Abstract
Background
Poor graft function (PGF) or prolonged isolated thrombocytopenia (PT), which are characterized by pancytopenia or thrombocytopenia, have become serious complications after allogeneic hematopoietic stem cell transplantation (allo-HSCT). Our previous single-arm trial suggests that N-acetyl-L-cysteine (NAC) prophylaxis reduced PGF or PT after allo-HSCT. Therefore, an open-label, randomized, phase 3 trial was performed to investigate the efficacy and tolerability of NAC prophylaxis to reduce PGF or PT after allo-HSCT.
Methods
A phase 3, open-label randomized trial was performed. Based on the percentage of CD34+VEGFR2 (CD309)+ endothelial cells (ECs) in bone marrow (BM) detected by flow cytometry at 14 days before conditioning, patients aged 15 to 60 years with acute leukemia undergoing haploidentical HSCT were categorized as low-risk (EC ≥ 0.1%) or high-risk (EC < 0.1%); patients at high risk were randomly assigned (2:1) to receive NAC prophylaxis or nonprophylaxis. The primary endpoint was PGF and PT incidence at +60 days post-HSCT.
Results
Between April 18, 2019, and June 24, 2021, 120 patients with BM EC <0.1% were randomly assigned for NAC (group A, N = 80) or nonprophylaxis (group B, N = 40), and 105 patients with EC≥0.1% (group C) were also analyzed. The +60 days incidence of PGF and PT was 7.5% (95% CI, 1.7 to 13.3%) and 22.5% (95% CI, 9.1 to 35.9%) in group A and group B (hazard ratio, 0.317; 95% CI, 0.113 to 0.890; P = 0.021) and 11.4% (95% CI, 5.2 to 17.6%) in group C (hazard ratio, 0.643; 95% CI, 0.242 to 1.715; P = 0.373). Consistently, NAC prophylaxis gradually improved BM ECs and CD34+ cells in group A, whereas reduced their reactive oxygen species (ROS) levels post-HSCT. Within 60 days post-HSCT, the most common grade 3 to 5 adverse events for the NAC and control groups were infections (19/80 [24%] vs. 10/40 [25%]) and gastrointestinal adverse events (16/80 [20%] vs. 7/40 [18%]). There were no treatment-related deaths.
Conclusions
N-Acetyl-L-cysteine prophylaxis can prevent the occurrence of poor hematopoietic function and is well tolerated in haploidentical HSCT. It may offer a potential pathogenesis-oriented therapeutic approach for patients with poor hematopoietic function.
Trial registration
This trial was registered at ClinicalTrials.gov as #NCT03967665.
Similar content being viewed by others
Background
Rapid and stable hematopoiesis recovery is a prerequisite for systemic and successful therapy in cancer patients [1, 2]. Moreover, poor hematopoietic function is a common feature of patients with bone marrow (BM) failure diseases, such as poor graft function (PGF) or prolonged isolated thrombocytopenia (PT) after allogeneic hematopoietic stem cell transplantation (allo-HSCT) [3,4,5,6,7,8,9], aplastic anemia [10, 11], and myelodysplastic syndromes [12,13,14]. Consequently, it is imperative to investigate how to promote hematopoiesis recovery in patients with poor hematopoietic function.
The specialized BM microenvironment is critical for the regulation of hematopoietic stem cells (HSCs) [15,16,17,18,19]. As a crucial element of the BM microenvironment, accumulating evidence indicates that endothelial cells (ECs) play essential roles in regulating hematopoiesis [20,21,22,23,24,25]. With the rapid development of haploidentical-HSCT (haplo-HSCT), poor hematopoietic function including PGF and PT [3,4,5,6,7,8,9], which is characterized by pancytopenia or thrombocytopenia, has become a serious threat after allo-HSCT because of the increased risk of infections and bleeding, hospitalization, even with worse health-related quality-of-life. Recently, our serial studies demonstrated that reduced and dysfunctional BM ECs, which are characterized by increased reactive oxygen species (ROS), induce the exhaustion of successfully engrafted donor HSCs, ultimately leading to the occurrence of poor hematopoietic function after allo-HSCT [3,4,5,6,7]. Therefore, BM EC dysfunction is the underlying pathogenesis in patients with poor hematopoietic function [3,4,5,6,7]. As an ROS scavenger, N-acety-L-cysteine (NAC) is widely used as an antioxidant and a mucolytic drug without significant side effects. NAC could enhance defective hematopoiesis by repairing the dysfunctional BM ECs of patients with PGF or PT in vitro [4, 7].
Considerable studies reported that the level of CD34+CD309+ EC detected by flow cytometry is a well-established prediction marker to identify patients at increased cardiovascular risk [26, 27]. Our recent single-arm trial [5] identified that BM CD34+CD309+ EC < 0.1% pre-haplo-HSCT is an independent risk factor for the occurrence of PGF or PT. Moreover, prophylactic oral NAC reduced the incidence of PGF or PT in EC < 0.1% group by improving BM ECs [5].
Therefore, we designed a phase 3, open-label randomized trial to validate the single-arm findings and to support the logical theory of novel BM microenvironment-directed therapies to promote hematopoietic reconstitution in patients with poor hematopoietic function.
Methods
Study design and participants
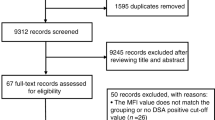
This phase 3, open-label randomized trial was performed at Peking University People’s Hospital between April 2019 and June 2021. Consecutive patients with acute leukemia (AL) undergoing first HSCT from haploidentical donors were eligible if they met the following criteria: (1) 15 to 60 years old with Eastern Cooperative Oncology Group (ECOG) performance status 0 to 2, (2) complete remission (CR) before HSCT, and (3) based on the percentage of BM ECs detected by flow cytometry at 14 days before conditioning (−24 days; detected by the same BM sample for morphology examination), patients were categorized as low-risk (EC ≥ 0.1%) or high-risk (EC < 0.1%); high-risk patients were randomly assigned (Fig. 1a). The AL diagnosis and CR identification was according to WHO criteria. Patients were excluded from the study if they had hypersensitivity to NAC, bronchial asthma, ejection fraction < 50%, creatinine ≥ 1.5 times the upper limit of normal (ULN), and total bilirubin or aminotransferase ≥ 2 times the ULN (detailed information on eligibility criteria is available in the study protocol, see Additional file 2).
As shown in Fig. 1a, a total of 120 high-risk (EC < 0.1%) patients were randomly assigned to receive NAC prophylaxis (group A, N = 80) or not to receive NAC prophylaxis (group B, N = 40), and low-risk (EC ≥ 0.1%) (group C, N = 105) patients were included in the final analysis.
The study protocol was approved by the ethics committee review board of Peking University People’s Hospital, and written informed consent was obtained from the subjects in accordance with the Declaration of Helsinki. This trial was registered at www.clinicaltrials.gov as # NCT03967665.
Randomization and masking
As shown in Fig. 1b, patients with AL in CR scheduled to undergo first HSCT from haploidentical donor were screened for eligibility, which was performed ≤ 3 days prior to randomization (at 14 days before conditioning (−24 days)). Enrolled subjects were stratified as high-risk (EC < 0.1%) or low-risk (EC ≥ 0.1%, group C) for developing PGF or PT according to the previously identified percentage of BM ECs pre-haplo-HSCT [5]. High-risk patients were randomly allocated in a 2:1 ratio to receive NAC prophylaxis (group A) or nonprophylaxis (group B) at 14 days before conditioning (−24 days). Randomization was performed with permuted blocks (block size four) and conducted by an interactive web-based response system (IWRS). The computer-generated randomization codes were sent to the IWRS vendor to implement the randomization. Study site staff recruited participants. The next assignment in the sequence was concealed. The investigators or subjects were not masked to assignment. The outcome assessments and data analysis were undertaken in a masked pattern.
Procedures
As previously described [4,5,6,7, 26,27,28], BM ECs were identified by mouse anti-human CD34, CD45, and vascular endothelial growth factor receptor 2 (VEGFR2, CD309) monoclonal antibodies (Becton Dickinson Biosciences, San Jose, CA) and analyzed using a BD LSRFortessa cell analyzer (Becton Dickinson). BM ECs were quantified by the percentages of CD34+CD309+ cells in total BM mononuclear cells (BMMNCs). The functions of BM ECs, including intracellular ROS levels, double-positive staining with both Dil-acetylated low-density lipoprotein (DiI-AcLDL) and fluorescein isothiocyanate–labeled Ulex Europaeus Agglutinin-1 (FITC-UEA-1), tube formation and migration assays, were analyzed pre- and post-HSCT as previously reported [4,5,6,7, 28].
Donor selection and human leukocyte antigen typing were performed as previously described [29]. All patients were given myeloablative chemotherapy-based conditioning regimen for a total of 10 days which included cytarabine (Ara-C, 4 g/m2/day, intravenously (i.v.), days −10 and −9), busulfan (Bu, 3.2 mg/kg/day, i.v., days −8 to −6), cyclophosphamide (Cy, 1.8 g/m2/day, i.v., days −5 and −4), and simustine (250 mg/m2, orally, day −3), plus antithymocyte globulin (ATG, 2.5 mg/kg/day, i.v., days −5 to −2), and received cyclosporin A (CsA), methotrexate (MTX), and mycophenolate (MMF) for graft-versus-host disease (GVHD) prophylaxis [30].
After enrollment, patients in group A were scheduled for NAC prophylaxis from 14 days before conditioning (−24 days) until +60 days post-HSCT. The initial dose of NAC was 400 mg orally three times daily (TID). For group B patients, NAC were not administered before +60 days post-HSCT. For patients in all the three groups, neither thrombopoietin (TPO) nor TPO receptor agonists (TPO-RAs) were administered before +60 days post-HSCT.
Outcomes
The primary endpoint was the incidence of PGF or PT. Secondary endpoints included cumulative incidences of leukemia relapse (CIR), GVHD, nonrelapse mortality (NRM), leukemia-free survival (LFS), overall survival (OS), and adverse events (AEs).
PGF [3, 5,6,7,8] was defined as the presence of 2 or 3 cytopenic counts (absolute neutrophil count (ANC) ≤ 0.5×109/L, platelet ≤ 20×109/L, or hemoglobin ≤ 70g/L) for at least 3 consecutive days post-HSCT with a transfusion requirement related to hypoplastic-aplastic BM in the presence of complete donor chimerism (CDC) without disease relapse. Primary PGF was identified as the failure to achieve initial reconstitution by +28d post-HSCT. Secondary PGF was defined as the fulfillment of the criteria of PGF after reconstitution [31]. PT [4, 9, 32, 33] was defined as a platelet count less than 20×109/L or a dependence on platelet transfusion with the engraftment of other cell lines (ANC > 0.5×109/L and hemoglobin > 70g/L without transfusion support) post-HSCT in the presence of CDC. Primary PT was defined as the failure to achieve platelet engraftment by +60 days post-HSCT and secondary PT as the fulfillment of the criteria after initial platelet engraftment [33]. Engraftment was marked by ANC > 0.5×109/L for 3 consecutive days without G-CSF administration, platelet > 20×109/L for 7 consecutive days without platelet transfusion, and hemoglobin > 70 g/L without red blood cell transfusion. In contrast, graft rejection, defined as never having achieved engraftment with mixed chimerism or complete recipient chimerism. Any measurable level of residual disease (MRD) as assessed by multiparameter flow cytometry and/or polymerase chain reaction was considered positive at the time of transplant [34, 35]. Relapse, NRM, LFS, and OS were defined as previously described [30, 35]. aGVHD were graded according to the literature [36]. AEs were graded based on the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE version 4.0) with the exception of hematologic AEs. Sinusoidal obstruction syndrome (SOS) was diagnosed according to the criteria stated by Jones et al. an onset before day 21 of hyperbilirubinemia and two of the following, weight gain >5%, tender hepatomegaly, and ascites [37].
Statistical analysis
This trial was designed to test the hypothesis that NAC prophylaxis was superior to nonprophylaxis in terms of PGF or PT. The sample size was calculated based on the incidence of primary or secondary PGF or PT at +60 days, which was approximately 30% in the AL patients with BM EC < 0.1% pre-haplo-HSCT without NAC prophylaxis [5, 31, 33, 38]. To identify a 20% absolute decrease in the incidence of PGF or PT with NAC prophylaxis, a minimum of 120 patients (80 in the study group and 40 in the control group) was required to provide the study with a one-sided significance level of 0.025 and a power of 80%. After adjusting for a 10% dropout, the total planned sample size was 130 patients. The sample size calculation was performed using PASS software (version 11.0).
The chi-square and Mann-Whitney U tests were performed for categorical variables and continuous variables, respectively. Cumulative incidences of PGF or PT, myeloid and platelet engraftment, relapse, NRM, and GVHD were calculated by accounting for competing risks using the Fine and Gray model [39]. OS and LFS were estimated by the Kaplan-Meier method and compared by the log-rank test. The corresponding hazard ratio (HR) and 95% CI were estimated using the Cox proportional hazard model. All variables in Table 1 were included in the univariable analysis. Only variables with P < 0.15 were included in the multivariable analysis. All statistical tests were two-tailed with a significance level of 0.05 except for the superiority hypothesis. SPSS 20.0 (SPSS Inc., Chicago, IL, USA) and R version 3.3.0 (R Development Core Team, Vienna, Austria) were used for data analysis.
Results
Study population
Between April 18, 2019, and June 24, 2021, 254 patients with AL scheduled to undergo first HSCT from haploidentical donors were screened. 130 were identified as high-risk (EC < 0.1%) for developing PGF or PT, and 124 were identified as low-risk (EC ≥ 0.1%). After screening, 10 patients with EC < 0.1% were excluded before randomization due to leukemia relapse (diagnosed by the same BM sample for EC detection), donor change (strongly positive donor-specific antibodies, donor decline), or contraindication to HSCT (organ failure diagnosed during the overall medical examination following BM EC detection before HSCT). Therefore, 120 of the 130 high-risk patients were randomly assigned at a 2:1 ratio to either receive (group A; N=80) or not receive (group B, N=40) NAC prophylaxis. Nineteen of the 124 low-risk patients (group C) were also excluded from data analysis due to leukemia relapse, donor change, contraindication to HSCT, or hesitation to undergo HSCT. The study flow diagram is shown in Fig. 1, and 120 randomized patients were included in the efficacy and safety analysis. Except for the BM EC percentage, the three groups (A, B, C) had balanced patient, donor and transplant characteristics including CD34+ cells infused, disease risk index [40], and MRD status before transplant (Table 1).
NAC prophylaxis significantly reduced PGF or PT
The +60 days cumulative incidence of PGF or PT was 7.5% (95% CI, 1.7 to13.3%) in group A compared to 22.5% (95% CI, 9.1 to 35.9%; P = 0.021) in group B and 11.4% (95% CI, 5.2 to17.6%; P = 0.373) in group C (Fig. 2a). Within +60 days, there were 27 PGF or PT including 1 primary PGF, 16 secondary PGF, 3 primary PT, and 7 secondary PT. Sensitivity analyses excluding subjects receiving haplo-HSCT using rituximab for desensitization with a positive donor-specific antibody indicated that there were 7.8% (95% CI, 1.8 to13.8%) with PGF or PT in group A (N = 77) compared to 23.1% (95% CI, 9.5 to 36.7%) in group B (N = 39; P = 0.023) and 9.9% (95% CI, 3.9 to 15.9%) in group C (N = 101; P = 0.627). The median time to platelet engraftment is shown in Table 2. Univariable analysis of PGF or PT is shown in Table 3. Results of an exploratory post hoc subgroup analysis are shown in Table 4.
Multivariable analysis revealed that NAC prophylaxis (P = 0.029; NAC prophylaxis vs. high-risk control: HR 0.274, 95% CI, 0.096 to 0.777; P = 0.015; NAC prophylaxis vs. low-risk control: HR 0.725, 95% CI, 0.270 to1.945; P = 0.523) and CD34+ cell count higher than the median (HR 0.400, 95% CI, 0.163 to 0.984; P = 0.046) were associated with lower incidence of PGF or PT (Table 3).
NAC prophylaxis did not affect neutrophil engraftment, GVHD, or virus infection
Neutrophil engraftment by +28 days was achieved in all of the patients except one in group C. There was no primary graft rejection. The median time to neutrophil engraftment did not differ between the three groups (Table 2). The 100-day cumulative incidence of aGVHD, CMV and EBV infection was also similar (Table 2).
NAC prophylaxis did not affect NRM, CIR, or survival
With a median follow-up of 347 days (range, 60–844 days) (Table 1) post-HSCT, the 1-year probabilities relapse, NRM, LFS, and OS were similar among the three groups (Table 2 and Fig. 2b, c). At the last follow-up, 212 patients survived, and 13 died after a median of 187 days (range, 54–290 days) post-HSCT. Causes of death are shown in Table 5.
Adverse events
AEs from enrollment to +60 days post-HSCT are shown in Table 6. Four patients died of AEs (three infections in group A and one infection in group B). All the grade 3 to 5 AEs were nontreatment-related. Since NAC is known to reduce the hepatotoxicity including SOS incidence and reduces Bu/Cy side effects [41, 42], liver function test values for both groups A and B are shown in Table 7. Liver enzymes and bilirubin values were most highly elevated in the high-risk control group B compared to NAC group A after BU conditioning, at +21 days, +60 days post-HSCT, although it did not reach statistical significance. None of the patients developed SOS.
Prophylactic NAC improved the quantity of BM ECs and their ROS levels in the EC < 0.1% group
To evaluate whether prophylactic NAC could improve the impaired BM ECs and hematopoiesis post-HSCT, the quantity and function of BM ECs and CD34+ cells were investigated kinetically before randomization (−24 days) at conditioning initiation (−10 days), +14 days, +30 days, and +60 days post-HSCT. The percentage of BM ECs in group C was significantly higher than the baseline level in group A and group B. Prophylactic NAC gradually improved the percentage (Fig. 3a; −10 days: 0.10±0.02 vs. 0.05±0.005; P = 0.02; +60 days: 0.10±0.01 vs. 0.07±0.007; P = 0.03) and functions of BM ECs including double-positive staining (Additional file 1: Fig. S1a; +60 days: 78.17±6.65 vs. 36.33±5.25; P = 0.001), the abilities of migration (Additional file 1: Fig. S1b; −10 days:162.17±19.56 vs. 92.5±4.26; P < 0.0001; +14 days: 121.33±16.16 vs. 68.67±13.39; P = 0.002; +60 days: 105.33±3.04 vs. 44.17±10.71; P = 0.0004), and tube formation (Additional file 1: Fig. S1c; +14 days: 579.72±49.14 vs. 174.97±51.22; P = 0.0005; +60 days: 599.32±34.23 vs. 240.57±42.44; P = 0.002) of BM ECs in group A compared with those in group B.
Prophylactic NAC improved BM ECs and CD34+ cells in EC<0.1% group post-HSCT. The dynamic reconstitution (left panel) and statistical analysis (right panel) of a BM EC percentage, b EC ROS level, c CD34+ cell percentage, and d CD34+ cell ROS level were analyzed by flow cytometry among the three groups before randomization (−24 days), at the time of conditioning initiation (−10 days), and +14, +30, +60 days post-HSCT. The data are expressed as the mean and SEM. P ≤ 0.05 was considered statistically significant and values are provided in the figure (*P ≤ 0.05, ** P ≤ 0.01, *** P ≤ 0.001, **** P ≤ 0.0001)
Elevated baseline ROS level in BM ECs was observed in group A (Fig. 3b; 3738.91±444.29 vs. 2179.90±265.73; P = 0.002) and group B (Fig. 3b; 3575.17±489.31 vs. 2179.90±265.73; P = 0.005) compared with group C before randomization. NAC prophylaxis significantly reduced the ROS level of BM ECs (Fig. 3b; 2178.92±227.67 vs. 3738.91±444.29; P = 0.02) at – 10 days compared to their baseline level in group A. In contrast, significantly higher ROS level of BM ECs was found at −10 days (Fig. 3b; 4069.43±604.72 vs. 2178.92±227.67; P = 0.01) and +30 days (Fig. 3b; 4204.17±569.79 vs. 2948.94±287.54; P = 0.03), and +60 days (Fig. 3b; 4192.74±360.1 vs. 3112.75±271.26; P = 0.07) in group B than in group A.
After NAC prophylaxis in group A, the percentage of BM ECs was significantly increased (Fig. 3a; 0.10±0.02 vs. 0.05±0.006; P = 0.0008). Moreover, NAC prophylaxis gradually improved the percentage and functions including double-positive staining (Additional file 1: Fig. S1a; −10 days:75.67±16.99 vs. 95.5±6.52; P = 0.19; +14 days: 58.67±6.61 vs. 84±15.20; P = 0.1; +30 days: 59.5±4.19 vs. 76.17±11.82; P = 0.27), the abilities of migration (Additional file 1: Fig. S1b; −10 days: 162.17±19.56 vs. 162.67±9.45; P=0.98; +14 days: 121.33±16.16 vs. 145.67±17.01; P = 0.2; +30 days: 82±7.66 vs. 108.33±10.26; P = 0.16) and tube formation (Additional file 1: Fig. S1c; −10 days: 470.22±122.76 vs. 912.1±65.52; P = 0.01; +14 days: 579.72±49.14 vs. 490.88±57.05; P = 0.56; +30 days: 377.58±63.07 vs. 781.9±185.53; P = 0.01) of BM ECs from patients in group A to the similar degree as those of group C. In contrast, no significant improvement in BM ECs was found in group B.
Prophylactic NAC improved the quantity of BM CD34+ cells and their ROS levels in the EC < 0.1% group
Consistent with the improvement of BM ECs, NAC prophylaxis gradually increased the percentage of BM CD34+ cells in group A to similar levels to those in group C at +14 days (Fig. 3c; 1.04±0.14 vs. 1.18±0.11; P = 0.59), +30 days (Fig. 3c; 1.1±0.24 vs. 1.16±0.16; P = 0.76), and +60 days (Fig. 3c; 1.17±0.15 vs. 1.31±0.07; P = 0.47), which were better than those in group B. The ROS levels of CD34+ cells in group A were gradually reduced to similar levels to those in group C at +30 days (Fig. 3d; 3987.06±406.87 vs. 4125.72±458.56; P = 0.85), +60 days (Fig. 3d; 3971.03±267.72 vs. 4285.54±607.1; P = 0.67), which were remarkably lower than those in group B.
Taken together, our data indicate that oral NAC prophylaxis could improve impaired BM EC reconstitution and therefore better support donor CD34+ cell engraftment post-HSCT.
Discussion
The current study is a phase 3, open-label randomized trial to demonstrate that NAC prophylaxis could promote hematopoietic reconstitution by improving the quantity and function of BM ECs after allo-HSCT and thereby reduce the incidence of PGF or PT in BM EC < 0.1% high-risk patients.
In this study, our results achieved the expected primary objective of testing for a reduction in the incidence of PGF or PT for the NAC and high-risk control groups (7.5% vs. 22.5%) while NAC prophylaxis obtained similar outcomes to those in low-risk group C. These results are consistent with our previous single-arm reports. In addition, the current randomized trial results further validated that BM EC is a reliable marker for predicting PGF or PT and that EC-directed NAC prophylaxis could offset the detrimental EC effect on poor hematopoietic reconstitution after allo-HSCT [5].
Unraveling how to improve dysfunctional BM ECs to enhance hematopoiesis will be of great importance to guide the establishment of new approaches. Recently, Hu et al. reported that multiple antioxidants, such as NAC, sulforaphane, and resveratrol, could alleviate the damage of radiation-induced bystander effects to human HSCs mainly through regulating their oxidative stress [43]. However, to our knowledge, the current RCT is the first to establish a novel BM microenvironment-directed antioxidant therapy to promote hematopoiesis in HSCT patients based on pathogenesis.
Tolerability is another issue of concern apart from efficacy. The overall grade 3 to 5 AEs within +60 days post-HSCT were similar between groups A and B and were nontreatment-related. In addition, NAC use did not affect GVHD or virus infection despite reducing PGF/PT, maybe partly due to the insufficient power to detect the difference for the second endpoints when considering the negative impact of PGF/PT on GVHD and viral infection, and also the intensified immune suppression itself having great effect on GVHD and viral infection.
We acknowledge the limitation of the relatively short follow-up and insufficient power to detect the difference for the second endpoints including GVHD, viral infection, and other transplant outcomes with respect to the clinical benefit. Nevertheless, the concerns about bleeding and infection risk caused by poor hematopoietic reconstitution might be ameliorated. Furthermore, NAC is reported to be a potential prophylactic treatment for hepatotoxicity during BU conditioning. With this regard, the lower dose and the oral administration of NAC in our study as compared to higher i.v. dose in previous reports might attribute to less striking effect [41, 42]. Longer follow-up and quality-of-life assessments as well as further studies with larger sample size are needed to explore additional clinical benefit.
Conclusions
In summary, a phase 3, open-label randomized trial confirmed that BM EC<0.1% pre-HSCT can identify high-risk patients for the occurrence of PGF or PT post-HSCT. Convenient oral NAC prophylaxis was safe and effective in preventing the occurrence of poor hematopoietic function by repairing impaired BM ECs. Therefore, our data indicate that improvement of the BM microenvironment may offer a potential pathogenesis-oriented therapeutic approach for poor hematopoietic function for future validation.
Availability of data and materials
The data that support the findings of this study are available upon reasonable request from the corresponding author.
Abbreviations
- allo-HSCT:
-
Allogeneic hematopoietic stem cell transplantation
- AL:
-
Acute leukemia
- Ara-C:
-
Cytarabine
- ATG:
-
Antithymocyte globulin
- AEs:
-
Adverse events
- BM:
-
Bone marrow
- BMMNCs:
-
BM mononuclear cells
- Bu:
-
Busulfan
- CR:
-
Complete remission
- Cy:
-
Cyclophosphamide
- CsA:
-
Cyclosporin A
- CIR:
-
Cumulative incidences of leukemia relapse
- CDC:
-
Complete donor chimerism
- DiI-AcLDL:
-
Dil-acetylated low-density lipoprotein
- ECs:
-
Endothelial cells
- FITC-UEA-1:
-
Fluorescein isothiocyanate–labeled Ulex Europaeus Agglutinin-1
- GVHD:
-
Graft-versus-host disease
- HSCs:
-
Hematopoietic stem cells
- haplo-HSCT:
-
Haploidentical-HSCT
- LFS:
-
Leukemia-free survival
- MMF:
-
Mycophenolate
- MTX:
-
Methotrexate
- MRD:
-
Measurable residual disease
- NAC:
-
N-Acetyl-L-cysteine
- NRM:
-
Nonrelapse mortality
- OS:
-
Overall survival
- PGF:
-
Poor graft function
- PT:
-
Prolonged isolated thrombocytopenia
- ROS:
-
Reactive oxygen species
- SOS:
-
Sinusoidal obstruction syndrome
- TID:
-
Three times daily
- TPO:
-
Thrombopoietin
- ULN:
-
Upper limit of normal
- VEGFR2:
-
Vascular endothelial growth factor receptor 2
References
Langer CJ, Gadgeel SM, Borghaei H, Papadimitrakopoulou VA, Patnaik A, Powell SF, et al. Carboplatin and pemetrexed with or without pembrolizumab for advanced, non-squamous non-small-cell lung cancer: a randomised, phase 2 cohort of the open-label KEYNOTE-021 study. Lancet Oncol. 2016;17(11):1497–508.
Paz-Ares L, Ciuleanu TE, Cobo M, Schenker M, Zurawski B, Menezes J, et al. First-line nivolumab plus ipilimumab combined with two cycles of chemotherapy in patients with non-small-cell lung cancer (CheckMate 9LA): an international, randomised, open-label, phase 3 trial. Lancet Oncol. 2021;22(2):198–211.
Kong Y. Poor graft function after allogeneic hematopoietic stem cell transplantation-an old complication with new insights(). Semin Hematol. 2019;56(3):215–20.
Kong Y, Shi MM, Zhang YY, Cao XN, Wang Y, Zhang XH, et al. N-acetyl-L-cysteine improves bone marrow endothelial progenitor cells in prolonged isolated thrombocytopenia patients post allogeneic hematopoietic stem cell transplantation. Am J Hematol. 2018;93(7):931–42.
Kong Y, Wang Y, Zhang YY, Shi MM, Mo XD, Sun YQ, et al. Prophylactic oral NAC reduced poor hematopoietic reconstitution by improving endothelial cells after haploidentical transplantation. Blood Adv. 2019;3(8):1303–17.
Lyu ZS, Cao XN, Wen Q, Mo XD, Zhao HY, Chen YH, et al. Autophagy in endothelial cells regulates their haematopoiesis-supporting ability. EBioMedicine. 2020;53:102677.
Shi MM, Kong Y, Song Y, Sun YQ, Wang Y, Zhang XH, et al. Atorvastatin enhances endothelial cell function in posttransplant poor graft function. Blood. 2016;128(25):2988–99.
Zhao HY, Lyu ZS, Duan CW, Song Y, Han TT, Mo XD, et al. An unbalanced monocyte macrophage polarization in the bone marrow microenvironment of patients with poor graft function after allogeneic haematopoietic stem cell transplantation. Br J Haematol. 2018;182(5):679–92.
Zhao HY, Zhang YY, Xing T, Tang SQ, Wen Q, Lyu ZS, et al. M2 macrophages, but not M1 macrophages, support megakaryopoiesis by upregulating PI3K-AKT pathway activity. Signal Transduct Target Ther. 2021;6(1):234.
Brodsky RA, Jones RJ. Aplastic anaemia. Lancet. 2005;365(9471):1647–56.
Young NS. Aplastic Anemia. N Engl J Med. 2018;379(17):1643–56.
Ades L, Itzykson R, Fenaux P. Myelodysplastic syndromes. Lancet. 2014;383(9936):2239–52.
Cazzola M. Myelodysplastic syndromes. N Engl J Med. 2020;383(14):1358–74.
Xing T, Lyu ZS, Duan CW, Wen Q, Zhao HY, Tang SQ, et al. Endothelial cell dysfunction is involved in the progression of myelodysplastic syndromes. 63rd Annual Meeting of the American Society of Hematology; Blood. 2021; 2021:3668.
Scadden DT. The stem-cell niche as an entity of action. Nature. 2006;441(7097):1075–9.
Morrison SJ, Scadden DT. The bone marrow niche for haematopoietic stem cells. Nature. 2014;505(7483):327–34.
Crane GM, Jeffery E, Morrison SJ. Adult haematopoietic stem cell niches. Nat Rev Immunol. 2017;17(9):573–90.
Pinho S, Frenette PS. Haematopoietic stem cell activity and interactions with the niche. Nat Rev Mol Cell Biol. 2019;20(5):303–20.
Yu VW, Scadden DT. Hematopoietic stem cell and its bone marrow niche. Curr Top Dev Biol. 2016;118:21–44.
Hooper AT, Butler JM, Nolan DJ, Kranz A, Iida K, Kobayashi M, et al. Engraftment and reconstitution of hematopoiesis is dependent on VEGFR2-mediated regeneration of sinusoidal endothelial cells. Cell Stem Cell. 2009;4(3):263–74.
Ding L, Saunders TL, Enikolopov G, Morrison SJ. Endothelial and perivascular cells maintain haematopoietic stem cells. Nature. 2012;481(7382):457–62.
Fadini GP, Coracina A, Baesso I, Agostini C, Tiengo A, Avogaro A, et al. Peripheral blood CD34+KDR+ endothelial progenitor cells are determinants of subclinical atherosclerosis in a middle-aged general population. Stroke. 2006;37(9):2277–82.
Itkin T, Gur-Cohen S, Spencer JA, Schajnovitz A, Ramasamy SK, Kusumbe AP, et al. Distinct bone marrow blood vessels differentially regulate haematopoiesis. Nature. 2016;532(7599):323–8.
Chute JP, Muramoto GG, Salter AB, Meadows SK, Rickman DW, Chen B, et al. Transplantation of vascular endothelial cells mediates the hematopoietic recovery and survival of lethally irradiated mice. Blood. 2007;109(6):2365–72.
Salter AB, Meadows SK, Muramoto GG, Himburg H, Doan P, Daher P, et al. Endothelial progenitor cell infusion induces hematopoietic stem cell reconstitution in vivo. Blood. 2009;113(9):2104–7.
Werner N, Kosiol S, Schiegl T, Ahlers P, Walenta K, Link A, et al. Circulating endothelial progenitor cells and cardiovascular outcomes. N Engl J Med. 2005;353(10):999–1007.
Fadini GP, Mehta A, Dhindsa DS, Bonora BM, Sreejit G, Nagareddy P, et al. Circulating stem cells and cardiovascular outcomes: from basic science to the clinic. Eur Heart J. 2020;41(44):4271–82.
Kong Y, Cao XN, Zhang XH, Shi MM, Lai YY, Wang Y, et al. Atorvastatin enhances bone marrow endothelial cell function in corticosteroid-resistant immune thrombocytopenia patients. Blood. 2018;131(11):1219–33.
Zhang XH, Chen J, Han MZ, Huang H, Jiang EL, Jiang M, et al. The consensus from The Chinese Society of Hematology on indications, conditioning regimens and donor selection for allogeneic hematopoietic stem cell transplantation: 2021 update. J Hematol Oncol. 2021;14(1):145.
Wang Y, Liu QF, Lin R, Yang T, Xu YJ, Mo XD, et al. Optimizing antithymocyte globulin dosing in haploidentical hematopoietic cell transplantation: long-term follow-up of a multicenter, randomized controlled trial. Sci Bull. 2021;24:2498–505.
Sun YQ, He GL, Chang YJ, Xu LP, Zhang XH, Han W, et al. The incidence, risk factors, and outcomes of primary poor graft function after unmanipulated haploidentical stem cell transplantation. Ann Hematol. 2015;94(10):1699–705.
Kim DH, Sohn SK, Jeon SB, Baek JH, Kim JG, Lee NY, et al. Prognostic significance of platelet recovery pattern after allogeneic HLA-identical sibling transplantation and its association with severe acute GVHD. Bone Marrow Transplant. 2006;37(1):101–8.
Tang FF, Sun YQ, Mo XD, Lv M, Chen YH, Wang Y, et al. Incidence, risk factors, and outcomes of primary prolonged isolated thrombocytopenia after haploidentical hematopoietic stem cell transplant. Biol Blood Marrow Transplant. 2020;26(8):1452–8.
Guo H, Chang YJ, Hong Y, Xu LP, Wang Y, Zhang XH, et al. Dynamic immune profiling identifies the stronger graft-versus-leukemia (GVL) effects with haploidentical allografts compared to HLA-matched stem cell transplantation. Cell Mol Immunol. 2021;18(5):1172–85.
Wang Y, Chen H, Chen J, Han M, Hu J, Jiong H, et al. The consensus on the monitoring, treatment, and prevention of leukemia relapse after allogeneic hematopoietic stem cell transplantation in China. Cancer Lett. 2018;438:63–75.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant. 1995;15(6):825–8.
Jones RJ, Lee KS, Beschorner WE, Vogel VG, Grochow LB, Braine HG, et al. Venoocclusive disease of the liver following bone marrow transplantation. Transplantation. 1987;44(6):778–83.
Sun YQ, Wang Y, Zhang XH, Xu LP, Liu KY, Yan CH, et al. Virus reactivation and low dose of CD34+ cell, rather than haploidentical transplantation, were associated with secondary poor graft function within the first 100 days after allogeneic stem cell transplantation. Ann Hematol. 2019;98(8):1877–83.
Austin PC, Fine JP. Practical recommendations for reporting Fine-Gray model analyses for competing risk data. Stat Med. 2017;36(27):4391–400.
Armand P, Kim HT, Logan BR, Wang Z, Alyea EP, Kalaycio ME, et al. Validation and refinement of the Disease Risk Index for allogeneic stem cell transplantation. Blood. 2014;123(23):3664–71.
El-Serafi I, Remberger M, El-Serafi A, Benkessou F, Zheng W, Martell E, et al. The effect of N-acetyl-l-cysteine (NAC) on liver toxicity and clinical outcome after hematopoietic stem cell transplantation. Sci Rep. 2018;8(1):8293.
Sjoo F, Aschan J, Barkholt L, Hassan Z, Ringden O, Hassan M. N-acetyl-L-cysteine does not affect the pharmacokinetics or myelosuppressive effect of busulfan during conditioning prior to allogeneic stem cell transplantation. Bone Marrow Transplant. 2003;32(4):349–54.
Hu L, Yin X, Zhang Y, Pang A, Xie X, Yang S, et al. Radiation-induced bystander effects impair transplanted human hematopoietic stem cells via oxidative DNA damage. Blood. 2021;137(24):3339–50.
Acknowledgements
The authors thank all of the core facilities at Peking University Institute of Hematology for patient care and sample collection. We thank QW and ZSL from Peking University People’s Hospital for their assistance in detecting EC in the study. American Journal Experts (www.journalexperts.com) provided editorial assistance to the authors during the preparation of the manuscript.
Funding
This work was supported by the National Key Research and Development Program (2019YFC0840606 & 2021YFA1100904 & 2017YFA0104500), National Natural Science Foundation of China (82070189 &82070188 & 81870139 & 81930004), and the Foundation for Innovative Research Groups of the National Natural Science Foundation of China (81621001).
Author information
Authors and Affiliations
Contributions
XJH were responsible for the conception and design. XJH, YW, and YK were responsible for the development of methodology. YW, YK, YYZ, HYZ, YZW, LPX, XHZ, and KYL were responsible for the acquisition of data (acquired and managed patients, provided facilities, etc.). YW and YK were responsible for the analysis and interpretation of data (e.g., statistical analysis, biostatistics, computational analysis). XJH, YW, YK, and HYZ were responsible for the writing, review, and/or revision of the manuscript. XJH, YW, and YK were responsible for the administrative, technical, or material support (i.e., reporting or organizing data, constructing databases). XJH were responsible for the study supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the ethics committee review board of Peking University People’s Hospital, and written informed consent was obtained from the subjects in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Prophylactic NAC improved function of ECs in EC<0.1% group to similar levels in EC>0.1% group.
Additional file 2.
Study protocol and statistical analysis plan.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, Y., Kong, Y., Zhao, HY. et al. Prophylactic NAC promoted hematopoietic reconstitution by improving endothelial cells after haploidentical HSCT: a phase 3, open-label randomized trial. BMC Med 20, 140 (2022). https://doi.org/10.1186/s12916-022-02338-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-022-02338-9