Abstract
Introduction
Endothelial dysfunction is a risk factor for cardiovascular disease in patients with diabetes. We hypothesized that imeglimin, a novel oral hypoglycemic agent, would improve endothelial function.
Methods
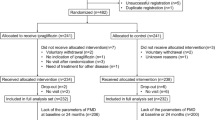
In this study, imeglimin was administered to patients with type 2 diabetes and HbA1c ≥ 6.5% who were not receiving insulin therapy. A meal tolerance test (592 kcal, glucose 75.0 g, fat 28.5 g) was performed before and 3 months after administration, and endothelial function, blood glucose, insulin, glucagon, and triglycerides were evaluated. Endothelial function was assessed by flow-mediated dilation (FMD).
Results
Twelve patients (50% male) with a median age of 55.5 years old (interquartile range [IQR] 51.3–66.0) were enrolled. Fasting FMD did not differ before or 3 months after imeglimin administration (from 6.1 [3.9–8.5] to 6.6 [3.9–9.0], p = 0.092), but 2 h postprandial FMD was significantly improved 3 months after imeglimin administration (from 2.3 [1.9–3.4] to 2.9 [2.4–4.7], p = 0.013). In terms of the glucose profile, imeglimin administration significantly improved HbA1c (from 7.2 ± 0.6% to 6.9 ± 0.6%, p = 0.007), fasting glucose (from 138 ± 19 mg/dL to 128 ± 20 mg/dL, p = 0.020), and 2 h postprandial glucose (from 251 ± 47 mg/dL to 215 ± 68 mg/dL, p = 0.035). The change in 2 h postprandial FMD between before and 3 months after imeglimin administration (Δ2 h postprandial FMD) was negatively correlated with Δ2 h postprandial glucose (r = − 0.653, p = 0.021) in a univariate correlation coefficient analysis. Both patients with and without decreased postprandial glucose 3 months after imeglimin administration had improved postprandial FMD.
Conclusion
In this small study, imeglimin administration improved 2 h postprandial FMD. Both glycemic control-dependent and -independent mechanisms might contribute to improved endothelial function.
Trial Registration
This research was registered in the University Hospital Medical Information Network (UMIN, UMIN000046311).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Endothelial function is impaired in diabetes, which leads to an increased incidence of cardiovascular events. |
We investigated whether imeglimin improved endothelial function by assessing flow-mediated dilation in patients with type 2 diabetes. |
What was learned from this study? |
Imeglimin administration for 3 months improved 2 h postprandial flow-mediated dilation. |
Imeglimin may have improved postprandial FMD by lowering postprandial glucose and impacting factors unrelated to glycemic control. |
This is a small observational study without a placebo group, and therefore further studies should verify the positive effects of imeglimin on endothelial function. |
Introduction
Cardiovascular disease (CVD) is the major cause of mortality in type 2 diabetes [1]. Hyperglycemia, dyslipidemia, and hypertension are CVD risk factors that contribute significantly to atherosclerosis [2]. The endothelium plays a central role in the development of atherosclerosis, and impaired endothelial function increases the risk of atherosclerotic vascular events [3]. Endothelial dysfunction results in impaired synthesis of nitric oxide, which can be estimated by measuring flow-mediated dilation (FMD) [4]. Patients with type 2 diabetes show lower FMD than individuals with normal glucose metabolism [5]. Postprandial FMD is lower than fasting FMD because endothelial function is affected by oxidative stress induced by postprandial hyperglycemia, hyperinsulinemia, and hypertriglyceridemia [6,7,8]. Postprandial FMD was significantly lower in patients with diabetes and CVD compared to those with diabetes but no CVD [9]. Importantly, an intervention that increased FMD reduced the incidence of CVD [3].
Imeglimin is a first-in-class novel oral hypoglycemic agent (OHA) that improves pancreatic β-cell function and enhances insulin action in the liver and skeletal muscle [10]. Imeglimin improves both insulin resistance and glucose-stimulated insulin secretion by activating transient receptor potential melastatin 2 (TRPM2) [11], which lowers both fasting and postprandial glucose levels for a full day [12,13,14]. A previous report showed that imeglimin prevented hyperglycemia-induced cell death in human endothelial cells [15]. At the cellular molecular level, imeglimin modulates mitochondrial function by reducing reactive oxygen species (ROS) [10]. Excess ROS due to hyperglycemia injures endothelial cells, leading to micro- and macroangiopathy [16]. Sodium–glucose cotransporter 2 (SGLT2) inhibitors were reported to directly improve endothelial function by reducing ROS independently of blood glucose level [17]. In a rat model of metabolic syndrome, imeglimin reduced ROS production and increased FMD of mesenteric arteries independently of glycemic control [18].
However, the effects of imeglimin on human endothelial function are unknown. We hypothesized that imeglimin administration would improve endothelial function, and tested this hypothesis in this study. The main outcome was the change in FMD in patients with type 2 diabetes before and after imeglimin administration. Secondary outcomes were the changes in glycemic control, body composition, blood pressure, hepatic and renal function, lipid metabolism, and uric acid metabolism.
Methods
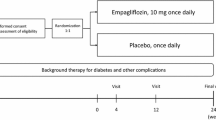
This was a prospective, single-center, observational study. The study protocol was approved by the ethics board of the University of Miyazaki (Approval No. O-1074), and it conforms to the provisions of the Declaration of Helsinki. The subjects were patients with type 2 diabetes (HbA1c ≥ 6.5%) who were aged 20 years or over and who were not receiving insulin therapy. Patients unable to take every imeglimin dose because of adverse effects were excluded from the analysis. Written informed consent was obtained from all patients, and imeglimin 2000 mg/day was initiated. None of the patients changed OHAs for at least 3 months prior to study entry, and all remained on their original OHAs until the end of the study. A meal tolerance test (MTT), endothelial function test by FMD, and atherosclerosis assessment by the cardio-ankle vascular index (CAVI) and ankle-brachial index (ABI) were performed before and 3 months after imeglimin administration. Body mass index (BMI), waist circumference, blood pressure, body composition, and blood tests for hepatic and renal function, uric acid, and cholesterol profile were assessed before and 1, 2, and 3 months after imeglimin administration. Body composition was analyzed using a multifrequency bioelectrical impedance analyzer (Inbody 720; InBody Japan, Tokyo, Japan) to measure skeletal muscle (kilograms) and body fat (kilograms). In terms of diabetic microangiopathy, diabetic retinopathy was defined as simple retinopathy or more advanced retinopathy according to the Davis classification [19]. Diabetic nephropathy was defined as nephropathy with a urinary albumin/creatinine ratio of ≥ 30 mg/g·Cr [20]. Diabetic neuropathy was defined according to the diagnostic criteria of the Toronto Diabetic Neuropathy Expert Group [21].
A commercially available test meal (Saraya, Osaka, Japan) consisting of 75.0 g glucose, 28.5 g fat, and 8.0 g protein with a total energy of 592 kcal was used for the MTT. Patients underwent a 12 h fast before the MTT, then consumed the test meal with 200 mL of water within 15 min. Blood samples were drawn at 0, 30, 60, and 120 min before and after the consumption of the test meal to measure the concentrations of plasma glucose, insulin, glucagon, and triglycerides. The areas under the curve (0–60 min, AUC60; 0–120 min, AUC120) for glucose, insulin, glucagon, and triglycerides were calculated using a brief trapezoid formulation. Glucose, insulin, glucagon, and triglyceride concentrations were determined by a commercial laboratory (SRL, Tokyo, Japan). β-cell function (HOMA2-%β), insulin resistance (HOMA2-IR), and insulin sensitivity (HOMA2-%S) were calculated using the HOMA2 calculator v2.2.3 (https://www.dtu.ox.ac.uk/homacalculator/). The insulinogenic index was measured as Δinsulin (0–30 min)/Δglucose (0–30 min), where insulin and glucose values were those at fasting and 30 min after the MTT [22].
Endothelial function was calculated by analyzing the percentage changes in the FMD increase in the brachial artery diameter using a UNEXEF38G semi-automated diagnostic ultrasound system (UNEX, Nagoya, Japan), as previously described [23]. CAVI and ABI were measured using a Vasera VS-2500 (Fukuda Denshi, Tokyo, Japan), as previously described [24].
All data are expressed as the median and interquartile range (IQR) or the average ± standard deviation (SD). We assumed that FMD increased by 2.0% after imeglimin administration, with an SD of 2.0%. A minimum sample size of 10 participants was required to detect statistical differences in FMD with a power of 80% and an α error of 5%. Data were tested for distribution using the Shapiro–Wilk normality test. Comparisons between groups were performed via paired t test, Wilcoxon signed-rank test, and two-way analysis of variance (ANOVA) with Bonferroni’s multiple comparisons test. The univariate correlation coefficient between the change in 2 h postprandial FMD before and 3 months after imeglimin administration (Δ2-hour postprandial FMD) and the change in each parameter before and after 3 months of imeglimin administration were calculated by Spearman’s rank correlation coefficient. R version 4.1.2 was used for all analyses. P < 0.05 was accepted as statistically significant.
Results
Thirteen patients were enrolled in this study and started imeglimin administration. One patient was excluded because they exhibited severe nausea and diarrhea within 2 weeks after imeglimin administration, and therefore 12 patients were finally analyzed (Table 1). The median age was 55.5 years (IQR 51.3–66.0), HbA1c was 7.2 ± 0.6%, and BMI was 32.4 kg/m2 (29.8–34.1), indicating greater obesity compared to the general Japanese population with diabetes mellitus. In terms of former diabetes treatment, six patients were OHA naïve with only diet therapy, three received dipeptidyl peptidase 4 (DPP4) inhibitor monotherapy, and two received SGLT2 inhibitor monotherapy (Table 1).
Imeglimin administration improved fasting FMD numerically but not significantly (from 6.1 [3.9–8.5] to 6.6 [3.9–9.0], p = 0.092). However, 2 h postprandial FMD was significantly improved (from 2.3 [1.9–3.4] to 2.9 [2.4–4.7], p = 0.013) (Fig. 1). Neither CAVI nor ABI changed from before to 3 months after imeglimin administration. HbA1c significantly improved 3 months after treatment (from 7.2 ± 0.6% to 6.9 ± 0.6%, p = 0.007), and BMI, waist circumference, blood pressure, skeletal muscle mass, body fat mass, and blood tests for hepatic and renal function, uric acid, and cholesterol profile was not changed by imeglimin initiation. The MTT showed that imeglimin significantly decreased fasting glucose (from 138 ± 19 mg/dL to 128 ± 20 mg/dL, p = 0.020) and 2-h postprandial glucose (from 251 ± 47 mg/dL to 215 ± 68 mg/dL, p = 0.035), while it increased fasting insulin (from 11.5 µU/mL to 19.1 µU/mL, p = 0.027) and insulin AUC60 (from 1340 µU/mL·min to 2420 µU/mL·min, p < 0.001) (Fig. 2, Table 2). Imeglimin had no effect on glucagon or triglycerides in the MTT (Fig. 2). Pre- to postprandial changes in FMD, glucose, insulin, glucagon, and triglycerides were not significantly altered by imeglimin administration (Supplementary Material S1). Δ2 h postprandial FMD was negatively correlated with Δ2 h postprandial glucose (r = − 0.653, p = 0.021) in univariate analysis (Table 3).
Among the 12 patients in this study, nine exhibited decreased 2 h postprandial glucose 3 months after imeglimin administration, while three did not. These two groups showed statistically similar Δ2 h postprandial FMD (Table 4). Regardless of whether patients had microvascular complications, imeglimin administration did not result in changes in any parameters (Supplementary Material S2 and S3).
Discussion
We showed here that imeglimin improved fasting and postprandial glucose and HbA1c. In addition, postprandial endothelial function was ameliorated by imeglimin administration. This is the first report to evaluate changes in endothelial function induced by imeglimin administration. Among OHAs, alpha-glucosidase inhibitors, glinides, DPP4 inhibitors, and SGLT2 inhibitors were previously reported to improve FMD in patients with type 2 diabetes [25,26,27,28]. Alpha-glucosidase inhibitors may increase FMD by improving postprandial hyperglycemia and dyslipidemia [25]. SGLT2 inhibitors effectively attenuated endothelial dysfunction independently of glycemic or lipid control [17]. Decreased postprandial FMD was affected by excess ROS caused by postprandial hyperglycemia, hyperinsulinemia, and hypertriglyceridemia [6,7,8]. In our study, 2 h postprandial FMD was significantly increased 3 months after imeglimin administration. Δ2 h FMD correlated with Δ2 h glucose (Table 3), suggesting that the reduction in 2 h postprandial glucose by imeglimin contributed to the postprandial improvement in FMD. On the other hand, postprandial FMD improved even in patients without decreased postprandial glucose (Table 4). These findings suggested that imeglimin exerted additional benefits on endothelial function beyond glycemic control. In rats, imeglimin improved FMD in the mesenteric artery by reducing ROS without modifying plasma glucose levels [18]. Imeglimin-induced ROS reduction might affect endothelial function independently of glycemic control.
Our study also showed that imeglimin significantly decreased 2 h postprandial glucose, but had no effect on 2 h postprandial insulin or glucagon (Fig. 2). Since imeglimin administration resulted in no significant difference in 2 h insulin but significantly increased insulin AUC60, an early postprandial increase in insulin secretion might be involved in the decrease in 2 h postprandial glucose. The early phase of glucose-induced insulin release was previously shown to be enhanced by imeglimin via the TRPM2 channel pathway [11], which is consistent with the present study.
In the assessment of atherosclerosis, there was no significant difference in CAVI or ABI before and after imeglimin initiation. FMD was reported to be more sensitive than ABI and CAVI for assessing the early phase of atherosclerosis [29, 30]. Additionally, FMD was evaluated both before and after the MTT, which may have captured the improved postprandial endothelial function associated with imeglimin administration.
The limitations of our study are as follows. First, this was a single-center study with a short observation period, and only a small number of Japanese patients were enrolled, with no placebo group. However, this study was able to identify an improvement in FMD despite the short 3-month duration of imeglimin administration. The results suggest that even brief treatment with imeglimin improves endothelial function. Second, this study included a population of patients with a relatively short history of diabetes mellitus (median 6.0 years) and only mild atherosclerosis. The effect of imeglimin on severe endothelial dysfunction and atherosclerosis could not be evaluated. Third, the study did not assess the direct effect of imeglimin on ROS. However, our data indicated that the improvement in FMD following imeglimin administration was not achieved solely by tightening glycemic control. Further studies are needed to better characterize the ability of imeglimin to improve endothelial function.
Conclusions
In the present study, 2 h postprandial FMD in patients with diabetes was ameliorated by 3 months of imeglimin administration. Imeglimin may have improved postprandial FMD by lowering postprandial glucose and influencing factors other than glycemic control. These effects may have a favorable impact on CVD in patients with type 2 diabetes.
References
Pyörälä K, Laakso M, Uusitupa M. Diabetes and atherosclerosis: an epidemiologic view. Diabetes Metab Rev. 1987;3(2):463–524. https://doi.org/10.1002/dmr.5610030206.
Creager MA, Lüscher TF, Cosentino F, Beckman JA. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part I. Circulation. 2003;108(12):1527–32. https://doi.org/10.1161/01.CIR.0000091257.27563.32.
Thijssen DHJ, Bruno RM, van Mil ACCM, et al. Expert consensus and evidence-based recommendations for the assessment of flow-mediated dilation in humans. Eur Heart J. 2019;40(30):2534–47. https://doi.org/10.1093/eurheartj/ehz350.
Ludmer PL, Selwyn AP, Shook TL, et al. Paradoxical vasoconstriction induced by acetylcholine in atherosclerotic coronary arteries. N Engl J Med. 1986;315(17):1046–51. https://doi.org/10.1056/NEJM198610233151702.
Henry RM, Ferreira I, Kostense PJ, et al. Type 2 diabetes is associated with impaired endothelium-dependent, flow-mediated dilation, but impaired glucose metabolism is not. Hoorn Study Atherosclerosis. 2004;174(1):49–56. https://doi.org/10.1016/j.atherosclerosis.2004.01.002.
Kawano H, Motoyama T, Hirashima O, et al. Hyperglycemia rapidly suppresses flow-mediated endothelium-dependent vasodilation of brachial artery. J Am Coll Cardiol. 1999;34(1):146–54. https://doi.org/10.1016/s0735-1097(99)00168-0.
Suzuki K, Watanabe K, Futami-Suda S, et al. The effects of postprandial glucose and insulin levels on postprandial endothelial function in subjects with normal glucose tolerance. Cardiovasc Diabetol. 2012;11:98. https://doi.org/10.1186/1475-2840-11-98.
Bae JH, Bassenge E, Kim KB, et al. Postprandial hypertriglyceridemia impairs endothelial function by enhanced oxidant stress. Atherosclerosis. 2001;155(2):517–23. https://doi.org/10.1016/s0021-9150(00)00601-8.
Kumar V, Jain N, Raizada N, et al. Postprandial endothelial dysfunction and CIMT after oral fat challenge in patients with type 2 diabetes mellitus with and without macrovascular disease—a preliminary study. Diabetes Metab Syndr. 2021;15(6):102317. https://doi.org/10.1016/j.dsx.2021.102317.
Hallakou-Bozec S, Vial G, Kergoat M, et al. Mechanism of action of imeglimin: a novel therapeutic agent for type 2 diabetes. Diabetes Obes Metab. 2021;23(3):664–73. https://doi.org/10.1111/dom.14277.
Funazaki S, Yoshida M, Yamada H, et al. A novel mechanism of imeglimin-mediated insulin secretion via the cADPR-TRP channel pathway. J Diabetes Investig. 2022;13(1):34–41. https://doi.org/10.1111/jdi.13669.
Dubourg J, Fouqueray P, Thang C, Grouin JM, Ueki K. Efficacy and safety of imeglimin monotherapy versus placebo in Japanese patients with type 2 diabetes (TIMES 1): a double-blind, randomized, placebo-controlled, parallel-group, multicenter phase 3 trial. Diabetes Care. 2021;44(4):952–9. https://doi.org/10.2337/dc20-0763.
Pacini G, Mari A, Fouqueray P, Bolze S, Roden M. Imeglimin increases glucose-dependent insulin secretion and improves β-cell function in patients with type 2 diabetes. Diabetes Obes Metab. 2015;17(6):541–5. https://doi.org/10.1111/dom.12452.
Oda T, Satoh M, Nagasawa K, et al. The effects of imeglimin on the daily glycemic profile evaluated by intermittently scanned continuous glucose monitoring: retrospective, single-center. Observational Study Diabetes Ther. 2022;13(9):1635–43. https://doi.org/10.1007/s13300-022-01298-w.
Detaille D, Vial G, Borel AL, Cottet-Rouselle C, et al. Imeglimin prevents human endothelial cell death by inhibiting mitochondrial permeability transition without inhibiting mitochondrial respiration. Cell Death Discovery. 2016;2(1):15072. https://doi.org/10.1038/cddiscovery.2015.72.
Chawla A, Chawla R, Jaggi S. Microvasular and macrovascular complications in diabetes mellitus: distinct or continuum? Indian J Endocrinol Metab. 2016;20(4):546–51. https://doi.org/10.4103/2230-8210.183480.
Alshnbari AS, Millar SA, O’Sullivan SE, Idris I. Effect of sodium-glucose cotransporter-2 inhibitors on endothelial function: a systematic review of preclinical studies. Diabetes Ther. 2020;11(9):1947–63. https://doi.org/10.1007/s13300-020-00885-z.
Lachaux M, Soulié M, Hamzaoui M, et al. Short-and long-term administration of imeglimin counters cardiorenal dysfunction in a rat model of metabolic syndrome. Endocrinol Diabetes Metab. 2020;3(3):e00128. https://doi.org/10.1002/edm2.128.
Davis MD. Vitreous contraction in proliferative diabetic retinopathy. Arch Ophthalmol. 1965;74(6):741–51. https://doi.org/10.1001/archopht.1965.00970040743003.
Stevens PE, Levin A, Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158(11):825–30.
Tesfaye S, Boulton AJ, Dyck PJ, et al. Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care. 2010;33(10):2285–93. https://doi.org/10.2337/dc10-1303.
Goedecke JH, Dave JA, Faulenbach MV, et al. Insulin response in relation to insulin sensitivity: an appropriate beta-cell response in black South African women. Diabetes Care. 2009;32(5):860–5. https://doi.org/10.2337/dc08-2048.
Morimoto S, Yurugi T, Aota Y, et al. Prognostic significance of ankle-brachial index, brachial-ankle pulse wave velocity, flow-mediated dilation, and nitroglycerin-mediated dilation in end-stage renal disease. Am J Nephrol. 2009;30(1):55–63. https://doi.org/10.1159/000201416.
Shirai K, Utino J, Otsuka K, Takata M. A novel blood pressure-independent arterial wall stiffness parameter; cardio-ankle vascular index (CAVI). J Atheroscler Thromb. 2006;13(2):101–7. https://doi.org/10.5551/jat.13.101.
Sawada T, Shiotani H, Terashita D, et al. Comparison of effects of α-glucosidase inhibitors and glinide drugs on endothelial dysfunction in diabetic patients with coronary artery disease. Circ J. 2014;78(1):248–55. https://doi.org/10.1253/circj.cj-13-0918.
Nakamura K, Oe H, Kihara H, et al. DPP-4 inhibitor and alpha-glucosidase inhibitor equally improve endothelial function in patients with type 2 diabetes: EDGE study. Cardiovasc Diabetol. 2014;13:110. https://doi.org/10.1186/s12933-014-0110-2.
Kato T, Inoue T, Node K. Postprandial endothelial dysfunction in subjects with new-onset type 2 diabetes: an acarbose and nateglinide comparative study. Cardiovasc Diabetol. 2010;9:12. https://doi.org/10.1186/1475-2840-9-12.
Sakai T, Miura S. Effects of sodium-glucose cotransporter 2 inhibitor on vascular endothelial and diastolic function in heart failure with preserved ejection fraction—novel prospective cohort study. Circ Rep. 2019;1(7):286–95. https://doi.org/10.1253/circrep.CR-19-0018.
Tachibana H, Washida K, Kowa H, Kanda F, Toda T. Vascular function in Alzheimer’s disease and vascular dementia. Am J Alzheimers Dis Other Demen. 2016;31(5):437–42. https://doi.org/10.1177/1533317516653820.
Watanabe D, Morimoto S, Morishima N, Ichihara A. Clinical impacts of endothelium-dependent flow-mediated vasodilation assessment on primary aldosteronism. Endocr Connect. 2021;10(6):578–87. https://doi.org/10.1530/EC-21-0057.
Acknowledgements
We thank the participants of the study.
Funding
This research was partially supported by Saraya Co., Ltd. The Rapid Service Fee was funded by the authors. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and the accuracy of the data analysis.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Taisuke Uchida: data acquisition; study conceptualization; data curation; formal analysis; investigation; methodology; writing – original draft. Hiroaki Ueno: supervision; validation; writing – review and editing. Norifumi Taniguchi: data acquisition; writing – review and editing. Fumiko Kogo: data acquisition; writing – review and editing. Yuma Nagatomo: data acquisition; writing – review and editing. Koichiro Shimizu: data acquisition; writing – review and editing. Tomomi Shiiya: data acquisition; writing – review and editing. Hideki Yamaguchi: supervision; writing – review and editing. Kazuya Shimoda: project administration; supervision; validation; writing – review and editing. All authors have approved the submitted version of the manuscript and have agreed to be accountable for all parts of the work.
Disclosures
Hiroaki Ueno has received a scholarship donation from Saraya Co., Ltd. Ayaka Konagata, Norifumi Taniguchi, Fumiko Kogo, Yuma Nagatomo, Koichiro Shimizu, Hideki Yamaguchi, and Kazuya Shimoda declare that they have no competing interests in connection with the submitted material.
Compliance with Ethics Guidelines
The protocol for this research project was approved by the ethics board of the University of Miyazaki (Approval No. O-1074), and it conforms to the provisions of the Declaration of Helsinki. This research was registered in the University Hospital Medical Information Network (UMIN, UMIN000046311). Informed consent was obtained from all subjects.
Data Availability
The data sets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Uchida, T., Ueno, H., Konagata, A. et al. Improving the Effects of Imeglimin on Endothelial Function: A Prospective, Single-Center, Observational Study. Diabetes Ther 14, 569–579 (2023). https://doi.org/10.1007/s13300-023-01370-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-023-01370-z