Abstract
Acne vulgaris is one of the most common skin disorders worldwide. It typically affects skin areas with a high density of sebaceous glands such as the face, upper arms, chest, and/or back. Historically, the majority of research efforts have focused on facial acne vulgaris, even though approximately half of patients with facial lesions demonstrate truncal involvement. Truncal acne vulgaris is challenging to treat and poses a significant psychosocial burden on patients. Despite these characteristics, studies specifically examining truncal acne vulgaris are limited, with treatment guidelines largely derived from facial protocols. Therefore, truncal acne remains an understudied clinical problem. Here, we provide a clinically focused review on the epidemiology, evaluation, and available treatment options for truncal acne vulgaris. In doing so, we highlight knowledge gaps with the goal of spurring further investigation into the management of truncal acne vulgaris.





Similar content being viewed by others
References
Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163–96.
McConnell RC, Fleischer AB Jr, Williford PM, et al. Most topical tretinoin treatment is for acne vulgaris through the age of 44 years: an analysis of the National Ambulatory Medical Care Survey, 1990–1994. J Am Acad Dermatol. 1998;38:221–6.
Collier CN, Harper JC, Cafardi JA, et al. The prevalence of acne in adults 20 years and older. J Am Acad Dermatol. 2008;58:56–9.
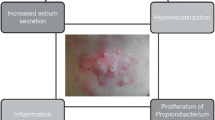
Moradi Tuchayi S, Makrantonaki E, Ganceviciene R, et al. Acne vulgaris. Nat Rev Dis Primers. 2015;1:15029.
Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74:945–73.
Nast A, Dreno B, Bettoli V, et al. European evidence-based (S3) guideline for the treatment of acne: update 2016: short version. J Eur Acad Dermatol Venereol. 2016;30:1261–8.
Del Rosso JQ, Bikowski JB, Baum E, et al. A closer look at truncal acne vulgaris: prevalence, severity, and clinical significance. J Drugs Dermatol. 2007;6:597–600.
Del Rosso JQ, Stein-Gold L, Lynde C, et al. Truncal acne: a neglected entity. J Drugs Dermatol. 2019;18:205–1208.
Tan J, Beissert S, Cook-Bolden F, et al. Impact of facial and truncal acne on quality of life: a multi-country population-based survey. JAAD Int. 2021;3:102–10.
Papadopoulos L, Walker C, Aitken D, Bor R. The relationship between body location and psychological morbidity in individuals with acne vulgaris. Psychol Health Med. 2000;5:431–8.
Hassan J, Grogan S, Clark-Carter D, et al. The individual health burden of acne: appearance-related distress in male and female adolescents and adults with back, chest and facial acne. J Health Psychol. 2009;14:1105–18.
Tan JJK, Tang J, Fung K, et al. Prevalence and severity of facial and truncal acne in a referral cohort. J Drugs Dermatol. 2008;7:551–6.
Dreno B, Jean-Decoster C, Georgescu V. Profile of patients with mild-to-moderate acne in Europe: a survey. Eur J Dermatol. 2016;26:177–84.
Goncalves G, Amado JM, Matos ME, et al. The prevalence of acne among a group of Portuguese medical students. J Eur Acad Dermatol Venereol. 2012;6:514–7.
Tan J, Del Rosso JQ, Weiss JS, et al. Prevalence and demographics of truncal involvement among acne patients: survey data and a review of the literature. J Clin Aesthet Dermatol. 2022;15:62–7.
Isaacsson VC, Almeida JRHL, Duquia RP, et al. Dissatisfaction and acne vulgaris in male adolescents and associated factors. An Bras Dermatol. 2014;89:576–9.
Dreno B, Thiboutot D, Layton AM, et al. Large-scale international study enhances understanding of an emerging acne population: adult females. J Eur Acad Dermatol Venereol. 2015;29:1096–106.
Radi R, Gold S, Acosta JP, et al. Treating acne in transgender persons receiving testosterone: a practical guide. Am J Clin Dermatol. 2022;23:219–29.
Wierckx K, Van de Peer F, Verhaeghe E, et al. Short- and long-term clinical skin effects of testosterone treatment in trans men. J Sex Med. 2014;11:222–9.
Plewig G, Melnik B, Chen W. Acne-mimicking diseases, Plewig and Kligman’s acne and rosacea. Cham: Springer International Publishing; 2019. p. 299–410.
Wu DC, Chan WW, Metelitsa AI, et al. Pseudomonas skin infection: clinical features, epidemiology, and management. Am J Clin Dermatol. 2011;12:157–69.
Boni R, Nehrhoff B. Treatment of gram-negative folliculitis in patients with acne. Am J Clin Dermatol. 2003;4:273–6.
Luelmo-Aguilar J, Santandreu MS. Folliculitis: recognition and management. Am J Clin Dermatol. 2004;5:301–10.
Back O, Faergemann J, Hornqvist R. Pityrosporum folliculitis: a common disease of the young and middle-aged. J Am Acad Dermatol. 1985;12:56–61.
Ayers K, Sweeney SM, Wiss K. Pityrosporum folliculitis: diagnosis and management in 6 female adolescents with acne vulgaris. Arch Pediatr Adolesc Med. 2005;159:64–7.
Ponka D, Baddar F. Wood lamp examination. Can Fam Physician. 2012;58:976.
Durdu M, Guran M, Ilkit M. Epidemiological characteristics of Malassezia folliculitis and use of the May-Grunwald-Giemsa stain to diagnose the infection. Diagn Microbiol Infect Dis. 2013;76:450–7.
Poli F. Differential diagnosis of facial acne on black skin. Int J Dermatol. 2012;51(24–26):27–9.
Jacinto-Jamora S, Tamesis J, Katigbak ML. Pityrosporum folliculitis in the Philippines: diagnosis, prevalence, and management. J Am Acad Dermatol. 1991;24:693–6.
Hald M, Arendrup MC, Svejgaard EL, et al. Evidence-based Danish guidelines for the treatment of Malassezia-related skin diseases. Acta Derm Venereol. 2015;95:12–9.
Rosenthal D, LeBoit PE, Klumpp L, et al. Human immunodeficiency virus-associated eosinophilic folliculitis: a unique dermatosis associated with advanced human immunodeficiency virus infection. Arch Dermatol. 1991;127:206–9.
Parker SR, Parker DC, McCall CO. Eosinophilic folliculitis in HIV-infected women: case series and review. Am J Clin Dermatol. 2006;7:193–200.
Bull RH, Harland CA, Fallowfield ME, et al. Eosinophilic folliculitis: a self-limiting illness in patients being treated for haematological malignancy. Br J Dermatol. 1993;129:178–82.
Evans TR, Mansi JL, Bull R, et al. Eosinophilic folliculitis occurring after bone marrow autograft in a patient with non-Hodgkin’s lymphoma. Cancer. 1994;73:2512–4.
Teraki Y, Konohana I, Shiohara T, et al. Eosinophilic pustular folliculitis (Ofuji’s disease): immunohistochemical analysis. Arch Dermatol. 1993;129:1015–9.
Ellis E, Scheinfeld N. Eosinophilic pustular folliculitis: a comprehensive review of treatment options. Am J Clin Dermatol. 2004;5:189–97.
Paichitrojjana A. Demodicosis imitating acne vulgaris: a case report. Clin Cosmet Investig Dermatol. 2022;15:497–501.
Chen W, Plewig G. Human demodicosis: revisit and a proposed classification. Br J Dermatol. 2014;170:1219–25.
Forton F, Seys B. Density of Demodex folliculorum in rosacea: a case-control study using standardized skin-surface biopsy. Br J Dermatol. 1993;128:650–9.
Huang HP, Hsu CK, Lee JY. A new superficial needle-scraping method for assessing Demodex density in papulopustular rosacea. J Cosmet Dermatol. 2020;19:896–900.
Aktas Karabay E, Aksu CA. Demodex folliculorum infestations in common facial dermatoses: acne vulgaris, rosacea, seborrheic dermatitis. An Bras Dermatol. 2020;95:187–93.
Salem DA, El-Shazly A, Nabih N, et al. Evaluation of the efficacy of oral ivermectin in comparison with ivermectin-metronidazole combined therapy in the treatment of ocular and skin lesions of Demodex folliculorum. Int J Infect Dis. 2013;17:e343–7.
Sarac G. A comparison of the efficacy and tolerability of topical agents used in facial Demodex treatment. J Cosmet Dermatol. 2019;18:1784–7.
Bikowski JB, Del Rosso JQ. Demodex dermatitis: a retrospective analysis of clinical diagnosis and successful treatment with topical crotamiton. J Clin Aesthet Dermatol. 2009;2:20–5.
Jacot W, Bessis D, Jorda E, et al. Acneiform eruption induced by epidermal growth factor receptor inhibitors in patients with solid tumours. Br J Dermatol. 2004;151:238–41.
Hurwitz RM. Steroid acne. J Am Acad Dermatol. 1989;21:1179–81.
Nielsen JN, Licht RW, Fogh K. Two cases of acneiform eruption associated with lamotrigine. J Clin Psychiatry. 2004;65:1720–2.
Yeung CK, Chan HH. Cutaneous adverse effects of lithium: epidemiology and management. Am J Clin Dermatol. 2004;5:3–8.
Bieber T, Simpson EL, Silverberg JI, et al. Abrocitinib versus placebo or dupilumab for atopic dermatitis. N Engl J Med. 2021;384:1101–12.
Kazandjieva J, Tsankov N. Drug-induced acne. Clin Dermatol. 2017;35:156–62.
Du-Thanh A, Kluger N, Bensalleh H, et al. Drug-induced acneiform eruption. Am J Clin Dermatol. 2011;12:233–45.
Scope A, Agero AL, Dusza SW, et al. Randomized double-blind trial of prophylactic oral minocycline and topical tazarotene for cetuximab-associated acne-like eruption. J Clin Oncol. 2007;25:5390–6.
Wenzel FG, Horn TD. Nonneoplastic disorders of the eccrine glands. J Am Acad Dermatol. 1998;38:1–17.
Carter R 3rd, Garcia AM, Souhan BE. Patients presenting with miliaria while wearing flame resistant clothing in high ambient temperatures: a case series. J Med Case Rep. 2011;5:474.
Ale I, Lachapelle JM, Maibach HI. Skin tolerability associated with transdermal drug delivery systems: an overview. Adv The. 2009;26:920–35.
Hu CH, Michel B, Farber EM. Transient acantholytic dermatosis (Grover’s disease): a skin disorder related to heat and sweating. Arch Dermatol. 1985;121:1439–41.
French LE, Piletta PA, Etienne A, et al. Incidence of transient acantholytic dermatosis (Grover’s disease) in a hospital setting. Dermatology. 1999;198:410–1.
Parsons JM. Transient acantholytic dermatosis (Grover’s disease): a global perspective. J Am Acad Dermatol. 1996;35:653–66.
Quirk CJ, Heenan PJ. Grover’s disease: 34 years on. Australas J Dermatol. 2004;45:83–6.
Orlowski TJR, Graham LV. Truncal demodex folliculitis. Skin. 2020;2:365–8.
Hafsi W, Badri T. Acne conglobata. Treasure Island: StatPearls; 2022.
Yiu ZZ, Madan V, Griffiths CE. Acne conglobata and adalimumab: use of tumour necrosis factor-alpha antagonists in treatment-resistant acne conglobata, and review of the literature. Clin Exp Dermatol. 2015;40:383–6.
Dessinioti C, Katsambas A. Difficult and rare forms of acne. Clin Dermatol. 2017;35:138–46.
Melnik B, Jansen T, Grabbe S. Abuse of anabolic-androgenic steroids and bodybuilding acne: an underestimated health problem. J Dtsch Dermatol Ges. 2017;5:110–7.
Weimann E, Bohles HJ. Acute acne fulminans et conglobata after the end of high-dose testosterone therapy for hereditary tall stature. Klin Padiatr. 1999;211:410–2.
Chicarilli ZN. Follicular occlusion triad: hidradenitis suppurativa, acne conglobata, and dissecting cellulitis of the scalp. Ann Plast Surg. 1987;18:230–7.
Vasanth V, Chandrashekar BS. Follicular occlusion tetrad. Indian Dermatol Online J. 2014;5:491–3.
Musumeci ML, Fiorentini F, Bianchi L, et al. Follicular occlusion tetrad in a male patient with pachyonychia congenita: clinical and genetic analysis. J Eur Acad Dermatol Venereol. 2019;33(Suppl. 6):36–9.
Peck GL, Olsen TG, Butkus D, et al. Isotretinoin versus placebo in the treatment of cystic acne. A randomized double-blind study. J Am Acad Dermatol. 1982;6:735–45.
Gollnick HP, Graupe K, Zaumseil RP. Comparison of combined azelaic acid cream plus oral minocycline with oral isotretinoin in severe acne. Eur J Dermatol. 2011;11:538–44.
Tan MG, Worley B, Kim WB, et al. Drug-induced intracranial hypertension:a systematic review and critical assessment of drug-induced causes. Am J Clin Dermatol. 2020;21:163–72.
Sand FL, Thomsen SF. Adalimumab for the treatment of refractory acne conglobata. JAMA Dermatol. 2013;149:1306–7.
Shirakawa M, Uramoto K, Harada FA. Treatment of acne conglobata with infliximab. J Am Acad Dermatol. 2006;55:344–6.
Greywal T, Zaenglein AL, Baldwin HE, et al. Evidence-based recommendations for the management of acne fulminans and its variants. J Am Acad Dermatol. 2017;77:109–17.
Li AW, Antaya RJ. Isotretinoin-induced acne fulminans without systemic symptoms with concurrent exuberant granulation tissue. Pediatr Dermatol. 2018;35:257–8.
Tan J, Thiboutot D, Popp G, et al. Randomized phase 3 evaluation of trifarotene 50 mug/g cream treatment of moderate facial and truncal acne. J Am Acad Dermatol. 2019;80:1691–9.
Mallon E, Newton JN, Klassen A, et al. The quality of life in acne: a comparison with general medical conditions using generic questionnaires. Br J Dermatol. 1999;140:672–6.
Tan JK, Zhang X, Jones E, et al. Correlation of photographic images from the Leeds revised acne grading system with a six-category global acne severity scale. J Eur Acad Dermatol Venereol. 2013;27:e414–9.
Obrien SCL, Cunliffe WJ. The Leeds revised acne grading system. J Dermatol Treat. 1998;9:215–20.
Allen BS, Smith JG Jr. Various parameters for grading acne vulgaris. Arch Dermatol. 1982;118:23–5.
Tan JK, Tang J, Fung K, et al. Development and validation of a comprehensive acne severity scale. J Cutan Med Surg. 2007;11:211–6.
Dreno B, Khammari A, Orain N, et al. ECCA grading scale: an original validated acne scar grading scale for clinical practice in dermatology. Dermatology. 2007;214:46–51.
Goodman GJ, Baron JA. Postacne scarring: a qualitative global scarring grading system. Dermatol Surg. 2006;32:1458–66.
Tan JK, Tang J, Fung K, et al. Development and validation of a scale for acne scar severity (SCAR-S) of the face and trunk. J Cutan Med Surg. 2010;14:156–60.
Gupta MA, Johnson AM, Gupta AK. The development of an Acne Quality of Life scale: reliability, validity, and relation to subjective acne severity in mild to moderate acne vulgaris. Acta Derm Venereol. 1998;78:451–6.
Martin AR, Lookingbill DP, Botek A, et al. Health-related quality of life among patients with facial acne: assessment of a new acne-specific questionnaire. Clin Exp Dermatol. 2001;26:380–5.
Tan JKL, Jones E, Allen E, et al. Evaluation of essential clinical components and features of current acne global grading scales. J Am Acad Dermatol. 2013;69:754–61.
Barratt H, Hamilton F, Car J, et al. Outcome measures in acne vulgaris: systematic review. Br J Dermatol. 2009;160:132–6.
Doshi A, Zaheer A, Stiller MJ. A comparison of current acne grading systems and proposal of a novel system. Int J Dermatol. 1997;36:416–8.
Bernardis E, Shou H, Barbieri JS, et al. Development and initial validation of a multidimensional acne global grading system integrating primary lesions and secondary changes. JAMA Dermatol. 2020;156:296–302.
Auffret N, Nguyen JM, Leccia MT, et al. TRASS: a global approach to assess the severity of truncal acne. J Eur Acad Dermatol Venereol. 2022;2:2.
Burke BM, Cunliffe WJ. The assessment of acne vulgaris: the Leeds technique. Br J Dermatol. 1984;111:83–92.
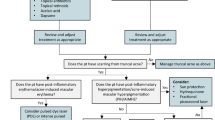
Tan J, Alexis A, Baldwin H, et al. Gaps and recommendations for clinical management of truncal acne from the Personalising Acne: Consensus of Experts Panel. JAAD Int. 2021;5:33–40.
Poli F, Auffret N, Leccia MT, et al. Truncal acne, what do we know? J Eur Acad Dermatol Venereol. 2020;34:2241–6.
Kircik L. Efficacy and safety of tazarotene lotion, 0.045% in the treatment of truncal acne vulgaris. J Drugs Dermatol. 2021;21:713–6.
Hoffman LK, Del Rosso JQ, Kircik LH. The efficacy and safety of azelaic acid 15% foam in the treatment of truncal acne vulgaris. J Drugs Dermatol. 2017;16:534–8.
Del Rosso JQ, Kircik L, Tanghetti E. Management of truncal acne vulgaris with topical dapsone 7.5% gel. J Clin Aesthet Dermatol. 2018;11:45–50.
Leyden JJ, Wortzman M, Baldwin EK. Antibiotic-resistant Propionibacterium acnes suppressed by a benzoyl peroxide cleanser 6%. Cutis. 2008;82:417–21.
Leyden JJ, Preston N, Osborn C, et al. In-vivo effectiveness of adapalene 0.1%/benzoyl peroxide 2.5% gel on antibiotic-sensitive and resistant Propionibacterium acnes. J Clin Aesthet Dermatol. 2011;4:22–6.
Gollnick H, Cunliffe W, Berson D, et al. Management of acne: a report from a global alliance to improve outcomes in acne. J Am Acad Dermatol. 2003;49:1–37.
Bikowski J. A review of the safety and efficacy of benzoyl peroxide (5.3%) emollient foam in the management of truncal acne vulgaris. J Clin Aesthet Dermatol. 2010;3:26–9.
Leyden JJ. Efficacy of benzoyl peroxide (5.3%) emollient foam and benzoyl peroxide (8%) wash in reducing Propionibacterium acnes on the back. J Drugs Dermatol. 2010;9:622–5.
Leyden JJ, Del Rosso JQ. The effect of benzoyl peroxide 9.8% emollient foam on reduction of Propionibacterium acnes on the back using a short contact therapy approach. J Drugs Dermatol. 2012;11:830–3.
Tanghetti E, Abramovits W, Solomon B, et al. Tazarotene versus tazarotene plus clindamycin/benzoyl peroxide in the treatment of acne vulgaris: a multicenter, double-blind, randomized parallel-group trial. J Drugs Dermatol. 2006;5:256–61.
Keating GM. Adapalene 0.1%/benzoyl peroxide 2.5% gel: a review of its use in the treatment of acne vulgaris in patients aged >/= 12 years. Am J Clin Dermatol. 2011;12:407–20.
Zouboulis CC, Fischer TC, Wohlrab J, et al. Study of the efficacy, tolerability, and safety of 2 fixed-dose combination gels in the management of acne vulgaris. Cutis. 2009;84:223–9.
Yang Z, Zhang Y, Lazic Mosler E, et al. Topical benzoyl peroxide for acne. Cochrane Database Syst Rev. 2020;3:11154.
Toyoda M, Morohashi M. An overview of topical antibiotics for acne treatment. Dermatology. 1998;6:130–4.
Mills O Jr, Thornsberry C, Cardin CW, et al. Bacterial resistance and therapeutic outcome following three months of topical acne therapy with 2% erythromycin gel versus its vehicle. Acta Derm Venereol. 2002;82:260–5.
Webster G, Rich P, Gold MH, et al. Efficacy and tolerability of a fixed combination of clindamycin phosphate (1.2%) and low concentration benzoyl peroxide (2.5%) aqueous gel in moderate or severe acne subpopulations. J Drugs Dermatol. 2009;8:736–43.
Thiboutot D, Zaenglein A, Weiss J, et al. An aqueous gel fixed combination of clindamycin phosphate 1.2% and benzoyl peroxide 2.5% for the once-daily treatment of moderate to severe acne vulgaris: assessment of efficacy and safety in 2813 patients. J Am Acad Dermatol. 2008;59:792–800.
Lookingbill DP, Chalker DK, Lindholm JS, et al. Treatment of acne with a combination clindamycin/benzoyl peroxide gel compared with clindamycin gel, benzoyl peroxide gel and vehicle gel: combined results of two double-blind investigations. J Am Acad Dermatol. 1997;37:590–5.
Tschen EH, Katz HI, Jones TM, et al. A combination benzoyl peroxide and clindamycin topical gel compared with benzoyl peroxide, clindamycin phosphate, and vehicle in the treatment of acne vulgaris. Cutis. 2001;67:165–9.
Leyden JJ, Hickman JG, Jarratt MT, et al. The efficacy and safety of a combination benzoyl peroxide/clindamycin topical gel compared with benzoyl peroxide alone and a benzoyl peroxide/erythromycin combination product. J Cutan Med Surg. 2001;5:37–42.
Pariser DM, Rich P, Cook-Bolden FE, et al. An aqueous gel fixed combination of clindamycin phosphate 1.2% and benzoyl peroxide 3.75% for the once-daily treatment of moderate to severe acne vulgaris. J Drugs Dermatol. 2014;13:1083–9.
F.P. Ltd. Foamix receives FDA approval of Amzeeq™ topical minocycline treatment for millions of moderate to severe acne sufferers, PR Newswire, 2019.
Martins AM, Marto JM, Johnson JL, et al. A review of systemic minocycline side effects and topical minocycline as a safer alternative for treating acne and rosacea. Antibiotics (Basel). 2021;10:2.
Gold LS, Dhawan S, Weiss J, et al. A novel topical minocycline foam for the treatment of moderate-to-severe acne vulgaris: Results of 2 randomized, double-blind, phase 3 studies. J Am Acad Dermatol. 2019;80:168–77.
Kolli SS, Pecone D, Pona A, et al. Topical retinoids in acne vulgaris: a systematic review. Am J Clin Dermatol. 2019;20:345–65.
Leyden J, Stein-Gold L, Weiss J. Why topical retinoids are mainstay of therapy for acne. Dermatol Ther (Heidelb). 2017;7:293–304.
Blume-Peytavi U, Fowler J, Kemeny L, et al. Long-term safety and efficacy of trifarotene 50 mug/g cream, a first-in-class RAR-gamma selective topical retinoid, in patients with moderate facial and truncal acne. J Eur Acad Dermatol Venereol. 2020;34:166–73.
Richter JR, Forstrom LR, Kiistala UO, et al. Efficacy of the fixed 1.2% clindamycin phosphate, 0.025% tretinoin gel formulation (Velac) and a proprietary 0.025% tretinoin gel formulation (Aberela) in the topical control of facial acne. J Eur Acad Dermatol Venereol. 1998;11:227–33.
Zouboulis CC, Derumeaux L, Decroix J, et al. A multicentre, single-blind, randomized comparison of a fixed clindamycin phosphate/tretinoin gel formulation (Velac) applied once daily and a clindamycin lotion formulation (Dalacin T) applied twice daily in the topical treatment of acne vulgaris. Br J Dermatol. 2000;143:498–505.
Dreno B, Bettoli V, Ochsendorf F, et al. Efficacy and safety of clindamycin phosphate 1.2%/tretinoin 0.025% formulation for the treatment of acne vulgaris: pooled analysis of data from three randomised, double-blind, parallel-group, phase III studies. Eur J Dermatol. 2014;24:201–9.
Dhillon S. Clascoterone: first approval. Drugs. 2020;80:1745–50.
Hebert A, Thiboutot D, Stein Gold L, et al. Efficacy and safety of topical clascoterone cream, 1%, for treatment in patients with facial acne: two phase 3 randomized clinical trials. JAMA Dermatol. 2020;156:621–30.
Ferraboschi P, Legnani L, Celasco G, et al. A full conformational characterization of antiandrogen cortexolone-17 alpha-propionate and related compounds through theoretical calculations and nuclear magnetic resonance spectroscopy. Medchemcomm. 2014;5:904–14.
Mazzetti A, Moro L, Gerloni M, et al. Pharmacokinetic profile, safety, and tolerability of clascoterone (cortexolone 17-alpha propionate, CB-03-01) topical cream, 1% in subjects with acne vulgaris: an open-label phase 2a study. J Drugs Dermatol. 2019;18:563.
Marks DH, Mansh MD. Potential role for topical antiandrogens in the management of acne among patients receiving masculinizing hormone therapy. JAMA Dermatol. 2020;156:1380–1.
Eichenfield L, Hebert A, Gold LS, et al. Open-label, long-term extension study to evaluate the safety of clascoterone (CB-03-01) cream, 1% twice daily, in patients with acne vulgaris. J Am Acad Dermatol. 2020;83:477–85.
Kainz JT, Berghammer G, Auer-Grumbach P, et al. Azelaic acid 20 % cream: effects on quality of life and disease severity in adult female acne patients. J Dtsch Dermatol Ges. 2016;14:1249–59.
Eastman WJ, Malahias S, Delconte J, et al. Assessing attributes of topical vehicles for the treatment of acne, atopic dermatitis, and plaque psoriasis. Cutis. 2014;94:46–53.
Tan HH. Antibacterial therapy for acne: a guide to selection and use of systemic agents. Am J Clin Dermatol. 2003;4:307–14.
Webster GF, McGinley KJ, Leyden JJ. Inhibition of lipase production in Propionibacterium acnes by sub-minimal-inhibitory concentrations of tetracycline and erythromycin. Br J Dermatol. 1981;104:453–7.
Armstrong AW, Hekmatjah J, Kircik LH. Oral tetracyclines and acne: a systematic review for dermatologists. J Drugs Dermatol. 2020;19:s6-13.
Leyden JJ, Bruce S, Lee CS, et al. A randomized, phase 2, dose-ranging study in the treatment of moderate to severe inflammatory facial acne vulgaris with doxycycline calcium. J Drugs Dermatol. 2013;12:658–63.
Patel M, Bowe WP, Heughebaert C, et al. The development of antimicrobial resistance due to the antibiotic treatment of acne vulgaris: a review. J Drugs Dermatol. 2010;9:655–64.
Del Rosso JQ, Webster GF, Rosen T, et al. Status report from the Scientific Panel on Antibiotic Use in Dermatology of the American Acne and Rosacea Society: part 1: antibiotic prescribing patterns, sources of antibiotic exposure, antibiotic consumption and emergence of antibiotic resistance, impact of alterations in antibiotic prescribing, and clinical sequelae of antibiotic use. J Clin Aesthet Dermatol. 2016;9:18–24.
Thompson KG, Rainer BM, Antonescu C, et al. Minocycline and its impact on microbial dysbiosis in the skin and gastrointestinal tract of acne patients. Ann Dermatol. 2020;32:21–30.
Francino MP. Antibiotics and the human gut microbiome: dysbioses and accumulation of resistances. Front Microbiol. 2015;6:1543.
Margolis DJ, Fanelli M, Hoffstad O, et al. Potential association between the oral tetracycline class of antimicrobials used to treat acne and inflammatory bowel disease. Am J Gastroenterol. 2010;105:2610–6.
Farrah G, Tan E. The use of oral antibiotics in treating acne vulgaris: a new approach. Dermatol Ther. 2016;29:377–84.
US Food and Drug Administration. Seysara® (sarecycline) tablets for oral use (package insert). Approved prescribing information. Almirall LLC.
Deeks ED. Sarecycline: first global approval. Drugs. 2019;79:325–9.
Batool Z, Lomakin IB, Polikanov YS, et al. Sarecycline interferes with tRNA accommodation and tethers mRNA to the 70S ribosome. Proc Natl Acad Sci U S A. 2020;117:20530–7.
Bunick CG, Keri J, Tanaka SK, et al. Antibacterial mechanisms and efficacy of sarecycline in animal models of infection and inflammation. Antibiotics (Basel). 2021;10:2.
Zhanel G, Critchley I, Lin LY, et al. Microbiological profile of sarecycline, a novel targeted spectrum tetracycline for the treatment of acne vulgaris. Antimicrob Agents Chemother. 2019;63:2.
Grada A, Bunick CG. Spectrum of antibiotic activity and its relevance to the microbiome. JAMA Netw Open. 2021;4: e215357.
Moore A, Green LJ, Bruce S, et al. Once-daily oral sarecycline 1.5 mg/kg/day is effective for moderate to severe acne vulgaris: results from two identically designed, phase 3, randomized, double-blind clinical trials. J Drugs Dermatol. 2018;17:987–96.
Del Rosso JQ, Stein Gold L, Baldwin H, et al. Management of truncal acne with oral sarecycline: pooled results from two phase-3 clinical trials. J Drugs Dermatol. 2021;20:634–40.
Nelson AM, Gilliland KL, Cong Z, et al. 13-cis Retinoic acid induces apoptosis and cell cycle arrest in human SEB-1 sebocytes. J Invest Dermatol. 2006;126:2178–89.
Webster GF, Leyden JJ, Gross JA. Results of a phase III, double-blind, randomized, parallel-group, non-inferiority study evaluating the safety and efficacy of Isotretinoin-Lidose in patients with severe recalcitrant nodular acne. J Drugs Dermatol. 2014;13:665–70.
Peck GL, Olsen TG, Yoder FW, et al. Prolonged remissions of cystic and conglobate acne with 13-cis-retinoic acid. N Engl J Med. 1979;300:329–33.
Layton A. The use of isotretinoin in acne. Dermatoendocrinol. 2009;1:162–9.
Rubinow DR, Peck GL, Squillace KM, et al. Reduced anxiety and depression in cystic acne patients after successful treatment with oral isotretinoin. J Am Acad Dermatol. 1987;17:25–32.
Marron SE, Tomas-Aragones L, Boira S. Anxiety, depression, quality of life and patient satisfaction in acne patients treated with oral isotretinoin. Acta Derm Venereol. 2013;93:701–6.
Layton AM, Knaggs H, Taylor J, et al. Isotretinoin for acne vulgaris: 10 years later: a safe and successful treatment. Br J Dermatol. 1993;129:292–6.
Goldsmith LA, Bolognia JL, Callen JP, et al. American Academy of Dermatology Consensus Conference on the safe and optimal use of isotretinoin: summary and recommendations. J Am Acad Dermatol. 2004;50:900–6.
Borghi A, Mantovani L, Minghetti S, et al. Low-cumulative dose isotretinoin treatment in mild-to-moderate acne: efficacy in achieving stable remission. J Eur Acad Dermatol Venereol. 2011;25:1094–8.
Amichai B, Shemer A, Grunwald MH. Low-dose isotretinoin in the treatment of acne vulgaris. J Am Acad Dermatol. 2006;54:644–6.
Strauss JS, Rapini RP, Shalita AR, et al. Isotretinoin therapy for acne: results of a multicenter dose-response study. J Am Acad Dermatol. 1984;10:490–6.
Blasiak RC, Stamey CR, Burkhart CN, et al. High-dose isotretinoin treatment and the rate of retrial, relapse, and adverse effects in patients with acne vulgaris. JAMA Dermatol. 2013;49:1392–8.
Cyrulnik AA, Viola KV, Gewirtzman AJ, et al. High-dose isotretinoin in acne vulgaris: improved treatment outcomes and quality of life. Int J Dermatol. 2012;51:1123–30.
Rademaker M. Isotretinoin: dose, duration and relapse. What does 30 years of usage tell us? Australas J Dermatol. 2013;54:157–62.
Zouboulis CC. The truth behind this undeniable efficacy: recurrence rates and relapse risk factors of acne treatment with oral isotretinoin. Dermatology. 2006;212:99–100.
Quereux G, Volteau C, N’Guyen JM, et al. Prospective study of risk factors of relapse after treatment of acne with oral isotretinoin. Dermatology. 2006;212:168–76.
Cunliffe WJ, Norris JF. Isotretinoin: an explanation for its long-term benefit. Dermatologica. 1987;175(Suppl. 1):133–7.
Rademaker M. Adverse effects of isotretinoin: a retrospective review of 1743 patients started on isotretinoin. Australas J Dermatol. 2010;51:248–53.
Ellis CN, Krach KJ. Uses and complications of isotretinoin therapy. J Am Acad Dermatol. 2001;45:S150–7.
Marqueling AL, Zane LT. Depression and suicidal behavior in acne patients treated with isotretinoin: a systematic review. Semin Cutan Med Surg. 2007;26:210–20.
Chia CY, Lane W, Chibnall J, et al. Isotretinoin therapy and mood changes in adolescents with moderate to severe acne: a cohort study. Arch Dermatol. 2005;141:557–60.
Rashtak S, Khaleghi S, Pittelkow MR, et al. Isotretinoin exposure and risk of inflammatory bowel disease. JAMA Dermatol. 2014;150:1322–6.
Paljarvi T, McPherson T, Luciano S, et al. Isotretinoin and adverse neuropsychiatric outcomes: retrospective cohort study using routine data. Br J Dermatol. 2022;187:64–72.
Dai WS, LaBraico JM, Stern RS. Epidemiology of isotretinoin exposure during pregnancy. J Am Acad Dermatol. 1992;26:599–606.
Collins MK, Moreau JF, Opel D, et al. Compliance with pregnancy prevention measures during isotretinoin therapy. J Am Acad Dermatol. 2014;70:55–9.
Thorneycroft IH, Stanczyk FZ, Bradshaw KD, et al. Effect of low-dose oral contraceptives on androgenic markers and acne. Contraception. 1999;60:255–62.
Panzer C, Wise S, Fantini G, et al. Impact of oral contraceptives on sex hormone-binding globulin and androgen levels: a retrospective study in women with sexual dysfunction. J Sex Med. 2006;3:104–13.
Koo EB, Petersen TD, Kimball AB. Meta-analysis comparing efficacy of antibiotics versus oral contraceptives in acne vulgaris. J Am Acad Dermatol. 2014;71:450–9.
Palli MB, Reyes-Habito CM, Lima XT, et al. A single-center, randomized double-blind, parallel-group study to examine the safety and efficacy of 3mg drospirenone/0.02 mg ethinyl estradiol compared with placebo in the treatment of moderate truncal acne vulgaris. J Drugs Dermatol. 2013;2:633–7.
Lidegaard O, Lokkegaard E, Svendsen AL, et al. Hormonal contraception and risk of venous thromboembolism: national follow-up study. BMJ. 2009;339: b2890.
Jick SS, Hernandez RK. Risk of non-fatal venous thromboembolism in women using oral contraceptives containing drospirenone compared with women using oral contraceptives containing levonorgestrel: case-control study using United States claims data. BMJ. 2011;342: d2151.
Gronich N, Lavi I, Rennert G. Higher risk of venous thrombosis associated with drospirenone-containing oral contraceptives: a population-based cohort study. CMAJ. 2011;183:E1319–25.
Katsambas AD, Dessinioti C. Hormonal therapy for acne: why not as first line therapy? Facts and controversies Clin Dermatol. 2010;28:17–23.
van Vlijmen EF, Veeger NJ, Middeldorp S, et al. Thrombotic risk during oral contraceptive use and pregnancy in women with factor V Leiden or prothrombin mutation: a rational approach to contraception. Blood. 2011;118:2055–61; quiz 2375.
Svoboda RM, Nawaz N, Zaenglein AL. Hormonal treatment of acne and hidradenitis suppurativa in adolescent patients. Dermatol Clin. 2022;40:167–78.
Gierisch JM, Coeytaux RR, Urrutia RP, et al. Oral contraceptive use and risk of breast, cervical, colorectal, and endometrial cancers: a systematic review. Cancer Epidemiol Biomarkers Prev. 2013;22:1931–43.
Krunic A, Ciurea A, Scheman A. Efficacy and tolerance of acne treatment using both spironolactone and a combined contraceptive containing drospirenone. J Am Acad Dermatol. 2008;58:60–2.
Menard RH, Stripp B, Gillette JR. Spironolactone and testicular cytochrome P-450: decreased testosterone formation in several species and changes in hepatic drug metabolism. Endocrinology. 1974;94:1628–36.
Boisselle A, Dionne FT, Tremblay RR. Interaction of spironolactone with rat skin androgen receptor. Can J Biochem. 1979;57:1042–6.
Layton AM, Eady EA, Whitehouse H, et al. Oral spironolactone for acne vulgaris in adult females: a hybrid systematic review. Am J Clin Dermatol. 2017;18:169–91.
Isvy-Joubert A, Nguyen JM, Gaultier A, et al. Adult female acne treated with spironolactone: a retrospective data review of 70 cases. Eur J Dermatol. 2017;27:393–8.
Charny JW, Choi JK, James WD. Spironolactone for the treatment of acne in women, a retrospective study of 110 patients. Int J Womens Dermatol. 2017;3:111–5.
Shaw JC, White LE. Long-term safety of spironolactone in acne: results of an 8-year followup study. J Cutan Med Surg. 2002;6:541–5.
Elsaie ML. Hormonal treatment of acne vulgaris: an update. Clin Cosmet Investig Dermatol. 2016;9:241–8.
Thiede RM, Rastogi S, Nardone B, et al. Hyperkalemia in women with acne exposed to oral spironolactone: a retrospective study from the RADAR (Research on Adverse Drug Events and Reports) program. Int J Womens Dermatol. 2019;5:155–7.
Plovanich M, Weng QY, Mostaghimi A. Low usefulness of potassium monitoring among healthy young women taking spironolactone for acne. JAMA Dermatol. 2015;151:941–4.
Layton AM, Henderson CA, Cunliffe WJ. A clinical evaluation of acne scarring and its incidence. Clin Exp Dermatol. 1994;19:303–8.
Holland DB, Jeremy AH, Roberts SG, et al. Inflammation in acne scarring: a comparison of the responses in lesions from patients prone and not prone to scar. Br J Dermatol. 2004;150:72–81.
Goodman GJ. Postacne scarring: a review of its pathophysiology and treatment. Dermatol Surg. 2000;26:857–71.
Layton A, Alexis A, Baldwin H, et al. Identifying gaps and providing recommendations to address shortcomings in the investigation of acne sequelae by the Personalising Acne: Consensus of Experts panel. JAAD Int. 2021;5:41–8.
Connolly D, Vu HL, Mariwalla K, et al. Acne scarring: pathogenesis, evaluation, and treatment options. J Clin Aesthet Dermatol. 2017;10:12–23.
Jacob CI, Dover JS, Kaminer MS. Acne scarring: a classification system and review of treatment options. J Am Acad Dermatol. 2001;45:109–17.
Jemec GB, Jemec B. Acne: treatment of scars. Clin Dermatol. 2004;22:434–8.
Saha AK, Mukhopadhyay M. A comparative clinical study on role of 5-flurouracil versus triamcinolone in the treatment of keloids. Indian J Surg. 2012;74:326–9.
Forbat E, Al-Niaimi F. Nonvascular uses of pulsed dye laser in clinical dermatology. J Cosmet Dermatol. 2019.
Yoon HJ, Lee DH, Kim SO, et al. Acne erythema improvement by long-pulsed 595-nm pulsed-dye laser treatment: a pilot study. J Dermatolog Treat. 2008;19:38–44.
Patel N, Clement M. Selective nonablative treatment of acne scarring with 585 nm flashlamp pulsed dye laser. Dermatol Surg. 2002;28:942–5.
Lee DH, Choi YS, Min SU, et al. Comparison of a 585-nm pulsed dye laser and a 1064-nm Nd:YAG laser for the treatment of acne scars: a randomized split-face clinical study. J Am Acad Dermatol. 2009;60:801–7.
Alster TS. Improvement of erythematous and hypertrophic scars by the 585-nm flashlamp-pumped pulsed dye laser. Ann Plast Surg. 1994;32:186–90.
Khatri KA, Mahoney DL, McCartney MJ. Laser scar revision: a review. J Cosmet Laser Ther. 2011;13:54–62.
Vrijman C, van Drooge AM, Limpens J, et al. Laser and intense pulsed light therapy for the treatment of hypertrophic scars: a systematic review. Br J Dermatol. 2011;165:934–42.
Kono T, Ercocen AR, Nakazawa H, et al. The flashlamp-pumped pulsed dye laser (585 nm) treatment of hypertrophic scars in Asians. Ann Plast Surg. 2003;51:366–71.
Rao J. Treatment of acne scarring. Facial Plast Surg Clin North Am. 2011;19:275–91.
Faghihi G, Isfahani AK, Hosseini SM, et al. Efficacy of intense pulsed light combined with topical erythromycin solution 2% versus topical erythromycin solution 2% alone in the treatment of persistent facial erythematous acne macules. Adv Biomed Res. 2012;1:70.
Feng H, Wu Y, Jiang M, et al. The efficacy and safety of fractional 1064 nm Nd:YAG picosecond laser combined with intense pulsed light in the treatment of atrophic acne scar: a split-face study. Lasers Surg Med. 2021;3:1356–63.
Wang B, Wu Y, Luo YJ, et al. Combination of intense pulsed light and fractional CO(2) laser treatments for patients with acne with inflammatory and scarring lesions. Clin Exp Dermatol. 2013;38:344–51.
Erol OO, Gurlek A, Agaoglu G, et al. Treatment of hypertrophic scars and keloids using intense pulsed light (IPL). Aesthetic Plast Surg. 2008;32:902–9.
Piccolo D, Kostaki D, Dianzani C, et al. Effective intense pulsed light protocol in the treatment of moderate to severe acne vulgaris of the chest and back. J Clin Aesthet Dermatol. 2022;15:22–5.
Salameh F, Shumaker PR, Goodman GJ, et al. Energy-based devices for the treatment of acne scars: 2022 international consensus recommendations. Lasers Surg Med. 2022;54:10–26.
Cohen BE, Brauer JA, Geronemus RG. Acne scarring: a review of available therapeutic lasers. Lasers Surg Med. 2016;48:95–115.
Chapas AM, Brightman L, Sukal S, et al. Successful treatment of acneiform scarring with CO2 ablative fractional resurfacing. Lasers Surg Med. 2008;40:381–6.
Chan NP, Ho SG, Yeung CK, et al. Fractional ablative carbon dioxide laser resurfacing for skin rejuvenation and acne scars in Asians. Lasers Surg Med. 2010;42:615–23.
Hu S, Hsiao WC, Chen MC, et al. Ablative fractional erbium-doped yttrium aluminum garnet laser with coagulation mode for the treatment of atrophic acne scars in Asian skin. Dermatol Surg. 2011;37:939–44.
Kim S, Cho KH. Clinical trial of dual treatment with an ablative fractional laser and a nonablative laser for the treatment of acne scars in Asian patients. Dermatol Surg. 2009;35:1089–98.
Cameli N, Mariano M, Serio M, et al. Preliminary comparison of fractional laser with fractional laser plus radiofrequency for the treatment of acne scars and photoaging. Dermatol Surg. 2014;40:553–61.
Faghihi G, Keyvan S, Asilian A, et al. Efficacy of autologous platelet-rich plasma combined with fractional ablative carbon dioxide resurfacing laser in treatment of facial atrophic acne scars: a split-face randomized clinical trial. Indian J Dermatol Venereol Leprol. 2016;82:162–8.
Gawdat HI, Hegazy RA, Fawzy MM, et al. Autologous platelet rich plasma: topical versus intradermal after fractional ablative carbon dioxide laser treatment of atrophic acne scars. Dermatol Surg. 2014;40:152–61.
Lee JW, Kim BJ, Kim MN, et al. The efficacy of autologous platelet rich plasma combined with ablative carbon dioxide fractional resurfacing for acne scars: a simultaneous split-face trial. Dermatol Surg. 2011;37:931–8.
Preissig J, Hamilton K, Markus R. Current laser resurfacing technologies: a review that delves beneath the surface. Semin Plast Surg. 2012;26:109–16.
Elsaie ML, Ibrahim SM, Saudi W. Ablative fractional 10 600 nm carbon dioxide laser versus non-ablative fractional 1540 nm erbium-glass laser in Egyptian post-acne scar patients. J Lasers Med Sci. 2018;9:32–5.
Cheng X, Yang Q, Su Y, et al. Comparison of 1565-nm nonablative fractional laser and 10600-nm ablative fractional laser in the treatment of mild to moderate atrophic acne scars. Dermatol Surg. 2021;47:392–6.
Sardana K, Manjhi M, Garg VK, et al. Which type of atrophic acne scar (ice-pick, boxcar, or rolling) responds to nonablative fractional laser therapy? Dermatol Surg. 2014;40:288–300.
Chan NP, Ho SG, Yeung CK, et al. The use of non-ablative fractional resurfacing in Asian acne scar patients. Lasers Surg Med. 2010;42:710–5.
Alexis AF, Coley MK, Nijhawan RI, et al. Nonablative fractional laser resurfacing for acne scarring in patients with Fitzpatrick skin phototypes IV-VI. Dermatol Surg. 2016;42:392–402.
Torbeck RL, Schilling L, Khorasani H, et al. Evolution of the picosecond laser: a review of literature. Dermatol Surg. 2019;45:183–94.
Lee CH, Jin EM, Seo HS, et al. Efficacy and safety of treatment with fractional 1,064-nm picosecond laser with diffractive optic element for wrinkles and acne scars: a clinical study. Ann Dermatol. 2021;33:254–62.
Choi ME, Paik SH, Lee WJ, et al. Treatment of acne scars with a fractional 1064-nm Nd:YAG picosecond laser and histopathologic findings. Dermatol Ther. 2020;33: e13297.
Chayavichitsilp P, Limtong P, Triyangkulsri K, et al. Comparison of fractional neodymium-doped yttrium aluminum garnet (Nd:YAG) 1064-nm picosecond laser and fractional 1550-nm erbium fiber laser in facial acne scar treatment. Lasers Med Sci. 2020;35:695–700.
Sirithanabadeekul P, Tantrapornpong P, Rattakul B, et al. Comparison of fractional picosecond 1064-nm laser and fractional carbon dioxide laser for treating atrophic acne scars: a randomized split-face trial. Dermatol Surg. 2021;47:e58-65.
Brauer JA, Kazlouskaya V, Alabdulrazzaq H, et al. Use of a picosecond pulse duration laser with specialized optic for treatment of facial acne scarring. JAMA Dermatol. 2015;151:278–84.
Boen M, Jacob C. A review and update of treatment options using the Acne Scar Classification System. Dermatol Surg. 2019;45:411–22.
Nitayavardhana S, Wanitphakdeedecha R, Ng JNC, et al. The efficacy and safety of fractional radiofrequency nanoneedle system in the treatment of atrophic acne scars in Asians. J Cosmet Dermatol. 2020;19:1636–41.
Goel A, Gatne V. Use of nanofractional radiofrequency for the treatment of acne scars in Indian skin. J Cosmet Dermatol. 2017;16:186–92.
Simmons BJ, Griffith RD, Falto-Aizpurua LA, et al. Use of radiofrequency in cosmetic dermatology: focus on nonablative treatment of acne scars. Clin Cosmet Investig Dermatol. 2014;7:335–9.
Min S, Park SY, Yoon JY, et al. Comparison of fractional microneedling radiofrequency and bipolar radiofrequency on acne and acne scar and investigation of mechanism: comparative randomized controlled clinical trial. Arch Dermatol Res. 2015;307:897–904.
Katz BE. The fate of active acne and acne scars following treatment with fractional radiofrequency. J Drugs Dermatol. 2019;18:1268–72.
Kacar N, Dursun R, Akbay M, et al. The early and late efficacy of single-pass fractional carbondioxide laser, fractional radiofrequency, and their combination in acne scars: a prospective, split-face, single-blinded, controlled clinical study. Dermatol Ther. 2020;33: e14444.
Tatliparmak A, Aksoy B, Shishehgarkhaneh LR, et al. Use of combined fractional carbon dioxide laser and fractional microneedle radiofrequency for the treatment of acne scars: a retrospective analysis of 1-month treatment outcome on scar severity and patient satisfaction. J Cosmet Dermatol. 2020;19:115–21.
Kim J, Lee YI, Kim J, et al. Safety of combined fractional microneedle radiofrequency and CO2 as an early intervention for inflammatory acne and scarring treated with concomitant isotretinoin. Dermatol Surg. 2020;46:e71–7.
Minh PPT, Bich DD, Hai VNT, et al. Microneedling therapy for atrophic acne scar: effectiveness and safety in Vietnamese patients. Open Access Maced J Med Sci. 2019;7:293–7.
El-Domyati M, Barakat M, Awad S, et al. Microneedling therapy for atrophic acne scars: an objective evaluation. J Clin Aesthet Dermatol. 2015;8:36–42.
Dogra S, Yadav S, Sarangal R. Microneedling for acne scars in Asian skin type: an effective low cost treatment modality. J Cosmet Dermatol. 2014;13:180–7.
Cachafeiro T, Escobar G, Maldonado G, et al. Comparison of nonablative fractional erbium laser 1,340 nm and microneedling for the treatment of atrophic acne scars: a randomized clinical trial. Dermatol Surg. 2016;42:232–41.
Asif M, Kanodia S, Singh K. Combined autologous platelet-rich plasma with microneedling verses microneedling with distilled water in the treatment of atrophic acne scars: a concurrent split-face study. J Cosmet Dermatol. 2016;15:434–43.
Ibrahim MK, Ibrahim SM, Salem AM. Skin microneedling plus platelet-rich plasma versus skin microneedling alone in the treatment of atrophic post acne scars: a split face comparative study. J Dermatolog Treat. 2018;29:281–6.
Schoenberg E, O’Connor M, Wang JV, et al. Microneedling and PRP for acne scars: a new tool in our arsenal. J Cosmet Dermatol. 2020;19:112–4.
Rana S, Mendiratta V, Chander R. Efficacy of microneedling with 70% glycolic acid peel vs microneedling alone in treatment of atrophic acne scars: a randomized controlled trial. J Cosmet Dermatol. 2017;16:454–9.
Sharad J. Combination of microneedling and glycolic acid peels for the treatment of acne scars in dark skin. J Cosmet Dermatol. 2011;10:317–23.
Morelli Coppola M, Salzillo R, Segreto F, et al. Triamcinolone acetonide intralesional injection for the treatment of keloid scars: patient selection and perspectives. Clin Cosmet Investig Dermatol. 2018;11:387–96.
Khan MA, Bashir MM, Khan FA. Intralesional triamcinolone alone and in combination with 5-fluorouracil for the treatment of keloid and hypertrophic scars. J Pak Med Assoc. 2014;64:1003–7.
Waibel JS, Wulkan AJ, Shumaker PR. Treatment of hypertrophic scars using laser and laser assisted corticosteroid delivery. Lasers Surg Med. 2013;45:135–40.
Tawfik AA, Fathy M, Badawi A, et al. Topical 5 fluorouracil cream vs combined 5 fluorouracil and fractional erbium YAG laser for treatment of severe hypertrophic scars. Clin Cosmet Investig Dermatol. 2019;12:173–80.
Waibel JS, Wulkan AJ, Rudnick A, et al. Treatment of hypertrophic scars using laser-sssisted corticosteroid versus laser-assisted 5-fluorouracil delivery. Dermatol Surg. 2019;45:423–30.
Beer K. A single-center, open-label study on the use of injectable poly-L-lactic acid for the treatment of moderate to severe scarring from acne or varicella. Dermatol Surg. 2007;33(Suppl. 2):S159–67.
Rkein A, Ozog D, Waibel JS. Treatment of atrophic scars with fractionated CO2 laser facilitating delivery of topically applied poly-L-lactic acid. Dermatol Surg. 2014;40:624–31.
Epstein RE, Spencer JM. Correction of atrophic scars with artefill: an open-label pilot study. J Drugs Dermatol. 2010;9:1062–4.
Karnik J, Baumann L, Bruce S, et al. A double-blind, randomized, multicenter, controlled trial of suspended polymethylmethacrylate microspheres for the correction of atrophic facial acne scars. J Am Acad Dermatol. 2014;71:77–83.
Biesman BS, Cohen JL, DiBernardo BE, et al. Treatment of atrophic facial acne scars with microneedling followed by polymethylmethacrylate-collagen gel dermal filler. Dermatol Surg. 2019;45:1570–9.
Acknowledgments
We thank the Yale Department of Dermatology Resident Slide Collection for providing clinical images. We thank Drs. T. Orlowski, H.H. Reynolds, and L.V. Graham for providing clinical images of truncal demodicosis. This work was supported by the NIH/NIGMS Medical Scientist Training Grant T32GM136651 for SGD.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were received for the preparation of this article.
Conflicts of interest
SGD, SRK, AG, and KCS have no disclosures; AYM has received funds, honoraria, or research grants as an advisory board member (A), consultant (C), clinical study investigator (I), and/or speaker (SP) for Almirall, Biofronterra, and Galderma; CGB has served as an (I) for Almirall; a (C) for AbbVie, Almirall, Arcutis, EpiHealth, LEO Pharma, Sanofi-Regeneron, and UCB; and a (SP) for and received honoraria from Allergan, Almirall, LEO Pharma, and UCB. These engagements did not influence the writing of this manuscript.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
Authors’ Contributions
SGD, SRK, AG, AYM, KCS, and CGB researched and/or provided data for the article. SGD and SRK wrote the first draft of the article. All authors contributed substantially to discussion of the content and reviewed and/or edited the manuscript before submission.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Daniele, S.G., Kim, S.R., Grada, A. et al. Truncal Acne and Scarring: A Comprehensive Review of Current Medical and Cosmetic Approaches to Treatment and Patient Management. Am J Clin Dermatol 24, 199–223 (2023). https://doi.org/10.1007/s40257-022-00746-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-022-00746-4