Abstract
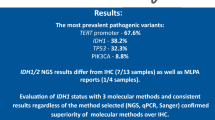
TP53 mutations are important molecular markers in diffuse astrocytic tumors and medulloblastomas. We examined the efficacy of a pre-screening method for high-resolution melting (HRM) analysis of TP53 mutation before direct sequencing using samples from patients with diffuse glioma. Surgical samples from 64 diffuse gliomas were classified based on the 2016 World Health Organization (WHO) histopathological grading system and the cIMPACT-NOW (consortium to inform molecular and practical approaches to CNS tumor taxonomy-not official WHO) update. TP53 mutations from exon 5 to exon 8 were assessed by direct sequencing. The results of HRM and p53 immunohistochemistry (IHC) analysis were compared by recording the sensitivity, specificity, and false negative and false positive rates. Direct sequencing detected TP53 mutations in 18 of 64 samples (28.1%): diffuse astrocytoma, IDH-mutant (n = 3); diffuse astrocytoma, IDH-wild type (n = 1); anaplastic astrocytoma, IDH-mutant (n = 3); anaplastic astrocytoma, IDH-wild type (n = 4); and glioblastoma, IDH-wild type (n = 7). A total of 22 mutations was detected in the 18 samples; 4 samples exhibited duplicate missense mutations. Sensitivity and specificity were 0.96 and 0.96, respectively, for HRM analysis; they were 0.89 and 0.52, respectively, for p53 IHC. Overall accuracy was 0.98 for HRM and 0.63 for IHC. HRM analysis is a good pre-screening method for the detection of TP53 mutation before direct sequencing.



Similar content being viewed by others
References
Komori T. The 2016 WHO classification of tumours of the central nervous system: the major points of revision. Neurol Med Chir Tokyo. 2017;57(7):301–11. https://doi.org/10.2176/nmc.ra.2017-0010.
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016;131(6):803–20. https://doi.org/10.1007/s00401-016-1545-1.
Von Deimling A, Perry A, Louis D, Ohgaki H, Wiestler O, Cavenee W. WHO classification of tumours of the central nervous system. Lyon: IARC; 2016.
Cambruzzi E. Medulloblastoma, WNT-activated/SHH-activated: clinical impact of molecular analysis and histogenetic evaluation. Childs Nerv Syst. 2018;34(5):809–15. https://doi.org/10.1007/s00381-018-3765-2.
Murnyak B, Hortobagyi T. Immunohistochemical correlates of TP53 somatic mutations in cancer. Oncotarget. 2016;7(40):64910–20. https://doi.org/10.18632/oncotarget.11912.
Bouaoun L, Sonkin D, Ardin M, Hollstein M, Byrnes G, Zavadil J, et al. TP53 variations in human cancers: new lessons from the IARC TP53 database and genomics data. Hum Mutat. 2016;37(9):865–76. https://doi.org/10.1002/humu.23035.
Salnikova LE. Clinicopathologic characteristics of brain tumors are associated with the presence and patterns of TP53 mutations: evidence from the IARC TP53 Database. Neuromol Med. 2014;16(2):431–47. https://doi.org/10.1007/s12017-014-8290-1.
Chan AK, Mao Y, Ng HK. TP53 and histone H3.3 mutations in triple-negative lower-grade gliomas. N Engl J Med. 2016;375(22):2206–8. https://doi.org/10.1056/nejmc1610144.
Nie E, Jin X, Wu W, Yu T, Zhou X, Zhi T, et al. BACH1 promotes temozolomide resistance in glioblastoma through antagonizing the function of p53. Sci Rep. 2016;6:39743. https://doi.org/10.1038/srep39743.
Ohgaki H, Dessen P, Jourde B, Horstmann S, Nishikawa T, Di Patre PL, et al. Genetic pathways to glioblastoma: a population-based study. Cancer Res. 2004;64(19):6892–9. https://doi.org/10.1158/0008-5472.CAN-04-1337.
Ohgaki H, Kleihues P. Genetic profile of astrocytic and oligodendroglial gliomas. Brain Tumor Pathol. 2011;28(3):177–83. https://doi.org/10.1007/s10014-011-0029-1.
Okamoto Y, Di Patre PL, Burkhard C, Horstmann S, Jourde B, Fahey M, et al. Population-based study on incidence, survival rates, and genetic alterations of low-grade diffuse astrocytomas and oligodendrogliomas. Acta Neuropathol. 2004;108(1):49–56. https://doi.org/10.1007/s00401-004-0861-z.
Sarma PP, Dutta D, Mirza Z, Saikia KK, Baishya BK. Point mutations in the DNA binding domain of p53 contribute to glioma progression and poor prognosis. Mol Biol Mosk. 2017;51(2):334–41. https://doi.org/10.7868/S0026898417020185.
Peraud A, Kreth FW, Wiestler OD, Kleihues P, Reulen HJ. Prognostic impact of TP53 mutations and P53 protein overexpression in supratentorial WHO grade II astrocytomas and oligoastrocytomas. Clin Cancer Res. 2002;8(5):1117–24.
Hermisson M, Klumpp A, Wick W, Wischhusen J, Nagel G, Roos W, et al. O6-methylguanine DNA methyltransferase and p53 status predict temozolomide sensitivity in human malignant glioma cells. J Neurochem. 2006;96(3):766–76. https://doi.org/10.1111/j.1471-4159.2005.03583.x.
Wang X, Chen JX, Liu JP, You C, Liu YH, Mao Q. Gain of function of mutant TP53 in glioblastoma: prognosis and response to temozolomide. Ann Surg Oncol. 2014;21(4):1337–44. https://doi.org/10.1245/s10434-013-3380-0.
Wang X, Chen JX, Liu YH, You C, Mao Q. Mutant TP53 enhances the resistance of glioblastoma cells to temozolomide by up-regulating O(6)-methylguanine DNA-methyltransferase. Neurol Sci. 2013;34(8):1421–8. https://doi.org/10.1007/s10072-012-1257-9.
Zhang C, Wang X, Hao S, Su Z, Zhang P, Li Y, et al. Analysis of treatment tolerance and factors associated with overall survival in elderly patients with glioblastoma. World Neurosurg. 2016;95:77–84. https://doi.org/10.1016/j.wneu.2016.07.079.
Newcomb EW, Madonia WJ, Pisharody S, Lang FF, Koslow M, Miller DC. A correlative study of p53 protein alteration and p53 gene mutation in glioblastoma multiforme. Brain Pathol. 1993;3(3):229–35.
Takami H, Yoshida A, Fukushima S, Arita H, Matsushita Y, Nakamura T, et al. Revisiting TP53 mutations and immunohistochemistry–a comparative study in 157 diffuse gliomas. Brain Pathol. 2015;25(3):256–65. https://doi.org/10.1111/bpa.12173.
Krypuy M, Ahmed AA, Etemadmoghadam D, Hyland SJ, Australian Ovarian Cancer Study G, DeFazio A, et al. High resolution melting for mutation scanning of TP53 exons 5-8. BMC Cancer. 2007;7:168. https://doi.org/10.1186/1471-2407-7-168.
Louis DN, Giannini C, Capper D, Paulus W, Figarella-Branger D, Lopes MB, et al. cIMPACT-NOW update 2: diagnostic clarifications for diffuse midline glioma, H3 K27M-mutant and diffuse astrocytoma/anaplastic astrocytoma, IDH-mutant. Acta Neuropathol. 2018;135(4):639–42. https://doi.org/10.1007/s00401-018-1826-y.
Louis DN, Wesseling P, Paulus W, Giannini C, Batchelor TT, Cairncross JG, et al. cIMPACT-NOW update 1: not otherwise specified (NOS) and not elsewhere classified (NEC). Acta Neuropathol. 2018;135(3):481–4. https://doi.org/10.1007/s00401-018-1808-0.
Hatae R, Hata N, Yoshimoto K, Kuga D, Akagi Y, Murata H, et al. Precise detection of IDH1/2 and BRAF hotspot mutations in clinical glioma tissues by a differential calculus analysis of high-resolution melting data. PLoS ONE. 2016;11(8):e0160489. https://doi.org/10.1371/journal.pone.0160489.
Gonzalez-Bosquet J, Calcei J, Wei JS, Garcia-Closas M, Sherman ME, Hewitt S, et al. Detection of somatic mutations by high-resolution DNA melting (HRM) analysis in multiple cancers. PLoS ONE. 2011;6(1):e14522. https://doi.org/10.1371/journal.pone.0014522.
Ihle MA, Fassunke J, Konig K, Grunewald I, Schlaak M, Kreuzberg N, et al. Comparison of high resolution melting analysis, pyrosequencing, next generation sequencing and immunohistochemistry to conventional Sanger sequencing for the detection of p.V600E and non-p.V600E BRAF mutations. BMC Cancer. 2014;14:13. https://doi.org/10.1186/1471-2407-14-13.
Yokogami K, Yamasaki K, Matsumoto F, Yamashita S, Saito K, Tacheva A, et al. Impact of PCR-based molecular analysis in daily diagnosis for the patient with gliomas. Brain Tumor Pathol. 2018. https://doi.org/10.1007/s10014-018-0322-3.
Baugh EH, Ke H, Levine AJ, Bonneau RA, Chan CS. Why are there hotspot mutations in the TP53 gene in human cancers? Cell Death Differ. 2018;25(1):154–60. https://doi.org/10.1038/cdd.2017.180.
Soussi T, Kato S, Levy PP, Ishioka C. Reassessment of the TP53 mutation database in human disease by data mining with a library of TP53 missense mutations. Hum Mutat. 2005;25(1):6–17. https://doi.org/10.1002/humu.20114.
Muller PA, Vousden KH. Mutant p53 in cancer: new functions and therapeutic opportunities. Cancer Cell. 2014;25(3):304–17. https://doi.org/10.1016/j.ccr.2014.01.021.
Kogan S, Carpizo DR. Zinc metallochaperones as mutant p53 reactivators: a new paradigm in cancer therapeutics. Cancers Basel. 2018. https://doi.org/10.3390/cancers10060166.
Zhao D, Tahaney WM, Mazumdar A, Savage MI, Brown PH. Molecularly targeted therapies for p53-mutant cancers. Cell Mol Life Sci. 2017;74(22):4171–87. https://doi.org/10.1007/s00018-017-2575-0.
Tindall EA, Petersen DC, Woodbridge P, Schipany K, Hayes VM. Assessing high-resolution melt curve analysis for accurate detection of gene variants in complex DNA fragments. Hum Mutat. 2009;30(6):876–83. https://doi.org/10.1002/humu.20919.
Davidson CJ, Zeringer E, Champion KJ, Gauthier M-P, Wang F, Boonyaratanakornkit J, et al. Improving the limit of detection for Sanger sequencing: a comparison of methodologies for KRAS variant detection. Biotechniques. 2012;53(3):182–8. https://doi.org/10.2144/000113913.
Sharma Y, Miladi M, Dukare S, Boulay K, Caudron-Herger M, Gross M, et al. A pan-cancer analysis of synonymous mutations. Nat Commun. 2019;10(1):2569. https://doi.org/10.1038/s41467-019-10489-2.
Duensing A, Duensing S. Guilt by association? p53 and the development of aneuploidy in cancer. Biochem Biophys Res Commun. 2005;331(3):694–700. https://doi.org/10.1016/j.bbrc.2005.03.157.
Acknowledgements
This research was supported by a Grant-in-Aid for Clinical Research from Miyazaki University Hospital. We especially thank Ms. Ayumi Nagatomo and Ms. Akemi Yoshida for technical assistance and Ms. Ursula Petralia for editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings reported in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Saito, K., Yokogami, K., Maekawa, K. et al. High-resolution melting effectively pre-screens for TP53 mutations before direct sequencing in patients with diffuse glioma. Human Cell 34, 644–653 (2021). https://doi.org/10.1007/s13577-020-00471-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13577-020-00471-2