Abstract
Aim
We aimed to assess the cost effectiveness of four different lipid-lowering strategies for primary prevention of coronary heart disease initiated at ages 30, 40, 50, and 60 years from the UK National Health Service perspective.
Methods
We developed a microsimulation model comparing the initiation of a lipid-lowering strategy to current standard of care (control). We included 458,692 participants of the UK Biobank study. The four lipid-lowering strategies were: (1) low/moderate-intensity statins; (2) high-intensity statins; (3) low/moderate-intensity statins and ezetimibe; and (4) inclisiran. The main outcome was the incremental cost-effectiveness ratio for each lipid-lowering strategy compared to the control, with 3.5% annual discounting using 2021 GBP (£); incremental cost-effectiveness ratios were compared to the UK willingness-to-pay threshold of £20,000–£30,000 per quality-adjusted life-year.
Results
The most effective intervention, low/moderate-intensity statins and ezetimibe, was projected to lead to a gain in quality-adjusted life-years of 0.067 per person initiated at 30 and 0.026 at age 60 years. Initiating therapy at 40 years of age was the most cost effective for all lipid-lowering strategies, with incremental cost-effectiveness ratios of £2553 (95% uncertainty interval: 1270, 3969), £4511 (3138, 6401), £11,107 (8655, 14,508), and £1,406,296 (1,121,775, 1,796,281) per quality-adjusted life-year gained for strategies 1–4, respectively. Incremental cost-effectiveness ratios were lower for male individuals (vs female individuals) and for people with higher (vs lower) low-density lipoprotein-cholesterol. For example, low/moderate-intensity statin use initiated from age 40 years had an incremental cost-effectiveness ratio of £5891 (3822, 9348), £2174 (772, 4216), and was dominant (i.e. cost saving; −2,760, 350) in female individuals with a low-density lipoprotein-cholesterol of ≥ 3.0, ≥ 4.0 and ≥ 5.0 mmol/L, respectively. Inclisiran was not cost effective in any sub-group at its current price.
Conclusions
Low-density lipoprotein-cholesterol lowering from early ages is a more cost-effective strategy than late intervention and cost effectiveness increased with the increasing lifetime risk of coronary heart disease.
Similar content being viewed by others
It is unclear at what age(s), and in which populations, is it cost effective to start lowering cholesterol (low-density lipoprotein-cholesterol) for primary prevention (i.e., first occurrence) of coronary heart disease. |
We show that statin-based lipid-lowering therapies are cost effective for primary prevention of coronary heart disease when initiated from as young as 30 years of age, and cost saving for many clinical populations. |
Low-density lipoprotein-cholesterol lowering from early ages is a more cost-effective strategy than late intervention and cost-effectiveness increases with the increasing lifetime risk of coronary heart disease. The approach to primary prevention of coronary heart disease may improve with a shift to early and sustained lowering of low-density lipoprotein-cholesterol. |
1 Introduction
Coronary heart disease (CHD) remains a leading cause of morbidity and mortality worldwide [1]. An important causal determinant of CHD are low-density lipoproteins (LDL) [2], whereby exposure to high levels of LDL over time exerts a cumulative effect on the risk for CHD (i.e. risk is proportional to both magnitude and duration of exposure) [3]. Concomitantly, there is evidence suggesting that early pharmacological lowering of LDL-cholesterol (LDL-C) leads to a marked reduction in the lifetime risk of CHD, with one study estimating a > 50% reduction in the lifetime risk of atherosclerotic cardiovascular disease with a 50% reduction in LDL-C from age 30 years compared with usual care [4]. Indeed, because current practice is based on 10-year absolute risk estimates, pharmacological lowering of LDL-C is rarely initiated in individuals under 50 years of age [5,6,7], and the potential benefits of lowering LDL-C earlier in life are forgone.
However, whether lowering LDL-C early in life would be cost effective, the age at which to intervene and how this varies for different clinical populations (e.g. by sex and baseline LDL-C level) are unknown. Recently, Kohli-Lynch and colleagues showed, for the first time, that statin use in young adults without CHD in the USA is likely cost effective, especially among male individuals [8]. However, this analysis did not explicitly consider the cumulative causal effect of LDL-C, was based on the US healthcare system and did not explore the available range of pharmacological lipid-lowering strategies (LLS) suitable for primary prevention of CHD. Thus, the optimal LLS and age to intervene to reduce CHD for specific clinical subgroups remain unknown.
These data would ideally be derived from a randomised clinical trial, but such a trial is unlikely to ever be undertaken given that it would take decades and would be prohibitively expensive. Therefore, in the present analysis, we used the cumulative causal effect of LDL-C on CHD derived from Mendelian randomisation analyses (as the best available source of causal evidence) to develop a microsimulation model to assess the cost effectiveness of LDL-C lowering from ages 30, 40, 50 and 60 years with four separate pharmacological LLS from the UK National Health Service perspective.
The four LLS selected were: (1) low/moderate-intensity statins; (2) high-intensity statins; (3) low/moderate-intensity statins and ezetimibe; and (4) inclisiran. Statins are the current mainstay LLS, being efficacious and cheap. However, statin intolerance and side effects occur in an important minority of users, with the risk of these outcomes increasing with increasing statin dose [9]. Ezetimibe offers an option for intensifying LDL-C reduction when used in combination with low/moderate-intensity statins, with this strategy leading to a greater LDL-C reduction and less intolerance-related drug discontinuation, although the treatment cost is higher [10, 11]. Finally, inclisiran (a short interfering RNA therapy directed at proprotein convertase subtilisin/kexin type 9) is injected twice a year and achieves large and sustained LDL-C reductions [12]. The fact that is only has to be administered twice per year may also offer an advantage over the other therapies in terms of adherence [13], which is notoriously low for statins [14]. Other proprotein convertase subtilisin/kexin type 9 inhibitors were not included as, given their more frequent dosing regimes, they are unlikely to improve adherence as much as inclisiran [13], will likely be more difficult to manufacture at the scale required for primary prevention than inclisiran [15], and inclisiran has already been approved for primary prevention of CHD by the US Food and Drug Administration [16].
2 Methods
A complete description of all analyses and data sources used in this study, as well as all analysis syntax, are available in the protocol. All analyses were conducted in Stata, Version 17.0 (StataCorp, College Station, TX, USA).
2.1 Study Population
The population for this study was sourced from the UK Biobank [17], which enrolled over 500,000 participants between 2006 and 2010 from 22 assessment centres across the UK. We included all participants with an available date of birth, LDL-C measurement (for most analyses) and who had not had a myocardial infarction (MI) prior to enrolment (n = 458,692). All participants provided written informed consent at enrolment; individuals who withdrew consent were removed.
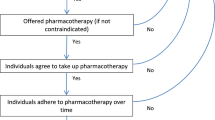
2.2 Model Overview
We developed a microsimulation model that aged UK Biobank participants from 30 to 85 years of age in 0.1-year increments (1-year increments were used in the probabilistic sensitivity analysis). Participants started at age 30 years alive and without established CHD. In each cycle, participants without a prior MI were at risk of non-fatal MI, fatal MI or coronary death, or non-CHD death; if a non-fatal MI occurred, individuals were then at risk of all-cause death (Fig. 1 of the Electronic Supplementary Material [ESM]). The risk for non-fatal MI, fatal MI or coronary death (fatal MI hereafter), and non-CHD death in people without prior MI, and risk for all-cause mortality in people with MI were all derived from the UK Biobank using data from the first assessment to the end of the follow-up (up to 30 September, 2021) via Poisson regression (see protocol p. 26–40). The two outcomes influenced by cumulative LDL-C were non-fatal MI and fatal MI. The incidence of these outcomes was modelled using Poisson regression with spline effects of age, period, and cohort (i.e. age-period-cohort models as described by Carstensen [18]), stratified by sex, using log of person-time as the offset. These risk estimates were then individualised by adjusting these risks based on cumulative LDL-C for each UK Biobank participant in the model. Similar methods for adjusting risk estimates based on cumulative LDL-C have been described for people with familial hypercholesterolaemia and individuals already receiving statin-based therapies [19, 20]. In the present study, risk adjustment by LDL-C was done by projecting the lifetime trajectory of LDL-C for each UK Biobank participant (protocol p. 41–59) under each scenario, and assuming the risk of non-fatal MI and fatal MI was proportional to the mean cumulative LDL-C at a given age. Thus, the risk of non-fatal MI and fatal MI for every individual participant at any given age was calculated using the formula: Ra = R × 0.48(LDLµ−LDLτ), where Ra is the adjusted individual age-specific rate, R is the original age-specific and sex-specific rate for the whole population, LDLµ is the mean cumulative LDL-C for the UK Biobank sample at that given age, and LDLτ is the mean cumulative LDL-C for the specific UK Biobank participant at that age (protocol p. 60–4). The value 0.48 was derived from a Mendelian randomisation study as the relative risk (converted from the original odds ratio of 0.46 presented in the study) of CHD per mmol/L decrease in LDL-C over the lifetime [3]. Thus, in the model, the risks of non-fatal MI and fatal MI were individualised to each participant and assumed to be a function of age, sex and mean cumulative LDL-C. The rate of non-CHD mortality was modelled using an age-period-cohort model [18], and assumed to be insensitive to cumulative LDL-C. All-cause mortality following an MI was modelled using Poisson regression with spline effects of age, time since MI, and age at MI (age minus time since MI), a log-linear effect of time (year), using the log of person-time as the offset [21]. All transition probabilities were divided by 10 when using 0.1-year increments. Because primary prevention was the focus, the effect of LDL-C on outcomes following MI was not incorporated into the model. All inputs to the model and their sources are shown in Table 1 of the ESM.
2.3 Interventions
We simulated four interventions for primary prevention of CHD initiated at four different ages (30, 40, 50 and 60 years) for a total of 16 intervention scenarios. The four interventions were: (1) low/moderate-intensity statins; (2) high-intensity statins; (3) low/moderate-intensity statins and ezetimibe; and (4) inclisiran. The effects of the first three interventions on LDL-C were based on systematic reviews [11, 22], and the complete rationale is explained in the protocol (p. 51–52). We estimated that low/moderate-intensity statin use (based on atorvastatin 10/20 mg) would lower LDL-C by 40% (95% confidence interval 39, 41), high-intensity statin use (based on atorvastatin 40/80 mg) would lower LDL-C by 50% (49, 51), and low/moderate-intensity statin and ezetimibe use would lower LDL-C by 55% (54, 56). For inclisiran, we estimated that a twice-yearly dose would lower LDL-C by 51.5% (95% confidence interval 49.0, 53.9). This was based on a weighted average of the results of the ORION-10 and ORION-11 trials of a 284-mg dose of inclisiran given twice yearly [12]. People were assumed to continue using each intervention following an MI. Once an intervention was initiated, we assumed no other lipid-lowering therapies were added, and that adherence was perfect (for the base case). For the interventions from ages 50 and 60 years, people were able to initiate baseline lipid-lowering therapies before the intervention, in line with current standard of care, but at the age of intervention, everyone in the sample either initiated the intervention therapy or switched from control lipid lowering to the intervention (see protocol p. 41–59; this only affected cumulative LDL-C, not costs, because costs were only tracked from the start of the intervention).
The comparator (i.e. the control scenario) was designed to mimic the current standard of care; thus, we used LDL-C trajectories in the UK Biobank including initiation of lipid-lowering therapies as per standard of care. Details about the current standard of care are available in the protocol (p. 41–42 and 51); briefly, for people without MI, anyone receiving lipid-lowering therapy at the baseline assessment in the UK Biobank was assumed to have initiated statins 5 years prior to their initial assessment and anyone not receiving lipid-lowering therapy at baseline initiated statin therapy at rates of 1 per 1000 person-years for people aged 40–49 years, 15 per 1000 person-years for people aged 50–59 years, and 35 per 1000 person-years for people aged 60 years and above [23]. Additionally, people who initiated statins were assumed to persist on them indefinitely. This meant that 0.2%, 1.7%, 13.5%, 39.3% and 54.9% of female individuals without MI were receiving statins by ages 40, 50, 60, 70 and 80 years, respectively; corresponding numbers in male individuals were 0.5%, 3.5%, 19.9%, 46.6% and 60.5% (Table 2 of the ESM). Statins were initiated following an MI in all people in the control scenario.
To include each intervention and the comparator in the model, the LDL-C trajectory for each UK biobank participant was estimated and the risk of non-fatal MI and fatal MI calculated under each of the scenarios by applying the formula derived from Mendelian Randomisation, described above (protocol p. 60–64). Thus, all interventions were assumed to mediate their effects via lowering LDL-C. These estimates were then used to run the microsimulation (protocol p. 65–146), comparing all results to the control (current LDL-C trajectories). Thus, each participant served as their own control for these simulations.
2.4 Quality of Life
Utilities quantify the perception of health for an individual and are measured on a scale where 0 represents death and 1 represents perfect health. All utilities were derived from the EuroQol-Five Dimensions (EQ-5D) questionnaire [24]. The utility for people without MI was set using the following equation: 0.9454933 + 0.0256466 × male − 0.0002213 × age − 0.0000294 × age2, which was derived from Ara and Brazier’s study using the Health Survey for England, in which they used the EQ-5D UK preference-based algorithm [25]. The chronic utility for people after an MI was set at 0.79 (95% confidence interval 0.73, 0.85), which was derived from a systematic review of utility values for people with MI (likely a mix of both EQ-5D-5L and EQ-5D-3L) [26], and applied to the background age-specific and sex-specific utility for people without MI. A non-fatal MI also incurred an acute disutility of 0.03 (0.01 for three cycles) [27], as previously described [28].
2.5 Healthcare Costs
A National Health Service perspective was adopted [29], and only direct costs were included in the analysis. The cost of acute MI in the UK was set at £2047.31, which was derived directly from the UK National Health Service Cost Schedule in 2021 (Table 3 of the ESM) [30]. Only incident MIs were counted; the cost of recurrent MIs were assumed to be encapsulated in the chronic cost of MI. The chronic cost of MI was set at £4705.45 (standard error: 112.71) for the first 6 months, and £1015.21 (standard error: 171.23) per year thereafter; these values were derived from a cohort study using the Clinical Practice Research Datalink in the UK [31], and inflated to 2021 GBP (£) using the UK National Health Service cost inflation index [32]. Except for inclisiran, medication costs were drawn directly from the National Health Service Electronic Drug Tariff from June 2021 [33]—the cost of lipid-lowering therapy in the control arm was based on the mean price for the most commonly used statins in June 2021 [34], and was set at £19.00 per year; the annual cost of low/moderate-intensity statins was set at £18.39; high-intensity statins set at £27.39; and low/moderate-intensity statins and ezetimibe at £49.31 (protocol p. 77–79) [33, 34]. Inclisiran has special cost arrangements in the UK, and is currently available at a price of £1987.36 per dose (£3974.72 per year) [35].
2.6 Outcomes
We tracked the age of incident MI, number of incident MIs, years of life lived, quality-adjusted life years (QALYs), and acute and chronic healthcare costs in each microsimulation. These outcomes were used to generate our primary outcome, the incremental cost-effectiveness ratio (ICER), defined as the incremental healthcare costs divided by the incremental QALYs for each intervention compared to the control scenario. Results were compared to The UK National Institute for Health and Care Excellence willingness-to-pay threshold range of £20,000–£30,000 per QALY [29]. All analyses were conducted in the overall population, then stratified by sex and LDL-C. The mean LDL-C in each subgroup is shown in Table 4 of the ESM. All health economic outcomes underwent discounting at 3.5% per year (in the base case; this meant calculating the discounting rate in 0.1-year increments for most analyses), as recommended by UK guidelines [29].
2.7 Sensitivity and Scenario Analyses
We conducted one-way sensitivity analyses to determine which of the inputs the model was most sensitive to (protocol p. 147–179). To determine the combined effect of uncertainty on outcomes, we also conducted probabilistic sensitivity analyses using 1000 Monte Carlo simulations based on the uncertainty in the model parameters, drawing values randomly from the distributions listed in Table 1 of the ESM (protocol p. 180–280; distributions of key inputs are shown in Figs. 2–5 of the ESM). This is the source for 95% uncertainty intervals where they are presented.
We also conducted four scenario analyses (protocol p. 281–314). In the first two, we reduced the discounting rate to 0% and 1.5%. For the third, we conducted a scenario analysis in which the efficacy of each intervention in lowering LDL-C was assumed to decrease by 1% per year. This was designed to mimic lower adherence and increasing discontinuation of statin-based LLS over time, while incurring costs (i.e. the worst scenario from the healthcare perspective—people still actively seek out their prescriptions, but do not take them, incurring costs without any benefits). Conversely, for inclisiran, which does not have this problem (i.e. people cannot incur a cost if they do not receive the therapy), this scenario encapsulates the uncertainty associated with its long-term efficacy, which has not been tested beyond 4 years [36], while still incurring costs (i.e. assuming that efficacy decreases while the injection schedule is unchanged). Additionally, for statin-based interventions only, 20% of people were assumed to discontinue statins immediately in this scenario. In the fourth scenario, to estimate the impact of lower adherence, 40% of users of LLT were assumed to discontinue therapy immediately, but not incur costs.
Finally, we conducted a threshold analysis to determine the maximum price at which inclisiran would be cost effective, increasing the price in £1 increments from £10 to £1000 (protocol p. 315–322).
3 Results
3.1 Cost Effectiveness of LLS
The lifetime risk of MI decreased with each younger age of intervention (Figs. 6–7 of the ESM), and absolute reduction was highest for higher risk people (i.e. male individuals and people with higher LDL-C; Figs. 8–11 of the ESM). Concomitantly, the reduction in MIs and gain in years of life lived decreased with the increasing age of intervention for all interventions, whereas the relative gain in QALYs was greatest for interventions started at age 40 years (Table 1, and Tables 5–8 and Fig. 12 of the ESM). For example, in the most effective intervention, low/moderate-intensity statins and ezetimibe, the number of MIs/coronary deaths was reduced by 51.6% with intervention from age 30 years, 41.2% from age 40 years, 28.8% from age 50 years and 16.8% from age 60 years, which corresponded to a relative gain of QALYs of 0.33%, 0.36%, 0.32% and 0.21%, respectively (Table 1). The relative increase in healthcare costs for each intervention also decreased with the increasing age of intervention and the ICER was lowest when intervening at age 40 years for all interventions (Table 1). Nevertheless, low/moderate-intensity statins and high-intensity statins were cost effective (using the lower £20,000 willingness-to-pay threshold) at all ages in all simulations (Fig. 12 of the ESM), and low/moderate-intensity statins and ezetimibe was cost effective if initiated at ages 30, 40 and 50 years (and at 60 years, if the more lenient £30,000 willingness-to-pay threshold is considered). Conversely, inclisiran was not cost effective in the overall population at any age of intervention at its current price.
Results stratified by sex are presented in Tables 9–10 and Fig. 13 of the ESM, and results stratified by sex and LDL-C are presented in Figs. 1, 2 and Tables 2, 3, and Tables 11–16 of the ESM. Quality-adjusted life-years gained in all interventions were higher for male individuals than female individuals, and overall healthcare costs were lower, leading to considerably lower ICERs in male individuals. Stratification by LDL-C showed that the QALY gain increased, and incremental costs decreased, with higher LDL-C (Figs. 1, 2). Indeed, for female individuals with an LDL-C ≥ 5.0 mmol/L, low/moderate-intensity statins were cost saving at all ages in most simulations, and low/moderate-intensity statins and ezetimibe was cost effective across most ages once LDL-C was above 4.0 mmol/L. For male individuals, the majority of simulations showed low/moderate-intensity statins to be cost saving when LDL-C was above 3.0 mmol/L, high-intensity statins to be cost saving once LDL-C was above 4.0 mmol/L (for ages 30, 40 and 50 years), and low/moderate-intensity statins and ezetimibe once LDL-C was above 5.0mmol/L. Inclisiran was not cost effective in any sub-group in any simulation (Figs. 14–15 of the ESM).
Results of 1,000 Monte Carlo simulations for each intervention presented in a common cost-effectiveness plane, by age of intervention and LDL-C for female individuals. Inclisiran is excluded in these figures as the costs were too high to appear on the same axes as the other interventions; see Supplementary Figure 14 for a plot including inclisiran. Solid line: £20,000 per QALY willingness- to-pay threshold; dashed line: £30,000 per QALY willingness-to-pay threshold. LDL-C Low-density lipoprotein cholesterol, QALYs Quality-adjusted life-years.
Results of 1,000 Monte Carlo simulations for each intervention presented in a common cost-effectiveness plane, by age of intervention and LDL-C for male individuals. Inclisiran is excluded in these figures as the costs were too high to appear on the same axes as the other interventions; see Supplementary Figure 15 for a plot including inclisiran. Solid line: £20,000 per QALY willingness- to-pay threshold; dashed line: £30,000 per QALY willingness-to-pay threshold. LDL-C Low-density lipoprotein cholesterol, QALYs Quality-adjusted life-years.
3.2 One-Way Sensitivity Analyses
Results from the one-way sensitivity analyses are presented in Fig. 16 of the ESM. For the low/moderate-intensity and high-intensity statin interventions from ages 30, 40 and 50 years, chronic MI cost was the most influential factor on the ICER. For low/moderate-intensity statins and ezetimibe and inclisiran from ages 30, 40 and 50 years, the most influential factor was the utility without MI, followed by the chronic utility value for people with MI. Nevertheless, even the most influential factors did not materially affect the ICERs. While the most influential factors differed by sex and LDL-C, as with the overall analysis, even the most influential factors had very little impact on ICERs.
3.3 Scenario Analyses
The discounting rate had a substantial impact on the results, especially at younger ages (results from the base case are shown for comparison in Table 17 of the ESM; from scenario analyses 1 and 2 in Tables 18 and 19 of the ESM). For example, in the base case, the QALY gain with low/moderate-intensity statin use from age 30 years was 21,782 (0.23% gain relative to control), whereas with 0% and 1.5% discounting, this value was 93,374 (0.47%) and 48,912 (0.35%). Conversely, for low/moderate-intensity statin use from age 60 years, the QALY gain was 6519 (0.12%) in the base case, and 12,361 (0.16%) and 9333 (0.14%) with 0% and 1.5% discounting, respectively. Moreover, incremental healthcare costs were much lower with lower discounting rates, leading to considerably lower ICERs at younger ages: at 3.5% discounting, ICERs for interventions from age 30 years were £3783, £6000, £13,467 and £1,578,096 per QALY gained for low/moderate-intensity statins, high-intensity statins, low/moderate-intensity statins and ezetimibe, and inclisiran, respectively; and at 0% discounting, the corresponding ICERs were −£390 (dominant), £845, £4635 and £790,823 per QALY, and intervention at age 30 years led to lower ICERs than intervention at age 40 years (Table 18 of the ESM).
When the intervention was assumed to decrease in efficacy by 1% per year (and 20% of the cohort immediately discontinued statin-based interventions, while still incurring costs), QALYs gained were lower and incremental healthcare costs higher, leading to higher ICERs than the base case (Table 20 of the ESM). Nevertheless, low/moderate-intensity statins and high-intensity statins remained cost effective at all ages, and low/moderate-intensity statins and ezetimibe remained cost effective from age 40 and 50 years (and age 30 years, if the £30,000 willingness-to-pay threshold is considered). When 40% of people were assumed to immediately cease LLT at initiation (with no medication costs incurred), incremental QALYs and healthcare costs were lower, and ICERs were slightly higher than the base case, but all interventions that were cost effective in the base case were also cost effective in this scenario (Table 21 of the ESM).
Finally, the threshold analyses indicated that inclisiran (284-mg dose given twice yearly) would be cost effective at annual prices that ranged from £31 in all female individuals from age 60 years, using the £20,000 per QALY gained willingness-to-pay threshold, to £451 in male individuals with an LDL-C ≥ 5.0 mmol/L from age 40 years, using the £30,000 per QALY gained willingness-to-pay threshold (the current annual price is £3974.72; Table 22 of the ESM).
4 Discussion
In the present study, we have shown that LLS initiated earlier are more cost effective than LLS initiated later in life. Moreover, because absolute risk is higher in male individuals and people with higher LDL-C, cost effectiveness improves by targeting LLS to these sub-groups. Indeed, some of the statin-based LLS were cost saving in people with high LDL-C, although they were also cost effective at all ages for most sub-groups. Inclisiran was not cost effective in any subgroup or any simulation. These results demonstrate that statin-based LLS are a highly cost-effective method of reducing the lifetime risk of CHD when initiated from as young as 30 years of age, and support a shift in the approach to primary prevention of CHD away from short-term absolute risk estimates to early and sustained lowering of LDL-C.
Currently, pharmacological lowering of LDL-C for primary prevention of CHD is rarely used in individuals aged under 50 years [7], whereas decades of evidence [2, 4], as well as our model, suggest that intervening in early adulthood would be the most efficacious time to intervene. We extend this evidence by showing that early intervention is also a more cost-effective strategy than initiating pharmacological lowering of LDL-C later in life. Current practice for initiating pharmacological LDL-C lowering in primary prevention is based largely on the calculation of a 10-year absolute risk of CHD [5, 6]; however, because older age is the predominant determinant of risk in the short term, while the development of atherosclerosis begins early in life [37, 38], this method of determining treatment initiation forgoes the benefits that could accrue if practice were to change to earlier lowering of LDL-C so that the cumulative accumulation of coronary plaque is attenuated. Our results add to the health economic justification for such a shift in clinical practice [8], as discussed in the World Heart Federation Cholesterol Roadmap 2022 [4].
Furthermore, our results suggest that early assessment of LDL-C and the lifetime risk of CHD would be useful in determining which interventions are cost effective for which clinical sub-groups, and at what age to intervene depending on the absolute lifetime risk of CHD. While we have presented results combined by sex and across all LDL-C levels to illustrate the effect of age of intervention on cost effectiveness, it would be rare to make clinical decisions without considering sex and LDL-C. Indeed, our results should not be taken to suggest that everyone can or should receive a pharmacological LLS from early in life—further research will be required into lifestyle interventions and to target treatment more effectively. For example, future studies could include other cardiovascular risk factors and examine the cost effectiveness of lifestyle interventions and pharmacological LLT by age in finer increments (than 10-year intervals). Moreover, because primary prevention strategies often by necessity target large numbers of people, the economic considerations move beyond cost effectiveness to a consideration of the overall cost of the intervention. It is therefore of significance that in several sub-groups, many of the statin-based LLS were cost saving.
It is worth also noting that, analogous to 10-year risk estimates biasing treatment towards older ages, by design, high discounting rates favour treatment decisions that focus on the short-term—we saw a large increase in the estimates of QALYs gained and healthcare costs prevented by the interventions when the discounting rate was decreased. It has been argued that constant discounting practices for longer term primary prevention strategies, where benefits are not expected to accrue for many decades, are unfair to future generations and may need to be re-considered [39].
Importantly, the statin-based LLS remained cost effective even when non-adherence was simulated. Nevertheless, statins have notoriously low long-term adherence [14, 40], and the efficacy of long-term LLS will require more research and interventions to ensure adherence to this therapy improves, although if the effect of LDL-C is cumulative and causal, it would be expected that benefits still accrue if statins are only taken for a period. Low adherence to statins was the predominant motivation for including inclisiran in our study [13]. However, inclisiran was not cost effective in any simulation, and the threshold analysis indicated that the maximum cost-effective price (£451 in male individuals with an LDL-C ≥5.0 mmol/L) is substantially lower than the current price (£3974.72). Moreover, these estimates were based on a comparison to current practice, whereas, because statin-based interventions were cost effective, the appropriate comparator is likely to change to one of the statin-based interventions we simulated, implying that inclisiran will need to be priced closer to statins if it is to be cost effective for primary prevention of CHD. Indeed, even in a secondary prevention population, inclisiran would need to be made available at a greatly reduced price (compared to other proprotein convertase subtilisin/kexin type 9 inhibitors) to be considered cost effective [41].
4.1 Limitations
There are important limitations to the present work. First, the UK Biobank suffers from a significant “healthy volunteer” selection bias [42], meaning we likely underestimated the absolute lifetime risk of MI and consequently underestimated the cost effectiveness of therapies, although this has little effect on our conclusions for statin-based interventions, which were highly cost effective in most populations. Nevertheless, the lifetime risk of MI in the control scenario presented here appears relatively consistent with the available literature (see discussion in the protocol p. 74).
Second, we did not include other modifiable risk factors in our estimation of lifetime risk, which could further target treatments and improve cost effectiveness. Incorporating MR-based estimates of lifetime risk in these models is an important area of further study.
Third, while the microsimulation model was based on causal evidence from Mendelian randomisation, the results cannot be considered as robust as those based on a randomised clinical trial. Indeed, the LDL-C reductions used here (37–52%) were far greater than the variation naturally present and used in Mendelian randomisation (~0–5% per allele [3]), meaning our results rely on extrapolation of these effect estimates under the assumption that LDL-C does indeed have a log-linear relationship with CHD risk across all values of LDL-C [43]. Thus, if interventions such as these are implemented, monitoring of long-term safety and effectiveness will be more important than usual. Notably, in certain high-risk populations, very long-term lipid lowering has been shown to be safe and effective [44], and the assumption that LDL-C has a log-linear relationship with CHD risk is supported by extensive evidence [2].
Fourth, to be conservative, we only considered the effect of LLS on MI and coronary death—it is likely that other conditions (such as ischaemic stroke, peripheral artery diseases, and abdominal aortic aneurysm [45,46,47]) would be impacted by lowering of LDL-C, which in turn would raise the overall clinical benefits and improve the cost effectiveness. Nevertheless, the causal effect of LDL-C on these outcomes is much weaker than for CHD (e.g. a 1-mmol/L increase in LDL-C over the lifetime is associated with a 12% increase in the odds of ischaemic stroke [48], compared with 117% for CHD [3]). Further, we have not considered the effect of LDL-C on outcomes following MI, which again would improve cost effectiveness. Conversely, we have not considered side effects, which would worsen cost effectiveness.
Fifth, consistent with the National Institute for Health and Care Excellence guidelines [29], we only considered healthcare costs associated with MI in this model. As healthcare costs increase considerably with age [49], it is unclear whether improved survival as a result of LLS would offset some of the cost savings from lower rates of MI. This is an area for further study. Sixth, we did not source healthcare costs or utility values directly from the UK Biobank sample as these were not available; others have used algorithms to derive utility scores directly from the UK Biobank [50], but we opted to use EQ5D-based measures of utility in this study. Finally, we did not consider the disutility associated with medicalising otherwise healthy young adults or, similarly, the acceptability of the LLS that were simulated.
5 Conclusions
Low-density lipoprotein-cholesterol lowering from early ages leads to a considerably greater reduction in the lifetime risk of MI than intervention at later ages and is also more cost effective. Cost effectiveness increased with increasing LDL-C and was higher for male individuals than female individuals (groups with a higher lifetime risk of CHD). It may be prudent to reconsider current approaches to primary prevention of CHD that focus on a 10-year absolute risk and instead focus more on early and sustained lowering of LDL-C for people with a higher lifetime risk of CHD.
References
Roth GA, Mensah GA, Johnson CO, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982–3021.
Ference BA, Ginsberg HN, Graham I, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies: a consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017;38(32):2459–72.
Ference BA, Bhatt DL, Catapano AL, et al. Association of genetic variants related to combined exposure to lower low-density lipoproteins and lower systolic blood pressure with lifetime risk of cardiovascular disease. JAMA. 2019;322(14):1381–91.
Ray KK, Ference BA, Séverin T, et al. World heart federation cholesterol roadmap 2022. Glob Heart. 2022;17(1):75.
Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation. 2019;140(11):e596-646.
Visseren FLJ, Mach F, Smulders YM, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice: developed by the Task Force for Cardiovascular Disease Prevention in Clinical Practice with representatives of the European Society of Cardiology and 12 medical societies with the special contribution of the European Association of Preventive Cardiology (EAPC). Eur Heart J. 2021;42(34):3227–337.
Keeffe AG, Petersen I, Nazareth I. Initiation rates of statin therapy for the primary prevention of cardiovascular disease: an assessment of differences between countries of the UK and between regions within England. BMJ Open. 2015;5(3): e007207.
Kohli-Lynch CN, Bellows BK, Zhang Y, et al. Cost-effectiveness of lipid-lowering treatments in young adults. J Am Coll Cardiol. 2021;78(20):1954–64.
Bytyçi I, Penson PE, Mikhailidis DP, et al. Prevalence of statin intolerance: a meta-analysis. Eur Heart J. 2022;43(34):3213–23.
Kim BK, Hong SJ, Lee YJ, et al. Long-term efficacy and safety of moderate-intensity statin with ezetimibe combination therapy versus high-intensity statin monotherapy in patients with atherosclerotic cardiovascular disease (RACING): a randomised, open-label, non-inferiority trial. Lancet. 2022;400(10349):380–90.
Ambegaonkar BM, Tipping D, Polis AB, et al. Achieving goal lipid levels with ezetimibe plus statin add-on or switch therapy compared with doubling the statin dose: a pooled analysis. Atherosclerosis. 2014;237(2):829–37.
Ray KK, Wright RS, Kallend D, et al. Two phase 3 trials of inclisiran in patients with elevated LDL cholesterol. N Engl J Med. 2020;382(16):1507–19.
Gencer B, Mach F. Inclisiran in primary prevention: reality or fiction? Eur Heart J. 2022;43(48):5058–60.
Talic S, Marquina C, Ofori-Asenso R, et al. Switching, persistence and adherence to statin therapy: a retrospective cohort study using the Australian National Pharmacy Data. Cardiovasc Drugs Ther. 2022;36(5):867–77.
Wellcome. Expanding access to monoclonal antibody-based products: a global call to action. Available from: https://wellcome.org/sites/default/files/expanding-access-to-monoclonal-antibody-based-products.pdf. [Accessed 27 Jun 2023].
Leqvio prescribing information. East Hanover, NJ: Novartis Pharmaceuticals Corp; 2023. Available from: https://www.novartis.com/us-en/sites/novartis_us/files/leqvio.pdf. [Accessed 16 Jul 2023].
Sudlow C, Gallacher J, Allen N, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12(3): e1001779.
Carstensen B. Age-period-cohort models for the Lexis diagram. Stat Med. 2007;26(15):3018–45.
Ademi Z, Norman R, Pang J, et al. Health economic evaluation of screening and treating children with familial hypercholesterolemia early in life: many happy returns on investment? Atherosclerosis. 2020;304:1–8.
Marquina C, Morton J, Zomer E, et al. Lost therapeutic benefit of delayed low-density lipoprotein cholesterol control in statin-treated patients and cost-effectiveness analysis of lipid-lowering intensification. Value Health. 2023;26(4):498–507.
Carstensen B, Rønn PF, Jørgensen ME. Prevalence, incidence and mortality of type 1 and type 2 diabetes in Denmark 1996–2016. BMJ Open Diabetes Res Care. 2020;8(1): e001071.
Adams SP, Tsang M, Wright JM. Lipid-lowering efficacy of atorvastatin. Cochrane Database Syst Rev. 2015;2015(3):8226.
O’Keeffe AG, Nazareth I, Petersen I. Time trends in the prescription of statins for the primary prevention of cardiovascular disease in the United Kingdom: a cohort study using The Health Improvement Network primary care data. Clin Epidemiol. 2016;8:123–32.
Rabin R, Oemar M, Oppe M, et al. EQ-5D-5L user guide: basic information on how to use the EQ-5D-5L instrument. Rotterdam: EuroQol Group; 2011; p. 22.
Ara R, Brazier JE. Populating an economic model with health state utility values: moving toward better practice. Value Health. 2010;13(5):509–18.
Betts MB, Rane P, Bergrath E, et al. Utility value estimates in cardiovascular disease and the effect of changing elicitation methods: a systematic literature review. Health Qual Life Outcomes. 2020;18(1):251.
Lewis EF, Li Y, Pfeffer MA, et al. Impact of cardiovascular events on change in quality of life and utilities in patients after myocardial infarction: a VALIANT study (valsartan in acute myocardial infarction). JACC Heart Fail. 2014;2(2):159–65.
Morton JI, Marquina C, Shaw JE, et al. Projecting the incidence and costs of major cardiovascular and kidney complications of type 2 diabetes with widespread SGLT2i and GLP-1 RA use: a cost-effectiveness analysis. Diabetologia. 2023;66(4):642–56.
National Institute for Health and Clinical Excellence. Guide to the methods of technology appraisal. London: National Institute for Health and Clinical Excellence (NICE); 2013.
National Health Service. 2020/21 national cost collection for the NHS. Available from: https://www.england.nhs.uk/costing-in-the-nhs/national-cost-collection/. [Accessed 1 Nov 2022].
Danese MD, Gleeson M, Kutikova L, et al. Estimating the economic burden of cardiovascular events in patients receiving lipid-modifying therapy in the UK. BMJ Open. 2016;6(8): e011805.
Personal Social Services Research Unit. Unit costs of health and social care 2021. V Sources of Information. 15. Inflation indices. Available from: https://www.pssru.ac.uk/project-pages/unit-costs/unit-costs-of-health-and-social-care-2021/. [Accessed 1 Nov 2022].
National Health Service. Prescription services: NHS electronic drug tariff June 2021. Available from: https://www.nhsbsa.nhs.uk/sites/default/files/2021-05/Drug%20Tariff%20June%202021.pdf [Accessed 25 Nov 2022].
National Health Service. English prescribing dataset June 2021. Available from: https://opendata.nhsbsa.net/dataset/english-prescribing-data-epd. [Accessed 25 Nov 2022].
National Health Service Dictionary of Medicines and Devices. Actual Medicinal Product pack (AMPP). Leqvio 284mg/1.5ml solution for injection pre-filled syringes (Novartis Pharmaceuticals UK Ltd) 1 pre-filled disposable injection. Available from: https://services.nhsbsa.nhs.uk/dmd-browser/ampp/view/184240. [Accessed 2 Dec 2022].
Ray KK, Troquay RPT, Visseren FLJ, et al. Long-term efficacy and safety of inclisiran in patients with high cardiovascular risk and elevated LDL cholesterol (ORION-3): results from the 4-year open-label extension of the ORION-1 trial. Lancet Diabetes Endocrinol. 2023;11(2):109–19.
Tuzcu EM, Kapadia SR, Tutar E, et al. High prevalence of coronary atherosclerosis in asymptomatic teenagers and young adults: evidence from intravascular ultrasound. Circulation. 2001;103(22):2705–10.
Strong JP, Malcom GT, McMahan CA, et al. Prevalence and extent of atherosclerosis in adolescents and young adults: implications for prevention from the Pathobiological Determinants of Atherosclerosis in Youth Study. JAMA. 1999;281(8):727–35.
Attema AE, Brouwer WBF, Claxton K. Discounting in economic evaluations. Pharmacoeconomics. 2018;36(7):745–58.
Chen S, Huang S, Shau W-Y, et al. Long-term statin adherence in patients after hospital discharge for new onset of atherosclerotic cardiovascular disease: a population-based study of real world prescriptions in Taiwan. BMC Cardiovasc Disord. 2019;19(1):62.
Kam N, Perera K, Zomer E, et al. Inclisiran as adjunct lipid-lowering therapy for patients with cardiovascular disease: a cost-effectiveness analysis. Pharmacoeconomics. 2020;38(9):1007–20.
Fry A, Littlejohns TJ, Sudlow C, et al. Comparison of sociodemographic and health-related characteristics of UK Biobank participants with those of the general population. Am J Epidemiol. 2017;186(9):1026–34.
Burgess S, Butterworth A, Malarstig A, et al. Use of Mendelian randomisation to assess potential benefit of clinical intervention. BMJ. 2012;345:2.
Luirink IK, Wiegman A, Kusters DM, et al. 20-Year follow-up of statins in children with familial hypercholesterolemia. N Engl J Med. 2019;381(16):1547–56.
Allara E, Morani G, Carter P, et al. Genetic determinants of lipids and cardiovascular disease outcomes. Circ Genom Precis Med. 2019;12(12): e002711.
Levin MG, Zuber V, Walker VM, et al. Prioritizing the role of major lipoproteins and subfractions as risk factors for peripheral artery disease. Circulation. 2021;144(5):353–64.
Hindy G, Engström G, Larsson SC, et al. Role of blood lipids in the development of ischemic stroke and its subtypes. Stroke. 2018;49(4):820–7.
Falcone GJ, Kirsch E, Acosta JN, et al. Genetically elevated LDL associates with lower risk of intracerebral hemorrhage. Ann Neurol. 2020;88(1):56–66.
Papanicolas I, Marino A, Lorenzoni L, et al. Comparison of health care spending by age in 8 high-income countries. JAMA Netw Open. 2020;3(8): e2014688.
Harrison S, Dixon P, Jones HE, et al. Long-term cost-effectiveness of interventions for obesity: a Mendelian randomisation study. PLoS Med. 2021;18(8): e1003725.
Acknowledgements
This research has been conducted using the UK Biobank Resource under Application Number 88775. This study used linked data from NHS England. Copyright © (2023), NHS England. Re-used with the permission of the NHS England [and/or UK Biobank]. All rights reserved. This research used data assets made available by National Safe Haven as part of the Data and Connectivity National Core Study, led by Health Data Research UK in partnership with the Office for National Statistics and funded by UK Research and Innovation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This work was supported by the National Health and Medical Research Council Ideas Grants Application ID: 2012582. Jedidiah I. Morton and Zanfina Ademi were supported by the National Health and Medical Research Council Ideas Grants Application ID: 2012582. The funder had no input into the design of the study or decision to submit for publication.
Conflicts of Interest
Gerald F. Watts declares financial support for research, conference travel or advisory boards from Amgen, Arrowhead, Novartis, Pfizer, Sanofi, Esperion and CRISPR Therapeutics outside of the submitted work. Sophia Zoungas reports payment to Monash University from Eli Lilly Australia Ltd, Boehringer-Ingelheim, MSD Australia, AstraZeneca, Novo Nordisk, Sanofi and Servier outside of the submitted work. Danny Liew declares previous grants, participation in advisory boards and receipt of honoraria from AbbVie, Amgen, Astellas, AstraZeneca, Bristol-Myers Squibb, Edwards Lifesciences, Novartis, Pfizer, Sanofi and Shire outside of the submitted work. Zanfina Ademi, Jedidiah I. Morton, Clara Marquina and Melanie Lloyd have no conflicts of interest that are directly relevant to the content of this article.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
Data from the UK Biobank study were used for this study. The dataset is accessible to researchers via https://www.ukbiobank.ac.uk/register-apply/.
Code Availability
All analysis syntax is available at https://github.com/jimb0w/LDL and in the protocol (Supplementary file 3).
Authors’ Contributions
JIM contributed to the study design, constructed the model, performed the analysis and literature search, contributed to acquisition and interpretation of data, wrote the protocol, and wrote and revised the manuscript. JIM is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. ZA is the senior author and obtained funding, conceived the study, supervision, contributed to the study design, acquisition and interpretation of data, and revision of the manuscript. All other authors contributed to the study design, interpretation of data, and revision of the manuscript. All authors read and approved the final manuscript and made the decision to submit for publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Morton, J.I., Marquina, C., Lloyd, M. et al. Lipid-Lowering Strategies for Primary Prevention of Coronary Heart Disease in the UK: A Cost-Effectiveness Analysis. PharmacoEconomics 42, 91–107 (2024). https://doi.org/10.1007/s40273-023-01306-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-023-01306-2