Abstract
Purpose
Positron emission tomography (PET) is a nuclear imaging technique that uses radiotracers to visualize metabolic processes of interest across different organs, to diagnose and manage diseases, and monitor therapeutic response. This systematic review aimed to characterize the value of PET for the assessment of renal metabolism and function in subjects with non-oncological metabolic disorders.
Methods
This review was conducted and reported in accordance with the PRISMA statement. Research articles reporting “kidney” or “renal” metabolism evaluated with PET imaging between 1980 and 2021 were systematically searched in Medline/PubMed, Science Direct, and the Cochrane Library. Search results were exported and stored in RefWorks, the duplicates were removed, and eligible studies were identified, evaluated, and summarized.
Results
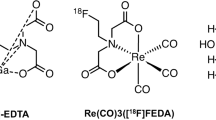
Thirty reports met the inclusion criteria. The majority of the studies were prospective (73.33%, n = 22) in nature. The most utilized PET radiotracers were 15O-labeled radio water (H215O, n = 14) and 18F-fluorodeoxyglucose (18F-FDG, n = 8). Other radiotracers used in at least one study were 14(R,S)-(18)F-fluoro-6-thia-heptadecanoic acid (18F-FTHA), 18F-Sodium Fluoride (18F-NaF), 11C-acetate, 68-Gallium (68Ga), 13N-ammonia (13N-NH3), Rubidium-82 (82Rb), radiolabeled cationic ferritin (RadioCF), 11C‐para-aminobenzoic acid (11C-PABA), Gallium-68 pentixafor (68Ga-Pentixafor), 2-deoxy-2-F-fluoro-d-sorbitol (F-FDS) and 55Co-ethylene diamine tetra acetic acid (55Co-EDTA).
Conclusion
PET imaging provides an effective modality for evaluating a range of metabolic functions including glucose and fatty acid uptake, oxygen consumption and renal perfusion. Multiple positron emitting radiolabeled racers can be used for renal imaging in clinical settings. PET imaging thus holds the potential to improve the diagnosis of renal disorders, and to monitor disease progression and treatment response.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The kidneys are complex metabolic organs that perform osmoregulatory and key endocrine functions [1]. They effectively filter, remove, and reabsorb both essential and non-essential solutes from plasma, while contributing to the regulation of the acid–base balance in the body [2, 3]. They also play important roles in the metabolism of carbohydrates, proteins, and other nutrients [4]. Given their functional and metabolic roles, diseases affecting kidneys such as acute or chronic renal failure usually result in complex deleterious alterations in the overall physiological and metabolic processes in the body [5].
The kidneys utilize several different substrates such as lactate, free fatty acids, glutamine, 3-hydroxybutyrate, glycerol and citrate for the functional activities [6]. The preferred substrates for cellular respiration in the renal cortex include both short- and long-chain fatty acids and some amino acids [7]. In the outer medulla, lactate appears to be the preferred substrate over glucose [7]. And in the inner medulla, oxygen consumption is much lower than in the cortex, while glucose is the preferred metabolic substrate [6].
During the postabsorptive period, the kidneys account for 10% of the whole-body glucose utilization. Normally, approximately 180 g of glucose are filtered every 24 h and almost all of it are reabsorbed by means of the sodium/glucose cotransporter 2 (SGLT2) system, which is expressed in the early proximal tubules of the nephron [2, 3]. Most of the remaining glucose absorption is by sodium/glucose cotransporter 1(SGLT1) located at a more distal sections of the proximal tubules [8]. Importantly, the reabsorption of sodium ions is mainly due to the extremely high oxidative metabolism of the renal system [9].
Metabolic disease/disorder is characterized by the disruption in normal metabolism which affects the performance of critical biochemical reactions involving the processing or transport of proteins (amino acids), carbohydrates (glucose), and lipids (fatty acids) [10]. Moreover, metabolic disease is associated with oxidative stress and mitochondrial dysfunction [10]. Previous studies have reported that individuals with metabolic abnormalities are at an increased risk of renal dysfunction, including chronic kidney disease which may lead to kidney failure and end-stage renal disease [11,12,13,14].
Positron emission tomography (PET) is a nuclear medicine-based imaging technique that can functionally evaluate metabolic processes within the body by the use of non-nephrotoxic tracer compounds [15, 16]. Its application has been extensive in the study of a variety of organs, and it is currently considered the gold standard for measuring tissue metabolic rates in vivo. PET data can be analyzed either semiquantitatively (through standardized uptake rate-SUV) or quantitatively (through graphical analysis, fractional uptake rate, compartmental models). The latter requiring determination of plasma input function, thus tracking the tracer uptake in the tissue of interest in respect to its availability in the circulation [17].
While PET applications in studies of brain [18], heart [19], liver [20], skeletal muscle [21] and adipose tissue [22, 23] are well established, there have been challenges in its implementation for the study of the kidneys. We believe, however, that renal PET has begun to demonstrate its unique potential in providing useful information in a relatively noninvasive manner. The present systematic review, therefore, aimed to identify and summarize all available studies that have evaluated kidney physiology (i.e., renal perfusion, glomerular filtration rate, glucose, and fatty acid metabolism) and pathophysiology (i.e., renal failure, acute rejection following kidney transplantation, renal cysts) though PET imaging in non-oncological patients with metabolic disorders.
Methods
Eligibility criteria
Peer reviewed publications reporting on the utilization of PET imaging for the evaluation of renal (patho) physiology in humans (namely renal perfusion, glucose, and fatty acid metabolism) from 1980 to 2021 (based on the time span of the technique’s existence) were included in this review. Editorials, letters, commentaries, perspectives, and conference abstracts were excluded together with PET studies involving oncological diseases with renal involvement. Only articles written in the English language were considered.
Information sources and search strategy
-
1.
Words that relate to the system: renal, kidney, nephrology.
-
2.
Words that relate to the technique: positron emission tomography.
-
3.
Words that relate to the studied function: renal metabolism in metabolic disorders.
We searched the MEDLINE (through PubMed), Science Direct and Cochrane databases. These databases were selected, because they provide extensive international journals and are regularly updated with relevant resources covering medicine, health sciences and related topics. Reference lists of relevant articles were hand-searched to identify additional articles. Relevant articles were then exported to and managed in the RefWorks Citation Manager®.
Study selection
After the deletion of duplicates, all titles and abstracts were duly reviewed and screened against the eligibility criteria. All ineligible articles were removed. Full texts of all relevant articles were then retrieved.
Data items and collection process
This systematic review was conducted and reported in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) statement [24]. Data were extracted into a standardized data collection form. Extracted data included: first author, publication year, demographics, study design, limitations, major findings, conclusion, and remarks. Each study was read and reread to identify core methodological aspects, perform data reduction and when possible, some comparisons. Two reviewers independently abstracted the contents of each included study. The risk of bias was appraised using Joanna Briggs Institute Critical Appraisal Checklist for Qualitative Research [25]. Discrepancies and disagreements were resolved through a third independent researcher.
Results
A total of 2502 articles were identified. After removal of duplicates and screening based on titles and abstracts, 73 articles underwent a full-text review out of which thirty met the inclusion criteria (Fig. 1, Table 1). Designs included prospective (73.33%, n = 22), retrospective (16.12%, n = 5), cross-sectional (6.45%, n = 2), and observational studies (3.22%, n = 1) studies. Most of the studies used 15O-labeled water (n = 14) or 18F-fluorodeoxyglucose (18F-FDG, n = 8) as the PET radiotracer. Tracers that were use in at least on study included 15O, 11C-acetate 18FFTHA, RadioCF, 82Rb, 11C-PABA, F-NaF, 18F-FDS, 68Ga-pentixafor, 82Rb, 13N-ammonia, and 68Ga-EDTA (Table 1).
Renal perfusion
A radiopharmaceutical is suitable for renal perfusion quantification if it shows high perfusion-rate-independent extraction from arterial blood in its first-pass transit through the renal capillaries [26]. The most commonly used PET tracer for perfusion measurement has been oxygen-15 radiolabeled water (H215O, radiowater) n = 15 [16, 27,28,29,30,31,32,33,34,35,36,37,38,39,40]. One study also reported that carbon-15 labeled acetate (11C-acetate) can be used for the same purpose [37]. A one-compartment model was used for the quantification of these tracers. Other tracers, which are not entirely freely diffusible, have also been used for perfusion quantification through implementation of the two-compartment Patlak model namely, Nitrogen-13 labeled ammonia (13N-ammonia) n = 1 [28] and rubidium-82 chloride (82Rb) n = 2 (which behaves like a K+ analogue and is very commonly used to measure myocardial perfusion) [41, 42].
Energy substrate metabolism
In a recent study that aimed to automatically quantify tracer uptake during euglycemic hyperinsulinemic clamp conditions, volume estimation by 18FDG was comparatively inaccurate in the kidneys [43]. This was largely due to spillover from urine. Furthermore, 14(R, S)-[18F] fluoro-6-thia-heptadecanoate (18F-FTHA) has been used to estimate cortical and medullar fatty acid uptake (n = 1) [38], while oxygen consumption has been quantified with 11C-acetate n = 1 [37].
Inflammation
18FDG has been shown to be useful in the noninvasive diagnostic workup in suspected allograft rejection n = 2 [44, 45]. In a small proof-of-concept study that included only two human subjects, Werner et al. suggested 2-deoxy-2-[18F] fluorosorbitol (18F-FDS) as an alternative to 18F-FDG in pediatric patients due to a lower radiation exposure [46]. In one study, gallium labelled 68Ga-pentixafor has been proposed as useful for detecting leukocytes in allografts when PET is combined with magnetic resonance imaging (MRI) [47].
Kidney function
In a study by Geist et al. [48], both the cortex and total kidney 18FDG glomerular filtration rate obtained from regression analysis of Patlak plots were shown to have strong positive correlations with the reference value for estimated glomerular filtration rate (eGFR) [48]. N = 2 studies have quantified renal clearance rate of 18FDG [49, 50]. One study calculated kidney function parameters from 18FDG standardized uptake values and time activity curves [51]. Parallelly, Minamimoto et al. [52] showed that mean 18FDG SUV in the kidney is higher in healthy volunteers than in patients with suspected renal failure [52]. GFR has been quantitated in n = 1 study with 68Ga-EDTA [53], while 11C-PABA has been shown to be safe in humans and could be used for functional renal imaging [54]. In a study by Baldelomar et al. [55], a mouse model was used to map nephron mass as proof of concept in a donated human kidney in vivo with RadioCF [55]. Higher renal artery F–Na–F uptake has also been associated with higher cardiovascular risk and lower GFR [56].
Discussion
Our systematic review assessed the application of PET imaging in the evaluation of renal metabolism in metabolic disorders based on 30 studies. The following key finding emerged. First, the largest proportion of studies reporting on kidney metabolism with PET were prospective reports. Second, 15O-labeled water and 18F-fluorodeoxyglucose were the most commonly used radiotracers for kidney metabolism. Third, a range of clinical features such as renal inflammation, glomerular filtration rate, and renal pathologies such as acute and chronic kidney diseases were studied with PET. Our findings reinforced the fact that PET imaging holds the potential for the assessment of renal function, and for the diagnosis of renal pathologies.
Renal physiology
Many tracers are cleared through the kidneys, which is why uptake appears high. This is the case with the widely used tracer 18F-FDG. Several experimental tracers, most of which likely have no or very little true uptake in the kidneys, also show high renal uptake: 68Ga-NODAGA-exendin-4 and 18F-FP-(+)-DTBZ, used for β-cell imaging [57, 58], 18F-Fluoro-L-DOPA, studied in infants with congenital hyperinsulinism [59], 11C-PK11195, used for assessing peripheral benzodiazepine receptor activity [60, 61], 18F-AH111585, a peptide with a high affinity for the αvβ3 integrin receptor involved in angiogenesis [62], 1C-PE2I, a cocaine analog tracer [63], 11C-PIB and 18F-FPYBF-2, which are amyloid imaging agents [64, 65], 11C-nicotine, used to detect nicotine receptors [59], 11C-metformin, used for studying the biodistribution and excretion of metformin [66], 11C-MP4B, a tracer for the assessment of butyrylcholinesterase activity [67], 86Y-SMT487, a radiolabeled somatostatin analogue [68] and 68Ga-NOTA-UBI, a potential tracer for diagnosing infectious processes [69].
Renal perfusion
Clearance-based methods used to estimate effective renal plasma flow (ERPF) are time consuming and stressful to the patient [48]. PET provides a noninvasive method for the quantification of renal perfusion [70]. Alternatively, current modalities such as magnetic resonance imaging (MRI) arterial spin labelling (ASL) technique utilizes magnetic labelling and endogenous tracer of water in arterial blood to generate maps of absolute regional perfusion without the use of exogenous contrast [71].
15O-H2O, also called “radiowater”, is the most commonly used tracer for measuring renal perfusion [33]. Damkjær et al. showed that even medullar blood flow can be separately assessed with radiowater [34]. Several studies investigating physiological mechanisms have been conducted with radiowater. Modest saline loading, which leads to a natriuretic response, did not always induce changes in renal perfusion in seven healthy subjects [34]. When the ACE inhibitor quinaprilat was given as an injection to n = 8 patients with hypertension and moderate chronic heart failure, renal blood flow was increased [32]. Enalapril also increases renal perfusion [33]. Middlekauff et al. observed decreased renal perfusion due to vasoconstriction in n = 29 healthy subjects in response to a static handgrip exercise [30]. The magnitude and duration of this effect were exaggerated in n = 39 heart failure patients, compared to n = 38 controls [31]. Middlekauff et al. [29] also investigated pulmonary baroreflex in n = 8 heart failure patients and noted that reflex control of circulation in the forearm but not kidneys was abnormal compared to n = 10 controls [29]. Radiowater was used to measure regional hemodynamics and metabolism in obese subjects and non-obese controls to determine the effects of major weight loss before and after bariatric surgery [38]. Cortical perfusion was found to be significantly higher as compared with medullary perfusion in both groups. Even though cortical and medullary blood perfusion rates (ml/100 g/min) were not different between the two groups, total renal blood flow was higher in the obese individuals, and it was significantly decreased following weight loss [38].
Three other PET tracers have also been shown to be usable in humans for the assessment of renal blood flow. Normand et al. validated a modeling method for [11C] acetate to measure perfusion, using radiowater as gold standard [37]. The benefit of the tracer is that it can also be used to measure oxidative metabolism and can thus provide information on two different functions [37]. 13N-ammonia has also been validated for measuring perfusion [28], but has since not been utilized in kidney studies. It is instead used in myocardial perfusion and blood flow studies [72]. 82Rb is also most commonly used to assess myocardial blood flow in patients suspected of ischemic heart disease, but 82Rb is also appropriate for modelling renal blood flow using dynamic PET methods, since the method has shown high image quality [41]. In a study assessing myocardial perfusion, regadenoson was shown to also increase kidney perfusion [42]. Another potential tracer for evaluating renal perfusion would be 62Cu-ETS [35], but so far validation results in humans comparing the tracer with radiowater, have only been presented as a meeting report [40].
Renal metabolism
Renal substrate metabolism is closely tied to renal hemodynamics; the well-perfused renal cortex is rich in mitochondria and depends predominantly on oxidative metabolism—mainly of fatty acids, but also of ketone bodies, and lactate, whereas the renal medulla, which operates in relative hypoxia, relies predominantly on glycolysis [73]. The proximal tubules are also equipped with the enzymes responsible for gluconeogenesis (glucose 6-phosphatase, fructose 1,6 diphosphatase, and phosphoenolpyruvate carboxykinase), making the kidney one of the organs which contribute to endogenous glucose production after the liver, and also to a lesser extent the intestines [74].
PET provides a method for investigating kidney energy metabolism in humans in vivo, yet very few studies have addressed these questions so far. 11C-acetate can be used for direct estimates of renal oxygen consumption [37]. It has recently been shown that renal FFA (i.e., cortical, and medullary) uptake using FTHA is increased in morbidly obese subjects compared to lean individuals, and that 6 months following bariatric surgery, renal FFA uptake remains high, because of the ongoing catabolic state [38]. 18F-FDG is a widely available tracer, which can be used for studying metabolic shifts in glucose utilization [75]. To the best of our knowledge thus far, there has been no study evaluating renal glucose uptake using 18FDG-PET. 18FDG is excreted into urine and thus addressing renal metabolism with 18F-FDG with current modeling methods is considered thus far to be heavily biased [76]. If the challenges with modeling kidney tracer uptake could be overcome, 18F-FDG could be used for studying metabolic shifts in kidneys as well. Since kidney energy metabolism is suggested to take part in the development of pathologies such as renal hypertension [74], PET has unused potential in investigating the development of these diseases in humans.
Renal function
Glomerular filtration rate (GFR) is defined as the rate of plasma flow through the glomerulus into the urinary space of the Bowman’s capsule and is the most effective index and key indicator for renal function [77]. GFR is of high clinical significance especially in the detection, treatment, and prevention of kidney disease, but it cannot discern between one- or two-sided defects in filtration rate.
The most commonly used PET radio tracer for examinations of renal functions is 18FDG. Pharmacokinetically, 18FDG enters the kidney through renal arteries, is filtered in the glomeruli, then partially reabsorbed in the proximal tubule, and finally excreted in the urine [78, 79]. As partly mentioned in the results, early 18FDG clearance (from injection) may also be used to estimate glomerular filtration rate (GFR) [48]. Both the cortex and total kidney 18FDG glomerular filtration rate [GFR(FDG)] were shown to have strong positive correlations with the reference value for GFR [GFR(ref)] [48]. The GFR(FDG) was obtained from a regression analysis of Patlak plots [48], whereas the GFR(ref) was estimated from creatinine values using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [80]. Based on this, it was estimated that GFR and EPRF can be assessed with 18FDG-PET in healthy kidneys [48]. FDG renal clearance has since been utilized to also estimate urinary glucose loss [81]. Rasul et al. have shown that mean transit time of 18FDG decreased with 2 weeks of SGLT2i treatment in T2D patients, shifting the transit time towards that of healthy controls [50].
Renal failure is characterized by the significant loss of kidney function with a GFR of less than 15 ml/min/1.73m2 [82]. Available treatment options for end-stage renal failure include kidney transplantation, hemodialysis, and peritoneal dialysis [83]. Although 18FDG-PET/CT can differentiate kidneys with end-stage renal disease from healthy kidneys, this by itself would be of limited clinical utility for patients who are already dependent on renal replacement therapy. Research shows that in patients with normal functioning kidneys, roughly 10% of the injected 18FDG is excreted in the urine in about 70 min after the tracer injection [84]. However, in individuals with chronic kidney failure (CKF) who are on hemodialysis, urinary 18FDG excretion is impaired and hence these subjects experience constant volume overload [85]. The 18FDG tracer is distributed more in regions such as brain, and less in the cardiovascular system compared to control subjects without CKD [52].
Assessment of GFR can also be done using 68Ga-EDTA [53] and 68Ga [15]. This agrees with Hofman et al. [86] who reported that 68Ga-GFR agreed well with 51Cr-GFR for estimation of GFR. It was also stated that PET dynamic imaging offers a method to estimate GFR with an added advantage of enabling renal imaging in a single study [86]. There was good agreement between 68Ga and 51Cr- EDTA GFR despite injection of both radiotracers simultaneously and the use of the same samples for positron and gamma counting [86]. Hofman et al. [86] showed that 51Cr- EDTA overestimates a GFR by about 10%. Despite this occurrence, Goethals et al. [87] stated that 51Cr-EDTA is accepted as the most reliable agent to study whole kidney GFR. The ability of PET to quantify activity in three dimensions makes it ideal for applications such as GFR estimation [86].
Renal vasculature
Renal artery stenosis is a form of atherosclerotic vascular disease and can result in kidney insufficiency and renal hypertension [36]. Few studies have addressed effects of renal vasculature with PET in humans. Higher renal artery wall F-NaF activity was associated with CV risk and inversely associated with GFR in a group with high CV risk [56]. In an observational study by Koivuviita et al. [36], it was shown that angiographic severity of renal artery stenosis did not determine the perfusion response to revascularization. They hypothesized that it might be due to concomitant microvascular disease [36].
PET as a diagnostic tool
We have previously discussed the impact of tracer secretion in renal insufficiency and have identified how FDG secretion is impaired. This could be of concern, since FDG is a commonly used tracer in oncology and in the diagnostic work up of fever of unknown origin, and renal failure is very common in a clinical setting. Although compromised kidneys tend to alter the biodistribution of drugs cleared by the renal systems, the presentation of renal diseases do not necessarily impact FDG uptake values in other organs and, therefore, tracer dose adjustment is not required in such subjects [83].
Two studies have assessed 18FDG PET/CT in the diagnostic work up of fever of unknown origin in end-stage renal disease patients, treated with dialysis. In a retrospective study on n = 22 patients, 15 patients showed metabolically active lesions and the scans lead to a change in treatment in 21 patients [88]. In a retrospective study on n = 46, 22 out of 46 scans identified the cause and a higher C-reactive protein level was predictive of a positive outcome [89]. The clinical utility was comparable to unselected patient populations. In a case study, including seven PET scans on three patients with autosomal dominant polycystic kidney disease, 18FDG PET could be used to diagnose or rule out cyst infection [90]. High 18FDG uptake can also be caused by urinary calculi [91].
Slowly progressing chronic kidney disease is common in kidney transplants, but PET has not been widely utilized for assessing this pathology. A pilot study showed that PET could measure kidney transplant perfusion and that microvascular dysfunction could be detected in transplants [39]. Larger studies are needed on transplant patients and patients with advanced CKD before the method can be implemented in clinical use.
Acute kidney injury caused by acute rejection (AR) is also common in renal transplants. Current immunosuppressive treatments can efficiently treat AR, and thus the timely diagnosis of AR is fundamental. In acute rejection, there is accumulation of activated leucocytes in the transplant, which are characterized by an increased avidity for glucose (and 18FDG) [92]. Diagnosis of AR is based on transplant needle biopsy, which is an invasive procedure. PET could, therefore, provide a noninvasive means for directing further diagnostic testing.
In a preclinical study in rats, Reuter and colleagues demonstrated, that 18FDG-PET uptake was increased in transplants which were undergoing AR [93]. This finding was later confirmed in a study in n = 31 humans [45]. However, in this study, even though the sensitivity of 18FDG-PET was 100%, the specificity was only 50% [45]. Jadoul et al. [44] later showed in a prospective n = 95 study that 18FDG is usable for disproving acute rejection since quantification was repeatable and reproducible [44]. Parameters obtained from 18FDG PET/MRI have also shown a possible predictive feature for renal recovery in solid organ kidney transplantation patients undergoing acute kidney injury [51]. 68Ga-pentixafor has been investigated in 13 patients with renal allografts and complicated urinary tract infection, to detect leukocytes in grafts [47].
A cross-sectional diagnostic test study by Aaltonen et al. [94], where 26 dialysis patients suspected for renal osteodystrophy were studied with 18F-NaF, showed that PET could provide a noninvasive diagnostic tool in patients that usually undergo bone biopsy for diagnosis [94].
Strengths and limitations
This review has followed the recommendations for the systematic search of articles and the PRSIMA statement, which is internationally recognized. The limitation of this study is that only single studies have been conducted for several PET tracers, such as 11C-acetate, 18FFTHA, 18F-NaF, RadioCF, 11C-PABA, 13N-ammonia 18F-FDS, 68Ga-pentixafor and 68Ga-EDTA, which importantly reduced the analytical and comparative possibilities of our report. Nevertheless, we have maintained the descriptive axis of a systematic review to inform about this publication pitfalls and current knowledge gaps.
Conclusion
PET imaging provides an effective modality for evaluating a range of metabolic functions including glucose and fatty acid uptake, oxygen consumption and renal perfusion. Patients may benefit from undergoing PET imaging of the renal system for a variety of purposes, including the assessment of renal function and metabolism, disease diagnosis and prognosis. However, several useful tracers, however, have only been marginally utilized in clinical studies. PET imaging is an effectively growing, and currently underused modality for the noninvasive evaluation of renal (patho)physiology and its expansion could benefit non-oncological patients who suffer from metabolic diseases.
References
Ogobuiro I, Tuma F. Physiology, renal. In: StatPearls. Treasure Island: StatPearls Publishing LLC; 2021. NBK538339 [bookaccession]
Gerich JE, Meyer C, Woerle HJ, Stumvoll M (2001) Renal gluconeogenesis: Its importance in human glucose homeostasis. Diabetes Care 24(2):382–391
Gerich JE (2010) Role of the kidney in normal glucose homeostasis and in the hyperglycaemia of diabetes mellitus: therapeutic implications. Diabetic Med 27:136–142
Joven J, Vilella E (1993) Lipoprotein heterogeneity in end-stage renal disease. Kidney Int 43:410–418
Webster AC, Bardhan M (2017) Chronic kidney disease. Lancet 389(10075):1238–1252
Guder WG, Wagner S, Wirthensohn G (1986) Metabolic fuels along the nephron: pathways and intracellular mechanisms of interaction. Kidney Int 29:41–45
Hems R, Ross B (1980) The metabolic fate of lactate in renal cortical tubules. Biochem J 190:27–37
Song P, Onishi A, Koepsell H, Vallon V (2016) Sodium glucose cotransporter SGLT1 as a therapeutic target in diabetes mellitus. Expert Opin Ther Targets 20(9):1109–1125
Blaine J, Chonchol M, Levi M (2015) Renal control of calcium, phosphate, and magnesium homeostasis. Clin J Am Soc Nephrol 10(7):1257–1272
Guertl B, Noehammer C, Hoefler G (2000) Metabolic cardiomyopathies. Int J Exp Pathol 81(6):349–372
Wang Y, Chen X, Song Y, Caballero B, Cheskin LJ (2008) Association between obesity and kidney disease: a systematic review and meta-analysis. Kidney Int 73(1):19–33
Klahr S, Levey AS, Beck GJ et al (1994) The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. Modification of diet in renal disease study group. N Engl J Med 330(13):877–884
Diabetes Control and Complications Trial Research Group, Nathan DM, Genuth S et al (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 329(14):977–986
Slee AD (2012) Exploring metabolic dysfunction in chronic kidney disease. Nutr Metab (Lond) 9(1):1–16
Werner R, Xinyu C (2019) The next era of renal radionuclide imaging: Novel PET radiotracers. Eur J Nucl Med Mol Imaging 46(9):1773–1786
Juillard L, Janier MF, Fouque D et al (2000) Renal blood flow measurement by positron emission tomography using 15O-labeled water. Kidney Int 57(6):2511–2518
Patlak CS, Blasberg RG (1985) Graphical evaluation of blood-to-brain transfer constants from multiple-time uptake data generalizations. J Cereb Blood Flow Metab 5(4):584–590
Rebelos E, Immonen H, Bucci M et al (2019) Brain glucose uptake is associated with endogenous glucose production in obese patients before and after bariatric surgery and predicts metabolic outcome at follow-up. Diabetes Obes Metab 21(2):218–226
Oldgren J, Laurila S, Åkerblom A et al (2021) Effects of 6 weeks of treatment with dapagliflozin, a sodium-glucose co-transporter-2 inhibitor, on myocardial function and metabolism in patients with type 2 diabetes: A randomized, placebo-controlled, exploratory study. Diabetes Obes Metab 23:1505–1517
Immonen H, Hannukainen JC, Iozzo P et al (2014) Effect of bariatric surgery on liver glucose metabolism in morbidly obese diabetic and non-diabetic patients. J Hepatol 60(2):377–383
Ng JM, Bertoldo A, Minhas DS et al (2014) Dynamic PET imaging reveals heterogeneity of skeletal muscle insulin resistance. J Clin Endocrinol Metab 99(1):E102–E106
Dadson P, Landini L, Helmio M et al (2016) Effect of bariatric surgery on adipose tissue glucose metabolism in different depots in patients with or without type 2 diabetes. Diabetes Care 39(2):292–299
Dadson P, Ferrannini E, Landini L et al (2017) Fatty acid uptake and blood flow in adipose tissue compartments of morbidly obese subjects with or without type 2 diabetes: effects of bariatric surgery. Am J Physiol Endocrinol Metab 313(2):E175–E182
Moher D, Shamseer L, Clarke M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4(1):1–9
Institute JB (2020) Critical appraisal tools for use in JBI systematic reviews checklist for prevalence studies. The University of Adelaide, Adelaide
Barrios L, Bergstrom K (2016) Radiolabeled sugars used for PET and SPECT imaging. Curr Radiopharm 9:180–186
Inaba T, Yamashita M, Kawase Y, Nakahashi H, Watanabe H (1989) Quantitative measurement of renal plasma flow by positron emission tomography with oxygen-15 water. Tohoku J Exp Med 159(4):283–289
Nitzschem EU, Choi Y, Killion D, Hoh CK, Hawkins RA, Schelbert R (1993) Quantification and parametric imaging of renal cortical blood flow in vivo based on patlak graphical analysis. Kidney Int 44(5):985–996
Middlekauff HR, Nitzsche EU, Hamilton MA et al (1995) Evidence for preserved cardiopulmonary baroreflex control of renal cortical blood flow in humans with advanced heart failure: a positron emission tomography study. Circulation 92:395–401
Middlekauff HR, Nitzsche EU, Nguyen AH, Hoh CK, Gibbs GG (1997) Modulation of renal cortical blood flow during static exercise in humans. Circ Res 80(1):62–68
Middlekauff HR, Nitzsche EU, Hoh CK et al (2000) Exaggerated renal vasoconstriction during exercise in heart failure patients. Circulation 101(7):784–789
Juillard L, Janier MF, Fouque D et al (2002) Dynamic renal blood flow measurement by positron emission tomography in patients with CRF. Am J Kidney Dis 40(5):947–954. https://doi.org/10.1053/ajkd.2002.36325
Kudomi N, Koivuviita N, Liukko KE et al (2009) Parametric renal blood flow imaging using [15O]H2O and PET. Eur J Nucl Med Mol Imaging 36(4):683–691
Damkjær M, Vafaee M, Braad PE, Petersen H, Høilund-Carlsen PF, Bie P (2012) Renal cortical and medullary blood flow during modest saline loading in humans. Acta physiol 205(4):472–483
Green MA, Hutchins GD (2011) Positron emission tomography (PET) assessment of renal perfusion. Semin Nephrol 31(3):291–299
Koivuviita N, Liukko K, Kudomim N et al (2012) The effect of revascularization of renal artery stenosis on renal perfusion in patients with atherosclerotic renovascular disease. Nephrol Dialysis Transp 27(10):3843–3848
Normand G, Lemoine S, Le Bars D et al (2019) PET [(11)C]acetate is also a perfusion tracer for kidney evaluation purposes. Nucl Med Biol 76–77:10–14
Rebelos E, Dadson P, Oikonen V et al (2019) Renal hemodynamics and fatty acid uptake: effects of obesity and weight loss. Am J Physiol Endocrinol Metab 317(5):E871–E878
Päivärinta J, Oikonen V, Räisänen-Sokolowski A et al (2019) Renal vascular resistance is increased in patients with kidney transplant. BMC Nephrol 20(1):437
Lacy J, Guerrero L, Christian B, Stone C (2010) Renal perfusion with 62cu-ETS in comparison with 15O-water PET. J Nucl Med 51(supplement 2):587–587
Tahari AK, Bravo PE, Rahmim A, Bengel FM (2014) Initial human experience with rubidium-82 renal PET/CT imaging. J Med Imaging Radiat Oncol 58:25–31
Keramida G, Gregg S, Peters AM (2020) Stimulation of the hepatic arterial buffer response using exogenous adenosine: hepatic rest/stress perfusion imaging. Eur Radiol 30(11):5852–5861
Guglielmo P, Ekström S, Strand R et al (2020) Validation of automated whole-body analysis of metabolic and morphological parameters from an integrated FDG-PET/MRI acquisition. Sci Rep 10(1):5331
Jadoul A, Lovinfosse P, Bouquegneau A et al (2020) Observer variability in the assessment of renal F-FDG uptake in kidney transplant recipients. Sci Rep 10(1):4617
Lovinfosse P, Weekers L, Bonvoisin C et al (2016) Fluorodeoxyglucose F(18) positron emission tomography coupled with computed tomography in suspected acute renal allograft rejection. Am J Transplant 16(1):310–316
Werner RA, Ordonez AA, Sanchez-Bautista J et al (2019) Novel functional renal PET imaging with 18F-FDS in human subjects. Clin Nucl Med 44(5):410–411
Derlin T, Gueler F, Bräsen JH et al (2017) Integrating MRI and chemokine receptor CXCR4-targeted PET for detection of leukocyte infiltration in complicated urinary tract infections after kidney transplantation. J Nucl Med 58(11):1831–1837
Geist B, Baltzer P, Fueger B, Hamboeck M, Hacker M, Staudenherz A (2018) Assessing the kidney function parameters glomerular filtration rate and effective renal plasma flow dynamic FDG-PET/MRI in healthy subjects. EJNMMI Res 8:37
Qiao H, Bai J, Chen Y, Tian J (2008) Modeling the excretion of FDG in human kidneys using dynamic PET. Comput Biol Med 38(11):1171–1176. https://doi.org/10.1016/j.compbiomed.2008.09.006
Rasul S, Geist BK, Brath H et al (2020) Response evaluation of SGLT2 inhibitor therapy in patients with type 2 diabetes mellitus using 18F-FDG PET/MRI. BMJ Open Diabetes Res Care 8(1):e001135
Pajenda S, Rasul S, Hacker M, Wagner L, Geist BK (2020) Dynamic 2-deoxy-2[18F] fluoro-D-glucose PET/MRI in human renal allotransplant patients undergoing acute kidney injury. Sci Rep 10(1):8270
Minamimoto R, Takahashi N, Inoue T (2007) FDG-PET of patients with suspected renal failure: Standardized uptake values in normal tissues. Ann Nucl Med 21(4):217–222
Yamashita M, Inaba T, Kawase Y et al (1988) Quantitative measurement of renal function using ga-68-EDTA. Tohoku J Exp Med 155(2):207–208
Ruiz-Bedoya CA, Ordonez AA, Werner RA et al (2020) C-PABA as a PET radiotracer for functional renal imaging: preclinical and first-in-human study. J Nucl Med 61(11):1665–1671
Baldelomar EJ, Reichert DE, Shoghi KI et al (2021) Mapping nephron mass in vivo using positron emission tomography. Am J Physiol Renal Physiol 320(2):F183–F192 (Epub 2020 Dec 7)
Oliveira-Santos M, McMahon G, Castelo-Branco M et al (2020) Renal artery wall 18F-NaF activity and glomerular filtration rate: an exploratory analysis in a high cardiovascular risk population. Nucl Med Commun 41(2):126–132
Boss M, Buitinga M, Jansen TJP, Brom M, Visser EP, Gotthardt M (2020) PET-based human dosimetry of 68ga-NODAGA-exendin-4, a tracer for β-cell imaging. J Nucl Med 61(1):112–116
Naganawa M, Lim K, Nabulsi NB et al (2018) Evaluation of pancreatic VMAT2 binding with active and inactive enantiomers of FFP-DTBZ in healthy subjects and patients with type 1 diabetes. Mol Imaging Biol 20(5):835–845
Garg PK, Lokitz SJ, Truong L et al (2017) Pancreatic uptake and radiation dosimetry of 6-[18F]fluoro-L-DOPA from PET imaging studies in infants with congenital hyperinsulinism. PLoS ONE 12(11):e0186340
Roivainen A, Någren K, Hirvonen J et al (2009) Whole-body distribution and metabolism of [N-methyl-11C](R)-1-(2-chlorophenyl)-N-(1methylpropyl)-3-isoquinolinecarboxamide in humans; an imaging agent for in vivo assessment of peripheral benzodiazepine receptor activity with positron emission tomography. Eur J Nucl Med Mol Imaging 36(4):671–682
Kumar A, Muzik O, Chugani D, Chakraborty P, Chugani HT (2009) PET-derived biodistribution and dosimetry of the benzodiazepine receptor-binding radioligand (11)C-(R)-PK11195 in children and adults. J Nucl Med 51(1):139–144
McParland BJ, Miller MP, Spinks TJ, Kenny LM, Osman S, Cohen PS (2008) The biodistribution and radiation dosimetry of the arg-gly-asp peptide 18F-AH111585 in healthy volunteers. J Nucl Med 49(10):1664–1667
Ribeiro MJ, Ricard M, Lièvre MA, Bourgeois S, Emond P, Syrota A (2007) Whole-body distribution and radiation dosimetry of the dopamine transporter radioligand [(11)C]PE2I in healthy volunteers. Nucl Med Biol 34(4):465–470
Scheinin NM, Tolvanen TK, Wilson IA, Arponen EM, Någren KA, Rinne JO (2007) Biodistribution and radiation dosimetry of the amyloid imaging agent 11C-PIB in humans. J Nucl Med 48(1):128–133
Nishii R, Higashi T, Kagawa S, Okuyama C, Saji H, Yamauchi H (2018) 18F-FPYBF-2, a new F-18 labelled amyloid imaging PET tracer: biodistribution and radiation dosimetry assessment of first-in-man 18F-FPYBF-2 PET imaging. Ann Nucl Med 32(4):256–263
Gormsen LC, Sundelin EI, Jensen JB et al (2016) In vivo imaging of human 11C-metformin in peripheral organs: dosimetry, biodistribution, and kinetic analyses. J Nucl Med 57(12):1920–1926
Roivainen A, Rinne J, Virta J et al (2004) Biodistribution and blood metabolism of 1–11C-methyl-4-piperidinyl n-butyrate inhumans: an imaging agent for in vivo assessment of butyrylcholinesterase activity with PET. J Nucl Med 45(12):2032–2039
Jamar F, Barone R, Mathieu I et al (2003) 86Y-DOTA0)-D-Phe1-Tyr3-octreotide (SMT487)—a phase 1 clinical study: Pharmacokinetics, biodistribution and renal protective effect of different regimens of amino acid co-infusion. Eur J Nucl Med Mol Imaging 30(4):510–518
Ebenhan T, Sathekge MM, Lengana T et al (2018) Ga-NOTA-functionalized ubiquicidin: cytotoxicity, biodistribution, radiation dosimetry, and first-in human PET/CT imaging of infections. J Nucl Med 59(2):334–339
Champion C, Loirec C (2007) Positron follow-up in liquid water: II. Spatial and energetic study for the most important radioisotope used in PET. Phys Med Biol 52:6605–6625
Odudu A, Nery F, Harteveld AA et al (2018) Arterial spin labelling MRI to measure renal perfusion: a systematic review and statement paper. Nephrol Dial Transplant 33(suppl_2):ii15–ii21
Iskandrian AE, Dilsizian V, Garcia EV et al (2018) Myocardial perfusion imaging: lessons learned and work to be done-update. J Nucl Cardiol 25(1):39–52
Meury L, Noël J, Tejedor A, Sénécal J, Gougoux A, Vinay P (1994) Glucose metabolism in dog inner medullary collecting ducts. Ren Physiol Biochem 17(5):246–266
Tian Z, Liang M (2021) Renal metabolism and hypertension. Nat Commun 12(1):1–12
Nuutila P, Koivisto VA, Knuuti J et al (1992) Glucose-free fatty acid cycle operates in human heart and skeletal muscle in vivo. J Clin Invest 89(6):1767–1774
Qiao H, Bai J, Chen Y, Tian J (2008) Modeling the excretion of FDG in human kidneys using dynamic PET. Comput Biol Med 38(11–12):1171–1176
Kaufman DP, Basit H, Knohl SJ. Physiology, glomerular filtration rate. In: StatPearls. Treasure Island: StatPearls Publishing LLC; 2021. NBK500032 [bookaccession].
Landau BR, Spring-Robinson CL, Muzic RF Jr et al (2007) 6-fluoro-6-deoxy-D-glucose as a tracer of glucose transport. Am J Physiol Endocrinol Metab 293(1):E237–E245
Scafoglio C, Hirayama BA, Kepe V et al (2015) Functional expression of sodium-glucose transporters in cancer. Proc Natl Acad Sci U S A 112(30):E4111–E4119
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Latva-Rasku A, Honka MJ, Kullberg J et al (2019) The SGLT2 inhibitor dapagliflozin reduces liver fat but does not affect tissue insulin sensitivity: a randomized, double-blind, placebo-controlled study with 8-week treatment in type 2 diabetes patients. Diabetes Care 42(5):931–937
Phoon RK (2012) Chronic kidney disease in the elderly—assessment and management. Aust Fam Physician 41(12):940–944
Kode V, Karsch H, Osman MM, Muzaffar R (2017) Impact of renal failure on F18-FDG PET/CT scans. Front Oncol 7:155
Bach-Gansmo T, Dybvik J, Adamsen T, Naum A (2012) Variation in urinary excretion of FDG, yet another uncertainty in quantitative PET. Acta Radiol Short Rep 1(8):1–3. https://doi.org/10.1258/arsr.2012.120038 (eCollection 2012)
Toriihara A, Kitazume Y, Nishida H, Kubota K, Nakadate M, Tateishi U (2015) Comparison of FDG-PET/CT images between chronic renal failure patients on hemodialysis and controls. Am J Nucl Med Mol Imaging 5(2):204–211
Hofman M, Binns D, Johnston V et al (2015) 68Ga-EDTA PET/CT imaging and plasma clearance for glomerular filtration rate quantification: comparison to conventional 51Cr-EDTA. J Nucl Med 56(3):405–409
Goethals P, Volkaert A, Vandewielle C, Dierckx R, Lameire N (2000) 55Co-EDTA for renal imaging using positron emission tomography (PET): a feasibility study. Nucl Med Biol 27(1):77–81
Tek CK, Chennu KK, Amancharla YL, Manthri GR, Rapur R, Vishnubotla SK (2017) Utility of 18 F-FDG PET/CT scan to diagnose the etiology of fever of unknown origin in patients on dialysis. Hemodial Int 21(2):224–231
Lawal IO, Popoola GO, Lengana T, Ankrah AO, Ebenhan T, Sathekge M (2019) Diagnostic utility of F-FDG PET/CT in fever of unknown origin among patients with end-stage renal disease treated with renal replacement therapy. Hellenic J Nucl Med 22(1):70–75
Bleeker-Rovers CP, de Sévaux RG, van Hamersvelt HW, Corstens FH, Oyen WJ (2003) Diagnosis of renal and hepatic cyst infections by 18-F-fluorodeoxyglucose positron emission tomography in autosomal dominant polycystic kidney disease. Am J Kidney Dis 41(6):E18-21
Fu Z, Li Z, Huang J et al (2016) High (18)F-FDG uptake in urinary calculi on PET/CT: An unrecognized non-malignant accumulation. Eur J Radiol 85(8):1395–1399
Hanssen O, Erpicum P, Lovinfosse P et al (2017) Non-invasive approaches in the diagnosis of acute rejection in kidney transplant recipients. Part I. in vivo imaging methods. Clin Kidney J 10(1):97–105
Reuter S, Schnockel U, Schroter R et al (2009) Non-invasive imaging of acute renal allograft rejection in rats using small animal F-FDG-PET. PLoS ONE 4:e5296
Aaltonen L, Koivuviita N, Seppänen M et al (2020) Correlation between (18)F-sodium fluoride positron emission tomography and bone histomorphometry in dialysis patients. Bone 134:11526
Funding
Open Access funding provided by University of Turku (UTU) including Turku University Central Hospital. The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
PD, ER, conceptualization. KAA, SL, PD, ER, literature search. KAA, SL, wrote the manuscript. LEJO, ABLM, DM, SL, ER, PD, critically reviewed and edited the manuscript. PD is the guarantor of this work and takes responsibility for the integrity of the data and the accuracy of the information herein presented.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare no potential conflicts of interest relevant to this article.
Ethical approval
This article is based on secondary analysis of existing data and does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Amoabeng, K.A., Laurila, S., Juárez-Orozco, L.E. et al. The utilization of positron emission tomography in the evaluation of renal health and disease. Clin Transl Imaging 10, 59–69 (2022). https://doi.org/10.1007/s40336-021-00469-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-021-00469-2