Abstract
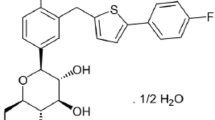
Ipragliflozin (Suglat®) is a potent and selective inhibitor of sodium-glucose cotransporter-2 that was recently launched in Japan. Its mechanism of action involves the suppression of glucose re-absorption in the kidney proximal tubules, causing excretion of glucose in the urine. The aim of this review is to provide a comprehensive overview of currently available pharmacokinetic and pharmacodynamic data on ipragliflozin, including studies in healthy subjects, patients with type 2 diabetes mellitus and special populations. In single- and multiple-dose studies, the maximum plasma concentration and area under the plasma concentration-time curve (AUC) for ipragliflozin increased in a dose-dependent manner. Although urinary excretion of ipragliflozin is low (approximately 1 %), tubular concentration of free ipragliflozin is adequate to provide pharmacological activities. No clinically relevant effects of age, gender or food on the exposure of ipragliflozin were observed. The AUC for ipragliflozin was 20–30 % greater in patients with moderate renal or hepatic impairment than in patients with normal renal or hepatic function. In drug–drug interaction studies, the pharmacokinetics of ipragliflozin and other oral antidiabetic drugs (metformin, sitagliptin, pioglitazone, glimepiride, miglitol and mitiglinide) were not significantly affected by their co-administration. Urinary glucose excretion (UGE) also increased in a dose-dependent manner, approaching a maximum effect at 50–100 mg dosages in Japanese healthy volunteers and patients with type 2 diabetes. The change in UGE from baseline (ΔUGE) tended to be lower in older subjects and female subjects, compared with younger subjects and male subjects, respectively. ΔUGE tended to decrease with decreasing renal function, especially in patients with type 2 diabetes with moderate or severe renal impairment.




Similar content being viewed by others
References
Shaw J, Sicree R, Zimmet P. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14.
International Diabetes Federation. Global guideline for type 2 diabetes 2005. Section 6: glucose control levels. http://www.idf.org/global-guideline-type-2-diabetes-2005. Accessed 2 Oct 2013.
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35:1364–79.
Bakris GL, Fonseca VA, Sharma K, et al. Renal sodium-glucose transport: role in diabetes mellitus and potential clinical implications. Kidney Int. 2009;75:1272–7.
Nair S, Wilding JP. Sodium glucose cotransporter 2 inhibitors as a new treatment for diabetes mellitus. J Clin Endocrinol Metab. 2010;95:34–42.
Imamura M, Nakanishi K, Suzuki T, et al. Discovery of ipragliflozin (ASP1941): a novel C-glucoside with benzothiophene structure as a potent and selective sodium glucose co-transporter 2 (SGLT2) inhibitor for the treatment of type 2 diabetes mellitus. Bioorg Med Chem. 2012;20:3263–79.
Kashiwagi A, Kazuta K, Yoshida S, Nagase I. Randomized, placebo-controlled, double-blind glycemic control trial of novel SGLT2 inhibitor ipragliflozin in Japanese patients with type 2 diabetes mellitus. J Diabetes Investig. 2014;5:382–91.
Kashiwagi A, Kazuta K, Takinami Y, et al. Ipragliflozin improves glycemic control in Japanese patients with type 2 diabetes mellitus: the BRIGHTEN study. Diabetol Int. 2014. doi:10.1007/s13340-014-0164-0.
Kashiwagi A, Akiyama A, Shiga T, et al. Efficacy and safety of ipragliflozin as an add-on to a sulfonylurea in Japanese patients with inadequately controlled type 2 diabetes: results of the randomized, placebo-controlled, double-blind, phase III EMIT study. Diabetol Int. 2014. doi:10.1007/s13340-014-0184-9.
Kashiwagi A, Shiga T, Akiyama A, et al. Efficacy and safety of ipragliflozin as an add-on to pioglitazone in Japanese patients with inadequately controlled type 2 diabetes: a randomized, double-blind, placebo-controlled study (the SPOTLIGHT study). Diabetol Int. 2014. doi:10.1007/s13340-014-0182-y.
Kashiwagi A, Kazuta K, Goto K, et al. Ipragliflozin in combination with metformin for the treatment of Japanese patients with type 2 diabetes: ILLUMINATE, a randomized, double-blind, placebo-controlled study. Diabetes Obes Metab. 2014. doi:10.1111/dom.12331.
Common technical document for ipragliflozin. http://www.info.pmda.go.jp/shinyaku/P201300172/index.html. Accessed 23 June 2014 (in Japanese).
Fujita E, Ushigome F, Suzuki K, et al. Characterization and identification of in vivo and in vitro metabolites of ipragliflozin. Poster presentation at the 25th 2011 AAPS Annual Meeting and Exposition, Washington, DC; October 23–27, 2011.
Ushigome F, Kasai Y, Uehara S, et al. Identification of UDP-glucuronosyltransferase (UGT) isozymes involved in ipragliflozin metabolism in human liver. Poster presentation at the 25th 2011 AAPS Annual Meeting and Exposition, Washington, DC; October 23–27, 2011.
Kadokura T, Saito M, Utsuno A, et al. Ipragliflozin (ASP1941), a selective sodium dependent glucose cotransporter 2 inhibitor, safely stimulates urinary glucose excretion without inducing hypoglycemia in healthy Japanese subjects. Diabetol Int. 2011;2:172–82.
Veltkamp S, Kadokura T, Krauwinkel W, et al. Effect of ipragliflozin (ASP1941), a novel selective sodium-dependent glucose co-transporter 2 inhibitor, on urinary glucose excretion in healthy subjects. Clin Drug Investig. 2011;31:839–51.
Kadokura T, Akiyama N, Kashiwagi A, et al. Pharmacokinetic and pharmacodynamic study of ipragliflozin in Japanese patients with type 2 diabetes mellitus: a randomized, double-blind, placebo-controlled study. Diabetes Res Clin Pract. 2014;106:50–6.
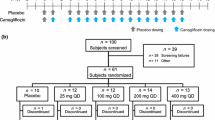
Schwartz SL, Akinlade B, Klasen S, et al. Safety, pharmacokinetic, and pharmacodynamic profiles of ipragliflozin (ASP1941), a novel and selective inhibitor of sodium-dependent glucose co-transporter 2, in patients with type 2 diabetes mellitus. Diabetes Technol Ther. 2011;13:1219–27.
Wright EM. Renal Na(+)-glucose cotransporters. Am J Physiol Renal Physiol. 2001;280:F10–8.
Farber SJ, Berger EY, Earle DP. Effect of diabetes and insulin on the maximum capacity of the renal tubules to reabsorb glucose. J Clin Invest. 1951;30:125–9.
Mogensen CE. Maximum tubular reabsorption capacity for glucose and renal hemodynamics during rapid hypertonic glucose infusion in normal and diabetic subjects. Scand J Clin Lab Invest. 1971;28:101–9.
Rahmoune H, Thompson PW, Ward JM, et al. Glucose transporters in human renal proximal tubular cells isolated from the urine of patients with non-insulin-dependent diabetes. Diabetes. 2004;54:3427–34.
Abdul-Ghani MA, DeFronzo RA, Norton L. Novel hypothesis to explain why SGLT2 inhibitors inhibit only 30–50 % of filtered glucose load in humans. Diabetes. 2013;62:3324–8.
Ferrannini E, Veltkamp SA, Smulders RA, et al. Renal glucose handling: impact of chronic kidney disease and sodium-glucose cotransporter 2 inhibition in patients with type 2 diabetes. Diabetes Care. 2013;36:1260–5.
Wilding J, Ferrannini E, Fonseca V, et al. Efficacy and safety of ipragliflozin in patients with type 2 diabetes inadequately controlled on metformin: a dose-finding study. Diabetes Obes Metab. 2013;15:403–9.
Retnakaran R, Cull CA, Thorne KI, et al. Risk factors for renal dysfunction in type 2 diabetes: UK Prospective Diabetes Study 74. Diabetes. 2006;55:1832–9.
Veltkamp SA, van Dijk J, Krauwinkel W, et al. The effect of renal impairment on the pharmacokinetics and urinary glucose excretion of the SGLT2 inhibitor ipragliflozin (ASP1941) in type 2 diabetes mellitus patients. Poster presentation at the 71st Scientific Sessions of the American Diabetes Association (ADA), San Diego, CA; June 24–28, 2011. Abstract Number: 1127-P.
Smulders R, Ishikawa H, Nakajo I, et al. The effect of renal impairment on the pharmacokinetics and urinary glucose excretion of the SGLT2 inhibitor ipragliflozin (ASP1941) in Japanese type 2 diabetes mellitus patients. Poster presentation at the 47th Annual Meeting of the European Association for the Study of Diabetes (EASD), Lisbon, Portugal; September 12–16, 2011. Abstract Number: 847.
Matsuo S, Imai E, Horio M, et al. Collaborators developing the Japanese equation for estimated GFR. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Levey AS, Bosch JP, Lewis JB, et al. Modification of Diet in Renal Disease Study Group. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med. 1999;130:461–70.
Takahashi H, Ishikawa H, Yoshida S, et al. A randomized, double blind, placebo-controlled study on long-term efficacy and safety of ipragliflozin treatment in patients with type 2 diabetes mellitus and renal impairment: results of the LANTERN study (long-term ASP1941 safety evaluation in T2DM patients with renal impairment). Poster presentation at the 57th Annual Meeting of the Japan Diabetes Society (JDS), Osaka, Japan; May 22–24, 2014. Abstract Number I-P-131 [in Japanese].
Zhang W, Krauwinkel WJ, Keirns J, et al. The effect of moderate hepatic impairment on the pharmacokinetics of ipragliflozin, a novel sodium glucose co-transporter 2 (SGLT2) inhibitor. Clin Drug Investig. 2013;33:489–96.
International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use. ICH Topic E14. The clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drugs, May 2005 (CHMP/ICH/2/04). http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E14/E14_Guideline.pdf. Accessed 2 Oct 2013.
Zhang W, Smulders R, Abeyratne A, et al. Ipragliflozin does not prolong QTc interval in healthy male and female subjects: a phase I study. Clin Ther. 2013;35:1150–61.
Veltkamp SA, van Dijk J, Collins C, et al. Combination treatment with ipragliflozin and metformin: a randomized, double-blind, placebo-controlled study in patients with type 2 diabetes mellitus. Clin Ther. 2012;34:1761–71.
Smulders RA, Zhang W, Veltkamp SA, et al. No pharmacokinetic interaction between ipragliflozin and sitagliptin, pioglitazone, or glimepiride in healthy subjects. Diabetes Obes Metab. 2012;14:937–43.
Kuboyama N, Hayashi I, Yamaguchi T. Pharmacokinetic, pharmacological, and clinical profile of miglitol (SEIBULE), a novel alpha-glucosidase inhibitor. Nihon Yakurigaku Zasshi. 2006;127:223–32 (in Japanese).
Nakajo I, Taniuchi Y, Yoshida S, et al. Drug interaction study of ipragliflozin and miglitol in healthy Japanese subjects. Poster presentation at the Annual Meeting of the American Society for Clinical Pharmacology and Therapeutics (ASCPT); National Harbor, MD; March 12–17, 2012.
Kitasato L, Tojo T, Hatakeyama Y, et al. Postprandial hyperglycemia and endothelial function in type 2 diabetes: focus on mitiglinide. Cardiovasc Diabetol. 2012;29:11–79.
Toyoshima J, Taniuchi Y, Smulders R, et al. Drug–drug interaction study between ipragliflozin and other oral anti-diabetics drugs. Poster presentation at the 57th Annual Meeting of the Japan Diabetes Society (JDS), Osaka, Japan; May 22–24, 2014. Abstract Number I-P-146 [in Japanese].
Kasichayanula S, Liu X, Lacreta F, et al. Clinical pharmacokinetics and pharmacodynamics of dapagliflozin, a selective inhibitor of sodium-glucose co-transporter type 2. Clin Pharmacokinet. 2014;53:17–27.
Scheen AJ. Pharmacokinetic and pharmacodynamic profile of empagliflozin, a sodium glucose co-transporter 2 inhibitor. Clin Pharmacokinet. 2014;53:213–25.
Scheen AJ. Drug–drug interactions with sodium-glucose cotransporters type 2 (SGLT2) inhibitors, new oral glucose-lowering agents for the management of type 2 diabetes mellitus. Clin Pharmacokinet. 2014;53:295–304.
Tahara A, Kurosaki E, Yokono M, et al. Pharmacological profile of ipragliflozin (ASP1941), a novel selective SGLT2 inhibitor, in vitro and in vivo. Naunyn Schmiedebergs Arch Pharmacol. 2012;385:423–36.
Kawano H, Kashiwagi A, Kazuta K, et al. Long-term safety, tolerability and efficacy of ipragliflozin in Japanese patients with type 2 diabetes mellitus: IGNITE. Abstract published in the 72nd Scientific Sessions of the American Diabetes Association (ADA), Philadelphia, PA; June 8–12, 2012. Abstract Number 2422-PO.
Acknowledgements
Ipragliflozin is under development by Astellas Pharma Inc. and Kotobuki Pharmaceutical Co., Ltd. This study was sponsored by Astellas. Medical writing and editorial support was funded by Astellas and provided by Dr. Nicholas D. Smith, Helen Roberton and ELMCOM™.
SL, RS and WK are employees of Astellas Pharma Global Development in EU. WZ and JK are employees of Astellas Pharma Global Development in US.
TK wrote the manuscript, WZ, JK and RS contributed to the writing of the manuscript and participated in the research design, SL and YT coordinated the clinical studies, and WK and IN performed the data analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kadokura, T., Zhang, W., Krauwinkel, W. et al. Clinical Pharmacokinetics and Pharmacodynamics of the Novel SGLT2 Inhibitor Ipragliflozin. Clin Pharmacokinet 53, 975–988 (2014). https://doi.org/10.1007/s40262-014-0180-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-014-0180-z