Abstract
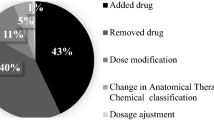
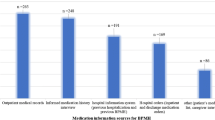
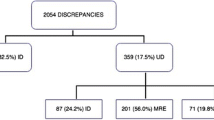
Background During care transitions, discrepancies and medication errors often occur, putting patients at risk, especially older patients with polypharmacy. Objective To assess the results of a medication reconciliation and information programme for discharge of geriatric patients conducted through hospital information systems. Setting A 1300-bed university hospital in Madrid, Spain. Method A prospective observational study. Geriatricians selected candidates for medication reconciliation at discharge, and sent an electronic inter-consultation request to the pharmacy department. Pharmacists reviewed the medication list, comparing it with electronic prescriptions, medication previously prescribed by primary care physicians and other medical records, and resolved any discrepancies. An individualized and tailored drug information at discharge sheet was sent to geriatricians and made available to primary care physicians. Main outcome measure The number and type of discrepancies, the number, type and severity of errors, and the main pharmacological groups involved. Results Medication reconciliation was performed for 118 patients with a mean age of 87 years (SD 5.9), involving a total of 2054 medications, or 17.4 per patient. Discrepancies were found in 723 (35 %) drugs, 105 of which were considered medication errors (15 %); 66 patients (56 %) had at least one error. This gave 0.9 reconciliation errors per patient reviewed and 1.6 per patient with errors. Of the 105 errors, 14 (13 %) were considered serious. The most frequent errors were incomplete prescriptions (40 %) and omissions (35 %). Conclusion An electronic medication reconciliation programme helps pharmacists detect serious medication errors in frail elderly patients and provides complete and up-to-date written information to prevent additional errors at home.


Similar content being viewed by others
References
Mueller SK, Sponsler KC, Kripalani S, Schnipper JL. Hospital-based medication reconciliation practices a systematic review. Arch Intern Med. 2012;172(14):1057–69.
Delgado Sánchez O, Anoz Jiménez L, Serrano Fabiá A, Pico JN. Medication reconciliation. Med Clin. 2007;129(9):343–8 (Spanish).
Lehnbom EC, Stewart MJ, Manias E, Westbrook JI. Impact of medication reconciliation and review on clinical outcomes. Ann Pharmacother. 2014;48(10):1298–312.
Institute for Healthcare Improvement [Internet]. Cambridge (MA): Medication reconciliation review. c2015 [cited 2015 Sept 17]. http://www.ihi.org/resources/Pages/Tools/MedicationReconciliationReview.aspx.
Institute for Safe Medication Practices Canada (ISMP Canada) [Internet]. Toronto: Medication reconciliation in Acute Care Getting Started Kit. Version 3.0.2011. c2000–2015 [cited 2015 Sept 15]. http://www.ismp-canada.org/medrec/.
Instituto para el Uso Seguro de Medicamentos y Productos Sanitarios (ISMP-España) [Internet]. Salamanca: [Recommendations for prevention of medication errors]. 2011 Dec. c2015 [cited 2015 Sept 18]. http://www.ismp-espana.org/ficheros/Bolet%C3%ADn%20n%C2%BA%2034%20%28Diciembre%202011%29.pdf (Spanish).
Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ. 2005;173(5):510–5. doi:10.1503/cmaj.045311 (Spanish).
Kwan JL, Lo L, Sampson M, Shojania KG. Medication reconciliation during transitions of care as a patient safety strategy. A systematic review. Ann Intern Med. 2013;158(5_Part_2):397–403. doi:10.7326/0003-4819-158-5-201303051-00006.
Quélennec B, Beretz L, Paya D, Blicklé JF, Gourieux B, Andrès E, et al. Potential clinical impact of medication discrepancies at hospital admission. Eur J Intern Med. 2013;24(6):530–5. doi:10.1016/j.ejim.2013.02.007.
Joint Commission on Accreditation of Healthcare Organization [Internet]. United States: National Patient Safety Goals. Goal 3 (NPSG.03.05.01). c2015 [cited 2015 Sept 8]. http://www.jointcommission.org/assets/1/6/2015_NPSG_HAP.pdf.
Joint Commission on Accreditation of Healthcare Organizations [Internet]. United States: Sentinel Event Alert/Topics Library Updates: issue 35; 2006 Jan 25 [updated 2006 Feb 9; cited 2015 Aug 25]. http://www.jointcommission.org/assets/1/18/SEA_35.pdf.
Villamañán E, Larrubia Y, Ruano M, Vélez M, Armada E, Herrero A, Álvarez-Sala R. Potential medication errors associated with computer prescriber order entry. Int J Clin Pharm. 2013;35(4):577–83. doi:10.1007/s11096-013-9771-2.
Zoni AC, Durán García ME, Jiménez Muñoz AB, Salomón Pérez R, Martín P, Herranz Alonso A. Impact of medication reconciliation program at admission in an internal medicine department. Eur J Int Med. 2012;23:696–700. doi:10.1016/j.ejim.2012.08.013.
Martín de Rosales Cabrera AM. Multidisciplinary coordination to ensure correct patient medication: medication reconciliation. Rev Calid Asist. 2010;25(5):239–43. doi:10.1016/j.cali.2010.04.003 (Spanish).
Delgado Sánchez O, Nicolás Picó J, Martínez López I, Serrano Fabiá A, Anoz Jiménez L, Fernández Cortés F. Reconciliation errors at admission and departure in old and polymedicated patients. Prospective, multicenter randomized study. Med Clin (Barc). 2009;133(19):741–4. doi:10.1016/j.medcli.2009.03.023 (Spanish).
Hernández C, Mira A, Arroyo E, Díaz M, Andreu L, Sánchez MI. Conciliation discrepancies at hospital discharge. Aten Primaria. 2008;40(12):597–601 (Spanish).
Cornish PL, Knowles SR, Marchesano R, Tam V, Shadowitz S, Juurlink DN, et al. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med. 2005;165(4):424–9.
Alfaro-Lara ER, Santos-Ramos B, González-Méndez AI, Galván-Banqueri M, Vega-Coca MD, Nieto-Martín MD, et al. Medication reconciliation on hospital admission in patients with multiple chronic diseases using a standardised methodology. Rev Esp Geriatr Gerontol. 2013;48(3):103–8. doi:10.1016/j.regg.2012.11.011 (Spanish).
Andreoli L, Alexandra JF, Tesmoingt C, Eerdekens C, Macrez A, Papo T, et al. Medication reconciliation: a prospective study in an internal medicine unit. Drugs Aging. 2014;31(5):387–93.
Peña Pedrosa JA, Santiago Pérez A, Bilbao Gómez-Martino C, Arias Fernández L. Influence of a medication reconciliation program in elderly patients on readmission rate. Pharm Care Esp [Internet]. 2014 [cited 2015 Aug 28];16(4):130–141. http://www.pharmcareesp.com/index.php/PharmaCARE/article/view/185/167. (Spanish).
European Union Network for Patient Safety and Quality of Care [Internet]. Saint-Denis La Plaine: Safe Clinical Practices for Implementation (WP5); c2012 [cited 2015 Aug 26]. http://www.pasq.eu/Wiki/SCP.aspx.
Roure C, Aznar T, Delgado O, Fuster L, Villar I, et al. Consensus document on terminology and classification in medication reconciliation. Barcelona: Ediciones Mayo; 2009. ISBN 978-84-9905-044-7. http://www.sefh.es/bibliotecavirtual/conciliacion/Libro_consenso_terminologia_conciliacion.pdf (Spanish).
Hartwig SC, Denger SD, Schneider PJ. Severity-indexed, incident report-based medication error-reporting program. Am J Hosp Pharm. 1991;48(12):2611–6.
World Health Organization Collaborating Centre for Drug Statistics Methodology [Internet]. Oslo: ATC/DDD Index 2015. C2015 [updated 2013 Dec 19; cited 2015 Jun 19]. http://www.whocc.no/atc_ddd_index/.
Pal A, Babbott S, Wilkinson ST. Can the targeted use of a discharge pharmacist significantly decrease 30-day readmissions? Hosp Pharm. 2013;48(5):380–8. doi:10.1310/hpj4805-380.
Mira JJ, Navarro IM, Guilabert M, Aranaz J. Frequency of medication errors by patients. Rev Panam Salud Publica. 2012;31(2):95–101 (Spanish).
Acknowledgments
We are grateful to Dr. Alberto Pardo Hernández for his support and collaboration in the structure of the project and to Dr. César Nombela Arrieta for his invaluable help in publishing it.
Funding
No funding support was obtained for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Moro Agud, M., Menéndez Colino, R., Mauleón Ladrero, M.d. et al. Analysis of an electronic medication reconciliation and information at discharge programme for frail elderly patients. Int J Clin Pharm 38, 996–1001 (2016). https://doi.org/10.1007/s11096-016-0331-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-016-0331-4