Abstract
Background
Medication errors (MEs) in older people are of importance due to global aging patterns. Following on from aging-related changes in pharmacokinetics, pharmacodynamics, and the potential presence of multiple co-morbidities treated with polypharmacy, older people are highly vulnerable to the effects and consequences of MEs.
Objective
The primary outcome of this study was to systematically review studies on the incidence and categories of MEs in older people. Secondary outcomes included economic and clinical consequences of MEs in older people, risk factors for MEs in older people, and medications involved.
Methods
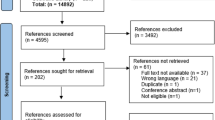
A comprehensive, electronic search was conducted using PubMed, EBSCOhost, OvidMedline and Proquest central databases for studies evaluating MEs in older people published in peer-reviewed journals before November 2017. A secondary manual search was also conducted by checking the bibliographies of included studies to identify other relevant studies. There was no limitation imposed on the language, time of publication, or the setting in which the study was carried out. The quality of identified studies was assessed based on 17 criteria adopted from Alsulami et al. and Metsälä et al. The results were categorized using the phases of medication use when the error was detected or occurred.
Results
Eighteen studies met the inclusion criteria with a total of 467,193 participants from 11 countries. Identified MEs were administration errors [number of times ME subcategory was reported (n = 7); error frequency rate 1.2–59.0%], prescribing errors (n = 7; 1.6–49.7%), transcribing errors (n = 5; 15.0–70.2%), reconciliation errors (n = 4; 5.0–53.6%), and dispensing errors (n = 2; 2.0–14.0%). People with polypharmacy had the highest tendency of MEs. Three studies reported severe clinical consequences from MEs ranging from 2.9% to 13.0%. The main category of medications involved in MEs were cardiovascular medications (n = 15); nervous system medications (n = 11); and medications for the alimentary tract and metabolism (n = 8).
Conclusions
Administration and prescribing errors were the most frequently reported MEs in older people. Medication classes that were most commonly reported in the context of MEs in older people were cardiovascular medications and nervous system medications. We identified polypharmacy as a risk factor for MEs, which was found to correlate with the number of MEs in many stages of medication use. A lack of studies from Asia, Latin America, and Africa highlights the need for future research in these regions.
PROSPERO registration number
CRD42016042975.

Similar content being viewed by others
References
National Coordinating Council for Medication Error Preventing and Reporting: definition of medication errors. Available from http://www.nccmerp.org/about-medication-errors Accessed 11 Oct 2017.
Shahrokhi A, Ebrahimpour F, Ghodousi A. Factors effective on medication errors: a nursing view. J Res Pharm Pract. 2013;2(1):18–23.
U.S. Department of Health & Human Services: Quality and Patient Safety. 2016.
Merle L, Laroche ML, Dantoine T, et al. Predicting and preventing adverse drug reactions in the very old. Drugs Aging. 2005;22(5):375–92.
Maher RL, Hajjar ER. Medication errors in the ambulatory elderly. Aging Health. 2012;8(2):127–35.
Tjia J, Velten SJ, Parsons C, et al. Studies to reduce unnecessary medication use in frail older adults: a systematic review. Drugs Aging. 2013;30(5):285–307.
Fulton MM, Allen ER. Polypharmacy in the elderly: a literature review. J Am Acad Nurse Pract. 2005;17(4):123–32.
Alsulami Z, Conroy S, Choonara I. Medication errors in the Middle East countries: a systematic review of the literature. Eur J Clin Pharmacol. 2013;69(4):995–1008.
Salmasi S, Khan TM, Hong YH et al: Medication errors in the Southeast Asian countries: A systematic review. PLoS One. 2015; 10(9). https://doi.org/10.1371/journal.pone.0136545.
Krzyzaniak N, Bajorek B. Medication safety in neonatal care: a review of medication errors among neonates. Ther Adv Drug Saf. 2016;7(3):102–19.
Ghaleb MA, Barber N, Franklin BD, et al. Systematic review of medication errors in pediatric patients. Ann Pharmacother. 2006;40(10):1766–76.
Miller MR, Robinson KA, Lubomski LH, et al. Medication errors in paediatric care: a systematic review of epidemiology and an evaluation of evidence supporting reduction strategy recommendations. Qual Saf Health Care. 2007;16(2):116–26.
Metsälä E, Vaherkoski U. Medication errors in elderly acute care—a systematic review. Scand J Caring Sci. 2014;28(1):12–28.
(UNFPA) UNPF: Ageing in the twenty-first century: a celebration and a challenge. In: UNFPA, New York, and HelpAge International (HAI); 2012.
Bennett S: WHO launches global effort to halve medication-related errors in 5 years. Available online: http://www.who.int/mediacentre/news/releases/2017/medication-related-errors/en/. Accessed 7 Dec 2017.
Beers MH, Ouslander JG, Rollingher I, et al. Explicit criteria for determining inappropriate medication use in nursing home residents. UCLA Division of Geriatric Medicine. Arch Intern Med. 1991;151(9):1825–32.
Cecile M, Seux V, Pauly V, et al. Accidents iatrogènes médicamenteux chez le sujet âgé hospitalisé en court séjour gériatrique: étude de prévalence et des facteurs de risques. Rev Med Interne. 2009;30(5):393–400.
Raimbault-Chupin M, Spiesser-Robelet L, Guir V, et al. Drug related problems and pharmacist interventions in a geriatric unit employing electronic prescribing. Int J Clin Pharm. 2013;35(5):847–53.
Kelly J, Wright D. Medicine administration errors and their severity in secondary care older persons’ ward: a multi-centre observational study. J Clin Nurs. 2012;21(13–14):1806.
Fahimi F, Baniasadi S, Najafi Zadeh K. Dose switch to another dosage form of Neoral increase the risk of medication error? Ann Transplant. 2009;14(4):58–60.
Fahimi F, Abbasi Nazari M, Abrishami R, et al. Transcription errors observed in a teaching hospital. Arch Iran Med. 2009;12(2):173–5.
World Health Organisation: Action on patient safety (High 5′s). In: Medication Reconciliation. vol. 1. Geneva: World Alliance for Patient Safety; 2010.
Abdullah DC, Ibrahim NS, Ibrahim MIM. Medication errors among geriatrics at the outpatient pharmacy in a teaching hospital in Kelantan. Malays J Med Sci. 2004;11(2):52–8.
Moro Agud M, Menendez Colino R, Mauleon Ladrero MD, et al. Analysis of an electronic medication reconciliation and information at discharge programme for frail elderly patients. Int J Clin Pharm. 2016;38(4):996–1001.
Beckett RD, Crank CW, Wehmeyer A. Effectiveness and feasibility of pharmacist-led admission medication reconciliation for geriatric patients. J Pharm Pract. 2012;25(2):136–41.
Midlov P, Bergkvist A, Bondesson A, et al. Medication errors when transferring elderly patients between primary health care and hospital care. Pharm World Sci. 2005;27(2):116–20.
Quelennec B, Beretz L, Paya D, et al. Potential clinical impact of medication discrepancies at hospital admission. Eur J Intern Med. 2013;24(6):530–5.
Somers A, Robays H, De Paepe P, et al. Evaluation of clinical pharmacist recommendations in the geriatric ward of a Belgian university hospital. Clin Interv Aging. 2013;8:703–9.
van den Bemt P, Idzinga JC, Robertz H, et al. Medication administration errors in nursing homes using an automated medication dispensing system. J Am Med Inform Assoc. 2009;16(4):486–92.
Verrue CL, Mehuys E, Somers A, et al. Medication administration in nursing homes: pharmacists’ contribution to error prevention. J Am Med Dir Assoc. 2010;11(4):275–83.
Young HM, Gray SL, McCormick WC, et al. Types, prevalence, and potential clinical significance of medication administration errors in assisted living. J Am Geriatr Soc. 2008;56(7):1199–205.
Cornish PL, Knowles SR, Marchesano R, et al. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med. 2005;165(4):424–9.
Ernawati DK, Lee YP, Hughes JD. Nature and frequency of medication errors in a geriatric ward: an Indonesian experience. Ther Clin Risk Manag. 2014;10:413–21.
Steinman MA, Miao Y, Boscardin WJ, et al. Prescribing quality in older veterans: a multifocal approach. J Gen Intern Med. 2014;29(10):1379–86.
Picone DM, Titler MG, Dochterman J, et al. Predictors of medication errors among elderly hospitalized patients. Am J Med Qual. 2008;23(2):115–27.
Ben-Yehuda A, Bitton Y, Sharon P, et al. Risk factors for prescribing and transcribing medication errors among elderly patients during acute hospitalization: a cohort, case-control study. Drugs Aging. 2011;28(6):491–500.
Szczepura A, Wild D, Nelson S. Medication administration errors for older people in long-term residential care. BMC Geriatr. 2011;11(1):1–10.
Salmasi S, Wimmer BC, Khan TM, et al. A proposed stepwise approach to reducing medication errors in older people. Res Social Adm Pharm. 2017. https://doi.org/10.1016/j.sapharm.2017.02.015.
Manser T, Foster S. Effective handover communication: an overview of research and improvement efforts. Best Pract Res Clin Anaesthesiol. 2011;25(2):181–91.
Fan JH, Lyons SA, Goodman MS, et al. Relationship between health literacy and unintentional and intentional medication nonadherence in medically underserved patients with type 2 diabetes. Diabetes Educ. 2016;42(2):199–208.
International Monetery Fund: Representative exchange rates for selected currencies. Available online: https://www.imf.org/external/np/fin/data/rms_rep.aspx. Accessed 5 Sept 2016.
National Coordinating Council for Medication Error Reporting and Prevention: Types of Medication Errors. NCC MERP Index for Categorizing Medication Errors. Available from: http://www.nccmerp.org/types-medication-errors. Accessed 9 December 2017. 2001.
Kohn LT, Corrigan J, Donaldson MS: To err is human: building a safer health system. 2000.
Ali Raza J, Movahed A. Use of cardiovascular medications in the elderly. Int J Cardiol. 2002;85(2–3):203–15.
Kaufmann CP, Tremp R, Hersberger KE, et al. Inappropriate prescribing: a systematic overview of published assessment tools. Eur J Clin Pharmacol. 2014;70(1):1–11.
Wastesson JW, Canudas-Romo V, Lindahl-Jacobsen R, et al. Remaining life expectancy with and without polypharmacy: a register-based study of Swedes aged 65 years and older. J Am Med Dir Assoc. 2015;17(1):31–5.
United Nations Statistic Division: Composition of macro geographical (continental) regions, geographical sub-regions, and selected economic and other groupings. Available from: http://unstats.un.org/unsd/methods/m49/m49regin.htm. Accessed 9 December 2017. 2013.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no competing interests exist.
Financial disclosure
The authors received no specific funding for this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Salmasi, S., Wimmer, B.C., Khan, T.M. et al. Quantitative exploration of medication errors among older people: a systematic review. Drugs Ther Perspect 34, 129–137 (2018). https://doi.org/10.1007/s40267-017-0468-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-017-0468-9