Abstract
Purpose of Review
This article provides a brief overview of the development of pediatric physiologically based pharmacokinetic (PPBPK) models, the challenges of uncertain systems information, and finally performance verification considering recent regulatory guidance.
Recent Findings
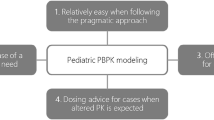
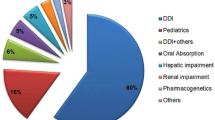
Pediatric PBPK (PPBPK) model can incorporate varied manifolds of drug and developmental system information to predict drug PK in children. Health authorities have been receiving a growing number of drug submissions that have used PPBPK. According to a recent review of the FDA office of Clinical Pharmacology, PPBPK modeling has been readily applied for dose regimen selection in a variety of pediatric patient groups via a “learn and confirm” approach. Before applying to pediatrics, a PBPK model is developed using physicochemical, biopharmaceutical, and metabolic parameters of drug and then verified by pharmacokinetics (PK) data in adults. Once the drug parameters are optimized, they can be used in the PPBPK model which contains the ‘systemic’ data of physiology and biochemistry in children. The drug absorption, distribution, metabolism, and excretion (ADME) parameters can be estimated according to developmental changes in physiology and biochemistry in various age groups of children. The model is then applied to simulate the exposure in children. The current challenge is the paucity of available pediatric systems information and oral biopharmaceutics. They are essential to verify PPBPK models and predict PK particularly in neonates and young infants. The recent research on intestinal and hepatic transporter ontogeny, via mRNA and proteomic data, gives us increased understanding of pediatric drug absorption, hepatic uptake, and biliary excretion. Nevertheless, more validated developmental ‘system’ data is needed in this field. Another gap is the lack of good quality pediatric drug studies performed across the age range, which currently is a limitation to the performance verification of PPBPK models.
Summary
PPBPK models have already improved the pediatric drug development process but the important challenges lie ahead. Further development and verification are constantly required. It may be possible to minimize the number of pediatric subjects used in PK studies and avoid some studies altogether.




Similar content being viewed by others
References
FDA, Leveraging Existing Clinical Data for Extrapolation to Pediatric Uses of Medical Devices Guidance for Industry and Food and Drug Administration Staff. https://www.fda.gov/downloads/medicaldevices/deviceregulationandguidance/guidancedocuments/ucm444591.pdf, 2016.
Johnson TN, Rostami-Hodjegan A. Resurgence in the use of physiologically based pharmacokinetic models in pediatric clinical pharmacology: parallel shift in incorporating the knowledge of biological elements and increased applicability to drug development and clinical practice. Paediatr Anaesth. 2011;21(3):291–301.
Strougo A, Eissing T, Yassen A, Willmann S, Danhof M, Freijer J. First dose in children: physiological insights into pharmacokinetic scaling approaches and their implications in paediatric drug development. J Pharmacokinet Pharmacodyn. 2012;39(2):195–203.
Barrett JS, Della Casa Alberighi O, Läer S, Meibohm B. Physiologically based pharmacokinetic (PBPK) modeling in children. Clin Pharmacol Ther. 2012;92(1):40–9.
Wagner C, Zhao P, Pan Y, Hsu V, Grillo J, Huang SM, et al. Application of physiologically based pharmacokinetic (PBPK) modeling to support dose selection: report of an FDA public workshop on PBPK. CPT Pharmacometrics Syst Pharmacol. 2015;4:226–30.
Mehrotra N, Bhattaram A, Earp JC, Florian J, Krudys K, Lee JE, et al. Role of quantitative clinical pharmacology in pediatric approval and labeling. Drug Metab Dispos. 2016;44(7):924–33.
Maharaj AR, Edginton AN. Physiologically based pharmacokinetic modeling and simulation in pediatric drug development. CPT Pharmacometrics Syst Pharmacol. 2014;3(11):1–13.
Zhou W, Johnson TN, Bui KH, Cheung SYA, Li J, Xu H, et al. Predictive performance of physiologically based pharmacokinetic (PBPK) modeling of drugs extensively metabolized by major cytochrome P450s in children. Clin Pharmacol Ther. 2017;104(1):188–200
de Zwart LL, Rompelberg CJM, Sips AJAM, Welink J, Van Engelen JGM. Anatomical and physiological differences between various species used in studies on the pharmacokinetics and toxicology of xenobiotics. A review of literature. Bilthoven (NL): National Institute of Public Health and the Environment; 1999. (Report No.: 623860 010.)
Leong R, Vieira MLT, Zhao P, Mulugeta Y, Lee CS, Huang SM, et al. Regulatory experience with physiologically based pharmacokinetic modeling for pediatric drug trials. Clin Pharmacol Ther. 2012;91(5):926–31.
Batchelora H, Kaukonena AM, Klein S, Davite B, Ju R, Ternik R, et al. Food effects in paediatric medicines development for products co-administered with food. Int J Pharm. 2018;536(2):530–535.
Batchelor HK, Fotaki N, Klein S. Paediatric oral biopharmaceutics: key considerations and current challenges. Adv Drug Deliv Rev. 2014;73:102–26.
SimulationsPlus, ADMET Predictor, 2016.
Tsamandouras N, Rostami-Hodjegan A, Aarons L. Combining the ‘bottom up’ and ‘top down’ approaches in pharmacokinetic modelling: fitting PBPK models to observed clinical data. Br J Clin Pharmacol. 2015;79(1):48–55.
Lin W, Heimbach T, Jain JP, Awasthi R, Hamed K, Sunkara G, et al. A physiologically based pharmacokinetic model to describe Artemether pharmacokinetics in adult and pediatric patients. J Pharm Sci. 2016;105(10):3205–13.
Bonner JJ, Vajjah P, Abduljalil K, Jamei M, Rostami-Hodjegan A, Tucker GT, et al. Does age affect gastric emptying time? A model-based metaanalysis of data from premature neonates through to adults. Biopharm Drug Dispos. 2015;36(4):245–57.
Colussi D, Parisot C, Legay F, Lefèvre G. Binding of artemether and lumefantrine to plasma proteins and erythrocytes. Eur J Pharm Sci. 1999;9:9–16.
Honda M, Muroi Y, Tamaki Y, Saigusa D, Suzuki N, Tomioka Y, et al. Functional characterization of CYP2B6 allelic variants in demethylation of antimalarial artemether. Drug Metab Dispos. 2011;39(10):1860–5.
Ezzet F, Mull R, Karbwang J. Population pharmacokinetics and therapeutic response of CGP 56697 (artemether + benflumetol) in malaria patients. Br J Clin Pharmacol. 1998;46(6):553–61.
Salman S, Page-Sharp M, Griffin S, Kose K, Siba PM, Ilett KF, et al. Population pharmacokinetics of artemether, lumefantrine, and their respective metabolites in Papua new Guinean children with uncomplicated malaria. Antimicrob Agents Chemother. 2011;55(11):5306–13.
Zhang T, Heimbach T, Lin W, Zhang J, He H. Prospective predictions of human pharmacokinetics for eighteen compounds. J Pharm Sci. 2015;104(9):2795–806.
Van Den Driessche M, et al. Lactose-[13C]ureide breath test: a new, noninvasive technique to determine orocecal transit time in children. J Pediatr Gastroenterol Nutr. 2000;31(4):433–8.
Jiang X-L, Zhao P, Barrett JS, Lesko LJ, Schmidt S. Application of physiologically based pharmacokinetic modeling to predict acetaminophen metabolism and pharmacokinetics in children. CPT Pharmacometrics Syst Pharmacol. 2013;2(10):e80.
Brown RP, Delp MD, Lindstedt SL, Rhomberg LR, Beliles RP. Physiological parameter values for physiologically based pharmacokinetic models. Toxicol Ind Health. 1997;13(4):407–84.
Zhang SC, Wang WL, Bai YZ, Yuan ZW, Wang W. Determination of total and segmental colonic transit time in constipated children. Zhonghua Er Ke Za Zhi. 2003;41(3):176–9.
Bautista Casasnovas A, et al. Measurement of colonic transit time in children. J Pediatr Gastroenterol Nutr. 1991;13(1):42–5.
Kohlmann P, Stillhart C, Kuentz M, Parrott N. Investigating Oral absorption of carbamazepine in pediatric populations. AAPS J. 2017;19(6):1864–77.
Murphy GM, Signer E. Bile acid metabolism in infants and children. Gut. 1974;15(2):151–63.
Maharaj AR, Edginton AN, Fotaki N. Assessment of age-related changes in pediatric gastrointestinal solubility. Pharm Res. 2016;33(1):52–71.
Villiger A, Stillhart C, Parrott N, Kuentz M. Using physiologically based pharmacokinetic (PBPK) modelling to gain insights into the effect of physiological factors on Oral absorption in Paediatric populations. AAPS J. 2016;18(4):933–47.
Mooij MG, Schwarz UI, de Koning BAE, Leeder JS, Gaedigk R, Samsom JN, et al. Ontogeny of human hepatic and intestinal transporter gene expression during childhood: age matters. Drug Metab Dispos. 2014;42(8):1268–74.
Mizuno T, Fukuda T, Masuda S, Uemoto S, Matsubara K, Inui KI, et al. Developmental trajectory of intestinal MDR1/ABCB1 mRNA expression in children. Br J Clin Pharmacol. 2014;77(5):910–2.
Lukacova V, Goelzer P, Reddy M, Greig G, Reigner B, Parrott N. A physiologically based pharmacokinetic model for ganciclovir and its prodrug Valganciclovir in adults and children. AAPS J. 2016;18(6):1453–63.
Lam J, Baello S, Iqbal M, Kelly LE, Shannon PT, Chitayat D, et al. The ontogeny of P-glycoprotein in the developing human blood-brain barrier: implication for opioid toxicity in neonates. Pediatr Res. 2015;78(4):417–21.
Einolf HJ, Lin W, Won CS, Wang L, Gu H, Chun DY, et al. Physiologically based pharmacokinetic model predictions of Panobinostat (LBH589) as a victim and perpetrator of drug-drug interactions. Drug Metab Dispos. 2017;45(12):1304–16.
Zhao P, Rowland M, Huang SM. Best practice in the use of physiologically based pharmacokinetic modeling and simulation to address clinical pharmacology regulatory questions. Clin Pharmacol Ther. 2012;92(1):17–20.
Howgate EM, Rowland Yeo K, Proctor NJ, Tucker GT, Rostami-Hodjegan A. Prediction of in vivo drug clearance from in vitro data. I: impact of inter-individual variability. Xenobiotica. 2006;36(6):473–97.
Upreti V. And W.J. L, Meta-analysis of hepatic cytochrome P450 ontogeny to underwrite the prediction of pediatric pharmacokinetics using physiologically based pharmacokinetic modeling. J Clin Pharmacol. 2016;56(3):266–83.
Salem F, Johnson TN, Abduljalil K, Tucker GT, Rostami-Hodjegan A. A re-evaluation and validation of ontogeny functions for cytochrome P450 1A2 and 3A4 based on in vivo data. Clin Pharmacokinet. 2014;53(7):625–36.
Zaya MJ, Hines RN, Stevens JC. Epirubicin glucuronidation and UGT2B7 developmental expression. Drug Metab Dispos. 2006;34(12):2097–101.
Holford NH, Ma SC, Anderson BJ. Prediction of morphine dose in humans. Paediatr Anaesth. 2012;22(3):209–22.
Chau N, Elliot DJ, Lewis BC, Burns K, Johnston MR, Mackenzie PI, et al. Morphine glucuronidation and glucosidation represent complementary metabolic pathways that are both catalyzed by UDP-glucuronosyltransferase 2B7: kinetic, inhibition, and molecular modeling studies. J Pharmacol Exp Ther. 2014;349(1):126–37.
Boberg M, Vrana M, Mehrotra A, Pearce RE, Gaedigk A, Bhatt DK, et al. Age-dependent absolute abundance of hepatic carboxylesterases (CES1 and CES2) by LC-MS/MS proteomics: application to PBPK modeling of oseltamivir in vivo pharmacokinetics in infants. Drug Metab Dispos. 2017;45(2):216–23.
Prasad B, Gaedigk A, Vrana M, Gaedigk R, Leeder JS, Salphati L, et al. Ontogeny of hepatic drug transporters as quantified by LC-MS/MS proteomics. Clin Pharmacol Ther. 2016;100(4):362–70.
Brouwer KL, et al. Human ontogeny of drug transporters: review and recommendations of the pediatric transporter working group. Clin Pharmacol Ther. 2015;98(3):266–87.
Johnson TN, Jamei M, Rowland-Yeo K. How does in vivo biliary elimination of drugs change with age? Evidence from in vitro and clinical data using a systems pharmacology approach. Drug Metab Dispos. 2016;44(7):1090–8.
Rhodin MM, Anderson BJ, Peters AM, Coulthard MG, Wilkins B, Cole M, et al. Human renal function maturation: a quantitative description using weight and postmenstrual age. Pediatr Nephrol. 2009;24(1):67–76.
Sweet DH, Bush KT, Nigam SK. The organic anion transporter family: from physiology to ontogeny and the clinic. Am J Physiol Renal Physiol. 2001;281(2):F197–205.
Jorga K, Chavanne C, Frey N, Lave T, Lukacova V, Parrott N, et al. Bottom-up meets top-down: complementary physiologically based pharmacokinetic and population pharmacokinetic modeling for regulatory approval of a dosing algorithm of Valganciclovir in very young children. Clin Pharmacol Ther. 2016;100(6):761–9.
Johnson TN, Rostami-Hodjegan A, Tucker GT. Prediction of the clearance of eleven drugs and associated variability in neonates, infants and children. Clin Pharmacokinet. 2006;45(9):931–56.
Abduljalil K, Jamei M, Rostami-Hodjegan A, Johnson TN. Changes in individual drug-independent system parameters during virtual paediatric pharmacokinetic trials: introducing time-varying physiology into a paediatric PBPK model. AAPS J. 2014;16(3):568–76.
Emoto C, Fukuda T, Johnson TN, Neuhoff S, Sadhasivam S, Vinks AA. Characterization of contributing factors to variability in morphine clearance through PBPK modeling implemented with OCT1 transporter. CPT Pharmacometrics Syst Pharmacol. 2017;6(2):110–9.
Fukuda T, Chidambaran V, Mizuno T, Venkatasubramanian R, Ngamprasertwong P, Olbrecht V, et al. OCT1 genetic variants influence the pharmacokinetics of morphine in children. Pharmacogenomics. 2013;14(10):1141–51.
Sinha, V. Application of PBPK Modeling and Simulations in Pediatric Drug Development. 2014 [cited 2015 Dec., 17th, 2015]; Available from: http://www.pharmacy.umaryland.edu/media/SOP/wwwpharmacyumarylandedu/centers/cersievents/pediatricpbpk/SinhaNotes.pdf.
Jamei M. Recent advances in development and application of physiologically-based pharmacokinetic (PBPK) models: a transition from academic curiosity to regulatory acceptance. Curr Pharmacol Rep. 2016;2:161–9.
EMA, Guideline on the qualification and reporting of physiologically based pharmacokinetic (PBPK) modelling and simulation. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2016/07/WC500211315.pdf, 2016.
FDA, Physiologically Based Pharmacokinetic Analyses — Format and Content Guidance for Industry Draft Guidance. https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM531207.pdf, 2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Wen Lin, Jing-He Yan, Tycho Heimbach, and Handan He declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pharmacometrics
Rights and permissions
About this article
Cite this article
Lin, W., Yan, JH., Heimbach, T. et al. Pediatric Physiologically Based Pharmacokinetic Model Development: Current Status and Challenges. Curr Pharmacol Rep 4, 491–501 (2018). https://doi.org/10.1007/s40495-018-0162-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40495-018-0162-1