Abstract
Biologic therapy involving anti-tumor necrosis factor-α (anti-TNFα) agents has fundamentally changed the management of patients with immune-mediated inflammatory diseases, including rheumatoid arthritis, thus benefiting many patients. Nevertheless, the inability of some patients to achieve low disease activity or clinical remission remains a major concern. To address such concerns, next-generation anti-TNFα agents that differ from the immunoglobulin G-format anti-TNFα agents that have been used to date are being developed using antibody-engineering technology. Their unique design employing novel molecular characteristics affords several advantages, such as early improvement of clinical symptoms, optimization of drug bioavailability, enhancement of tissue penetration, and a reduction in side effects. This holds promise for a new paradigm shift in biologic therapy via the use of next-generation anti-TNFα agents. Ozoralizumab, a next-generation anti-TNFα agent that was recently approved in Japan, comprises a variable region heavy-chain format. It has a completely different structure from conventional therapeutic antibodies, such as a small molecular size, an albumin-binding module, and a unique format that produces an avidity effect. Ozoralizumab exhibited rapid biodistribution into joints, provided attenuation of Fcγ receptor-mediated inflammatory responses, and had a high binding affinity to TNFα in non-clinical studies. In clinical trials, ozoralizumab yielded an early improvement in clinical symptoms, a sustained efficacy for up to 52 weeks, and an acceptable tolerability in patients with rheumatoid arthritis. This review focuses on the results of pre-clinical and clinical trials for ozoralizumab and outlines the progress in next-generation antibody development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Although anti-tumor necrosis factor-α agents remain at the forefront of therapy more than 20 years after their introduction, several limitations in terms of a loss of drug efficacy because of secondary failure, poor bioavailability, and an unwanted immune response led to the development of next-generation anti-tumor necrosis factor-α agents. |
Ozoralizumab is a next-generation anti-tumor necrosis factor-α agent that adopts the variable-domain heavy-chain format to enhance the biodistribution to target tissue, prolong the half-life, and reduce unwanted immune responses. Ozoralizumab was successful in solving various issues in non-clinical studies and afforded an early improvement of clinical symptoms in clinical trials. |
The remarkable improvement that ozoralizumab has shown in phase III trials suggests the potential for a new paradigm shift using next-generation antibodies, for the treatment not only of rheumatoid arthritis, but also of several other diseases. |
1 Introduction
Biologics are one of the most widely used drug platforms for treating various diseases because they can selectively target immune cells, infected cells, cancer cells, and even pathogens. In particular, multiple biologics targeting tumor necrosis factor-α (TNFα) have been used for decades to treat immune-mediated inflammatory diseases, thus placing these agents among the best-selling drugs worldwide [1, 2]. The development of anti-TNFα agents has markedly advanced the pharmacotherapy of immune-mediated inflammatory diseases and caused a major paradigm shift in their diagnosis and treatment [3,4,5]. Despite the availability of other targeted biologics for immune-mediated inflammatory diseases, anti-TNFα agents remain at the forefront of therapy more than 20 years after their introduction. However, some of the patients who are treated with these agents do not achieve low disease activity and clinical remission; therefore, a high demand exists for new anti-TNFα agents to which these patients will respond [6, 7]. Anti-TNFα agents exhibit immunogenicity, which, after repeated administration, leads to the formation of antidrug antibodies (ADAs). By neutralizing the function of the anti-TNFα agents or accelerating its clearance, ADA formation leads to the loss of clinical response (secondary failure), which can occur in up to 30% of patients [8]. The rheumatoid factor (RF), which is an endogenous antibody that can bind to the fragment crystallizable (Fc) region of immunoglobulin G (IgG) [9], is among the poor prognostic factors, and its positivity is higher in difficult-to-treat patients [10]. In patients treated with anti-TNFα agents, inadequate clinical response has been reported to be higher in the RF-positive group compared with the RF-negative group, suggesting that the RF attenuates the effect of anti-TNFα agents [11,12,13]. In recent years, patient-reported outcomes, which reflect the most relevant symptoms of the disease and their impact on the lives of patients without a physician’s intervention, have become more important for clinical evaluation. In addition to reducing the patient burden of drug administration, such as the frequency of administration and pain during injection, the rapid improvement of these patient-reported outcomes is challenging [14,15,16].
To address these issues, the development of next-generation anti-TNFα agents using novel modalities other than the IgG format, (such as fragment antibodies, small molecules, nanoparticles, antisense oligonucleotides, and small interfering RNAs) is in full swing. In 2022, ozoralizumab, which is a next-generation antibody with a variable-domain heavy-chain (VHH) format, was approved as a novel anti-TNFα agent for the first time in approximately 10 years, thus attracting considerable attention. This review summarizes the progress in the development of next-generation antibodies and the most developed application of these novel therapeutic modalities for clinical use, and focuses on their application to anti-TNFα therapy as well as on the results of the pre-clinical and clinical trials of ozoralizumab.
2 Fragment Antibodies
Next-generation antibody drugs are molecules that are constructed using antibody engineering techniques, such as the addition of small molecules to the substructure of the conventional IgG, the mixing of substructures, and the use of easily engineered small antibodies. In particular, fragment antibodies have been developed in various formats using antibody-engineering techniques, to provide specialized functions for various purposes, such as therapeutic drugs and diagnostic drugs [17]. The typical fragment antibodies include Fab, single-chain Fv (scFv), and VHH antibodies.
A comparison of the properties of each antibody format is summarized in Fig. 1. In general, IgG antibodies must be expressed in mammalian cells. Conversely, fragment antibodies can be expressed in microorganisms such as Escherichia coli, which significantly reduces production costs. Another advantage is their lower molecular weight, which facilitates their genetic engineering compared with IgG antibodies. As shown in Fig. 1, Fab, scFv, and VHH formats have different molecular characteristics compared with IgG, such as a much shorter half-life in the blood and the inability to exert an effector function via the Fc region [18]; hence, it is important to understand these molecular characteristics and select the appropriate antibody format according to the targeted field during drug development. Full-length IgG antibodies account for >90% of all antibody drugs approved to date, and methods for drug development using low-molecular-weight antibodies remain in their infancy. However, approximately half of the fragment antibodies that have been approved as drugs to date were mostly authorized around the year 2020, suggesting that the evolution of antibody engineering technologies is accelerating the realization of the potential of fragment antibodies (Table 1). In addition, the fragment antibody format is being used for the development of therapeutic drugs for use beyond cancer and autoimmune diseases, thus demonstrating its versatility.
Comparison of the properties of the different antibody formats. The molecular weight of classical immunoglobulin G (IgG), which consists of heavy and light chains, is approximately 150–160 kDa. Fragment antibodies (Fab, single-chain Fv [scFv], and variable-domain heavy-chain [VHH]) are much smaller than IgG and can be easily genetically engineered. Their small size also allows them to be expressed in Escherichia coli and other bacteria, which is a cost-effective approach. Conversely, fragment antibodies lack the fragment crystallizable (Fc) region, have a short half-life, and do not possess an effector function
2.1 scFv
As shown in Fig. 1, IgG consists of an antigen recognition region and a Fc region, used for interaction with the receptors expressed on immune cells. These molecules play various roles in a wide variety of fields, and the antigen-recognition region and the Fc region can exist independently as stable molecules. Therefore, antibody-engineering techniques, such as genetic modification and enzymatic cleavage, can be used to produce antibody fragments consisting only of the antigen recognition region (Fab), or single-chain antibodies carrying the variable region linked by an amino acid linker (scFv) [Fig. 1] [19].
The three antibody drugs with the scFv format that have been approved to date are brolucizumab, blinatumomab, and tebentafusp [20,21,22] (Table 1). Among them, brolucizumab is the only antibody drug that is used as a stand-alone scFv, whereas tebentafusp is a fusion format of an scFv and a T-cell receptor-derived domain. In turn, blinatumomab is a tandem scFv antibody consisting of the scFv-recognizing CD3 (i.e., a membrane protein that is expressed on B cells) and the scFv-recognizing CD19 (i.e., a membrane protein that is expressed on T cells), linked by an amino acid linker. The two scFVs recognize their respective target molecules simultaneously, bringing the target B cells and T cells into close proximity and eliminating the target cells [23]. Ferrari et al. showed that a dual-specificity antibody combining a single-chain variable fragment specific for the microvasculature of human arthritic synovium (scFv A7) and the scFv of adalimumab improved local inflammation via the efficient delivery of adalimumab to the inflamed synovium in a mouse model and demonstrated the potential of scFv application for the treatment of rheumatoid arthritis (RA) [24].
2.2 VHH
Camelids have heavy-chain antibodies that function with the heavy chain exclusively, and not with the light chain [25]. Subsequently, a VHH antibody was developed by excising the variable region of this heavy-chain antibody (Fig. 2) [26]. This VHH has a molecular weight of approximately 15 kDa, which is about one tenth that of IgG and half that of scFv. Moreover, although it has a binding affinity to antigens that is comparable to that of IgG antibodies, it exhibits molecular characteristics that include a higher tissue penetration than that of IgG. In addition, it has a good expression yield, not only in mammalian systems, but also in E. coli, thereby attracting attention as a new format for drug development. Three antibodies with a VHH format have been approved as drugs to date: caplacizumab, ozoralizumab, and envafolimab (Table 1) [27,28,29]. No stand-alone VHH has ever been launched as a therapeutic biologic, and all three approved agents have an ingenious format that affords an avidity effect. Caplacizumab is a molecule consisting of equivalent VHH domains connected by an alanine linker, whereas ozoralizumab is a multivalent molecule composed of two VHH molecules against TNFα and one VHH molecule against human serum albumin (HSA), which are connected by an amino acid linker; in turn, envafolimab is a molecule that carries the VHH domain fused to the Fc region of human IgG1. Ozoralizumab employs an HSA-specific VHH, whereas envafolimab uses the human IgG1 Fc region, which is expected to improve the pharmacokinetics while maintaining the high tissue-penetration potential of VHH. Regarding the mechanism of action, caplacizumab uses an anti-von Willebrand factor VHH to inhibit the interaction between von Willebrand factor multimers and platelets [30], whereas ozoralizumab binds to the TNFα trimer and inhibits its interaction with the receptor [31]. Finally, envafolimab binds to programmed death-ligand 1 and inhibits its interaction with programmed cell death protein 1 [32].
Schematic of conventional immunoglobulin G (IgG), single-chain Fv (scFv), heavy-chain antibody, and variable-domain heavy-chain (VHH) antibodies. The heavy-chain antibody expressed in camelids has three complementarity determining regions (CDRs) and exhibits an antigen-binding ability that is comparable to that of IgG with six CDRs. Variable-domain heavy-chain antibodies are produced via fragmentation of the variable region of heavy-chain antibodies. Variable-domain heavy-chain antibodies retain their binding ability and are approximately one tenth the size of IgG. CH constant region of heavy chain, CL constant region of light chain, Fc fragment crystallizable, VH variable regions of heavy chain, VL variable regions of light chain
3 Ozoralizumab
3.1 Structure and Binding Affinity of Ozoralizumab
As mentioned above, ozoralizumab is one of the VHH-format antibodies that has been approved to date. This antibody functions as a treatment for RA that was approved in Japan in 2022, ahead of the rest of the world. Ozoralizumab is a next-generation anti-TNFα agent consisting of a trivalent VHH structure composed of two anti-human TNFα VHHs and one anti-HSA VHH connected by two glycine-serine linkers consisting of nine amino acids [33]. The anti-human TNFα VHH domain of ozoralizumab was produced via the conventional phage-display technology using RNA isolated from llama-derived peripheral blood lymphocytes that had been immunized with human TNFα [34]. Ozoralizumab is produced as a single-chain protein using recombinant genetic technology in Chinese hamster ovary cell lines [35]. Moreover, ozoralizumab exhibits a high binding affinity for TNFα (Kd value for human TNFα: 20.2 pmol/L) by bivalent binding to a single TNFα trimer via the two anti-human TNFα VHHs, thus inhibits the bioactivity of both soluble form and membrane-bound forms of TNFα [36]. In vitro, it inhibited the cytotoxicity induced by the addition of human TNFα to mouse fibroblasts (L929) in a concentration-dependent manner, with a half maximal inhibitory concentration value of 22.5 pmol/L [36]. In vivo, in a mouse air pouch model, ozoralizumab significantly inhibited the cellular infiltration induced by the administration of human TNFα at ≥0.125 mg/kg [36]. In addition, it has been experimentally demonstrated that ozoralizumab does not interact with Fcγ receptors or complement components because it does not possess an Fc region, which renders it less likely to cause local acute inflammation [37]. Furthermore, the molecular weight of ozoralizumab is approximately 38 kDa, which is about one fourth the molecular weight of a typical IgG antibody (approximately 150 kDa). Although this molecular weight is below 50 kDa, which is considered to be filtered by glomeruli in the kidney, it is believed that ozoralizumab binds to HSA via the anti-HSA VHH, thus avoiding renal excretion and achieving a longer half-life in the blood (Fig. 3). The Kd value of ozoralizumab for HSA is 4.28 nmol/L [36]. Even in this multivalent VHH format, it exerts a rapid absorption compared with IgG, leading to faster biodistribution into joints and quicker drug effects compared with the IgG antibody [38].
Schematic of ozoralizumab. Ozoralizumab comprises two anti-human tumor necrosis factor-α (hTNFα) variable-domain heavy-chain (VHH) antibodies and one anti-human serum albumin (HSA) VHH antibody connected by two glycine-serine linkers (9GS) linkers. Ozoralizumab can bivalently bind to a single TNFα trimer using two anti-human TNFα VHH antibodies to exert an avidity effect. The anti-HSA VHH antibody contributes to the long serum half-life of ozoralizumab
3.2 Model Structure of Ozoralizumab and Trimeric TNFα
The individual anti-TNFα VHH units present in ozoralizumab have a high affinity at the nanomolar level alone; however, when acting in tandem with ozoralizumab, it exhibits a higher affinity than do individual anti-TNFα VHH units (avidity effect). Interestingly, it has been shown that, if the distance between two anti-TNFα VHHs, including the linker, is shorter than the distance between the two binding sites of the trimeric TNFα, the avidity effect is not exerted [34, 39]. Kyuuma et al. have proposed an interesting model structure for the complex of ozoralizumab with trimeric TNFα using the crystal structure of TNFα and a surrogate antibody of ozoralizumab (VHH2), which differs from ozoralizumab by only five amino acids [34]. Molecular dynamic simulations using the GROMACS software were performed on the model structure of the complex of ozoralizumab with the TNFα trimer, which was constructed using the MOE/Homology Modeler. It was shown that this structure is energetically stable, with no significant structural changes observed within the calculation time range (Fig. 4) [37]. The distance between the N-termini and C-termini of the two anti-TNFα VHHs that were simultaneously bound to the trimeric TNFα was 58.1 Å, indicating that the molecular length of the anti-HSA VHH and glycine-serine linkers located between these VHHs had been optimized. The model structure also showed that the HSA binding site is opposite to TNFα, suggesting that TNFα and HSA can bind to ozoralizumab simultaneously without steric interference. This elegant molecular design using anti-HSA VHH that improves the pharmacokinetics as a linker was validated via molecular dynamic calculations of the model structure.
Front (left) and bottom (right) views of the predicted three-dimensional structure of the ozoralizumab-tumor necrosis factor-α (TNFα) trimer complex. The human TNFα (hTNFα) trimer molecule is shown with the molecular surface of each TNFα monomer unit colored in dark yellow, light yellow, and light gray, respectively. The framework regions of the anti-TNFα NANOBODY® molecules and the anti-human serum albumin (HSA) NANOBODY® molecule are colored in green and white, respectively. The CDRs are defined according to the Kabat numbering scheme and colored in orange (CDR 1 and 2) and red (CDR3), respectively, whereas the two linkers are colored in dark gray (adapted from Kyuuma et al. [37]). The figure is used under the CC-BY license (https://creativecommons.org/licenses/by/4.0/)
4 Clinical Studies
A phase II/III study of ozoralizumab was conducted to assess the early improvement in clinical symptoms, sustained efficacy up to 52 weeks, and acceptable tolerability afforded by this agent [40, 41]. The following subsection outlines the results of the phase II/III study (OHZORA trial) [40, 41], the phase III study (NATSUZORA trial) [42], and the results of the extended dosing interval conducted in the long-term extension study (HOSHIZORA trial) [43]. The designs of these clinical studies are summarized in Table 2.
4.1 Efficacy in Patients with RA
4.1.1 Phase II/III Trial (OHZORA Trial)
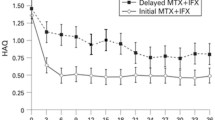
A multicenter, double-blind, parallel-group, placebo-controlled, phase II/III trial (JapicCTI-184029) was conducted to evaluate the efficacy and safety of the subcutaneous administration of ozoralizumab plus methotrexate (MTX) in patients with active RA despite MTX therapy [40, 41]. In this trial, a total of 381 patients were allocated to receive placebo, ozoralizumab 30 mg, or ozoralizumab 80 mg at a ratio of 1:2:2. These drugs were administered subcutaneously every 4 weeks for 24 weeks in combination with MTX. The primary endpoint of the American College of Rheumatology (ACR) 20 response rate at week 16 was significantly higher in the two ozoralizumab groups (30 mg: 79.6%; 80 mg: 75.3%) compared with the placebo group (37.3%) [p < 0.001] [40]. Similar results were obtained for the ACR50 and ACR70 response rates. Furthermore, the results obtained at week 24 were comparable. However, there was no significant difference in the other primary endpoint, i.e., the amount of change from the baseline in the modified total sharp score at week 24 in the ozoralizumab 30-mg and 80-mg groups compared with the placebo group. However, the proportion of patients without progression of structural damage (change from the baseline in the modified total sharp score ≤ 0) was smaller in the 30-mg and 80-mg groups compared with the placebo group, and a significant difference was observed [40]. In addition, a significant improvement was observed in the ozoralizumab 30-mg and 80-mg groups compared with the placebo group from day 3 of treatment in terms of disease activity evaluation indices, such as the Disease Activity Score 28 (DAS28) using the C-reactive protein, patient-reported outcomes (such as the visual analog scale [VAS] for patient pain), and inflammatory markers (such as high-sensitivity C-reactive protein) [40]. In this trial, all patients received ozoralizumab 30 mg or 80 mg from week 24 onward. In the non-blinded evaluations, the effects were maintained for 52 weeks at both ozoralizumab doses [41].
4.1.2 Phase III Trial (NATSUZORA Trial)
The safety and efficacy of ozoralizumab were examined in an open phase III trial (JapicCTI-184031) that included 140 Japanese patients with RA who had discontinued conventional synthetic disease-modifying anti-rheumatic drugs because of safety reasons or an inadequate response [42]. Ozoralizumab (30 mg: 80 mg at a ratio of 2:1) was administered subcutaneously every 4 weeks for 52 weeks without MTX, yielding continuation rates of 87.1% up to week 24 and 72.1% up to week 52. The ACR20, ACR50, and ACR70 response rates improved from the timepoint of the initial evaluation at week 1, with the effects being maintained for 52 weeks (72.3%/51.1%/30.9% in the 30-mg group and 78.3%/54.3%/37.0% in the 80-mg group) [42]. A similar tendency was observed for the remaining efficacy endpoints, including physician’s global VAS, patient’s global VAS, patient pain VAS, and the number of tender or swollen joints, as well as for the inflammatory markers.
4.2 Pharmacodynamics and Effect of Trough Concentration on Drug Efficacy
In the OHZORA trial, the plasma concentrations of ozoralizumab after the single subcutaneous administration of ozoralizumab 30 mg in combination with MTX in Japanese patients with RA reached a maximum concentration on day 6 after the administration (time to maximum concentration), and then slowly disappeared with a half-life of approximately 18 days. The maximum concentration was 4.55 ± 1.1 μg/mL, and the area under the concentration–time curve from zero to infinity was 3280 ± 1280 h/μg/mL [44]. The plasma concentration after a repeated subcutaneous administration of ozoralizumab 30 mg every 4 weeks stabilized by week 16 after the start of the administration regardless of the presence or absence of MTX and was maintained at approximately 2 μg/mL up to week 52. This suggests that ozoralizumab obtained long-term retention benefits from the albumin recycling mechanism through the anti-HSA VHH.
To evaluate the relationship between pharmacodynamics and efficacy, a receiver operating characteristic analysis was performed using the ACR20 and ACR50 response rates and the trough concentrations of ozoralizumab [44]. As a result, a cut-off value of 1 μg/mL for the trough concentration at week 16 was obtained in both the OHZORA trial with MTX and the NATSUZORA trial without MTX. In groups with plasma concentrations above this cut-off value, a high response was confirmed regarding the efficacy indices. In contrast, at week 24, the cut-off value was reduced or could no longer be obtained, and at week 52, the cut-off value could no longer be obtained in either of the trials. The effect of the plasma trough concentration of ozoralizumab on its efficacy decreased with long-term continued treatment, suggesting that the effect was to be expected independent of the trough concentration of the drug. Furthermore, the simulation of the trough concentration when ozoralizumab 30 mg was administered every 6 weeks resulted in a trough concentration of 1.2 μg/mL. This finding suggests that the effect can be maintained even when treatment is administered at intervals of 6 weeks because of factors such as the delay in hospital visits.
4.3 Prolongation of the Treatment Interval (Administration Every 8 Weeks)
The HOSHIZORA trial (NCT04077567) was a multicenter, open, long-term extension study that evaluated the long-term efficacy and safety of ozoralizumab in patients who had completed the OHZORA and NATSUZORA trials [43]. In the HOSHIZORA trial, the treatment interval was allowed to extend from every 4 weeks to every 8 weeks at the doctor’s discretion for patients receiving ozoralizumab 30 mg and exhibiting a 28-Joint DAS that was maintained at < 3.2 based on the DAS28 erythrocyte sedimentation rate (ESR). The treatment interval was extended in 32 patients, and 28 (87.5%) patients remained on every 8 weeks for 24 weeks. Furthermore, at week 24, 23 of these 32 patients achieved a DAS28-ESR of < 2.6, and 27 patients achieved a DAS28-ESR of < 3.2. Importantly, there were no safety concerns associated with the extension of the treatment interval [43]. These results suggest that the treatment interval can be extended in patients who maintain a DAS28-ESR < 3.2 during the long-term administration of ozoralizumab. Although the concentration of ozoralizumab was not evaluated in this study, these results supported the hypothesis that efficacy is independent of the trough concentration in long-term continuous treatment with ozoralizumab.
4.4 Immunogenicity
Regarding the development of ADAs against ozoralizumab, 29.2–46.8% of the patients showed an increase in the antibody titer or newly generated antibodies by week 52 regardless of the dose of ozoralizumab administered and of whether MTX was used concomitantly [41, 42]. The proportion of neutralizing antibody-positive patients detected by week 52 was 7.0% (10/143 patients) and 5.2% (8/154 patients) for ozoralizumab 30 mg and 80 mg in the OHZORA trial, respectively [41]; and 27.7% (26/94 patients) and 2.2% (1/46 patients) for ozoralizumab 30 mg and 80 mg in the NATSUZORA trial, respectively [42]. Although a reduced efficacy was observed in some patients who were positive for neutralizing antibodies in the 30 mg in the NATSUZORA trial, only 11.5% of them (3/26 patients) discontinued the study because of disease progression.
4.5 Safety
A summary of safety through week 24 (period A; the double-blind treatment period) in the OHZORA trial is shown in Table 3. Most adverse events were mild or moderate. In the ozoralizumab 80-mg group, one event of disseminated tuberculosis was reported as an adverse event leading to death and was determined to be causally related to the drug [40].
Safety data obtained for up to 52 weeks after drug administration in the OHZORA and NATSUZORA trials were combined and evaluated [45]. The incidence of adverse events was 83.8% (243/290 patients) in the 30-mg group and 88.8% (206/232 patients) in the 80-mg group; moreover, the incidences of adverse drug reactions were similar, i.e., 41.0% (119/290 patients) and 41.4% (96/232 patients), respectively. During the safety evaluation of ozoralizumab, adverse events of special interest (such as serious infections and malignancies) were assessed based on the characteristic side-effect profiles identified for existing TNFα inhibitors; however, no events were considered to be at a particularly high risk of occurrence after the administration of ozoralizumab treatment. Furthermore, the incidence of adverse events corresponding to a “reaction at injection site” was 1.4% (4/290 patients) in the 30-mg group and 1.3% (3/232 patients) in the 80-mg group. There was no clear impact on safety based on the presence or absence of expression of ADAs and neutralizing antibodies [45].
5 Summary
The advent of anti-TNFα agents targeting TNFα has significantly advanced the pharmacotherapy of immune-mediated inflammatory diseases. Nevertheless, many unmet needs persist, and the research and development of next-generation anti-TNFα agents constructed in formats different from that of conventional IgG is underway, to provide new therapeutic avenues for these diseases. A llama-derived VHH was developed as a novel format that allows a unique structural design, different from that of previous antibody drugs. Ozoralizumab is a next-generation anti-TNFα agent consisting of two human anti-TNFα VHHs and one anti-HSA VHH connected by glycine-serine linkers. Analyses that were performed using model structures of ozoralizumab and the TNFα trimer suggested that this antibody can simultaneously bind to two sites on a TNFα homotrimer, thus allowing the ozoralizumab-TNFα trimer complex to exist stably. This is the first case of an approved biologic in which such structural stability as a molecule and pharmacokinetic stability obtained through HSA binding were successfully achieved simultaneously.
Ozoralizumab exhibits excellent pharmacokinetics with a plasma half-life of approximately 18 days because of its HSA-binding affinity, which enables its administration to patients with RA at 4-week intervals. In the OHZORA and NATSUZORA trials, an improvement in clinical symptoms was observed at the 30-mg dose, in the presence or in the presence concomitant MTX administration. In addition, sustained efficacy was confirmed for up to 52 weeks. Furthermore, a long-term extension study of patients who achieved a DAS28-ESR < 3.2 in the long-term HOSHIZORA trial suggested that the dosing interval could be extended to 8 weeks.
The unique structure of next-generation antibodies, including ozoralizumab, offers the potential for an early improvement of clinical symptoms, the optimization of drug bioavailability, enhanced tissue penetration, and reduced side effects. A new paradigm shift in biologic therapy using these next-generation anti-TNFα agents is expected.
References
Evangelatos G, Bamias G, Kitas GD, et al. The second decade of anti-TNF-a therapy in clinical practice: new lessons and future directions in the COVID-19 era. Rheumatol Int. 2022;42:1493–511.
Martin KP, Grimaldi C, Grempler R, et al. Trends in industrialization of biotherapeutics: a survey of product characteristics of 89 antibody-based biotherapeutics. MAbs. 2023;15:2191301.
Curtis JR, Singh JA. Use of biologics in rheumatoid arthritis: current and emerging paradigms of care. Clin Ther. 2011;33:679–707.
Takeuchi T. Cytokines and cytokine receptors as targets of immune-mediated inflammatory diseases: RA as a role model. Inflamm Regen. 2022;42:35.
Feldmann M, Maini RN, Soriano ER, Strand V, Takeuchi T. 25 years of biologic DMARDs in rheumatology. Nat Rev Rheumatol. 2023;19:761–6.
Du Pan SM, Dehler S, Ciurea A, et al. Comparison of drug retention rates and causes of drug discontinuation between anti-tumor necrosis factor agents in rheumatoid arthritis. Arthritis Rheum. 2009;61:560–8.
Radawski C, Genovese MC, Hauber B, et al. Patient perceptions of unmet medical need in rheumatoid arthritis: a cross-sectional survey in the USA. Rheumatol Ther. 2019;6:461–71.
Bandrés Ciga S, Salvatierra J, López-Sidro M, et al. An examination of the mechanisms involved in secondary clinical failure to adalimumab or etanercept in inflammatory arthropathies. J Clin Rheumatol. 2015;21:115–9.
Maibom-Thomsen SL, Trier NH, Holm BE, et al. Immunoglobulin G structure and rheumatoid factor epitopes. PLoS ONE. 2019;14: e0217624.
Takanashi S, Kaneko Y, Takeuchi T. Characteristics of patients with difficult-to-treat rheumatoid arthritis in clinical practice. Rheumatology (Oxford). 2021;60:5247–56.
Santos-Moreno P, Sánchez G, Castro C. Rheumatoid factor as predictor of response to treatment with anti-TNF alpha drugs in patients with rheumatoid arthritis: results of a cohort study. Medicine. 2019;98: e14181.
Mancarella L, Bobbio-Pallavicini F, Ceccarelli F, et al. Good clinical response, remission, and predictors of remission in rheumatoid arthritis patients treated with tumor necrosis factor-alpha blockers: the GISEA study. J Rheumatol. 2007;34:1670–3.
Potter C, Hyrich KL, Tracey A, et al. Association of rheumatoid factor and anti-cyclic citrullinated peptide positivity, but not carriage of shared epitope or PTPN22 susceptibility variants, with anti-tumour necrosis factor response in rheumatoid arthritis. Ann Rheum Dis. 2009;68:69–74.
Tugwell PS, Petersson IF, Boers M, et al. Domains selection for patient-reported outcomes: current activities and options for future methods. J Rheumatol. 2011;38:1702–10.
Frank L, Basch E, Selby JV, Patient-Centered Outcomes Research Institute. The PCORI perspective on patient-centered outcomes research. JAMA. 2014;312:1513–4.
Orbai AM, Bingham CO 3rd. Patient reported outcomes in rheumatoid arthritis clinical trials. Curr Rheumatol Rep. 2015;17:28.
Nelson AL. Antibody fragments: hope and hype. MAbs. 2010;2:77–83.
Freise AC, Wu AM. In vivo imaging with antibodies and engineered fragments. Mol Immunol. 2015;67(2):142–52.
Holliger P, Hudson PJ. Engineered antibody fragments and the rise of single domains. Nat Biotechnol. 2005;23:1126–36.
Markham A. Brolucizumab: first approval. Drugs. 2019;79(18):1997–2000.
Sanford M. Blinatumomab: first global approval. Drugs. 2015;75(3):321–7.
Dhillon S. Tebentafusp: first approval. Drugs. 2022;82(6):703–10.
Hathaway L, Sen JM, Keng M. Impact of blinatumomab on patient outcomes in relapsed/refractory acute lymphoblastic leukemia: evidence to date. Patient Relat Outcome Meas. 2018;9:329–37.
Ferrari M, Onuoha SC, Fossati-Jimack L, et al. Novel bispecific antibody for synovial-specific target delivery of anti-TNF therapy in rheumatoid arthritis. Front Immunol. 2021;12: 640070.
Hamers-Casterman C, Atarhouch T, Muyldermans S, et al. Naturally occurring antibodies devoid of light chains. Nature. 1993;363:446–8.
Muyldermans S. Nanobodies: natural single-domain antibodies. Annu Rev Biochem. 2013;82:775–97.
Duggan S. Caplacizumab: first global approval. Drugs. 2018;78:1639–42.
Keam SJ. Ozoralizumab: first approval. Drugs. 2023;83:87–92.
Markham A. Envafolimab: first approval. Drugs. 2022;82:235–40.
Besnerais M, Veyradier A, Benhamou Y, Coppo P. Caplacizumab: a change in the paradigm of thrombotic thrombocytopenic purpura treatment. Expert Opin Biol Ther. 2019;19:1127–34.
Ishiwatari-Ogata C, Kyuuma M, Ogata H, et al. Ozoralizumab, a humanized anti-TNFα NANOBODY® compound, exhibits efficacy not only at the onset of arthritis in a human TNF transgenic mouse but also during secondary failure of administration of an anti-TNFα IgG. Front Immunol. 2022;13: 853008.
Zhang F, Wei H, Wang X, et al. Structural basis of a novel PD-L1 nanobody for immune checkpoint blockade. Cell Discov. 2017;3:17004.
Takeuchi T. Structural, nonclinical, and clinical features of ozoralizumab: a novel tumour necrosis factor inhibitor. Mod Rheumatol. 2023;33:1059–67.
Beirnaert E, Desmyter A, Spinelli S, et al. Bivalent Llama Single-domain antibody fragments against tumor necrosis factor have picomolar potencies due to intramolecular interactions. Front Immunol. 2017;8:867. https://doi.org/10.3389/fimmu.2017.00867.
Taisho Pharmaceutical Co., Ltd. Nanozora (ozoralizumab) 30 mg syringes/autoinjectors for S.C. injection package insert [in Japanese]. 2022. https://www.info.pmda.go.jp/go/pack/3999467G1023_1_03/?view=frame&style=XML&lang=ja. Accessed 23 Jan 2024.
Taisho Pharmaceutical Co., Ltd. Nanozora (ozoralizumab) common technical document [in Japanese]. https://www.pmda.go.jp/drugs/2022/P20220824002/index.html. Accessed 23 Jan 2024.
Kyuuma M, Kaku A, Mishima-Tsumagari C, et al. Unique structure of ozoralizumab, a trivalent anti-TNFα NANOBODY® compound, offers the potential advantage of mitigating the risk of immune complex-induced inflammation. Front Immunol. 2023;14:1149874.
Oyama S, Ebina K, Etani Y, et al. A novel anti-TNF-α drug ozoralizumab rapidly distributes to inflamed joint tissues in a mouse model of collagen induced arthritis. Sci Rep. 2022;12:18102.
Coppieters K, Dreier T, Silence K, et al. Formatted anti-tumor necrosis factor α VHH proteins derived from camelids show superior potency and targeting to inflamed joints in a murine model of collagen-induced arthritis. Arthritis Rheum. 2006;54:1856–66.
Takeuchi T, Kawanishi M, Nakanishi M, et al. Phase II/III results of a trial of anti-tumor necrosis factor multivalent NANOBODY compound ozoralizumab in patients with rheumatoid arthritis. Arthritis Rheumatol. 2022;74:1776–85.
Tanaka Y, Kawanishi M, Nakanishi M, et al. Efficacy and safety of the anti-TNF multivalent NANOBODY® compound ozoralizumab in patients with rheumatoid arthritis and an inadequate response to methotrexate: a 52-week result of a phase II/III study (OHZORA trial). Mod Rheumatol. 2023;33:883–90.
Tanaka Y, Kawanishi M, Nakanishi M, et al. Efficacy and safety of anti-TNF multivalent NANOBODY® compound ‘ozoralizumab’ without methotrexate co-administration in patients with active rheumatoid arthritis: a 52-week result of phase III, randomised, open-label trial (NATSUZORA trial). Mod Rheumatol. 2023;33(5):875–82.
Takeuchi T, Nakanishi M, Kawanishi M, et al. Effect of extended dosing interval of anti-TNF-alpha NANOBODY® compound ozoralizumab in patients with low disease activity rheumatoid arthritis. Mod Rheumatol. 2023. https://doi.org/10.1093/mr/road097.
Takeuchi T, Chino Y, Kawanishi M, et al. Efficacy and pharmacokinetics of ozoralizumab, an anti-TNFα NANOBODY® compound, in patients with rheumatoid arthritis: 52-week results from the OHZORA and NATSUZORA trials. Arthritis Res Ther. 2023;25:60.
Kawanishi M, Fujii Y. Pharmacological profiles and clinical efficacy of ozoralizumab (Nanozora® 30 mg syringes for S.C. injection), the first Nanobody® compound in Japan [in Japanese]. Nihon Yakurigaku Zasshi. 2023;158:490–9.
Acknowledgements
NANOBODY® is a registered trademark of Ablynx NV, an affiliate of Sanofi. Ablynx NV originally discovered and performed the initial development of the NANOBODY® compounds ozoralizumab and caplacizumab.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Funding support for the original clinical studies of ozoralizumab was provided by Taisho Pharmaceutical Co., Ltd. In addition, Taisho Pharmaceutical Co., Ltd. provided funding for editorial support and publication of the article.
Conflicts of interest/competing interests
Kouhei Tsumoto and Tsutomu Takeuchi have received honoraria for lectures and consulting fees from Taisho Pharmaceutical Co. Ltd.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
The data generated and/or analyzed in the cited papers of ozoralizumab used to write this review article was supplied by Taisho Pharmaceutical Co., Ltd. under license and, therefore, cannot be made freely available. Requests for access to these data should be made to the corresponding author.
Code availability
Not applicable.
Authors’ contributions
TT drafted the overall concept and primarily wrote the manuscript regarding the clinical trials. KT mainly prepared the manuscript for the fragment antibody and ozoralizumab (Sects. 2 and 3). All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Tsumoto, K., Takeuchi, T. Next-Generation Anti-TNFα Agents: The Example of Ozoralizumab. BioDrugs 38, 341–351 (2024). https://doi.org/10.1007/s40259-024-00648-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-024-00648-3