Abstract
Background
Childhood illness can impose significant costs and health strains on family members, but these are not routinely captured by pediatric economic evaluations. This review investigated how family “spillover effects” related to costs and health outcomes are considered in pediatric cost-utility analyses (CUAs).
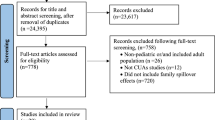
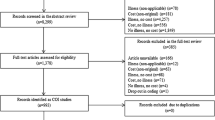
Methods
We reviewed pediatric CUAs published between 2000 and 2015 using the Tufts Medical Center Cost-effectiveness Analysis (CEA) Registry and the Pediatric Economic Database Evaluation (PEDE) Registry. We selected studies conducted from the societal perspective and included in both registries. We investigated how frequently family spillover was incorporated into analyses, and how the inclusion of spillover health effects and costs changed CUA results.
Results
We found 142 pediatric CUAs meeting inclusion criteria. Of those, 105 (72%) considered either family spillover costs (n = 98 time costs, n = 33 out-of-pocket costs, n = 2 caregiver healthcare costs) or health outcomes (n = 15). Twenty-four studies included 43 pairs of incremental cost-effectiveness ratios (ICERs) with and without spillover. In 19 pairs of ICERs, adding spillover changed the ICER enough to cross a common cost-effectiveness threshold (i.e., $50,000/QALY, $100,000/QALY, $150,000/QALY; values are in 2016 US$). Incorporating spillover generally made interventions more cost-effective (n = 18; 42%), or did not change CUA results enough to cross a threshold (n = 24; 56%). Including family spillover reduced ICERs by 31% ($40,000/QALY) on average.
Conclusion
Most pediatric CUAs conducted from a societal perspective include family costs but fewer include family health effects. Inclusion of family spillover effects tends to make CUA results more favorable. Future pediatric CUAs should aim to more fully incorporate the family burden of illness.

Source: Authors’ calculation based on data from: 1 Bos et al. 2003 [60]; 2 Coyle and Barbeau [61]; 3–8 Barton et al. [62]; 9–11 Coco [63]; 12–14 Goossens et al. [30]; 15 Bergman et al. [64]; 16 Luce et al. [65]; 17–20 Bilcke et al. [28]; 21 Martin et al. [33]; 22 Shim and Galvani [37]; 23 Talbird et al. [66]; 24 Tan et al. [67]; 25 Rozenbaum et al. [35]; 26 Sato et al. [36]; 27–28 Perez-Rubio et al. [34]; 29–32 Coyle et al. [29]; 33–34 Hoshi et al. [68]; 35 Suwantika et al. [38]; 36 Itzler et al. [32]; 37 Imaz et al. [31]; 38 Shiragami et al. [69]; 39 Al Awaidy et al. [27]; 40–41 van der Schans et al. [25]; 42–43 Schawo et al. [26]

Source: Authors’ calculation based on data from 17 studies: 1 Bos et al. [60]; 2 Coyle and Barbeau [61]; 3–8 Barton et al. [62]; 9–10 Coco [63]; 11–13 Goossens et al. [30]; 14 Bergman et al. [64]; 15 Luce et al. [65]; 16 Martin et al. [33]; 17 Talbird et al. [66]; 18 Tan et al. [67]; 19 Sato et al. [36]; 20–21 Hoshi et al. [68]; 22 Suwantika et al. [38]; 23 Shiragami et al. [69]; 24–25 van der Schans et al. [25]; 26–27 Bilcke et al. [28]; 28–29 Coyle et al. [29]
Similar content being viewed by others
Data Availability Statement
In a supplementary document (Online Supplementary Material), we have included all abstracted data for a subset of 24 of the studies in our review that were used to recalculate incremental cost effectiveness ratios with and without spillover included. Abstracted data from remaining studies are available in the referenced literature.
References
Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-effectiveness in health and medicine. Oxford: Oxford University Press; 1996.
Neumann PJ, Sanders GD, Russell LB, Siegel JE, Ganiats TG. Cost-effectiveness in health and medicine. Oxford: Oxford University Press; 2016.
Guidelines for the Economic Evaluation of Health Technologies: Canadian Agency for Drugs and Technologies in Health. 2017.
National Institute for Health and Care Excellence (NICE). Guide to the methods of technology appraisal. London: National Institute for Health and Care Excellence; 2013.
NHS Scotland-Scottish Medicines Consortium. Guidance to manufacturers for completion of new product assessment form 2007. http://www.ispor.org/PEguidelines/source/GuidanceinScotland-June2007.pdf. Accessed 22 Apr 2018.
Zorginstituut Nederland. Guideline for the Conduct of Economic Evaluations in Health Care. 2016. http://www.ispor.org/PEguidelines/source/Netherlands_Guideline_for_economic_evaluations_in_healthcare.pdf. Accessed 22 Apr 2018.
Krol M, Papenburg J, van Exel J. Does including informal care in economic evaluations matter? A systematic review of inclusion and impact of informal care in cost-effectiveness studies. Pharmacoeconomics. 2015;33(2):123–35.
Basu A, Meltzer D. Implications of spillover effects within the family for medical cost-effectiveness analysis. J Health Econ. 2005;24(4):751–73.
Brouwer WBF, van Exel Job, Mick TJ. Incorporating caregiver and family effects in economic evaluations of child health. In: Ungar W, editor. Economic evaluation in child health. Toronto: Oxford Scholarship Online; 2010.
Lavelle TA, Wittenberg E, Lamarand K, Prosser LA. Variation in the spillover effects of illness on parents, spouses, and children of the chronically ill. Appl Health Econ Health Policy. 2014;12(2):117–24.
van Oers HA, Haverman L, Limperg PF, van Dijk-Lokkart EM, Maurice-Stam H, Grootenhuis MA. Anxiety and depression in mothers and fathers of a chronically ill child. Matern Child Health J. 2014;18(8):1993–2002.
Wittenberg E, Ritter GA, Prosser LA. Evidence of spillover of illness among household members: EQ-5D scores from a US sample. Med Decis Making. 2013;33(2):235–43.
Winthrop AL, Brasel KJ, Stahovic L, Paulson J, Schneeberger B, Kuhn EM. Quality of life and functional outcome after pediatric trauma. J Trauma. 2005;58(3):468–73.
Ortega-Sanchez IR, Molinari NA, Fairbrother G, Szilagyi PG, Edwards KM, Griffin MR, et al. Indirect, out-of-pocket and medical costs from influenza-related illness in young children. Vaccine. 2012;30(28):4175–81.
Brouwer WB, van Exel NJ, van den Berg B, van den Bos GA, Koopmanschap MA. Process utility from providing informal care: the benefit of caring. Health Policy. 2005;74(1):85–99.
Wittenberg E, Saada A, Prosser LA. How illness affects family members: a qualitative interview survey. Patient Patient Center Outcomes Res. 2013;6(4):257–68.
Goodrich K, Kaambwa B, Al-Janabi H. The inclusion of informal care in applied economic evaluation: a review. Value Health. 2012;15(6):975–81.
Thorat T, Cangelosi M, Neumann PJ. Skills of the trade: the Tufts Cost-Effectiveness Analysis (CEA) Registry. J Benefit Cost Anal. 2012;3:1–9.
Ungar WJ. The Pediatric Economic Database Evaluation (PEDE) project. 2015. http://pede.ccb.sickkids.ca/pede/index.jsp. Accessed 22 Apr 2018.
Ungar WJ, Santos MT. The Pediatric Economic Database Evaluation (PEDE) Project: establishing a database to study trends in pediatric economic evaluation. Med Care. 2003;41(10):1142–52.
Neumann PJ, Greenberg D, Olchanski NV, Stone PW, Rosen AB. Growth and quality of the cost-utility literature, 1976-2001. Value Health. 2005;8(1):3–9.
Neumann PJ, Thorat T, Shi J, Saret CJ, Cohen JT. The changing face of the cost-utility literature, 1990-2012. Value Health. 2015;18(2):271–7.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42(2):377–81.
Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness–the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371(9):796–7.
van der Schans J, Kotsopoulos N, Hoekstra PJ, Hak E, Postma MJ. Cost-effectiveness of extended-release methylphenidate in children and adolescents with attention-deficit/hyperactivity disorder sub-optimally treated with immediate release methylphenidate. PLoS One. 2015;10(5):e0127237.
Schawo S, van der Kolk A, Bouwmans C, Annemans L, Postma M, Buitelaar J, et al. Probabilistic markov model estimating cost effectiveness of methylphenidate osmotic-release oral system versus immediate-release methylphenidate in children and adolescents: which information is needed? Pharmacoeconomics. 2015;33(5):489–509.
Al Awaidy ST, Gebremeskel BG, Al Obeidani I, Al Baqlani S, Haddadin W, O’Brien MA. Cost effectiveness of a pentavalent rotavirus vaccine in Oman. BMC Infect Dis. 2014;17(14):334.
Bilcke J, Van Damme P, Beutels P. Cost-effectiveness of rotavirus vaccination: exploring caregiver(s) and “no medical care’’ disease impact in Belgium. Med Decis Making. 2009;29(1):33–50.
Coyle D, Coyle K, Bettinger JA, Halperin SA, Vaudry W, Scheifele DW, et al. Cost effectiveness of infant vaccination for rotavirus in Canada. Can J Infect Dis Med Microbiol. 2012;23(2):71–7.
Goossens LM, Standaert B, Hartwig N, Hovels AM, Al MJ. The cost-utility of rotavirus vaccination with Rotarix (RIX4414) in the Netherlands. Vaccine. 2008;26(8):1118–27.
Imaz I, Rubio B, Cornejo AM, Gonzalez-Enriquez J. Budget impact and cost-utility analysis of universal infant rotavirus vaccination in Spain. Prev Med. 2014;61:116–21.
Itzler R, O’Brien MA, Yamabe K, Abe M, Dhankhar P. Cost-effectiveness of a pentavalent rotavirus vaccine in Japan. J Med Econ. 2013;16(10):1216–27.
Martin A, Batty A, Roberts JA, Standaert B. Cost-effectiveness of infant vaccination with RIX4414 (Rotarix) in the UK. Vaccine. 2009;27(33):4520–8.
Perez-Rubio A, Luquero FJ, Eiros Bouza JM, Castrodeza Sanz JJ, Bachiller Luque MR, de Lejarazu RO, et al. Socio-economic modelling of rotavirus vaccination in Castilla y Leon, Spain. Infez Med. 2011;19(3):166–75.
Rozenbaum MH, Mangen MJ, Giaquinto C, Wilschut JC, Hak E, Postma MJ, et al. Cost-effectiveness of rotavirus vaccination in the Netherlands; the results of a consensus model. BMC Public Health. 2011;10(11):462.
Sato T, Nakagomi T, Nakagomi O. Cost-effectiveness analysis of a universal rotavirus immunization program in Japan. Jpn J Infect Dis. 2011;64(4):277–83.
Shim E, Galvani AP. Impact of transmission dynamics on the cost-effectiveness of rotavirus vaccination. Vaccine. 2009;27(30):4025–30.
Suwantika AA, Tu HA, Postma MJ. Cost-effectiveness of rotavirus immunization in Indonesia: taking breastfeeding patterns into account. Vaccine. 2013;31(32):3300–7.
Al-Janabi H, Van Exel J, Brouwer W, Trotter C, Glennie L, Hannigan L, et al. measuring health spillovers for economic evaluation: a case study in meningitis. Health Econ. 2016;25(12):1529–44.
Brooks R. EuroQol: the current state of play. Health Policy. 1996;37(1):53–72.
Khanna R, Jariwala K, Bentley JP. Psychometric properties of the EuroQol Five Dimensional Questionnaire (EQ-5D-3L) in caregivers of autistic children. Qual Life Res. 2013;22(10):2909–20.
Bhadhuri A, Jowett S, Jolly K, Al-Janabi H. A comparison of the validity and responsiveness of the EQ-5D-5L and SF-6D for measuring health spillovers: a study of the family impact of meningitis. Med Decis Making. 2017;37(8):882–93.
EuroQol Group. EuroQol–a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208.
Brouwer WB, van Exel NJ, van Gorp B, Redekop WK. The CarerQol instrument: a new instrument to measure care-related quality of life of informal caregivers for use in economic evaluations. Qual Life Res. 2006;15(6):1005–21.
Al-Janabi H, Flynn TN, Coast J. Estimation of a preference-based carer experience scale. Med Decis Making. 2011;31(3):458–68.
Prosser LA, Hammitt JK, Keren R. Measuring health preferences for use in cost-utility and cost-benefit analyses of interventions in children: theoretical and methodological considerations. Pharmacoeconomics. 2007;25(9):713–26.
Petrou S. Methodological issues raised by preference-based approaches to measuring the health status of children. Health Econ. 2003;12(8):697–702.
O’Brien MA, Prosser LA, Paradise JL, Ray GT, Kulldorff M, Kurs-Lasky M, et al. New vaccines against otitis media: projected benefits and cost-effectiveness. Pediatrics. 2009;123(6):1452–63.
Prosser LA, Meltzer MI, Fiore A, Epperson S, Bridges CB, Hinrichsen V, et al. Effects of adverse events on the projected population benefits and cost-effectiveness of using live attenuated influenza vaccine in children aged 6 months to 4 years. Arch Pediatr Adolesc Med. 2011;165(2):112–8.
Bobinac A, van Exel NJ, Rutten FF, Brouwer WB. Health effects in significant others: separating family and care-giving effects. Med Decis Making. 2011;31(2):292–8.
Hoefman RJ, van Exel J, Brouwer W. How to include informal care in economic evaluations. Pharmacoeconomics. 2013;31(12):1105–19.
Bobinac A, van Exel NJ, Rutten FF, Brouwer WB. Caring for and caring about: disentangling the caregiver effect and the family effect. J Health Econ. 2010;29(4):549–56.
Prosser LA, Lamarand K, Gebremariam A, Wittenberg E. Measuring family HRQoL spillover effects using direct health utility assessment. Med Decis Making. 2015;35(1):81–93.
Al-Janabi H, van Exel J, Brouwer W, Coast J. A framework for including family health spillovers in economic evaluation. Med Decis Making. 2016;36(2):176–86.
Richardson JS. Assessing the Economic and Quality of Life Impacts of Grief and Suicide in the United States [dissertation]: The University of Michigan; 2018.
Fox M, Cacciatore J, Lacasse JR. Child death in the United States: productivity and the economic burden of parental grief. Death Stud. 2014;38(6–10):597–602.
Lichtenthal WG, Corner GW, Sweeney CR, Wiener L, Roberts KE, Baser RE, et al. Mental Health services for parents who lost a child to cancer: if we build them, will they come? J Clin Oncol. 2015;33(20):2246–53.
Ungar W. Economic evaluation in child health. Oxford: Oxford University Press; 2009.
Lavelle TA, Weinstein MC, Newhouse JP, Munir K, Kuhlthau KA, Prosser LA. Economic burden of childhood autism spectrum disorders. Pediatrics. 2014;133(3):e520–9.
Bos JM, Rumke H, Welte R, Postma MJ. Epidemiologic impact and cost-effectiveness of universal infant vaccination with a 7-valent conjugated pneumococcal vaccine in the Netherlands. Clin Ther. 2003;25(10):2614–30.
Coyle D, Barbeau M. Cost effectiveness of Elidel in the management of patients with atopic dermatitis in Canada. J Cutan Med Surg. 2004;8(6):405–10.
Barton GR, Stacey PC, Fortnum HM, Summerfield AQ. Hearing-impaired children in the United Kingdom, IV: cost-effectiveness of pediatric cochlear implantation. Ear Hear. 2006;27(5):575–88.
Coco AS. Cost-effectiveness analysis of treatment options for acute otitis media. Ann Fam Med. 2007;5(1):29–38.
Bergman A, Hjelmgren J, Ortqvist A, Wisloff T, Kristiansen IS, Hogberg LD, et al. Cost-effectiveness analysis of a universal vaccination programme with the 7-valent pneumococcal conjugate vaccine (PCV-7) in Sweden. Scand J Infect Dis. 2008;40(9):721–9.
Luce BR, Nichol KL, Belshe RB, Frick KD, Li SX, Boscoe A, et al. Cost-effectiveness of live attenuated influenza vaccine versus inactivated influenza vaccine among children aged 24–59 months in the United States. Vaccine. 2008;26(23):2841–8.
Talbird SE, Brogan AJ, Winiarski AP, Sander B. Cost-effectiveness of treating influenzalike illness with oseltamivir in the United States. Am J Health Syst Pharm. 2009;66(5):469–80.
Tan SS, van Linschoten RL, van Middelkoop M, Koes BW, Bierma-Zeinstra SM, Koopmanschap MA. Cost-utility of exercise therapy in adolescents and young adults suffering from the patellofemoral pain syndrome. Scand J Med Sci Sports. 2010;20(4):568–79.
Hoshi SL, Kondo M, Okubo I. Economic evaluation of vaccination programme of 13-valent pneumococcal conjugate vaccine to the birth cohort in Japan. Vaccine. 2013;31(25):2762–71.
Shiragami M, Mizukami A, Leeuwenkamp O, et al. Cost-Effectiveness evaluation of the 10-valent pneumococcal non-typeable haemophilus influenzae protein D conjugate vaccine and 13-valent pneumococcal vaccine in Japanese children. Infect Dis Ther. 2015;4(1):93–112. https://doi.org/10.1007/s40121-014-0053-7.
Acknowledgements
We would like to acknowledge Ashley Leech, PhD for her comments during the literature review process, and Peter Neumann, ScD for his comments on the manuscript.
Author information
Authors and Affiliations
Contributions
Study concept and design: Lavelle, Lin, D’Cruz, Prosser, Ungar, Mohit, Vera-Llonch; data acquisition: Tsiplova, Lin, D’Cruz, and Lavelle; drafting publication: Lavelle, Lin, D’Cruz; all authors participated in analysis or interpretation of data as well as preparation and critical revision of the manuscript.
Corresponding author
Ethics declarations
Funding
This study was supported by research funding from Shire Pharmaceuticals to Tufts Medical Center.
Conflict of interest
Montserrat Vera-Llonch is an employee of Shire and owns stock/options. Tara Lavelle, Brittany D’Cruz, and Pei-Jung Lin were funded by a grant from Shire during this work. Wendy Ungar reports receiving a consulting fee from Tufts Medical Center for her contribution to this work. Babak Mohit reports receiving funds from Bayer to support his post-doctoral fellowship. Pei-Jung Lin reports personal fees from Avanir and Otsuka, outside of the scope of this work. Lisa Prosser and Kate Tsiplova report no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lavelle, T.A., D’Cruz, B.N., Mohit, B. et al. Family Spillover Effects in Pediatric Cost-Utility Analyses. Appl Health Econ Health Policy 17, 163–174 (2019). https://doi.org/10.1007/s40258-018-0436-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-018-0436-0