi A, Ratcliffe D (2020) Exploring the experiences of women who develop restrictive eating behaviours after bariatric surgery. Obes Surg 30(6):2131–2139
Ralph AF et al (2022) Management of eating disorders for people with higher weight: clinical practice guideline. J Eat Disord 10(1):121
Acknowledgements
Isabella Lobo and Felipe Q da Luz are supported by Young Investigator Grants, Fellowships, and/or Scholarships from the São Paulo Research Foundation—FAPESP (2018/18028-2, 2020/04181-3, 2019/14622-0). Amanda Sainsbury was supported by the National Health and Medical Research Council (NHMRC) of Australia via a Senior Research Fellowship (1135897). Zubeyir Salis is the recipient of a Swiss Government Excellence Scholarship and an Australian Government Research Training Program Scholarship.
Funding
Open access funding provided by University of Geneva This study was supported by Fundação de Amparo à Pesquisa do Estado de São Paulo (Grant numbers 2018/18028-2, 2020/04181-3, 2019/14622-0); National Health and Medical Research Council (Grant number 1135897).
Author information
Authors and Affiliations
Contributions
IL and FQdL were responsible for designing the review protocol, writing the protocol, screening potentially eligible studies and interpreting the results. IL conducted the search, extracted and analyzed data, updated reference lists and conceived the work that led to the submission. TG contributed to the screening of potentially eligible studies. PT contributed to the assessment of the quality of the studies included in the systematic review with ILS. Zubeyir Salis was responsible for meta-analyses, conducted the meta-regression analyses and revised the manuscript and approved the final version. All authors revised the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
Amanda Sainsbury and Zubeyir Salis own 50% each of the shares in Zuman International, a company that receives royalties and other payments for educational resources and services about adult weight management and research methodology. Amanda Sainsbury has also received presentation fees and travel reimbursements from Eli Lilly and Co, the Pharmacy Guild of Australia, Novo Nordisk, the Dietitians Association of Australia, Shoalhaven Family Medical Centres, the Pharmaceutical Society of Australia, and Metagenics, and served on the Nestlé Health Science Optifast VLCD advisory board from 2016 to 2018. Phillipa Hay receives/has received sessional fees and lecture fees from the Australian Medical Council, Therapeutic Guidelines publication, and HETI New South Wales Institute of Psychiatry and royalties/honoraria from Hogrefe and Huber, McGraw Hill Education, and Blackwell Scientific Publications, Biomed Central and PlosMedicine and she has received research grants from the NHMRC and ARC. She is Chair of the National Eating Disorders Collaboration Steering Committee in Australia and was a Member of the ICD-11 Working Group for Eating Disorders (2012–2019), and was Chair Clinical Practice Guidelines Project Working Group (Eating Disorders) of RANZCP (2012–2015). She has prepared a report under contract for Shire Pharmaceuticals regarding Binge Eating Disorder (July 2017) and consulting fees for the education of doctors from Takeda Pharmaceuticals. All views in this paper are her own. Author A and B declare they have no financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lobo, I., da Luz, F.Q., Hay, P. et al. Is binge eating associated with poor weight loss outcomes in people with a high body weight? A systematic review with meta-analyses. Eat Weight Disord 28, 89 (2023). https://doi.org/10.1007/s40519-023-01613-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40519-023-01613-9