Abstract
Background
In Italy, there is scarce evidence on the epidemiological and economic burden induced by primary antibody deficiencies.
Objective
The aim of this study was to elaborate the available epidemiological and cost data in order to estimate the annual expenditure induced by the management of patients affected by the common variable immunodeficiency (CVID) and X-linked agammaglobulinemia (XLA) requiring immunoglobulin (Ig) replacement therapy.
Methods
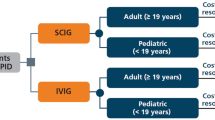
A probabilistic cost-of-illness model was developed to estimate the number of patients with CVID and XLA, and the economic burden associated with their therapy in terms of direct or indirect costs. A systematic literature review was carried out to reveal both epidemiological and economic data. Furthermore, a probabilistic sensitivity analysis with 5000 Monte Carlo simulations was performed.
Results
The epidemiological model allowed us to estimate the number of prevalent patients affected by XLA and CVID in Italy in 2017, corresponding to 1885 (95% confidence interval [CI] 944–3145) and 133 (95% CI 115–152) patients, respectively. The estimated total expenditure for the treatment and management of patients with CVID and XLA requiring Ig replacement therapy amounts to €42.68 million (95% CI €14.38–€86.1 million).
Conclusions
This information provides a comprehensive perspective of the economic issues, and facilitates better-informed public health decision making, in the management of CVID and XLA in Italy.





Similar content being viewed by others
References
Driessen G, van der Burg M. Educational paper: primary antibody deficiencies. Eur J Pediatr. 2011;170(6):693–702.
Stonebraker JS, et al. Modeling primary immunodeficiency disease epidemiology and its treatment to estimate latent therapeutic demand for immunoglobulin. J Clin Immunol. 2014;34(2):233–44.
Shehata N, et al. The use of immunoglobulin therapy for patients with primary immune deficiency: an evidence-based practice guideline. Transfus Med Rev. 2010;24(Suppl 1):S28–50.
Quinti IB, Barilaro G. Le immunoglobuline per uso endovenoso: efficacia, tollerabilità e consumo. Rivista di Immunologia e Allergologia Pediatrica. 2013;5:28–36.
Kerr J, et al. Is dosing of therapeutic immunoglobulins optimal? A review of a three-decade long debate in Europe. Front Immunol. 2014;5:629.
European Primary Immunodeficiencies Consensus Conference, Consensus Report and Recommendations, in European Primary Immunodeficiencies Consensus Conference. 19–20 June 2006: Paul-Ehrlich-Institut, Langen, Germany.
Berger M. Subcutaneous immunoglobulin replacement in primary immunodeficiencies. Clin Immunol. 2004;112(1):1–7.
Berger M. Subcutaneous administration of IgG. Immunol Allergy Clin North Am. 2008;28(4):779–802, viii.
Bonilla FA. Intravenous immunoglobulin: adverse reactions and management. J Allergy Clin Immunol. 2008;122(6):1238–9.
Wasserman RL. Subcutaneous immunoglobulin: facilitated infusion and advances in administration. Clin Exp Immunol. 2014;178(Suppl 1):75–7.
Matucci A, et al. Analisi di minimizzazione dei costi della terapia con Immunoglobuline (Ig) per il trattamento di pazienti con immunodeficienza primaria: confronto tra terapia con Ig sottocute vs endovena. Giornale Italiano di Health Technology Assessment. 2008;1(1):31–7.
Grimbacher B. ESID Registry Working Party, The European Society for Immunodeficiencies (ESID) registry 2014. Clin Exp Immunol. 2014;178(Suppl 1):18–20.
Angelis A, Tordrup D, Kanavos P. Socio-economic burden of rare diseases: a systematic review of cost of illness evidence. Health Policy. 2015;119(7):964–79.
Mazzucato M, et al. A population-based registry as a source of health indicators for rare diseases: the ten-year experience of the Veneto Region’s rare diseases registry. Orphanet J Rare Dis. 2014;9:37.
Hodgson TA, Meiners MR. Cost of illness methodology: a guide to current practices and procedures. Milbank Memor Fund Q. 1982;60(3):429–62.
Berger ML, et al. Cost of Illness Study. In: Bingefors K, Pashos CL, Dix Smith M, Berger ML, Hedblom EC, Torrance GW, editors. Health care cost, quality, and outcomes: ISPOR book of terms. Lawrenceville: ISPOR; 2003. p. 43–4.
Segel JE. Cost-of-illness studies—a primer. RTI-UNC Center of Excellence in Health Promotion Economics; 2006.
Green S, Higgins J. Cochrane handbook for systematic reviews of interventions 4.2.5. The Cochrane Collaboration 2005. 19 May 2009. http://www.cochrane.org/resources/glossary.htm. Accessed 31 Jul 2018.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA STATEMENT. PLoS Med. 2009;6(7):e1000097.
CEREDIH: The French PID Study Group. The French national registry of primary immunodeficiency diseases. Clin Immunol. 2010;135(2):264–72.
Edgar JD, et al. The United Kingdom Primary Immune Deficiency (UKPID) Registry: report of the first 4 years’ activity 2008-2012. Clin Exp Immunol. 2014;175(1):68–78.
Kobrynski L, Powell RW, Bowen S. Prevalence and morbidity of primary immunodeficiency diseases, United States 2001–2007. J Clin Immunol. 2014;34(8):954–61.
Gathmann B, et al. The European internet-based patient and research database for primary immunodeficiencies: results 2006-2008. Clin Exp Immunol. 2009;157(Suppl 1):3–11.
Calizzani G, et al. Analisi della domanda dei principali medicinali plasmaderivati in Italia. Anni 2007–2011. Rapporto ISTISAN 2012, Isituto Superiore di Sanità. p. 167.
Quinti I, et al. Effectiveness of immunoglobulin replacement therapy on clinical outcome in patients with primary antibody deficiencies: results from a multicenter prospective cohort study. J Clin Immunol. 2011;31(3):315–22.
Istituto Nazionale di Statistica. Rivalutazione e documentazione su prezzi, costi e retribuzioni contrattuali. Indice dei prezzi al consumo per famiglie operai e impiegati. Novembre 2013. http://rivaluta.istat.it/. Accessed 31 Jul 2018.
Gazzetta Ufficiale della Repubblica Italiana. Regime di rimborsabilità e prezzo di vendita di nuove confezioni dei medicinali. 2015. http://www.gazzettaufficiale.it. Accessed 31 Jul 2018.
Farmadati Italia. Banca Dati Online [cited May 2016]. http://www.farmadati.it/default.aspx. Accessed 31 Jul 2018.
Berger M. Adverse effects of IgG therapy. J Allergy Clin Immunol Pract. 2013;1(6):558–66.
EUROSTAT. Hourly labour costs by NACE Rev. 1.1 activity. 2004. http://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=lc_an_costh&lang=en. Accessed 31 Jul 2018.
Briggs A, Claxton K, Sculpher M. Decision modelling for health economic evaluation. New York; O.U.P. Inc.; 2007.
Stewart WF, et al. Cost of lost productive work time among US workers with depression. JAMA. 2003;289(23):3135–44.
Hemp P. Presenteeism: at work—but out of it. Harv Bus Rev. 2004;82(10):49–58, 155.
Capone A, et al. Health Data Entanglement and artificial intelligence-based analysis: a brand new methodology to improve the effectiveness of healthcare services. Clin Ter. 2016;167(5):e102–11.
Mahlaoui N, et al. The European Society for Immunodeficiencies (ESID) Registry: recent advancements in the epidemiology of Primary Immunodeficiencies and how does that translate in clinical care. Rare Diseases and Orphan Drugs. 2014;1(4):25–7.
Wasserman RL, et al. Recombinant human hyaluronidase-facilitated subcutaneous infusion of human immunoglobulins for primary immunodeficiency. J Allergy Clin Immunol. 2012;130(4):951–7.e11.
Baio G, et al. Economic burden of human papillomavirus-related diseases in Italy. PLoS One. 2012;7(11):e49699.
Marcellusi A, et al. The economic burden of HCV-induced diseases in Italy. A probabilistic cost of illness model. Eur Rev Med Pharmacol Sci. 2015;19(9):1610–20.
Stiehm ER. Adverse effects of human immunoglobulin therapy. Transfus Med Rev. 2013;27(3):171–8.
Istituto Nazionale di Statistica. ISTAT. 2017 [cited 2017; Italian employment rate]. http://www.istat.it/it/. Accessed 31 Jul 2018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This analysis was funded by Baxalta SpA. The authors confirm that the paper is an accurate representation of the study results.
Conflicts of interest
Viti Raffaella, Marcellusi Andrea, Capone Alessandro, Matucci Andrea, Vultaggio Alessandra, Pignata Claudio, Spadaro Giuseppe, Vacca Angelo, Marasco Carolina, Agostini Carlo, and Mennini Francesco Saverio declare that there are no conflicts of interest regarding the publication of this paper.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Viti, R., Marcellusi, A., Capone, A. et al. Direct and Indirect Costs of Immunoglobulin Replacement Therapy in Patients with Common Variable Immunodeficiency (CVID) and X-Linked Agammaglobulinemia (XLA) in Italy. Clin Drug Investig 38, 955–965 (2018). https://doi.org/10.1007/s40261-018-0688-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-018-0688-3



