Abstract
Background and Objective
There are some potential concerns about the currently marketed solid oral dosage forms of tramadol, including decreased adherence to immediate-release (IR) formulations due to the high number of doses taken each day and the slow rise in the blood tramadol concentration after administration of sustained-release (SR) formulations, which may not achieve a rapid analgesic effect. To overcome these potential concerns, a twice-daily double-layered tablet formulation of tramadol comprising IR and SR layers was developed. This article reports studies that assessed its physicochemical and pharmacokinetic properties.
Methods
Dissolution tests of five bilayer tablet formulations (designated tablets A–E) and pharmacokinetic studies of tablets A and B were conducted to investigate the appropriate ratio of the IR/SR layers in the double-layered tablet. Additionally, pharmacokinetic studies of three finished dosage formulations (tablets C–E) were performed in healthy adult males to investigate the effect of food intake on drug absorption.
Results
Adjusting the excipients and tramadol content in the IR and SR layers of tablets A–E altered their dissolution profiles in a manner that could be predicted based on their compositions. The IR layer was released within 15 min, and the SR layer was slowly released over 10 h. In the pharmacokinetic study, the time to maximum plasma concentration (tmax) of tramadol after administration of tablets A (IR:SR: 20:80 mg) and B (40:60 mg) was shorter than that of a commercially available SR tablet, and the half-life (t1/2) was longer than that of a commercially available IR tablet. For tablets C–E, administration after food did not affect the area under the concentration-time curve (AUC) or maximum drug concentration (Cmax) of tramadol, but the tmax was prolonged by about 1 h compared with administration in fasting conditions. The mean ± standard deviation tmax and t1/2 for tablet D (IR:SR: 35:65 mg) in the fasting condition was 1.09 ± 0.56 h and 7.82 ± 0.85 h, respectively. The respective values in the fed condition were 2.47 ± 1.06 h and 7.12 ± 0.85 h, respectively.
Conclusions
To address the potential concerns regarding existing formulations of tramadol, a twice-daily, extended-release bilayer formulation of tramadol consisting of an IR and SR layer was developed. Pharmacokinetic studies confirmed that the plasma tramadol concentration increased quickly after administration and was maintained over a long period of time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
By adjusting the composition of the excipients, tramadol formulations with various dissolution rates could be prepared, and twice-daily bilayer tablets could be formulated with 35% of tramadol in the immediate-release (IR) portion and 65% in the sustained-release (SR) portion. |
The area under the plasma tramadol concentration-time curve (AUC) of the bilayer tablets was similar to that of commercially available IR and SR formulations. The maximum plasma tramadol concentration (Cmax) was lower than that of the IR formulation and higher than that of the SR formulation. The time to the maximum tramadol concentration (tmax) was earlier than that of the SR formulation and similar to that of the IR formulation. The half-life (t1/2) was longer than that of the IR and SR formulations. |
Since the Cmax and AUC were equivalent when administered in combination with food, there was no effect on bioavailability. |
1 Introduction
Tramadol hydrochloride [(1RS,2RS)-2-[(dimethylamino)methyl]-1-(3-methoxyphenyl) cyclohexanol monohydrochloride] is a centrally acting analgesic that acts as a μ-opioid receptor agonist and inhibits serotonin and noradrenalin reuptake [1,2,3]. Tramadol has been used as an analgesic in patients with carcinoma-associated pain intractable to nonopioid analgesics and for managing chronic pain [4, 5]. It is now available in more than 100 countries, and it was first approved in Japan as an injectable agent in 1978 [6].
Tramadol is available in a variety of formulations, including capsule, tablet, liquid, injectable and suppository preparations. In Japan, oral tramadol was first approved as an immediate-release (IR) formulation (four times daily; QID) in 2010 [7]. This was followed by the approval of a combination tablet with acetaminophen, another analgesic with a different mechanism of action, in 2011 [8] and a once-daily (QD) sustained-release (SR) formulation in 2015 [9]. IR formulations can provide an immediate onset of pain relief, but frequent dosing (QID) may compromise adherence, which may result in inadequate pain relief [10, 11]. The SR formulations, by comparison, may achieve greater adherence and pain relief, but the slow uptake after administration precludes a rapid onset of the analgesic effect [12,13,14]. Furthermore, it may take several days to reach a stable steady state, in which time the analgesic effect may be inadequate.
In clinical settings, the tramadol formulation prescribed should be chosen after considering various factors, including the patient’s condition, pain severity, history of drug adherence, concomitant medications and lifestyle [4, 5]. Considering these factors and the properties of the available formulations, alternative formulations of tramadol that provide optimal pharmacotherapy, including a rapid onset of action combined with sustained analgesia, are desired.
The following characteristics were considered necessary during development: (1) effective hemodynamic activity with sustained plasma drug concentrations with twice-daily (BID) oral administration; (2) the blood tramadol concentration should increase quickly after administration of each tablet with sustained levels between doses; (3) an appropriately sized tablet that is easy to swallow; (4) good stability with a formulation allowing effective quality control and manufacturability. Therefore, a novel SR formulation of tramadol that combines SR and IR components in a bilayer tablet with these properties was designed and developed (Fig. 1). It was hypothesized that this double-layered tablet would function as an eroding–dissolving SR formulation, in which the IR layer would be immediately released upon administration, and the remaining SR layer would gradually dissolve while forming a gel. This article describes the development, physicochemical characteristics and human pharmacokinetics of this novel tramadol formulation.
2 Methods
2.1 Materials
Tramadol was manufactured by Cadila Healthcare Ltd. (India) and milled and powdered for use. It was combined with the following additives: lactose hydrate (LH; DFE Pharma, The Netherlands; disintegration aid), microcrystalline cellulose (MCC; Asahi Kasei, Japan; binder) and erythritol (Nikken Chemical, Japan; dissolution aid) as excipients; croscarmellose sodium (CCMC-Na; DuPont, USA) and partly pregelatinized starch (PCS; Asahi Kasei) as disintegrators; pullulan (Hayashibara, Japan), hydroxypropyl cellulose-SL (HPC-SL; Nippon Soda, Japan), carboxyvinyl polymer (CVP; Lubrizol, USA), hydroxypropyl cellulose-H (HPC-H; Nippon Soda) and carmellose sodium (CMC-Na; Daicel Miraizu, Japan) as binders; magnesium stearate (MgSt; Taihei Chemical Industrial, Japan) as a lubricant; hypromellose (HM; Shin-Etsu Chemical, Japan) and macrogol 6000 (PEG6000; macrogol 6000P, NOF Corp., Japan) as a plasticizer; and yellow and red ferric oxide (Kishi Kasei, Japan) as coloring agents. Tramadol, MCC, CCMC-Na, HPC-SL, HPC-H, pullulan, CMC-Na, MgSt, HM and PEG6000 all conformed to the Japanese Pharmacopoeia [15].
Reference tramadol products were BID SR tablets (ZSR; Zydol® SR tablet 100 mg, Grünenthal, Germany) and QID IR capsules (ZIR; Zydol® capsule 50 mg, Grünenthal) marketed outside Japan, as well as the following tramadol formulations marketed in Japan: 25 mg and 50 mg QID IR tablets (IR25, Tramal® OD tablet 25 mg; IR50, Tramal® OD tablet 50 mg, Nippon Shinyaku, Japan), QD SR tablets (SR100; Onetram® QD tablet 100 mg, Nippon Shinyaku), QID tramadol/acetaminophen combination tablet (tramadol/acetaminophen tablet; Tramcet® 37.5 mg tramadol/325 mg acetaminophen combination tablet, Janssen Pharmaceutical, Japan) and bilayer SR tramadol tablets (TZ100; Tramadol Sandoz® SR, tramadol sustained release tablet; Sandoz, Australia).
2.2 Preparation of the Test Tablets
Tablets A–E were prepared by combining tramadol granules with varying compositions and excipients to adjust the dissolution profiles. The composition, size and weight of the test tablets are summarized in Table 1. The methods and conditions used to prepare the tramadol granules are described in the subsequent sections.
2.2.1 Preparation of Tramadol Granules for the IR and SR Layers for Tablets A and B
To prepare the IR layer granules, tramadol and erythritol were mixed. Then, a binder solution (containing pullulan 2% w/V) was sprayed in a fluidized bed granulator (Freund Corp., Japan; inlet air temperature: 70 °C; exhaust air temperature: 30 °C). The mixture was dried (exhaust air temperature: 40 °C) and sieved through an 850-µm mesh. The sieved product was mixed with a disintegrator (CCMC-Na) and a lubricant (MgSt). The resulting granules were used as the IR layer.
To prepare the SR layer granules, tramadol, HPC-H and CMC-Na were mixed and granulated by spraying purified water in the fluidized bed granulator (inlet air temperature: 70 °C; exhaust air temperature: 30 °C). The mixture was then granulated and dried (exhaust air temperature: 40 °C). After sieving the dried mixture through a 355-µm mesh, the sieved product was mixed with CVP and a lubricant (MgSt). The resulting granules were used as the SR layer.
Prototype tablets containing different matrices, as SR formulations, were prepared by adjusting the ratios of HPC-H, CVP and CMC-Na to alter the kinetics of tramadol release from the tablet formulations. These prototype tablets are designated X, Y and Z.
2.2.2 Preparation of Tramadol Granules for the IR and SR Layers in Tablets C, D and E
For tablets C, D and E (finished dosage formulations), tramadol granules exhibiting IR and SR properties were prepared. For the IR layer granules, tramadol, PCS, MCC and LH were mixed and granulated by spraying HPC-SL solution (3.5% w/V) containing dye (yellow ferric oxide and/or red ferric oxide) in the fluidized bed granulator (inlet air temperature: 60 °C; exhaust air temperature: 31‒47 °C) and dried (exhaust air temperature: 63 °C). The dried product was sieved through a 991-μm mesh, and the sieved product was mixed with the lubricant (MgSt) to yield the IR layer granules.
For the SR layer granules, tramadol, HPC-H and CMC-Na were mixed and granulated by spraying purified water in the fluidized bed granulator (inlet air temperature: 60 °C; exhaust air temperature: 33‒46 °C) and dried (inlet air temperature: 85 °C; exhaust air temperature: 55 °C). The dried product was sieved through a 991-μm mesh, and the sieved product was mixed with CVP and MgSt to yield the SR layer granules.
2.2.3 Preparation and Film-Coating of Double-Layered Tablets
The SR granules and IR granules were added, in that order, to a rotary press mold (Hata Tekkosho Co., Ltd., Japan) to prepare double-layered tablets. The double-layered tablets were then film-coated by spraying them with a coating solution (HM and PEG6000) under an air dryer (inlet air temperature: 70 °C; exhaust air temperature: 25‒48 °C) using film coating apparatus from Powrex Corp. (Japan).
2.3 Dissolution Test
The dissolution of the test tablets and commercially available formulations was determined according to the recommendations of the Japanese Pharmacopoeia [15]. For the dissolution test using the “second fluid,” a single tablet was placed in 900 ml of a mixture of phosphate buffer solution (pH 6.8) and water (1:1) (Kanto Chemical Co., Inc., Japan) and agitated using a paddle at several rotation speeds (50, 100 or 200 rpm) or immersed in McIlvaine buffer solution using a basket using dissolution test apparatus from Toyama Sangyo Co., Ltd. (Japan). For all tests, samples of the dissolution medium were taken at the intervals specified in the corresponding figure legends. The concentrations of tramadol were determined by high-performance liquid chromatography (HPLC) using the Alliance e2695 system (Nihon Waters, Japan) with an ultraviolet detector (2489UV/Vis Detector, Nihon Waters) and a TSK gel ODS-80TS QA column (4.6 mm inner diameter × 150 mm, 5 µm; Tosoh Corp., Japan). The mobile phase consisted of diluted trifluoroacetate (1:2000)/acetonitrile mixture (3:1) (Kishida Chemical Co., Ltd., Japan) injected at a flow rate of 1 ml/min. The column temperature was 40 °C. The HPLC procedures were validated internally.
2.4 Pharmacokinetic Studies
2.4.1 Single-Dose Pharmacokinetic Study Using Tablets A and B and Reference Products (ZSR and ZIR)
Twenty-six healthy adult, non-Japanese, white male volunteers aged 18–44 years old (inclusive) were enrolled and allocated to 1 of 24 possible treatment sequences, comprising a single 100 mg dose of two of four potential candidate formulations of tramadol HCl and a single 100 mg dose of one of the control formulations (ZIR or ZSR). A formal sample size calculation was not done. This study was conducted at Inveresk Research (Edinburgh, UK) between January 11, 2003, and March 5, 2003.
We report data for two formulations (referred to as tablets A and B in the present report) out of four candidate formulations. The participants received the allocated drugs in a three-period crossover design, with a 7-day washout period between each dose: (1) one allocated test formulation (one tablet), (2) ZSR (one tablet) or ZIR (two capsules) and (3) a second allocated test formulation. All drugs were administered orally in the morning in fasting conditions (≥ 9 h prior to study drug administration) together with 200 ml water. Blood samples (approximately 5 ml per sample) were obtained at the following times: predose, 0.5, 0.75, 1, 1.5, 2, 2.5, 3, 4, 5, 6, 8, 10, 12, 24 and 48 h postdose. Plasma samples were prepared and stored at –80 °C until analysis. The plasma concentrations of tramadol and the major active metabolite M1 (O-demethyl tramadol) were determined by HPLC, as described in the section Measurement of Plasma Drug Concentrations (heading #2.5).
2.4.2 Effects of Food on Pharmacokinetics of Tablets C–E Study
We investigated the effects of food on the bioavailability and safety of three types of test tablets when administered as a single dose under fasting and fed conditions in multiple studies. In each study, with a single study drug (tablets C, D or E) per dose (50, 100 or 150 mg), 20 healthy adult Japanese males aged 20–44 years old were assigned to two groups (fasting-first and fed-first; 10 per group) in a two-period crossover design with a washout period of ≥ 7 days between the doses in the first and second periods. A formal sample size calculation was not done. This study was conducted at SOUSEIKAI Hakata Clinic (Fukuoka, Japan) and SOUSEIKAI Nishi Kumamoto Hospital (Kumamoto, Japan) between May 23, 2019 and June 17, 2019.
In the fasting condition (≥ 10 h prior to study drug administration; morning), one tablet (tablet C, D or E) was orally administered together with 150 ml water. Blood samples (approximately 2 ml per sample) were collected at the following times: predose, 0.25, 0.5, 0.75, 1, 1.25, 1.5, 2, 2.5, 3, 4, 5, 6, 9, 12, 24 and 48 h postdose. Plasma samples were prepared and stored at −80 °C until analysis.
The plasma tramadol and M1 concentrations were measured by liquid chromatography (LC) tandem mass-spectrometry (MS/MS). In the fed condition, the subjects were given breakfast in the morning and, up to 10 min later, were orally administered one test tablet together with 150 ml water. The remaining study procedures were identical to those in the fasting condition. As a reference, the pharmacokinetics of tablet D were compared with those of published data for commercially available IR and SR formulations [7, 9].
2.4.3 Ethics
The pharmacokinetic studies were conducted by research organizations (Inveresk Research, SOUSEIKAI Hakata Clinic and SOUSEIKAI Nishi Kumamoto Hospital) under contract with Nippon Zoki Pharmaceutical Co., Ltd. The studies were approved by the ethical review committees at the research organizations. All participants provided written informed consent.
2.5 Measurement of Plasma Drug Concentrations
2.5.1 Plasma Concentrations of Tablets A and B and Reference Products ZSR and ZIR
To prepare the sample solutions, 50 µl of the internal standard solution (O-ethyl tramadol; Nippon Zoki Pharmaceutical Company Ltd., Japan) and 100 μl water were added to 500 μl plasma. Next, 50 μl 25% ammonium hydroxide (Sigma, USA) was added and briefly stirred, followed by 4 ml dichloromethane (Rathbum Chemicals Ltd., UK), and mixed by inversion for 10 min. After centrifugation (2500 rpm, 10 min), the supernatant was transferred to another container; 4 ml dichloromethane was added to the transferred supernatant, mixed by inversion for 10 min and centrifuged, after which the supernatant was discarded. Two dichloromethane layers were pooled together and allowed to evaporate under a nitrogen stream at 40 °C. Then, 240 μl of a mixture of water and methanol (7:3) (Rathbum Chemicals Ltd.) was added and stirred for about 30 s for use as the sample solution.
The HPLC system consisted of a fluorescence detector (FP920, Jasco Corp., Japan), a pump (HP1050, Agilent, USA), and an auto sampler (HP1050, Agilent). The HPLC measurement was performed using a column (Develosil ODS-HG, 4.6 mm inner diameter × 250 mm, 5 µm; Nomura Chemical Co., Ltd., Japan). The mobile phase consisted of 0.05 mol/l of a sodium phosphate buffer solution (pH 2.5; Sigma)/acetonitrile (Rathbum Chemicals Ltd.)/tetrahydrofuran (Rathbum Chemicals Ltd.) mixture (85:11:4) at a flow rate of 0.7–0.8 ml/min with a column temperature of 30 °C. For the fluorescence detector, the excitation wavelength was 270 nm and the fluorescence wavelength was 296 nm. For the quantitative estimation, the peak area ratio of the sample solution to the internal standard was calculated and compared with the peak area ratio of the sample solution to the standard solution. The HPLC procedures were validated internally.
2.5.2 Plasma Concentrations of Tablets C, D and E
To prepare the sample solutions, 10 µl of the internal standard solution (mixture of tramadol-d6 and O-demethyl tramadol-d6; Clearsynth Labs Ltd., India) and 150 µl of acetonitrile (Fujifilm Wako Pure Chemical Corp., Japan) were added to 50 μl plasma and stirred. After centrifuging, 50 µl of the supernatant was transferred to another container, and 100 µl of a 10 mmol/l formic acid ammonium solution containing 0.1 vol% formic acid (Fujifilm Wako Pure Chemical Corp.) and 50 µl of methanol (Fujifilm Wako Pure Chemical Corp.) were added, stirred thoroughly and used as the sample solution.
HPLC was performed using the Shimadzu 30A system (Shimadzu Corp., Japan) with an API4000 MS/MS (AB Sciex, USA). The HPLC measurement was performed using an Acquity UPLC BEH C18 column (2.1 mm inner diameter × 50 mm, 1.7 µm; Waters) under a gradient of mobile phases A (10 mmol/l formic acid ammonium solution containing 0.1 vol% formic acid) and B (methanol) at a flow rate of 0.45 ml/min and a column temperature of 50 °C.
MS/MS measurements were performed in the positive electrospray ionization mode to detect the precursor ions at m/z 264.3 (tramadol), m/z 250.3 (M1), m/z 270.3 (tramadol-d6) and m/z 256.3 (O-demethyl tramadol-d6), fragment ions at m/z 58.1 (tramadol and M1) and m/z 64.1 (tramadol-d6 and O-demethyl tramadol-d6) and optimized values for the setting values. For these ions, the declustering potentials were 41 V (tramadol and tramadol-d6), 37 V (M1) and 52 V (O-demethyl tramadol-d6), collision energies were 48 eV (tramadol and tramadol-d6), 39 eV (M1) and 42 eV (O-demethyl tramadol-d6), collision cell exit potentials were 11 V (tramadol and tramadol-d6) and 10 V (M1 and O-demethyl tramadol-d6), collision-activated dissociation gas pressure was 8 psi, curtain gas pressure was 40 psi, and temperature was 600 °C. LC/MS/MS was performed using an internally validated method.
For the quantitative estimation, the peak area ratio of the sample solution to the internal standard substance was calculated and compared with the peak area ratio of the sample solution to the standard solution.
2.6 Determination of Pharmacokinetic Parameters
The following pharmacokinetic parameters for tramadol and M1 were determined from non-compartmental models: area under the concentration–time curve from 0 to time t (trapezoidal method; AUC0–t), AUC from time 0 to infinity (AUC0–inf), maximum concentration (Cmax; measured values), time to the maximum concentration (tmax) and the half-life (t1/2). WinNonlin version 3.1 was used for the data obtained in the single-dose study (see Single-Dose Pharmacokinetic Study Using Tablets A and B and Reference Products (ZSR and ZIR); heading #2.4.1), and version 8.1 was used for the data obtained in the food-effect study (see Effects of Food on Pharmacokinetics of Tablets C–E Study; heading #2.4.2).
For the single-dose study, analysis of variance (ANOVA) techniques were used to compare the natural log-transformed values for AUC0–inf and Cmax of tramadol after administration of tablets A and B versus administration of ZSR and ZIR and to determine the 90% confidence intervals (CI). For the food-effect study, ANOVA was performed using natural log-transformed values for AUC0–t, Cmax and t1/2 and for untransformed tmax of tramadol. Differences in the mean of the natural logarithm-transformed AUC0–t and Cmax of tramadol were calculated between administration under fasting and fed conditions in the food-effect study, and their 90% CIs were determined. Bioequivalence was assumed for mean ratios within the range of log(0.80) to log(1.25). In both studies, the natural log-transformed values were inverse-log-transformed for reporting in this article.
Significance testing was not performed for any of the pharmacokinetic parameters of M1.
2.7 Simulation of Tramadol Concentrations During Multiple Dosing
Simulation of plasma tramadol concentrations during multiple dosing was performed using the superimposition method in WinNonlin software [16]. The simulations involved a scenario where tablet D is administered BID for 5 days.
3 Results
3.1 SR Layer
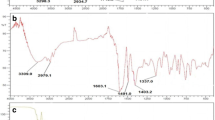
Cellulose, synthetic polymer and natural polymer bases, which provide a hydrophilic matrix, can be used to prepare eroding–dissolving SR formulations. Potential formulations were screened in a trial-and-error approach to determine optimal formulations based on the tablet’s properties, stability and dissolution profiles. Polymer-grade hydroxypropyl cellulose (HPC-H) provided excellent formability as a base and could be combined with CVP and CMC-Na to facilitate water absorption and gel-forming capacity. Figure 2 shows the tramadol dissolution profiles of three prototype tablets (formulations X, Y and Z) relative to that of the reference product ZSR. All prototype tablets showed erosion and dissolution, with dissolution profiles tending to shift upwards, with a visually similar profile to that of ZSR, suggesting comparable dissolution mechanisms. The release of tramadol could be adjusted by varying the proportions of the base components, and formulation Z (HPC-H, CVP and CMC-Na 73:22:5) had a dissolution pattern closest to ZSR. Furthermore, adjusting the proportion of highly water-absorbable CMC-Na prolonged drug release in formulation X (HPC-H, CVP and CMC-Na 70:10:20) and formulation Y (HPC-H, CVP and CMC-Na 50:20:30).
In vitro dissolution profiles of various prototype tablet formulations (designated X, Y and Z) using different ratios of HPC-H, CVP and CMC-Na as the matrix base and of a reference formulation (ZSR). Paddle speed: 50 rpm. Samples were collected at 0, 15 min, 30 min, 1 h, 2 h, 3 h, 4 h, 6 h and 8 h. CMC-Na carmellose sodium, CVP carboxyvinyl polymer, HPC-H hydroxypropyl cellulose-H, ZSR Zydol® sustained-release tablet
3.2 Ratio of the IR/SR Layers in the Combination Tablet
We next adjusted the release rate of the IR and SR layers, such that the dissolution profile of the IR layer was visually similar to that of a marketed QID IR formulation (ZIR) and the SR layer was comparable to that of a BID SR formulation (ZSR) available in countries other than Japan. The ratio of IR and SR layers was varied to achieve the desired formulation properties. For this, formulation Z was used as the SR layer and the optimum combination ratio was explored by using tablets A and B, in which the ratio of the IR to SR layers was 20:80 and 40:60, respectively. The composition, size and mass of tablets A and B are shown in Table 1.
Figure 3 shows the dissolution profiles measured over 8 h for tablets A and B as well as the reference products ZIR and ZSR. Tablets A and B both displayed biphasic dissolution profiles, characterized by a rapid initial increase followed by a sustained release at a constant rate. The mean dissolution of tablets A and B was 25% and 46%, respectively, at 15 min after the start of the test, indicating that the IR layer was rapidly dissolved, and was followed by a pseudolinear concentration curve with 75% and 83% of the drug released by 8 h. The mean dissolution of ZIR was 98% at 15 min, which indicated that almost the entire dose was released within this period of time. The mean dissolution of ZSR was 13% at 15 min, followed by the pseudolinear curve reaching a dissolution of 91% at 8 h.
Comparative in vitro dissolution profiles of tablets A and B and two reference formulations in the Japanese Pharmacopoeia [15] dissolution test (pH 6.8) with paddle stirring at 50 rpm (n = 3). Paddle speed: 50 rpm. Samples were collected at 0, 15 min, 30 min, 1 h, 2 h, 3 h, 4 h, 6 h and 8 h. ZIR Zydol® immediate-release tablet, ZSR Zydol® sustained-release tablet
Figure 4 shows the dissolution and disintegration behaviors of tablet C in water. The IR layer began to disintegrate within 4 min and was completely dissolved 8 min later. By comparison, the remaining SR layer formed a gel from the surface and gradually dissolved through erosion.
Dissolution of the double-layered tablet (tablet C) in water. Photographs were taken at the start of stirring (a), after 4 min (the IR layer of the tablet quickly disintegrated and dissolved; b) and after 8 min (the IR layer had disappeared, and gelation of the SR layer was initiated on the surface; c)
3.3 Pharmacokinetics of Tablets A and B and Reference Products ZSR and ZIR
A single dose of tablet A or B (1 tablet) or the reference products ZSR (1 tablet) or ZIR (2 capsules) were administered to 11–12 healthy adults in fasting conditions. Figure 5a shows the plasma tramadol concentrations measured for 24 h postdose. The pharmacokinetic parameters are summarized in Table 2. The plasma concentrations of tramadol increased rapidly after administration of tablets A and B, and the maximum plasma concentration was reached (i.e., tmax) at 1.92 and 1.16 h postdose, respectively. After administration of ZSR, the plasma tramadol concentration increased at a slower rate, and the tmax was 3.29 h. For ZIR, the plasma tramadol concentration increased rapidly with tmax of 1.00 h. The AUC0–inf for tablets A and B showed bioequivalence to those of ZSR and ZIR, suggesting comparable bioavailability. The Cmax for tablets A and B was 38% and 52%, respectively, of that of ZIR, indicating that tablets A and B achieved lower peaks in tramadol concentrations and may thus reduced the risk of adverse drug reactions associated with high peak concentrations. The t1/2 for tablets A and B was 12.24 and 11.14 h, respectively. Table 3 and Fig. 5b show the pharmacokinetic profile for M1 after administration of each formulation.
Mean plasma tramadol (a) and tramadol metabolite M1 (b) concentrations versus time profiles after a single oral dose of tablets A and B or two reference products in healthy male volunteers under fasting conditions. Values are means ± standard deviation (n = 11–12). IR immediate release, SR sustained release, ZIR Zydol® IR tablet, ZSR Zydol® SR tablet
3.4 Preparation of the Final Candidate Formulation
Considering the pharmacokinetic properties of tablets A and B, particularly the slightly greater Cmax of tablet B relative to that of ZSR, the appropriate combination ratio of the IR:SR layers was explored, and the ratio 35:65 was chosen to facilitate its manufacturability and quality control. Three alternative formulations were also prepared with slight modifications to the formulation in consideration of manufacturing suitability, quality control, dosage and identifiability (Table 1).
3.5 Dissolution Profiles of the Finished Dosage Formulations (Tablets C–E) and Other Tramadol Formulations Available in Japan
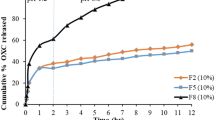
Figure 6 shows the results of dissolution studies performed as recommended by the Japanese Pharmacopoeia [15] (second fluid for the dissolution test, paddle method, 50 rpm) for the finished dosage formulations (tablets C–E) as well as four commercially available formulations (IR25, IR50, SR100 and tramadol/acetaminophen combination tablet). The commercially available formulations all released nearly the entire dose within 15 min. The commercial SR100 tablet showed an almost linear SR profile with a mean dissolution of approximately 60% at 10 h. By contrast, tablets C, D and E (IR layer: 35% and SR layer: 65%) displayed biphasic dissolution profiles with an initial immediate release followed by a slower release. The mean dissolution was 40% at 15 min, indicating that the total amount of tramadol contained in the IR layer was released quickly. Thereafter, the drug was released more gradually, with a mean dissolution of 56% at 1 h, 75% at 4 h and 93% at 10 h, with a near-linear release after 1 h (see tablets C, D and E in Fig. 6a). Despite concern that the initial increase in the plasma tramadol concentration following administration of tablet C would exceed that of the IR25 tablet and tramadol/acetaminophen combination tablet, the amount released within 15 min was 22.9 mg for tablet C, 24.4 mg for the QD25 tablet and 37.9 mg for the tramadol/acetaminophen combination tablet, suggesting that the plasma tramadol concentration after administration of tablet C is unlikely to exceed the concentration achieved with the commercial tablets. Figure 6b compares the dissolution of tablet D, the final formulation, with that of a commercially available bilayer tablet (TZ100). As illustrated in this figure, tramadol was released from tablet D more quickly, by 15 min, and the dissolution was higher for up to 4 h compared with TZ100.
a Dissolution profiles of the finished dosage formulations (tablets C–E) and three commercially available products in the second fluid (pH 6.8). b Dissolution profiles of tablet D and commercially available bilayer sustained-release tramadol tablets (TZ100). Values in (a) and (b) are means ± standard deviation (n = 6). Paddle speed: 50 rpm. Samples were collected at 0, 5 min, 10 min, 15 min, 30 min, 1 h, 2 h, 4 h, 6 h, 8 h and 10 h. IR25 Tramal® OD tablet 25 mg, IR50 Tramal® OD tablet 50 mg, SR100 Onetram® QD tablet 100 mg, TZ100 Tramadol Sandoz® sustained-release 100 mg bilayer tablet
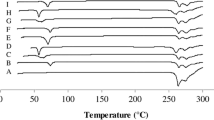
To assess the resistance of the proposed formulation to different types of physical stress in the gastrointestinal tract, the dissolution test was repeated by changing the stirring speed (50, 100 or 200 rpm), moisture (adding 1% polysorbate 80), pH (1.2, 6.8, 7.5, water) and the test apparatus (basket or disintegration apparatus). Figure 7 shows the results of these tests using tablet C. There were minimal differences in the mean dissolution at 15 min, 2 h and 10 h in the test conditions, which suggests that the proposed formulation would be resilient to pH fluctuations or mechanical forces in the gastrointestinal tract.
Comparison of the amount of tramadol released from tablet C after 15 min, 2 h and 10 h in various test conditions. (1) Paddle, 50 rpm, diluted McIlvaine buffer solution (pH 7.5). (2) Paddle, 100 rpm, diluted McIlvaine buffer solution (pH 7.5). (3) Paddle, 200 rpm, diluted McIlvaine buffer solution (pH 7.5). (4) Paddle, 50 rpm, diluted McIlvaine buffer solution (pH 7.5) + 1% polysorbate 80. (5) Paddle, 50 rpm, first fluid for dissolution test (pH 1.2). (6) Paddle, 50 rpm, second fluid for dissolution test (pH 6.8). (7) Paddle, 50 rpm, water. (8) Basket, 200 rpm, diluted McIlvaine buffer solution (pH 7.5). (9) Disintegration apparatus, diluted McIlvaine buffer solution (pH 7.5). Values are means ± standard deviation (n = 6)
3.6 Effects of Food on the Pharmacokinetics of the Finished Dosage Formulations (Tablets C–E)
In this study, healthy adults were administered with a single dose (1 tablet) of tablet C, D or E (20 adults per study) in fasting and fed conditions in a two-period crossover. Figure 8a shows the plasma tramadol concentrations measured over a period of 48 h after administration using tablet D as an example. Table 4 summarizes the pharmacokinetic data for each tablet. For tablet D, the plasma tramadol concentration increased rapidly after administration, and the maximum plasma concentration was reached at 1.09 h postdose in fasting conditions and at 2.47 h in fed conditions. Similar results were obtained for tablets C and E. The 90% CI for the mean ratios of the natural logarithm-transformed AUC0–t and Cmax after a single dose of tablets C, D and E under fasting and fed conditions fell within the range of log(0.80) to log(1.25), satisfying the criteria for bioequivalence and indicating that AUC0–t and Cmax would not be affected by administration in fed or fasting conditions. However, tmax was delayed by approximately 1 h in fed conditions. The corresponding data for the active metabolite, M1, are shown in Table 5 and Fig. 8b (for tablet D as an example).
3.7 Simulated Pharmacokinetics During Multiple Doses
Finally, the pharmacokinetics and plasma tramadol concentrations were simulated during multiple doses of tablet D. As illustrated in Fig. 9, the plasma tramadol concentration reached a near steady state about 24 h postdose without excessive accumulation. The estimated maximum (peak) and minimum (trough) plasma concentrations at steady state were approximately 300 ng/ml and 120 ng/ml, respectively. Supporting this simulation, a pharmacokinetic study in which 100 mg tablets with equivalent dissolution properties to tablet D were administered for 7 days (QD on days 1 and 7; BID on days 2–5) in seven healthy adult males [17]. In that study, the steady state was achieved about 24 h after the first dose [17, 18]. The trough tramadol concentration was consistent with the results of the simulation, as depicted in Fig. 9.
4 Discussion
This article described the development and pharmacokinetic properties of double-layer tablet formulations of tramadol that combine an IR layer providing rapid absorption and onset of the analgesic effect together with a matrix-type SR layer providing a sustained analgesic effect.
In general, SR formulations release the drug gradually to provide prolonged activity over a long period of time [13, 14]. However, the slow dissolution results in a slow increase in the plasma drug concentration, thus delaying the onset of the clinical effect. Therefore, the goal was to develop an SR formulation that combined the properties of an immediate onset of analgesic effect with a sustained analgesic effect from BID administration, with reference to the desired characteristics described in the Introduction. Based on the results of the physicochemical tests, a formulation comprising IR and SR layers was developed in a tablet form.
To confirm that the physicochemical properties translated into the physiological setting, pharmacokinetic studies were performed for the finished dosage formulations (tablets C–E). When administered in combination with food, the AUC0–t and Cmax of tablets C–E were equivalent to those in fasting conditions, suggesting no impact on bioavailability, but absorption was delayed by approximately 1 h. The pharmacokinetic characteristics of the chosen formulation, tablet D, were also compared with those of published data for commercially marketed SR (SR100 tablets [9]) and IR (IR50 capsule [7]) formulations (Table 6). The tmax was numerically similar to that of the IR50 capsule × 2, and the t1/2 was approximately 1–2 h longer than that reported for the SR100 tablets and IR50 capsule × 2. These findings suggest that the IR and SR components of the bilayer tablets mimic those of formulations containing either IR or SR tramadol.
Because the pharmacokinetic studies involved a single dose, the pharmacokinetics of tramadol during multiple oral doses of tablet D over 5 days under fasting conditions were simulated. This analysis indicated that the plasma tramadol concentrations would reach near steady state at approximately 24 h postdose without excessive accumulation. From a clinical perspective, this suggests that the plasma tramadol concentration would reach a clinically relevant level within 1 day of twice-daily administration.
Prior studies have compared the bioequivalence and pharmacokinetics of IR and SR formulations of tramadol, including Contramid® OAD, which also comprises IR and SR layers, as dry-coated tablets that are intended for once-daily administration [19].
A double-layered, extended-release tramadol tablet with IR and SR portions, similar to the developed formulation, is marketed in several countries, including Switzerland, Australia, the UK and South Korea. That formulation is produced with a white IR layer and a green SR layer and is intended for twice-daily administration. The Australian package insert [20] for that formulation reported a Cmax of 142 ng/ml and a tmax of 4.9 h. In the pharmacokinetic studies of tablet D (100 mg tablet), the final formulation, the Cmax was 219.8 ng/ml and the tmax was 1.09 h (Table 4). In the dissolution tests (Fig. 6b), tramadol was released more quickly from tablet D, by 15 min, and the dissolution rate was higher for up to 4 h thereafter, compared with TZ100. Overall, these findings suggest that the ratio of tramadol in the IR/SR layers was optimal, based on appropriate selection of the excipients, allowing the final formulation to achieve the desired characteristics described in the Introduction.
Some physicians may also prefer twice-daily administration. In an online survey of 408 physicians conducted in February 2018 in Japan that was sponsored by the manufacturer, 63% of the physicians reported that they preferred twice-daily administration of tramadol tablets (unpublished data). Although the reason for this preference was not explored, administration BID may facilitate dose adjustments to achieve the desired clinical effect and could reduce the possibility of emergent pain due to missing one dose.
As part of the clinical development of this SR formulation of tramadol, two phase III, randomized placebo-controlled treatment-withdrawal studies were conducted in Japanese patients with chronic pain associated with knee osteoarthritis [18] or postherpetic neuralgia [21]. In both studies, tramadol was superior to placebo in terms of the time from randomization to an inadequate analgesic effect and the proportion of patients experiencing inadequate analgesic effects.
Thus, to the best of our knowledge, this is the only twice-daily formulation of tramadol bilayer tablets comprising IR and SR portions for which the efficacy has been assessed in double-blind controlled trials [18, 21].
The most frequent adverse events in both studies were constipation, nausea, somnolence and dizziness, which are common in studies of tramadol. Nevertheless, the frequencies of adverse events in both studies were numerically similar to or lower than those reported in prior studies of tramadol in Japanese patients. At the end of the study or upon treatment withdrawal, patients in both studies completed questionnaires and reported few or no signs of drug dependence in terms of irritability/restlessness, sleeplessness, nausea/vomiting/trembling/sweating, desire to take the medication, convulsions and dizziness/hallucinations.
The proposed formulation of tramadol was subsequently approved in Japan in September 2020 for the indication of chronic pain, and an additional indication for cancer pain was approved in May 2022 [21].
4.1 Limitations
We also mention some limitations of this study. First, the tests described here do not cover all of the preclinical tests performed. Second, the pharmacokinetic tests do not confirm that the rapid absorption translates into a rapid onset of analgesia; additional pharmacodynamic tests are required to confirm the rapid onset of analgesia after administration. The pharmacokinetic study of tablets A and B relative to marketed formulations was performed in white males, whereas the pharmacokinetic study of tablets C–E was performed in Japanese males. Therefore, results may not be directly transferable because of possible genetic differences between Japanese and non-Japanese individuals. However, these data were used to evaluate formulations under development, and the final marketed formulation was tested in Japanese individuals. Finally, the simulation study was performed to predict the pharmacokinetics during 5 days of multiple doses, and different results may be obtained in real clinical studies. Nevertheless, the results of published phase III studies confirm that the chosen tramadol formulation exerts analgesic effects in patients with various forms of pain, extending the findings of these pharmacokinetic studies.
4.2 Conclusion
In conclusion, this SR formulation of tramadol comprises two layers with differing dissolution profiles, with 35% in the IR layer and 65% in the SR layer. The IR layer dissolves quickly with a rapid increase in the plasma tramadol concentrations. The SR layer forms a gel matrix that slows its dissolution and absorption to maintain plasma concentrations at clinically relevant levels for a longer time after administration.
References
Subedi M, Bajaj S, Kumar MS, Yc M. An overview of tramadol and its usage in pain management and future perspective. Biomed Pharmacother. 2019;111:443–51. https://doi.org/10.1016/j.biopha.2018.12.085.
Boureau F, Legallicier P, Kabir-Ahmadi M. Tramadol in post-herpetic neuralgia: a randomized, double-blind, placebo-controlled trial. Pain. 2003;104(1–2):323–31. https://doi.org/10.1016/s0304-3959(03)00020-4.
Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, Gilron I, Haanpää M, Hansson P, Jensen TS, Kamerman PR, Lund K, Moore A, Raja SN, Rice AS, Rowbotham M, Sena E, Siddall P, Smith BH, Wallace M. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14(2):162–73. https://doi.org/10.1016/s1474-4422(14)70251-0.
Japan Society of Pain Clinicians Committee for the Guidelines for the Pharmacologic Management of Neuropathic Pain. Guidelines for the Pharmacologic Management of Neuropathic Pain, 2nd ed, 2016. Tokyo: Shinko Trading Co., Ltd.
Japanese Society for Palliative Medicine. Clinical Guidelines for Cancer Pain Management, 2nd ed, 2020. Tokyo: Kanehara & Co., Ltd.
Nippon Shinyaku Co., Ltd. Tramal® Injection 100, Interview Form, June 2020 (8th ed). Available at: https://www.info.pmda.go.jp/go/interview/1/530263_1149400A1049_1_11F_1F.pdf. Accessed September 6, 2023. In Japanese.
Nippon Shinyaku Co., Ltd. Tramal® OD Tablets 25 mg, 50 mg, Interview Form, July 2023 (18th ed). Available at: https://www.info.pmda.go.jp/go/interview/1/530263_1149038F1024_1_10F_1F.pdf. Accessed July 5, 2023. In Japanese.
Janssen Pharma Co., Ltd., Mochda Pharmaceutical Co., Ltd. Tramcet® combination tablets (tramadol hydrochloride, acetaminophen), Interview Form, May 2023 (10th ed). Available at: https://www.info.pmda.go.jp/go/interview/1/800155_1149117F1020_1_010_2F.pdf. Accessed September 26, 2023. In Japanese.
Nippon Shinyaku Co., Ltd. Onetram® Tablets 100 mg, Interview Form, July 2023 (11th ed). Available at: https://www.info.pmda.go.jp/go/interview/1/530263_1149038G1020_1_15F_1F.pdf. Accessed July 5, 2023. In Japanese.
Klotz U. Tramadol–the impact of its pharmacokinetic and pharmacodynamic properties on the clinical management of pain. Arzneimittelforschung. 2003;53(10):681–7. https://doi.org/10.1055/s-0031-1299812.
Reeves RR, Burke RS. Tramadol: basic pharmacology and emerging concepts. Drugs Today (Barc). 2008;44(11):827–36.
Barkin RL. Extended-release tramadol (ULTRAM ER): a pharmacotherapeutic, pharmacokinetic, and pharmacodynamic focus on effectiveness and safety in patients with chronic/persistent pain. Am J Ther. 2008;15(2):157–66. https://doi.org/10.1097/MJT.0b013e31815b035b.
Keating GM. Tramadol sustained-release capsules. Drugs. 2006;66(2):223–30. https://doi.org/10.2165/00003495-200666020-00006.
Kizilbash A, Ngô-Minh CT. Review of extended-release formulations of tramadol for the management of chronic non-cancer pain: focus on marketed formulations. J Pain Res. 2014;7:149–61. https://doi.org/10.2147/jpr.S49502.
Ministry of Health, Labour and Welfare. Japanese Pharmacopoeia, 18th ed. Available at: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000066597.html.
Certara Phoenix Assistance. Nonparametric superposition methodology. Available at: https://onlinehelp.certara.com/phoenix/8.3/topics/NonParametric_Superposition_methodology.htm. Accessed July 5, 2022.
Nippon Zoki Pharmaceutical Co., Ltd. Twotram® (tramadol) tablets, 25 mg, 50 mg, 100 mg, 150 mg. Interview Form, December 2022 (9th ed). Available at: https://www.info.pmda.go.jp/go/interview/1/530288_1149038G2026_1_101_1F.pdf. Accessed July 5, 2023. In Japanese.
Kawai S, Sobajima S, Jinnouchi M, Nakano H, Ohtani H, Sakata M, Adachi T. Efficacy and safety of tramadol hydrochloride twice-daily sustained-release bilayer tablets with an immediate-release component for chronic pain associated with knee osteoarthritis: a randomized, double-blind, placebo-controlled, treatment-withdrawal study. Clin Drug Investig. 2022;42(5):403–16. https://doi.org/10.1007/s40261-022-01139-5.
Mongin G. Tramadol extended-release formulations in the management of pain due to osteoarthritis. Expert Rev Neurother. 2007;7(12):1775–84. https://doi.org/10.1586/14737175.7.12.1775.
Sandoz Pty Ltd. Tramadol Sandoz® SR (tramadol hydrochloride) sustained release tablets. Australian Product Information. July 18, 2023. Available at: https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2009-PI-01198-3. Accessed September 25, 2023.
Kawai S, Hasegawa J, Ito H, Yasuo F, Fukuuchi Y, Nakano H, Ohtani H, Sasaki K, Adachi T. Efficacy and safety of twice-daily tramadol hydrochloride bilayer sustained-release tablets with an immediate release component for postherpetic neuralgia: results of a phase III, randomized, double-blind, placebo-controlled, treatment-withdrawal study. Pain Pract. 2023;23(3):277–89. https://doi.org/10.1111/papr.13190.
Acknowledgments
The authors thank Nicholas D. Smith (EMC K.K.) for medical writing support, which was funded by Nippon Zoki Pharmaceutical Co., Ltd.
Funding
This study was funded by Nippon Zoki Pharmaceutical Co., Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors are employees of Nippon Zoki Pharmaceutical Co., Ltd. The authors are also listed as co-inventors on patent applications filed by Nippon Zoki Pharmaceutical Co., Ltd.
Ethics approval
The pharmacokinetic studies were conducted under contract with Nippon Zoki Pharmaceutical Co., Ltd., by the following research organizations, with approval from their ethical review committees: Inveresk Research (approval date: January 11, 2003), SOUSEIKAI Hakata Clinic (approval date: May 11, 2019) and SOUSEIKAI Nishi Kumamoto Hospital (approval date: May 11, 2019). All procedures in these studies were performed in accordance with the 1964 Helsinki Declaration (and its amendments).
Consent to participate
All participants provided written informed consent to participate.
Consent for publication
Not applicable.
Author contributions
Study conception: all authors. Study design: NI, SO, HS, MK, TA and KM. Data acquisition: NI, SO, HS, MK, TA and KM. Data analysis and interpretation: NI, HS and TA. Drafting of the manuscript: NI, HS, MK, TA and KM. Critical revision: all authors. Final approval: all authors. Accountable for the accuracy and integrity of the work: all authors.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ishitsubo, N., Oguro, S., Shimahashi, H. et al. Development, Physicochemical Characteristics and Pharmacokinetics of a New Sustained-Release Bilayer Tablet Formulation of Tramadol with an Immediate-Release Component for Twice-Daily Administration. Eur J Drug Metab Pharmacokinet 49, 87–100 (2024). https://doi.org/10.1007/s13318-023-00865-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-023-00865-1