Abstract
In human leukocyte antigen (HLA)-mismatched allogeneic stem cell transplantation settings, donor-specific anti-HLA antibodies (DSAs) can independently lead to graft failure, including both primary graft rejection and primary poor graft function. Although several strategies, such as plasma exchange, intravenous immunoglobulin, rituximab, and bortezomib, have been used for DSA desensitization, the effectiveness of desensitization and transplantation outcomes in some patients remain unsatisfactory. In this review, we summarized recent research on the prevalence of anti-HLA antibodies and the underlying mechanism of DSAs in the pathogenesis of graft failure. We mainly focused on desensitization strategies for DSAs, especially novel methods that are being investigated in the preclinical stage and those with promising outcomes after preliminary clinical application.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Risk factors for anti-human leukocyte antigen (HLA) antibodies or donor-specific anti-HLA antibodies (DSAs) reported thus far include female sex, older age, pregnancy, and transfusion. |
DSAs are strongly associated with primary graft failure, such as primary graft rejection and primary poor graft function, and survival, in patients who underwent HLA-mismatched allogeneic transplantation. |
The pathogenesis of graft failure caused by DSAs after allogeneic transplantation may not only be related to follicular T cells but also to B cells and plasma cells. |
Combinations of different methods that target different immune cells involved in the pathogenesis of graft failure might be more effective than a single approach, especially for those subjects with a DSA mean fluorescence intensity (MFI) greater than 5000 or 10,000. |
Further efforts are needed to answer the unanswered questions, for example, the optimal combination of different desensitization strategies for patients with high levels of DSAs. |
Introduction
Allogeneic stem cell transplantation (allo-SCT) remains a curative therapy for patients with either hematological or nonhematological malignancies [1,2,3,4,5,6,7]. In the past 2 decades, due to the use of human leukocyte antigen (HLA)-mismatched donors, nearly each transplant candidate has a donor [8,9,10,11,12]. Currently, the proportions of HLA-matched sibling donor transplantation are only 27.7%, 21.0%, and 28.8% of the total allo-SCT population according to activity survey data from Europe, the USA, and China, respectively [13,14,15]. For HLA-mismatched allo-SCT recipients, primary graft failure, including primary graft rejection (GR) and primary poor graft function (PGF), remains one of the barriers to successful hematopoietic reconstitution posed by donor-specific anti-HLA antibodies (DSAs) and one of the main causes of death [16,17,18,19].
Presently, several strategies, such as plasma exchange, intravenous immunoglobulin, rituximab, and bortezomib, have been successfully used for DSA desensitization [20,21,22,23,24]. However, no single desensitization method or an optimal combination of different desensitization approaches is suitable for all DSA-positive hematopoietic stem cell transplantation (HSCT) candidates. In addition, some patients fail DSA desensitization and experience poor transplant outcomes. More recently, in vitro and in vivo studies have shown that targeting T follicular helper (Tfh) cells is a novel approach for DSA desensitization in patients who are candidates for HLA-mismatched SCT [25, 26]. In a mouse model, researchers from the USA demonstrated that treatment of allo-sensitized hosts with chimeric antigen receptor T (CAR-T) cells targeting allo-specific memory B cells (Bmems) and long-lived plasma cells (LLPCs) can successfully eliminate DSAs and mitigate hyperacute rejection of subsequent islet allografts [27]. In this review, we aimed to discuss recent studies on the prevalence of anti-HLA antibodies, the association of DSAs with graft failure, and the underlying mechanism of DSAs in the pathogenesis of graft failure in HLA-mismatched transplant candidates. We focused mainly on advances in novel desensitization methods investigated at the preclinical stage and those with promising outcomes after preliminary clinical application.
This article is based on previously conducted research and does not contain any new studies with animals or human participants carried out by any of the authors.
Prevalence and Risk Factors for HLA Antibodies and DSAs in Allogeneic Transplantation Recipients
The prevalence of anti-HLA antibodies ranges from < 1% to 5% in healthy volunteers, 24.4% to 54.4% in pregnant women, and 23.2% to 32.8% in organ transplant candidates [28,29,30,31,32,33,34,35,36]. Gladstone et al. reported that the overall incidence of anti-HLA antibodies was 23%, which was greater among parous females than among males and nulliparous females. The risk of DSAs to potential donors was 14.5%, which included moderate to strong reactivity in 68.4% of the haploidentical donors and 46.7% of the unrelated donors. For female recipients, DSAs were more common against their children than against their siblings or parents [37]. Ciurea et al. reported that 18% of 122 patients who received haplo-HSCT were DSA-positive. A greater percentage of DSA-positive patients were diagnosed with acute myeloid leukemia (AML)/myelodysplastic syndromes (MDS) than patients who are DSA-negative[38]. Overall, in haploidentical transplant modalities, the incidences of anti-HLA antibodies and DSAs are approximately 20–70% and 10–30%, respectively [16, 39,40,41]. However, in unrelated donor or cord blood transplant settings, the prevalences of anti-HLA antibodies and DSAs are approximately 20–40% and 1–7%, respectively [42,43,44,45].
The current cutoff values for identifying positivity for anti-HLA antibodies or DSAs are not consistent in the available literature [16, 39,40,41,42,43,44,45]. A recent prospective study enrolled 3805 patients with hematologic disease. Ma et al. reported that 20.2% of patients were positive for anti-HLA class I or II antibodies, 17.9% were positive for anti-HLA class I antibodies, 9.5% were positive for anti-HLA class II antibodies, and 7.1% were positive for both anti-HLA class I and class II antibodies, according to an mean fluorescence intensity (MFI) cutoff value ≥ 500 [29, 42, 46,47,48,49,50,51,52]. A multivariate analysis indicated that platelet transfusion and pregnancy were the most important risk factors for the presence of anti-HLA antibodies according to different MFI cutoff values, such as 1000, 2000, 5000, and 10,000, for antibody positivity [53]. However, the prevalence of DSAs was not shown in this study. In summary, the risk factors for anti-HLA antibodies or DSAs reported thus far, such as female sex, older age, pregnancy, and transfusion, can serve as biomarkers for evaluating anti-HLA antibodies and DSAs as well as aiding donor selection [11, 23, 54].
Associations of DSAs with Primary Graft Failure and Survival
Multiple studies have demonstrated that DSAs are strongly associated with primary graft failure, such as primary graft rejection (GR) and primary poor graft function (PGF), and survival (Table 1), in haplo-HSCT and unrelated donor transplant modalities and in cord blood transplantation settings. However, these studies have failed to show these associations, which may be related to the small number of patients or heterogeneous transplant modalities [16, 17, 39, 44, 55, 56]. In addition to antibodies that target the HLA-A, HLA-B, HLA-C, and HLA-DRB1 loci, the association of DSAs that target other HLA loci with transplant outcomes remains unclear. Ciurea et al. investigated the presence of anti-HLA antibodies (Abs) pre-HSCT in 592 patients who underwent HLA-matched unrelated donor transplantation (MUDT). They demonstrated that the percentage of patients with anti-HLA Abs was 19.6% but that these antibodies were not reactive to donor HLA loci. Only 1.4% of the patients had DSAs, which were all directed against the HLA-DPB1 molecule. The cumulative incidence of graft failure (GF) was 2.7% in patients without DSAs compared with 37% in those with DSAs [42]. More recently, Lima et al. found that the presence of DSAs was a significant risk factor for GF in 303 patients who underwent MUDT, and of these, most DSAs were against HLA-DP directed primarily to public epitopes [17]. The association of DSAs that target other loci, such as DQA1, DPA1, DPB1, DRB3, DRB4, and DRB5, with GF and inferior survival has been suggested by several researchers [17, 39, 55, 56]. Therefore, prospective, multicenter, large-sample studies are warranted to confirm the above-mentioned findings.
Another issue is the optimal cutoff value of DSAs pre-HSCT that negatively affects hematopoietic engraftment. The currently available literature on the cutoff value for DSAs before transplantation includes several MFI values, such as 500, 1000, 2000, and 5000 [24, 41, 42, 46,47,48,49, 52, 57,58,59]. In a larger study that includes 345 patients, of whom 11.3% were DSA-positive, multivariate models showed that DSAs (MFI ≥ 10,000) were correlated with primary GR and inferior survival and that DSAs (MFI ≥ 2000) were strongly associated with primary PGF [58]. The differences in underlying diseases as well as transplant modality, conditioning regimen, and GVHD prophylaxis may account for the differences in the cutoff values of DSAs and primary GF reported in the current literature [56, 60,61,62,63]. Therefore, future studies should investigate the optimal cutoff value of DSAs pre-HSCT to determine the impact on outcomes in patients with different diseases who are treated with different HLA-mismatched transplant modalities.
More recently, a multicenter retrospective study from China showed that, for patients (n = 402) who underwent HLA-matched sibling donor transplantation, the presence of anti-HLA Abs before transplantation was an independent risk factor for delayed neutrophil engraftment (HR 1.42, p = 0.003), a higher incidence of CMV reactivation (HR 2.03, p = 0.009), and inferior overall survival (OS) at 180 days (HR 2.32, p = 0.042) [64]. Sadowska-Klasa et al. showed that the presence of anti-HLA recipient-specific antibodies (RSAs) could be associated with delayed platelet and red blood cell engraftment, transfusion refractoriness, and increased rates of transplantation-associated thrombotic microangiopathy in mismatched HCT recipients [55]. These two reports [55, 64] suggest that further studies are needed to investigate the effects of anti-HLA Abs and RSAs on clinical outcomes in HLA-mismatched allo-HSCT settings.
The Effects of DSAs on the Pathogenesis of Graft Failure
The pathogenesis of graft rejection and/or poor graft function caused by DSAs after allogeneic transplantation might be less understood than that after organ transplantation [65, 66]. On the basis of studies of antibody production by B cells in healthy humans, patients with autoimmune disease, and those who underwent organ transplantation [25, 65,66,67,68,69,70,71,72], the role of DSAs in graft failure in HSCT recipients could be proposed as follows: First, after the entry of allogeneic HLA antigens into recipients, antigen-presenting cells (APCs) can present HLA antigens to CD4+ naïve T cells. With the help of secondary signaling by CD80 and/or CD86 on APCs and CD28 on T cells, naïve CD4+ T cells are activated, after which they differentiate into follicular helper T (Tfh) cells. Bcl6 plays an important role in this process. The interaction between Tfh cells and naïve B cells via immunological synapses, which are composed of a number of receptors and ligands (e.g., CD28-B7, ICOS-ICOSL, CD40-CD40L, CD27-CD70, and LFA-1-ICAM-1), promotes the differentiation of naïve B cells into DSA-secreting cells, including memory B cells, plasmablasts, and plasma cells. Other molecules or cytokines, such as CXCL-13, IL-6, and the IL-6 receptor, as well as IL-21, also facilitate the conversion of Tfh cells to B cells. Second, the destruction of hematopoietic progenitor/stem cells and supporting cells, such as endothelial cells (ECs) and mesenchymal stem cells (MSCs), by DSAs may lead to graft rejection or poor graft function through three pathways: (i) antibody binding can cause direct complement-mediated cell lysis, (ii) antibody-dependent cellular cytotoxicity (ADCC), and (iii) phagocytosis by macrophages (Fig. 1).
The pathogenesis of graft failure by DSAs after HLA-mismatched allogeneic HSCT. APCs display HLA antigens to naïve CD4+ T cells and then promote their differentiation into T follicular (Tfh) cells in the germinal center. Tfh cells facilitate the differentiation of activated B cells into memory B cells, plasmablasts, and plasma cells that produce DSAs. High-affinity DSAs, or rather, complement-activating DSAs, activate NK cells through the FCGR and stimulate them to release effector cytokines, which can enhance the cytotoxicity of nearby monocytes and increase damage through ADCC. In addition, activated monocytes release cytokines to facilitate the recruitment of additional NK cells. DSAs can also activate the classical complement cascade, leading to the formation of the membrane attack complex (MAC) C5b–C9. This causes the lysis of hematopoietic progenitor/stem cells and supporting cells, such as endothelial cells (ECs) and mesenchymal stem cells (MSCs), which facilitates graft rejection or poor graft function
Recently, researchers at Peking University reported the exhaustion of quiescent CD34+ hematopoietic stem cells with increased reactive oxygen species (ROS) levels in patients with PGF [73]. In addition, dysfunctional bone marrow ECs and MSCs can also lead to PGF in patients who undergo allogeneic transplantation [74,75,76]. Unfortunately, whether DSAs can result in CD34+ hematopoietic stem cell exhaustion and EC and MSC dysfunction as well as the mechanism remain unclear, although a randomized trial demonstrated that prophylactic N-acetyl-L-cysteine can reduce PGF by improving ECs after haploidentical HSCT [77].
Strategies for DSA Desensitization
Presently, a number of approaches, such as blocking the function of B cells and plasma cells and removing or neutralizing antibodies in serum, have been successfully used for desensitization of DSAs [21, 23, 61]. However, current desensitization approaches often fail to deplete allo-specific memory B cells (Bmems) and long-lived plasma cells (LLPCs). Moreover, the complexity of the pathogenesis of primary GR and PGF caused by DSAs (Fig. 1) suggests that multiple novel approaches will likely be required for effective desensitization (Table 2).
Methods Targeting B Cells or Plasma Cells
Chen et al. reported that CTLA-4Ig can inhibit Bmem cell responses and enhance allograft survival in sensitized mouse recipients [78]. Kim et al. showed that, in allograft settings, ibrutinib could effectively suppress alloantibody responses through blocking BTK-BCR signaling pathways via a decrease in the numbers of B cells and short-lived PCs in the spleens of mice in a skin allograft model [79]. The role of ibrutinib in DSA desensitization was further confirmed by Han et al. in a cardiac transplantation mouse model [80]. These two studies suggest that Bruton’s tyrosine kinase antagonists could be potential agents for DSA desensitization. In addition, Webber et al. demonstrated that HLA-Fc fusion proteins can target DSA-producing cells, lyse these cells via complement-dependent cytotoxicity in vitro, and deplete the target cells in a mouse model. Their findings suggest that HLA-Fc might be a novel strategy for DSA desensitization [81].
In a pre-sensitized skin mouse model of islet allograft transplantation, Zhang et al. reported that the treatment of recipient mice with CD19 and B-cell maturation antigen (BCMA) chimeric antigen receptor (CAR) T cells (CART-19 and CART-BCMA) targeting Bmems and LLPCs can eliminate DSAs and ensure successful transplantation [27]. Clinically, in three multiple myeloma (MM) patients who received CAR-T-19 and CAR-BCMA, HLA alloantibodies decreased by 47–97% over the course of 12 months following CAR-T-cell infusion. This study suggested that immunotherapies targeting CD19 and BCMA represent promising desensitization strategies.
The effectiveness of daratumumab for DSA desensitization was reported by Li et al. [82]. Then Ibrahim et al. reported a patient with high-titer DSAs (MFI = 18,600) who failed to respond to a dose of rituximab and three sessions of therapeutic plasma exchange. Therefore, after intravenous administration of eight weekly doses of 16 mg/kg daratumumab, the DSAs decreased to an MFI of 2488 [83]. Data obtained from mouse models and clinical data suggest that desensitization strategies targeting CD38 and BCMA in plasma cells and CD19 in B cells might be novel methods for DSA desensitization, especially for DSA-positive transplant candidates who have CD38-positive, BCMA-positive, and/or CD19-positive hematological malignancies [82,83,84].
Considering the role of B cells and plasma cells in DSA production, the drugs currently used to treat B-cell or plasma cell malignancies could be potential approaches for DSA desensitization [85, 86]. These drugs include blinatumomab (a CD3-CD19 bispecific antibody), mosunetuzumab or glofitamab (CD3-CD20 bispecific antibodies), isatuximab (an anti-CD38 antibody), and indatuximab ravtansine (an anti-CD138 antibody) [85, 86]. Therefore, further pilot or prospective studies are needed to investigate the role of these agents in DSA desensitization.
Approaches Targeting Tfh Cells
As reported by others and by our group, Tfh cells are important for antibody production [87,88,89,90,91]. In vitro experiments have shown that targeting Tfh cells with sirolimus can inhibit their auxiliary function in assisting B cells [25]. In vivo clinical studies revealed that the overall response rates of DSA-positive transplant candidates treated with both sirolimus and rituximab and those of patients treated with either sirolimus or rituximab alone were 60%, 43.75%, and 30%, respectively. All 12 patients who were desensitized with both sirolimus and rituximab and subsequently received haploidentical transplantation achieved complete hematopoietic reconstitution without the onset of primary graft failure [26]. Therefore, targeting Tfh cells might represent a novel approach for DSA desensitization in allograft settings.
Multiple Tfh-related therapies for patients with autoimmune diseases have been approved or are currently being tested in clinical trials [87,88,89,90,91] and include the following: (i) olokizumab and sirukumab, which target the Tfh-related cytokines IL-21 and IL-6, respectively; (ii) tocilizumab and sarilumab, which target IL-6R; and (iii) methods that block costimulatory molecules, such as AMG557, abatacept, BI655064, and VIB4920/BG9588, which target ICOSL, CD28, CD40, and CD40L, respectively (Table 3). Therefore, pilot studies are needed to investigate the effectiveness of these approaches for DSA desensitization.
Combined Methods for DSA Desensitization
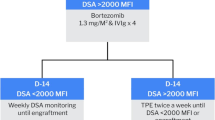
Our previous study showed that, in haploidentical HSCT based on immune tolerance induced by granulocyte colony-stimulating factor and anti-thymocyte globulin, a single dose of rituximab could effectively prevent the onset of primary PGF. However, DSA levels (MFI greater than 5000) have a negative impact on the efficiency of single-dose rituximab for desensitization. Therefore, combinations of different methods are needed, especially for those subjects with a DSA MFI greater than 5000 or 10,000.
In a study from MD Anderson, Ciurea et al. combined alternate plasmapheresis followed by rituximab and 1 g/kg IVIG with an irradiated, donor-derived buffy coat infused on day −1 [92]. The authors showed that the cumulative incidence of neutrophil engraftment, nonrelapse mortality (NRM), and survival were not significantly different between patients without DSAs and those with DSAs with an MFI up to 20,000, while patients with DSAs with an MFI > 20,000 had a greater rate of graft failure, greater NRM, and poorer outcomes. Moreover, compared with desensitization without a buffy coat, incorporation of a buffy coat infusion into the desensitization regimen increased the likelihood of neutrophil engraftment [short-term hematopoietic reconstruction (SHR) 2.09, p = 0.049]. This protocol was further confirmed by scholars from Saudi Arabia [93]. In another study, the effectiveness of desensitization protocols, including double-filtration plasmapheresis (DFPP) and rituximab, was reported [61]. Liu et al. demonstrated that all patients who are DSA-positive (n = 33) achieved hematopoietic reconstitution. The 3-year nonrelapse mortality (6.39% and 8.72%, p = 0.972) and overall survival (72.0% and 87.8%, p = 0.148) rates were comparable between patients in the DSA cohort and those in the negative control cohort. This study indicated that DFPP and rituximab were effective for desensitization of DSAs [61].
Overall, the available literature supports the notion that, for patients with a high level of DSAs (MFI greater than 5000), DSA desensitization using combinations of different methods may be more effective than desensitization using a single approach (Table 2) [22, 60, 61, 63, 94,95,96,97,98]. Unfortunately, many questions remain unanswered (Box 1). For example, we still do not know the optimal combination of different desensitization methods or whether the dose of each agent should be modulated in the combination protocol compared with a single agent for desensitization. In addition, for patients with DSAs that target HLA-I loci or HLA-II loci alone or in combination, should different desensitization protocols be used in different settings?
Future Directions
In HLA-mismatched allogeneic transplantation settings, DSA is an important variable for optimal donor selection [99, 100]. Unfortunately, current desensitization strategies elicit a poor response in some DSA-positive patients, especially those with an MFI greater than 10,000 [22, 60, 61, 94,95,96,97,98]. First, the mechanisms underlying the onset of DSAs and the pathogenesis of graft failure should be further elucidated. For example, for patients who are refractory to desensitization, defining the characteristics of Tfh cells, B cells, and plasma cells might reveal the underlying mechanism of refractory disease. Second, differences in the cutoff values of DSAs for initiating desensitization and differences in the approaches used for DSA elimination at different transplant centers increase the difficulty in establishing a protocol that is suitable for all DSA-positive HSCT candidates. Therefore, prospective, multicenter, large-sample studies are warranted to establish standard DSA desensitization protocols. Third, current desensitization methods focus on transplant recipients with DSAs before HSCT; however, the kinetics of DSAs after transplantation and the effects of DSAs on outcomes remain poorly understood [101]. Thus, future studies should evaluate the profiles of DSAs after transplantation and the way DSA-positive transplant recipients should be treated. In summary, multiple issues in the field of DSA desensitization should be addressed in the future (Box 1). These unanswered questions will enable the desensitization of DSAs and enhance the hematopoietic recovery of patients who undergo HLA-mismatched allogeneic transplantation.
Box 1. Basic and Answerable Questions Regarding DSA Desensitization in Patients who Underwent HLA-Mismatched Allogeneic Transplantation
-
How can the underlying mechanism be elucidated in transplant recipients who have no anti-HLA antibodies including those with several risk factors, such as pregnancy and transfusion?
-
What is the role of C1q binding to DSAs in other transplant modalities, except for in patients who receive haploidentical allografts?
-
What are the effects of non-DSAs pre-HSCT on transplant outcomes?
-
What are the kinetics of DSAs and non-DSAs after HLA-mismatched allograft transplantation and their association with transplant outcomes?
-
What is the optimal cutoff value for the DSA level for desensitization? Are there different DSA cutoff values for desensitization among different transplant modalities?
-
What is the optimal combination of different desensitization strategies for patients with high levels of DSAs?
-
How can individualized desensitization therapy be administered according to the individual’s DSA level?
-
Which biomarkers could predict the effectiveness of DSA desensitization strategies?
Data Availability
Data sharing is not applicable to this article.
References
Ali H, Bacigalupo A. 2024 update on allogeneic hematopoietic stem cell transplant for myelofibrosis: A review of current data and applications on risk stratification and management. Am J Hematol. 2024;99(5):938–45.
Bai L, Zhang ZX, Hu GH, Cheng YF, Suo P, Wang Y, et al. Long-term follow-up of haploidentical haematopoietic stem cell transplantation in paediatric patients with high-risk acute myeloid leukaemia: Report from a single centre. Br J Haematol. 2023;204(2):585–94.
Berning P, Schmitz N, Ngoya M, Finel H, Boumendil A, Wang F, et al. Allogeneic hematopoietic stem cell transplantation for NK/T-cell lymphoma: An international collaborative analysis. Leukemia. 2023;37(7):1511–20.
Elmakaty I, Saglio G, Al-Khabori M, Elsayed A, Elsayed B, Elmarasi M, et al. The contemporary role of hematopoietic stem cell transplantation in the management of chronic myeloid leukemia: Is it the same in all settings? Cancers. 2024;16(4).
Shang Q, Bai L, Cheng Y, Suo P, Hu G, Yan C, et al. Outcomes and prognosis of haploidentical haematopoietic stem cell transplantation in children with FLT3-ITD mutated acute myeloid leukaemia. Bone Marrow Transplantation. 2024.
Wu L, Wu Y, Shi J, Lai X, Zhao Y, Liu L, et al. Survival and late mortality among patients who survived disease-free for 2 years after stem cell transplantation. Br J Haematol. 2023;202(3):608–22.
Xu Z-L, Xu L-P, Zhang Y-C, Zhou Y-H, Jiang E-L, Zhang J-P, et al. The outcome and predictive model of allogeneic hematopoietic stem cell transplantation among elderly patients with severe aplastic anemia from the Chinese Blood and Marrow Transplant Registry Group. Haematologica. 2024.
Chang YJ, Luznik L, Fuchs EJ, Huang XJ. How do we choose the best donor for T-cell-replete, HLA-haploidentical transplantation? J Hematol Oncol. 2016;9:35.
Gale RP, Eapen M. Who is the best alternative allotransplant donor? Bone Marrow Transplant. 2015;50(S2):S40–2.
Nagler A, Labopin M, Mielke S, Passweg J, Blaise D, Gedde-Dahl T, et al. Matched related versus unrelated versus haploidentical donors for allogeneic transplantation in AML patients achieving first complete remission after two induction courses: A study from the ALWP/EBMT. Bone Marrow Transplant. 2023;58(7):791–800.
Wang Y, Wu DP, Liu QF, Xu LP, Liu KY, Zhang XH, et al. Donor and recipient age, gender and ABO incompatibility regardless of donor source: Validated criteria for donor selection for haematopoietic transplants. Leukemia. 2017;32(2):492–8.
Xu LP, Wang SQ, Ma YR, Gao SJ, Cheng YF, Zhang YY, et al. Who is the best haploidentical donor for acquired severe aplastic anemia? Experience from a multicenter study. J Hematol Oncol. 2019;12(1):87.
Passweg JR, Baldomero H, Ciceri F, Corbacioglu S, de la Cámara R, Dolstra H, et al. Hematopoietic cell transplantation and cellular therapies in Europe 2021. The second year of the SARS-CoV-2 pandemic. A Report from the EBMT Activity Survey. Bone Marrow Transplantation. 2023;58(6):647–658.
Chang Y-J, Pei X-Y, Huang X-J. Haematopoietic stem-cell transplantation in China in the era of targeted therapies: Current advances, challenges, and future directions. Lancet Haematology. 2022;9(12):e919–29.
CIBMTR. The US summary slides—HCTtrends and survival data. 2022. [Available from: https://cibmtr.org/CIBMTR/Resources/Summary-Slides-Reports.
Bramanti S, Calafiore V, Longhi E, Mariotti J, Crespiatico L, Sarina B, et al. Donor-specific anti-HLA antibodies in haploidentical stem cell transplantation with post-transplantation cyclophosphamide: Risk of graft failure, poor graft function, and impact on outcomes. Biol Blood Marrow Transplant. 2019;25(7):1395–406.
Lima ACM, Getz J, do Amaral GB, Loth G, Funke VAM, Nabhan SK, et al. Donor-specific HLA antibodies are associated with graft failure and delayed hematologic recovery after unrelated donor hematopoietic cell transplantation. Transplantation and Cellular Therapy. 2023;29(8):493.e491–493.e410.
Ozdemir ZN, Civriz BS. Graft failure after allogeneic hematopoietic stem cell transplantation. Transfus Apheres Sci. 2018;57(2):163–7.
Huang XJ. Overcoming graft failure after haploidentical transplantation: Is this a possibility? Best Pract Res Clin Haematol. 2021;34(1): 101255.
Barge AJ, Johnson G, Witherspoon R, Torok-Storb B. Antibody-mediated marrow failure after allogeneic bone marrow transplantation. Blood. 1989;74(5):1477–80.
Chang Y-J, Xu L-P, Wang Y, Zhang X-H, Chen H, Chen Y-H, et al. Rituximab for desensitization during HLA-mismatched stem cell transplantation in patients with a positive donor-specific anti-HLA antibody. Bone Marrow Transplant. 2020;55(7):1326–36.
Ciurea SO, Al Malki MM, Kongtim P, Zou J, Aung FM, Rondon G, et al. Treatment of allosensitized patients receiving allogeneic transplantation. Blood Adv. 2021;5(20):4031–43.
Ciurea SO, Cao K, Fernandez-Vina M, Kongtim P, Malki MA, Fuchs E, et al. The European Society for Blood and Marrow Transplantation (EBMT) Consensus Guidelines for the Detection and Treatment of Donor-Specific Anti-HLA Antibodies (DSA) in Haploidentical Hematopoietic Cell Transplantation. Bone Marrow Transplant. 2018;53(5):521–34.
Zheng X, Yan H, Han D, Ding L, Zhu L, Liu J, et al. Successful desensitization of high level donor-specific anti-HLA antibody in patients with hematological diseases receiving haploidentical allografts. Ann Hematol. 2022;101(8):1777–83.
Ma N, Wu WB, Zhao XY, Xu LP, Zhang XH, Wang Y, et al. Targeting T(FH) cells is a novel approach for donor-specific antibody desensitization of allograft candidates: An in vitro and in vivo study. Haematologica. 2024;109(4):1233–46.
Ma N, Wang ZD, Sun YQ, Yan CH, Wang FR, Mo XD, et al. Effect of sirolimus combined with anti-CD20 monoclonal antibody desensitization on the prognosis of patients underwent haploidentical stem cell transplantation. Zhonghua Yi Xue Za Zhi. 2024;104(11):843–9.
Zhang Z, Markmann C, Yu M, Agarwal D, Rostami S, Wang W, et al. Immunotherapy targeting B cells and long-lived plasma cells effectively eliminates pre-existing donor-specific allo-antibodies. Cell Rep Med. 2023;4(12): 101336.
Middelburg RA, Porcelijn L, Lardy N, Briët E, Vrielink H. Prevalence of leucocyte antibodies in the Dutch donor population. Vox Sang. 2010;100(3):327–35.
Endres RO, Kleinman SH, Carrick DM, Steele WR, Wright DJ, Norris PJ, et al. Identification of specificities of antibodies against human leukocyte antigens in blood donors. Transfusion. 2010;50(8):1749–60.
Kakaiya RM, Triulzi DJ, Wright DJ, Steele WR, Kleinman SH, Busch MP, et al. Prevalence of HLA antibodies in remotely transfused or alloexposed volunteer blood donors. Transfusion. 2010;50(6):1328–34.
De Clippel D, Baeten M, Torfs A, Emonds MP, Feys HB, Compernolle V, et al. Screening for HLA antibodies in plateletpheresis donors with a history of transfusion or pregnancy. Transfusion. 2014;54(12):3036–42.
Masson E, Vidal C, Deschamps M, Bongain S, Thevenin C, Dupont I, et al. Incidence and risk factors of anti-HLA immunization after pregnancy. Hum Immunol. 2013;74(8):946–51.
Triulzi DJ, Kleinman S, Kakaiya RM, Busch MP, Norris PJ, Steele WR, et al. The effect of previous pregnancy and transfusion on HLA alloimmunization in blood donors: Implications for a transfusion-related acute lung injury risk reduction strategy. Transfusion. 2009;49(9):1825–35.
Akgul SU, Ciftci HS, Temurhan S, Caliskan Y, Bayraktar A, Tefik T, et al. Association between HLA antibodies and different sensitization events in renal transplant candidates. Transpl Proc. 2017;49(3):425–9.
Hung S-Y, Lin T-M, Chang M-Y, Wang H-H, Lee Y-C, Ho L-C, et al. Risk factors of sensitization to human leukocyte antigen in end-stage renal disease patients. Hum Immunol. 2014;75(6):531–5.
Ling M, Marfo K, Masiakos P, Aljanabi A, Lindower J, Glicklich D, et al. Pretransplant anti-HLA-Cw and anti-HLA-DP antibodies in sensitized patients. Hum Immunol. 2012;73(9):879–83.
Gladstone DE, Zachary AA, Fuchs EJ, Luznik L, Kasamon YL, King KE, et al. Partially mismatched transplantation and human leukocyte antigen donor-specific antibodies. Biol Blood Marrow Transplant. 2013;19(4):647–52.
Ciurea SO, Thall PF, Milton DR, Barnes TH, Kongtim P, Carmazzi Y, et al. Complement-binding donor-specific anti-HLA antibodies and risk of primary graft failure in hematopoietic stem cell Transplantation. Biol Blood Marrow Transplant. 2015;21(8):1392–8.
Lima ACM, Bonfim C, Getz J, Dornelles LN, do Amaral GB, Petterle RR, et al. The impact of donor‐specific anti‐human leukocyte antigen antibodies in salvage haploidentical hematopoietic cell transplantation with posttransplant cyclophosphamide in patients with nonmalignant disorders. HLA. 2021;97(6):493–504.
Carter M, Taniguchi M, Yang D, Arslan S, Shouse G, Ali H, et al. Donor-specific HLA antibodies associate with chronic graft-versus-host disease in haploidentical hematopoietic stem cell transplantation with post-transplant cyclophosphamide. Bone Marrow Transplant. 2021;57(1):134–6.
Lima ACM, Bonfim C, Getz J, do Amaral GB, Petterle RR, Loth G, et al. Untreated donor-specific HLA antibodies are associated with graft failure and poor survival after haploidentical transplantation with post-transplantation cyclophosphamide in pediatric patients with nonmalignant disorders. Transplantation and Cellular Therapy. 2022;28(10):698.e691–698.e611.
Ciurea SO, Thall PF, Wang X, Wang SA, Hu Y, Cano P, et al. Donor-specific anti-HLA Abs and graft failure in matched unrelated donor hematopoietic stem cell transplantation. Blood. 2011;118(22):5957–64.
Takanashi M, Atsuta Y, Fujiwara K, Kodo H, Kai S, Sato H, et al. The impact of anti-HLA antibodies on unrelated cord blood transplantations. Blood. 2010;116(15):2839–46.
Fuji S, Oshima K, Ohashi K, Sawa M, Saito T, Eto T, et al. Impact of pretransplant donor-specific anti-HLA antibodies on cord blood transplantation on behalf of the Transplant Complications Working Group of Japan Society for Hematopoietic Cell Transplantation. Bone Marrow Transplant. 2019;55(4):722–8.
Detrait M, Dubois V, Sobh M, Morisset S, Tedone N, Labussière H, et al. Impact of anti-HLA antibodies on allogeneic hematopoietic stem cell transplantation outcomes after reduced-intensity conditioning regimens. Exp Hematol. 2012;40(10):792–9.
Yoshihara S, Maruya E, Taniguchi K, Kaida K, Kato R, Inoue T, et al. Risk and prevention of graft failure in patients with preexisting donor-specific HLA antibodies undergoing unmanipulated haploidentical SCT. Bone Marrow Transplant. 2011;47(4):508–15.
Lv M, Zhai S-Z, Wang Y, Xu L-P, Zhang X-H, Chen H, et al. Class I and II human leukocyte antibodies in pediatric haploidentical allograft candidates: Prevalence and risk factors. Bone Marrow Transplant. 2019;54(8):1287–94.
Cao LQ, Lv M, Xu LP, Zhang XH, Chen H, Chen YH, et al. Prevalence and risk factors of having antibodies to class I and II human leukocyte antigens in older haploidentical allograft candidates. Sci Rep. 2020;10(1):2367.
Ciurea SO, de Lima M, Cano P, Korbling M, Giralt S, Shpall EJ, et al. High risk of graft failure in patients with anti-HLA antibodies undergoing haploidentical stem-cell transplantation. Transplantation. 2009;88(8):1019–24.
Ferrandiz I, Congy-Jolivet N, Del Bello A, Debiol B, Trébern-Launay K, Esposito L, et al. Impact of early blood transfusion after kidney transplantation on the incidence of donor-specific anti-LA antibodies. Am J Transplant. 2016;16(9):2661–9.
Thiyagarajan UM, Bagul A, Frost J, Horsburgh T, Nicholson ML. Role of human leukocyte antigen, donor-specific antibodies, and their impact in renal transplantation. Transpl Proc. 2012;44(5):1231–5.
Waiser J, Duerr M, Budde K, Rudolph B, Wu K, Bachmann F, et al. Treatment of acute antibody-mediated renal allograft rejection with cyclophosphamide. Transplantation. 2017;101(10):2545–52.
Ma N, Guo JP, Zhao XY, Xu LP, Zhang XH, Wang Y, et al. Prevalence and risk factors of antibodies to HLA according to different cut-off values of mean fluorescence intensity in haploidentical allograft candidates: A prospective study of 3805 subjects. Hla. 2022;100(4):312–24.
Krummey SM, Gareau AJ. Donor specific HLA antibody in hematopoietic stem cell transplantation: Implications for donor selection. Front Immunol. 2022;13: 916200.
Sadowska-Klasa A, Dukat-Mazurek A, Zielińska H, Dębska-Zielkowska J, Piekarska A, Moszkowska G, et al. Incidence and role of recipient-specific antibodies in allogeneic hematopoietic cell transplantation from mismatched related donors. Transplantation and Cellular Therapy. 2024;30(1):99.e91-99.e10.
Jo T, Arai Y, Hatanaka K, Ishii H, Ono A, Matsuyama N, et al. Adverse effect of donor-specific anti-human leukocyte antigen (HLA) antibodies directed at HLA-DP/-DQ on engraftment in cord blood transplantation. Cytotherapy. 2023;25(4):407–14.
Cutler C, Kim HT, Sun L, Sese D, Glotzbecker B, Armand P, et al. Donor-specific anti-HLA antibodies predict outcome in double umbilical cord blood transplantation. Blood. 2011;118(25):6691–7.
Chang YJ, Zhao XY, Xu LP, Zhang XH, Wang Y, Han W, et al. Donor-specific anti-human leukocyte antigen antibodies were associated with primary graft failure after unmanipulated haploidentical blood and marrow transplantation: A prospective study with randomly assigned training and validation sets. J Hematol Oncol. 2015;8:84.
Spellman S, Bray R, Rosen-Bronson S, Haagenson M, Klein J, Flesch S, et al. The detection of donor-directed, HLA-specific alloantibodies in recipients of unrelated hematopoietic cell transplantation is predictive of graft failure. Blood. 2010;115(13):2704–8.
Liu J, Zhao XY, Xu LP, Zhang XH, Wang Y, Mo XD, et al. The impact of donor-specific anti-HLA antibody levels on primary poor graft function and graft rejection in rituximab desensitized haploidentical stem cell transplantation. HLA. 2024;103(1): e15300.
Liu L, Ji X, Zhu P, Yang L, Shi J, Zhao Y, et al. Double filtration plasmapheresis combined with rituximab for donor-specific antibody desensitization in haploidentical haematopoietic stem cell transplantation. Br J Haematol. 2023;203(5):829–39.
Bramanti S, Nocco A, Mauro E, Milone G, Morabito L, Sarina B, et al. Desensitization with plasma exchange in a patient with human leukocyte antigen donor-specific antibodies before T-cell–replete haploidentical transplantation. Transfusion. 2016;56(5):1096–100.
Zhu J, Wang Q, Liu Y, Dong Y, Liang Z, Yin Y, et al. High-dose immunoglobulin intervention as an effective and simple strategy for donor specific anti-HLA antibody desensitization in haploidentical transplant. Int Immunopharmacol. 2023;120: 110299.
Wei X, Chang Y, Zhu X, Hu X, Guo R, Zhang Y, et al. The impact of pre-transplant anti-HLA antibodies in transplants from HLA-identical sibling donors: A multicenter study. HLA. 2024;103(1): e15286.
Mohammed MT, Cai S, Hanson BL, Zhang H, Clement RL, Daccache J, et al. Follicular T cells mediate donor-specific antibody and rejection after solid organ transplantation. Am J Transplant. 2021;21(5):1893–901.
Heeger PS, Haro MC, Jordan S. Translating B cell immunology to the treatment of antibody-mediated allograft rejection. Nat Rev Nephrol. 2024;20(4):218–32.
Zhang H, Cavazzoni CB, Podesta MA, Bechu ED, Ralli G, Chandrakar P, et al. IL-21-producing effector Tfh cells promote B cell alloimmunity in lymph nodes and kidney allografts. JCI Insight. 2023;8(20): e169793.
Short S, Lewik G, Issa F. An immune atlas of T cells in transplant rejection: Pathways and therapeutic opportunities. Transplantation. 2023;107(11):2341–52.
Cano-Romero FL, Laguna Goya R, Utrero-Rico A, Gómez-Massa E, Arroyo-Sánchez D, Suárez-Fernández P, et al. Longitudinal profile of circulating T follicular helper lymphocytes parallels anti-HLA sensitization in renal transplant recipients. Am J Transplant. 2019;19(1):89–97.
He J, Tsai Louis M, Leong Yew A, Hu X, Ma Cindy S, Chevalier N, et al. Circulating precursor CCR7loPD-1hi CXCR5+ CD4+ T cells indicate Tfh cell activity and promote antibody responses upon antigen reexposure. Immunity. 2013;39(4):770–81.
Morita R, Schmitt N, Bentebibel S-E, Ranganathan R, Bourdery L, Zurawski G, et al. Human Blood CXCR5+CD4+ T cells are counterparts of T follicular cells and contain specific subsets that differentially support antibody secretion. Immunity. 2011;34(1):108–21.
Walker LSK. The link between circulating follicular helper T cells and autoimmunity. Nat Rev Immunol. 2022;22(9):567–75.
Kong Y. Poor graft function after allogeneic hematopoietic stem cell transplantation—an old complication with new insights☆. Semin Hematol. 2019;56(3):215–20.
Lyu ZS, Cao XN, Wen Q, Mo XD, Zhao HY, Chen YH, et al. Autophagy in endothelial cells regulates their haematopoiesis-supporting ability. EBioMedicine. 2020;53: 102677.
Song Y, Zhao H-Y, Lyu Z-S, Cao X-N, Shi M-M, Wen Q, et al. Dysfunctional bone marrow mesenchymal stem cells in patients with poor graft function after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2018;24(10):1981–9.
Shi M-M, Kong Y, Song Y, Sun Y-Q, Wang Y, Zhang X-H, et al. Atorvastatin enhances endothelial cell function in posttransplant poor graft function. Blood. 2016;128(25):2988–99.
Wang Y, Kong Y, Zhao HY, Zhang YY, Wang YZ, Xu LP, et al. Prophylactic NAC promoted hematopoietic reconstitution by improving endothelial cells after haploidentical HSCT: A phase 3, open-label randomized trial. BMC Med. 2022;20(1):140.
Chen J, Wang Q, Yin D, Vu V, Sciammas R, Chong AS. Cutting edge: CTLA-4Ig inhibits memory B cell responses and promotes allograft survival in sensitized recipients. J Immunol. 2015;195(9):4069–73.
Kim I, Wu G, Chai N-n, Klein AS, Jordan S. Ibrutinib suppresses alloantibody responses in a mouse model of allosensitization. Transplant Immunology. 2017;45:59–64.
Han F, Shi X, Liao T, Zhang W, Ma M, Leng Q, et al. Bruton’s tyrosine kinase ablation inhibits B cell responses and antibody production for the prevention of chronic rejection in cardiac transplantation. Clin Immunol. 2024;261: 109941.
Webber AM, Bradstreet TR, Wang X, Guo H, Nelson CA, Fremont DH, et al. Antigen-guided depletion of anti-HLA antibody–producing cells by HLA-Fc fusion proteins. Blood. 2022;140(16):1803–15.
Li X, Zhu H, Sui T, Zhao X, Deng Q. A case of daratumumab-induced significant decrease in donor-specific HLA antibodies and remission induction before haploidentical stem cell transplantation in a refractory B-ALL patient. Cell Transplant. 2022;31:9636897221132502.
Ibrahim U, Keyzner A. Daratumumab for donor-specific anti-HLA antibody desensitization in a case of HLA-mismatched allogeneic stem cell transplantation. Hematology, Transfusion and Cell Therapy. 2023;45(4):510–2.
Kunvarjee B, Contreras Yametti GP, Blouin AG, Linder GE, Borge PD, Maryamchik E, et al. Donor-specific antibody desensitization with daratumumab prior to haematopoietic cell transplant for sickle cell disease: A case report. Br J Haematol. 2024;204(4):1540–4.
Abou Dalle I, Dulery R, Moukalled N, Ricard L, Stocker N, El-Cheikh J, et al. Bi- and tri-specific antibodies in non-Hodgkin lymphoma: Current data and perspectives. Blood Cancer J. 2024;14(1):23.
Cipkar C, Chen C, Trudel S. Antibodies and bispecifics for multiple myeloma: Effective effector therapy. Hematology Am Soc Hematol Educ Program. 2022;2022(1):163–72.
Feist E, Fatenejad S, Grishin S, Korneva E, Luggen ME, Nasonov E, et al. Olokizumab, a monoclonal antibody against interleukin-6, in combination with methotrexate in patients with rheumatoid arthritis inadequately controlled by tumour necrosis factor inhibitor therapy: Efficacy and safety results of a randomised controlled phase III study. Ann Rheum Dis. 2022;81(12):1661–8.
Takeuchi T, Yamanaka H, Harigai M, Tamamura R, Kato Y, Ukyo Y, et al. Sirukumab in rheumatoid arthritis refractory to sulfasalazine or methotrexate: A randomized phase 3 safety and efficacy study in Japanese patients. Arthritis Res Ther. 2018;20(1):42.
Rech J, Tascilar K, Hagen M, Kleyer A, Manger B, Schoenau V, et al. Abatacept inhibits inflammation and onset of rheumatoid arthritis in individuals at high risk (ARIAA): A randomised, international, multicentre, double-blind, placebo-controlled trial. Lancet (London, England). 2024;403(10429):850–9.
Cope AP, Jasenecova M, Vasconcelos JC, Filer A, Raza K, Qureshi S, et al. Abatacept in individuals at high risk of rheumatoid arthritis (APIPPRA): A randomised, double-blind, multicentre, parallel, placebo-controlled, phase 2b clinical trial. Lancet (London, England). 2024;403(10429):838–49.
Lu J, Wu J, Xia X, Peng H, Wang S. Follicular helper T cells: potential therapeutic targets in rheumatoid arthritis. Cellular and molecular life sciences : CMLS. 2021;78(12):5095–106.
Ciurea SO, Thall PF, Milton DR, Barnes TH, Kongtim P, Carmazzi Y, et al. Complement-binding donor-specific anti-HLA antibodies and risk of primary graft failure in hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2015;21(8):1392–8.
Altareb M, Al-Awwami M, Alfraih F, Alhayli S, Ahmed SO, Shaheen M, et al. Incidence and significance of donor-specific antibodies in haploidentical stem cell transplantation. Bone Marrow Transplant. 2023;58(6):680–6.
Cochran H, Slade M, Gao F, Godbole S, Pruitt A, De Togni E, et al. Pretransplant desensitization of donor-specific anti-HLA antibodies with plasmapheresis and immunoglobulin produces equivalent outcomes to patients with no donor specific antibodies in haploidentical hematopoietic cell transplant. Res Sq. 2024.
Bailen R, Alenda R, Herruzo-Delgado B, Acosta-Fleitas C, Valles A, Esquirol A, et al. Results of haploidentical transplant in patients with donor-specific antibodies: A survey on behalf of the Spanish Group of Hematopoietic Transplant and Cell Therapy. Front Immunol. 2023;14:1165759.
Anurathapan U, Hongeng S, Pakakasama S, Songdej D, Sirachainan N, Pongphitcha P, et al. Hematopoietic stem cell transplantation for severe thalassemia patients from haploidentical donors using a novel conditioning regimen. Biol Blood Marrow Transplant. 2020;26(6):1106–12.
Choe H, Gergis U, Hsu J, Phillips A, Shore T, Christos P, et al. Bortezomib and immune globulin have limited effects on donor-specific HLA antibodies in haploidentical cord blood stem cell transplantation: Detrimental effect of persistent haploidentical donor-specific HLA antibodies. Biol Blood Marrow Transplant. 2019;25(2):e60–4.
Shen Y, Zhang L, Zhang X, Zhang T, Jiang E, Feng S, et al. Treatment with the combination of rituximab and intravenous γ globulin is effective in promoting engraftment in donor-specific antibody positive patients receiving myeloablative conditioning haploidentical stem cell transplantation. Transplantation and cellular therapy. 2023;29(8):514.e511-514.e516.
Zhang XH, Chen J, Han MZ, Huang H, Jiang EL, Jiang M, et al. The consensus from The Chinese Society of Hematology on indications, conditioning regimens and donor selection for allogeneic hematopoietic stem cell transplantation: 2021 update. J Hematol Oncol. 2021;14(1):145.
Ciurea SO, Al Malki MM, Kongtim P, Fuchs EJ, Luznik L, Huang XJ, et al. The European Society for Blood and Marrow Transplantation (EBMT) consensus recommendations for donor selection in haploidentical hematopoietic cell transplantation. Bone Marrow Transplant. 2020;55(1):12–24.
Wang L, Ji K, Chen L, Li Y, Zhu W, Yuan X, et al. Posttransplant de novo DSA and NDSA affect GvHD, OS, and DFS after haplo-HSCT in patients without pre-existing HLA antibodies of hematological malignancies. Front Immunol. 2022;13:1047200.
Funding
This work was supported (in part) by the Beijing Municipal Science and Technology Commission (No. Z181100009618032). No funding or sponsorship was received for the publication of this article.
Author information
Authors and Affiliations
Contributions
Ying-Jun Chang designed the study; Ying-Jun Chang, Yang Zhou, and Yu-Lun Chen conceived the project and drafted the manuscript; Yang Zhou, Yu-Lun Chen, Xi-Yi Huang, and Ying-Jun Chang contributed to data interpretation and manuscript preparation. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Yang Zhou, Yu-Lun Chen, Xi-Yi Huang, and Ying-Jun Chang confirm that they have no competing interests to declare.
Ethical Approval
This article is based on previously conducted research and does not contain any new studies with animals or human participants carried out by any of the authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zhou, Y., Chen, YL., Huang, XY. et al. Desensitization Strategies for Donor-Specific Antibodies in HLA-Mismatched Stem Cell Transplantation Recipients: What We Know and What We Do Not Know. Oncol Ther (2024). https://doi.org/10.1007/s40487-024-00283-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40487-024-00283-6