Abstract
Introduction
In this ORION study subgroup analysis, the safety and effectiveness of insulin glargine 300 U/mL (Gla-300) was evaluated in people from the South Asia region with type 2 diabetes mellitus (T2DM) before, during, and after Ramadan, in a real-world setting.
Methods
The ORION study was a real-world, prospective, observational, non-comparative study conducted across 11 countries. The current subgroup analysis included participants from the South Asia region (India and Pakistan) who fasted during Ramadan. The primary endpoint was the percentage of participants experiencing ≥ 1 event of severe and/or symptomatic documented hypoglycemia with self-monitored plasma glucose (SMPG) ≤ 70 mg/dL during Ramadan. Secondary endpoints analyzed were changes in glycated hemoglobin (HbA1c), fasting plasma glucose (FPG), SMPG, insulin dose, and adverse events (AEs).
Results
This subgroup analysis included 106 participants from the South Asia region with mean (standard deviation) age of 51.3 (10.9) years and mean number of 29.8 (4.0) fasting days. The number of severe and/or symptomatic documented hypoglycemia events was low in the pre-Ramadan (SMPG ≤ 70 mg/dL: 1 event [0.9%]; SMPG < 54 mg/dL: 1 event [0.9%]) and Ramadan periods (SMPG ≤ 70 mg/dL: 1 event [0.9%]; SMPG < 54 mg/dL: 0 events), and none in the post-Ramadan period. One participant reported severe hypoglycemia (any time of the day: nocturnal or daytime) throughout the pre-Ramadan period. A reduction in HbA1c and FPG levels was seen during the pre- to post-Ramadan period; however, a slight increase in SMPG levels was reported during this same period. Gla-300 daily dose was reduced from 21.6 (9.6) U to 20.2 (8.9) U during the pre-Ramadan to Ramadan period. The incidence of AEs was 1.9%.
Conclusions
The real-world data from the ORION study indicate that Gla-300 is effective, with low risk of hypoglycemia, for the management of T2DM during Ramadan in the South Asian population.
Trial Registration
CTRI/2019/02/017636.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Islam is the second largest religion in South Asia, with approximately 600 million Muslims living in this region, representing about one third of the population of South Asia. |
Muslim people with type 2 diabetes mellitus (T2DM) who choose to fast during the holy month of Ramadan are at risk of hypoglycemia. |
This subgroup analysis of the real-world ORION study, conducted in participants with T2DM from India and Pakistant who fasted during Ramadan, assessed the safety and effectiveness of insulin glargine 300 U/mL (Gla-300) during the pre-Ramadan, Ramadan, and post-Ramadan periods. |
What was learned from this study? |
The incidence of severe and/or symptomatic hypoglycemia in this South Asian subpopulation was low, with no severe hypoglycemic events reported during Ramadan. |
A reduction in glycated hemoglobin levels was also observed during the pre-Ramadan to post-Ramadan period, indicating a clinical improvement. |
Introduction
Ramadan fasting is widely observed by Muslims all over the world [1, 2]. It is characterized by religious fasting from dawn until sunset during the ninth month of the Islamic Lunar calendar [3, 4]. Globally, more than 50 million Muslims with diabetes fast during the holy month of Ramadan each year [5, 6]. South Asia has the largest population of Muslims in the world. Studies that included Indian cohorts showed that about 79–94% of Muslims with type 2 diabetes mellitus (T2DM) fasted for at least 15 days during Ramadan [7, 8]. Moreover, in Pakistan, which has a predominantly Islamic population, the overall weighted prevalence of diabetes was 26.3% in 2016–2017 [9]. Taken together, it can be concluded that a large percentage of people with diabetes from India and Pakistan partake in fasting during Ramadan. Further, in the Indian subcontinent, the average daily duration of Ramadan fasting is 14–15 h [10]. Additionally, Ramadan meals tend to be rich in carbohydrates and saturated oils, which may further impact glycemic excursions during this period. Hence, the insulin taken during Ramadan should be effective and have a low risk of hypoglycemia and weight gain [11].
The International Diabetes Federation and Diabetes and Ramadan International Alliance (IDF-DAR) guidelines describe three risk factors, including hypoglycemia, hyperglycemia, and diabetic ketoacidosis, based on clinical experience, to determine an individual patient’s risk of potential complications during fasting throughout Ramadan [12]. In the CREED study, logistic regression analysis indicated that individuals who had at least one episode of hypoglycemia before Ramadan had a 7.8-fold higer risk of experiencing a subsequent hypoglycemic episode during Ramadan compared with those who had no prior episodes. The same study also indicated that Asian individuals with T2DM were 12-fold more likely to have a hypoglycemic episode during Ramadan if they had an episode before Ramadan. This observation suggests that although population-wide hypoglycemia is managed well during Ramadan, Asians may be at an increased risk due to ethnic differences [13]. Further, the DAR-Middle East and North Africa (MENA) research also found that confirmed hypoglycemia and severe hypoglycemia increased significantly during Ramadan compared with 4 weeks before Ramadan [14].
The second-generation basal insulin analogs, such as insulin glargine 300 U/mL (Gla-300), provide physicians with new treatment options to achieve targeted glycemic control. While providing similar efficacy in lowering glycated hemoglobin (HbA1c) as first-generation insulin analogs, Gla-300 has additional clinical benefits, including a more stable, long duration of action that enables once-daily administration with flexibility in daily injection time, together with a lower risk of hypoglycemia [15]. However, research on the clinical aspects of the second-generation basal insulin analogs in people with T2DM who fast throughout Ramadan is lacking. The real-world ORION study evaluated the safety and effectiveness of Gla-300 treatment in people with T2DM who fasted during Ramadan. The results showed that Gla-300 treatment during Ramadan was associated with a low incidence of hypoglycemia and improved glycemic control [16]. The current subgroup analysis of the ORION study focuses on the safety and effectiveness of Gla-300 in people with T2DM from the South Asia region who fasted during Ramadan.
Methods
Details of the study design (Electronic Supplementary Material [ESM] Fig. S1) have previously been published [16]. Key methodological details are presented in the following subsections.
Study Design
The ORION study was an international, prospective, real-world study conducted across 64 centers in 11 countries in participants with T2DM treated with Gla-300 who fasted during Ramadan. This study was conducted in accordance with the guidelines for Good Epidemiology Practice and the Declaration of Helsinki of 1964 and subsequent amendments, and the study is registered with the World Health Organization International Clinical Trials Registry Platform registration number CTRI/2019/02/017636. The ORION study protocol was reviewed and approved by the Institutional Review Board/Institutional Ethics Committee in accordance with the local regulations in each participating country/study center. All participants provided written informed consent. The study was conducted in 2019, with the Ramadan fast occurring between 5 May and 4 June. This subgroup analysis included participants from India and Pakistan, henceforth collectively referred as participants from South Asia.
Participants who had Gla-300 treatment prescribed as per routine clinical practice visited the study centers at three time points, including the recruitment period (in the 3-month period prior to Ramadan), the pre-Ramadan period (1–3 months prior to Ramadan), and the post-Ramadan period (1 month after Ramadan) [16]; dose adjustments during Ramadan were made based on the advice of the treating physician, guidance by IDF-DAR recommendations, and individual patient characteristics [12]. Likewise, hypoglycemia and adverse events (AEs) occurring 1 month after the end of Ramadan were recorded if the patient visit was made > 1 month after Ramadan. Diaries completed by participants containing information on glucose values, basal insulin doses, episodes of symptomatic hypoglycemia, and days with/without fasting were also recorded.
Participants
The ORION study included adult participants (aged ≥ 18 years) with T2DM who were on basal insulin therapy with Gla-300 for ≥ 8 weeks and who were expected to continue Gla-300 treatment and fast for ≥ 15 days during Ramadan. Participants reporting hypersensitivity/intolerance to Gla-300 (or its excipients) and women who were pregnant or breastfeeding were excluded from the study. Additionally, participants who had used basal–bolus or premix insulin within 6 months or any other investigational medication within 1 month or five half-lives prior to the selection visit were also excluded.
Study Endpoints
The primary objective of the study was to assess the percentage of participants who had experienced ≥ 1 episode of severe and/or symptomatic documented hypoglycemia with self-monitored plasma glucose (SMPG) ≤ 70 mg/dL during the Ramadan period. The secondary endpoints of the study were the incidence of severe and/or symptomatic hypoglycemia with SMPG < 54 mg/dL and event rates of severe and/or symptomatic documented hypoglycemia (SMPG ≤ 70 mg/dL and < 54 mg/dL, respectively) across the three time periods. Symptomatic hypoglycemia events were assessed as per the American Diabetes Association (ADA) classification and analyzed by time of occurrence: daytime (06:00 a.m. to 11:59 p.m.) and nocturnal (12:00 a.m. to 05:59 a.m.) during the pre- and post-Ramadan periods, as well as fasting (between Suhur and Iftar) and non-fasting (between Iftar and Suhur) periods during Ramadan. The secondary endpoints analyzed in the study were mean changes in HbA1c, fasting plasma glucose (FPG), fasting SMPG, insulin dose, and body weight, assessed during the pre- and post-Ramadan periods, and mean fasting SMPG before Iftar (evening meal; during Ramadan). AEs and serious AEs were also recorded throughout the study.
Data Collection and Statistical Analyses
This subgroup analysis evaluated the primary and secondary endpoints in eligible participants from the South Asia region. Data for the ORION study were collected at the recruitment visits, i.e., during the pre-Ramadan (defined as 1–3 months prior to Ramadan), Ramadan, and post-Ramadan (1 month after Ramadan) periods. The primary endpoint of the number of participants with ≥ 1 severe and/or symptomatic documented hypoglycemia (SMPG ≤ 70 mg/dL) was reported with the two-sided 95% confidence interval (CI) for the percentage of participants. The secondary endpoint of percentage of participants with ≥ 1 severe and/or symptomatic documented hypoglycemia (SMPG < 54 mg/dL), across the three periods, was analyzed similar to primary endpoint. The event rates of severe and/or symptomatic hypoglycemia with SMPG ≤ 70 mg/dL and < 54 mg/dL, respectively, were analyzed during the pre-Ramadan (1–3 months), Ramadan (1 month), and post-Ramadan (1–2 months) periods. Data were summarized using descriptive statistics.
Results
Patient Demographics and Baseline Characteristics
A total of 502 participants were included in the ORION study, among whom 106 participants from the South Asia region (India, n = 73; Pakistan, n = 33) were considered for inclusion in the current subgroup analysis.
At baseline, the participants’ mean (standard deviation [SD]) age was 51.3 (10.9) years, and 54.7% of participants were female (Table 1). The mean (SD) body mass index (BMI) was 29.1 (5.4) kg/m2, and 79 (75.2%) participants had a BMI of ≥ 25 kg/m2. The mean (SD) duration of diabetes was 7.9 (5.1) years, and age of onset of diabetes in this population was 43.5 (10.1) years. The majority of participants in this subgroup analysis were recent insulin users (median [quartile 1: quartile 3] 0.9 [0.2: 2.0] years), with a mean (SD) Gla-300 treatment duration of 4.7 (3.0) months, whereas Gla-300 treatment duration was < 6 months for 78 (73.6%) participants. More than half of the participants (52.8%) had received any insulin treatment for the first time only within 1 year, whereas the mean (SD) time elapsed since participants first received any non-insulin antidiabetic treatment was 7.2 (4.7) years. During the pre-Ramadan period, recommendations for Gla-300 dose adjustments were provided, which were every week for 59 (55.7%) participants and more frequent (every 1–6 days) for 47 (44.3%) participants. The dose increment of 2 U per adjustment was recommended for (95 [89.6%]) participants. No participant from the subgroup analysis had diabetic ketoacidosis within 3 months prior to Ramadan. The mean (SD) individualized HbA1c target was 6.9% (0.3%) (52.3 (3.7) mmol/mol), and only nine (10.0%) participants were at target during the pre-Ramadan period. The majority (101 [95.3%]) of the participants were considered to have moderate/low risk of complications when fasting, as determined by their physician. During the pre-Ramadan period, a high number (52 [49.1%]) of participants were treated with > 2 non-insulin antidiabetic treatments, with the most common being sulfonylureas (71 [67.0%]) (Table 2).
Most (86 [81.9%]) participants fasted for the entire Ramadan period, with a mean (SD) of 29.8 (4.0) fasting days. Nineteen (18.1%) participants broke their fast during Ramadan, among whom six (31.6%) had menses, five (26.3%) were traveling, three (15.8%) had hypoglycemia, one (5.3%) due to illness, and four (21.1%) participants broke the fast due to other reasons. Also, among these 19 participants, 13 (12.4%) fasted for > 25 days but had at least a 1-day break from fasting. The recommended timing for Gla-300 dose injection was in the evening (at Iftar) for 102 (97.1%) participants; all of these 102 participants complied with this recommendation. Most (94 [89.5%]) participants reported full adherence to daily treatment (i.e., Gla-300 was administered every day during the Ramadan period).
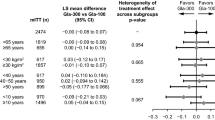
Severe and/or Symptomatic Documented Hypoglycemia
Overall, the number of participants experiencing ≥ 1 event of severe and/or symptomatic documented hypoglycemia with SMPG ≤ 70 mg/dL after taking Gla-300 during the study period (pre-Ramadan, Ramadan, and post-Ramadan) was low, i.e., one (0.9%) participant each during the pre-Ramadan and Ramadan periods and no participant during the post-Ramadan period (Fig. 1; ESM Table S1). No participants had reported severe hypoglycemia during the Ramadan and post-Ramadan periods. No symptomatic documented hypoglycemia with SMPG < 54 mg/dL was reported during the Ramadan or post-Ramadan periods. However, during the pre-Ramadan period, one (0.9%) participant reported symptomatic documented hypoglycemia with SMPG < 54 mg/dL. Further, in the last month of the pre-Ramadan period, none of the participant reported symptomatic documented hypoglycemia with SMPG < 54 mg/dL. During the entire study duration, only one participant from the South Asia group reported severe hypoglycemia (any time of the day: nocturnal or daytime) during the whole pre-Ramadan period.
Changes in glycemic Endpoints (HbA1c, FPG, and SMPG)
The mean (SD) HbA1c value was 8.18% (1.05%) [65.9 (11.5) mmol/mol] in the pre-Ramadan period, and a decrease in mean (SD) HbA1c values (7.78% (0.95%) [61.6 (10.4) mmol/mol] was noted in the pre- to post-Ramadan period. The mean (SD) change was −0.37% (0.88%) [−4.1 (9.6) mmol/mol]) (Fig. 2a).
The mean (SD) FPG also decreased from 130.2 (33.3) mg/dL [7.23 (1.85) mmol/mol] to 115.5 (28.4) mg/dL [6.41 (1.58) mmol/mol] during the pre-Ramadan to the post-Ramadan period; the mean (SD) change was −13.2 (43.3) mg/dL [−0.73 (2.40) mmol/mol] (Fig. 2b). There was a slight increase in mean (SD) fasting SMPG from 116.5 (19.0) mg/dL [6.47 (1.05) mmol/mol] to 119.8 (17.7) mg/dL [6.65 (0.99) mmol/mol] during the pre-Ramadan to post-Ramadan period; the mean (SD) change was 3.7 (20.6) mg/dL [0.21 (1.14) mmol/mol] (Fig. 2c).
Change in Insulin Dose
The mean (SD) daily dose of Gla-300 during the pre-Ramadan period, 21.6 (9.6) U (0.28 ± 0.12 U/kg), fell to 20.2 (8.9) U (0.27 ± 0.11 U/kg) during the Ramadan period; the mean (SD) change noted was −1.30 (3.25) U [−0.017 (0.04) U/kg] (Fig. 2d). A relative reduction in the Gla-300 dose of > 15% in the pre-Ramadan to Ramadan period was seen in a total of 27 (25.8%) participants. The mean (SD) daily dose of Gla-300 was 21.9 (9.8) U [0.290 (0.12) U/kg] during the post-Ramadan period, with a change of 0.39 (3.59) U [0.005 (0.05) U/kg] from the pre-Ramadan to post-Ramadan period. The relative change during the pre-Ramadan to Ramadan period was −0.049 (0.15) U [−0.050 (0.15) U/kg] and during the pre-Ramadan to post-Ramadan period 0.032 (0.18) U [0.032 (0.18) U/kg].
Change in Body Weight
A marginal difference in mean (SD) body weight was observed from the pre-Ramadan period to the post-Ramadan period, 76.5 (14.2) kg to 76.0 (13.9) kg, respectively; i.e., a change of −0.5 (2.3) kg.
Adverse Events
Two (1.9%) participants reported AEs from the South Asia group during the study period; however, no participant reported a serious AE from this group. Of the two participants who reported an AE, one (0.9%) participant reported AE of hyperglycemia whereas the other (0.9%) participant who reported AE related to Gla-300, the AE was due to accidental overdose of Gla-300 which did not occur during Ramadan period and had not resulted in discontinuation of the study treatment. There were no deaths during the study period (Table 3).
Discussion
This subgroup analysis of the ORION study including 106 Muslim participants from the South Asia region showed that Gla-300 had a favorable safety profile and improved glycemic control during Ramadan fasting in a real-world setting. In addition, few hypoglycemic events were reported by these participants during the study period, and none were severe.
The participants from the South Asia region included in this subgroup analysis were relatively younger and had a lower mean BMI (29 kg/m2) than the global ORION study population, and also included a high proportion (95.3%) of people who were in the IDF-DAR moderated-/low-risk category. This finding was similar to that reported by the DIA-RAMADAN study in a population from the Indian subcontinent [17]. In addition, in the current subgroup analysis, the majority (81.9%) of participants fasted during the entire Ramadan period, the mean diabetes duration was 7.9 years, and a few (10.0%) participants were at their HbA1c target in the pre-Ramadan period. However, these findings are in contrast with those reported for the ORION global study population, namely, a longer duration of diabetes in participants (10.7 years) and a greater percentage (15.3%) of participants at their HbA1c target level. Additionally, in comparison with the overall ORION study population, the participants from South Asia had fewer comorbidities (38.9 vs. 32.1%) [16].
The reported percentage of severe and/or symptomatic documented hypoglycemia with SMPG ≤ 70 mg/dL threshold was low before and during Ramadan, while no such event was reported after Ramadan, and no severe and/or symptomatic hypoglycemia with an SMPG < 54 mg/dL was reported during the Ramadan or post-Ramadan periods. These findings are very encouraging, given that at study initiation about 49.1% of participants were treated with > 2 concomitant non-insulin medications and 67.0% of participants were treated with sulfonylureas. Moreover, these findings echo the findings from other randomized controlled trials (RCTs) and real-world studies of Gla-300. The EDITION 1 and EDITION 2 RCTs compared Gla-300 with Gla-100 in people with T2DM and reported a significantly lower percentage of participants with severe or confirmed hypoglycemic (≤ 3.9 mmol/mol [≤ 70 mg/dL]) events at month 6 with Gla-300 than with Gla-100 [18, 19]. Further, a low incidence of documented symptomatic hypoglycemia was reported in the real-world ATOS study, which evaluated the effectiveness and safety of Gla-300 in insulin-naïve people with T2DM from five different regions of the world, including Asia [20]. Moreover, both the RCTs and the real-world study were conducted in non-fasting patients (not Ramadan specific).
Changes in glycemic parameters, such as HbA1c, FPG, and fasting SMPG levels, from the pre-Ramadan to post-Ramadan period in participants from the South Asia region were similar to those observed in the overall study population [16]. Additionally, considering the short duration of the ORION study, the reduction in HbA1c of 0.4% in the participants from South Asia over a period of 3 months is noteworthy; however, fasting per se may have contributed to the reduction in HbA1c [4, 16, 17]. Also, the analysis of the participants from South Asia showed a divergence with respect to FPG and SMPG. Baseline FPG was lower in the South Asian population in the present subgroup analysis than in the overall ORION study population (close to target FPG of 130 mg/dL) and decreased substantially post-Ramadan. For SMPG, although a numerical increase was observed in the current subgroup analysis, the starting SMPG levels were lower than that in the overall ORION study population, and despite the increase, the SMPG level remained within the target range.
The IDF-DAR guidelines recommend that people with T2DM who are at “high risk” should not fast during Ramadan [12]. This recommendation was not strictly adhered to, as 4.7% of participants from the South Asia region in the ORION study (which specifically recruited participants who intended to fast during Ramadan) were at high risk, Furthermore, 101 (95.3%) participants from this region were in the moderate-/low-risk category.
During Ramadan, Gla-300 injections were recommended at Iftar, as per the DAR recommendations for basal insulins [12]. In this present subgroup analysis, 97.1% of participants complied with this recommendation. Studies investigating the effects of fasting during Ramadan have also found that high (> 8%) HbA1c levels in the pre-Ramadan period are common [3, 21]. A reduced (15–30%) insulin dose is also advised during Ramadan [12]; in the present analysis, approximately one-quarter of participants reduced their Gla-300 dose by > 15%. The low percentage of participants implementing a Gla-300 dose change may be due to the Gla-300 dose generally being low in the pre-Ramadan period and a large proportion (81.3%) of participants not being at their individualized HbA1c target.
In the EDITION 2 RCT, Gla-300 treatment was associated with decreased body weight during the first 12 weeks of treatment [19]. This finding is consistent with the results from the current subgroup analysis showing a small mean (SD) reduction of − 0.5 (2.3) kg in body weight in participants from the pre-Ramadan to the post-Ramadan period, similar to the findings of global study [16].
This subgroup analysis of the ORION study focused on participants from the South Asia region, and the results add to the current body of evidence on the management of T2DM in Muslim individuals from this region who choose to fast during Ramadan. The safety and effectiveness results observed in this subgroup analysis are consistent with the results previously reported in the global analysis [16].
In the real-world CREED study, most participants were treated with oral anti-hyperglycemic drugs, and only 5% of participants received insulin alone [13]. Likewise, in another real-world evidence study, DAR-MENA, of the 57.3% of participants who fasted during Ramadan, only one-third were treated with insulin [14]. In contrast, in the current subgroup analysis of participants in the ORION study from the South Asia region, a higher percentage (81.9%) of participants fasted during Ramadan; all received insulin, with concomitant antidiabetic non-insulin medication received by 97.2% of participants. It is worth noting that, despite the CREED and DAR-MENA studies having a lower proportion of participants who received insulin compared with the population in the current subgroup analysis, both of the former studies reported a higher incidence of hypoglycemia than found in the current analysis. In the CREED study, 8.8% of participants experienced hypoglycemia throughout the study period, whereas in the DAR-MENA study, the incidence of hypoglycemic events was 4.4% before Ramadan and 10.4% during the Ramadan period. The incidence of hypoglycemia reported in the current subgroup analysis of participants receiving Gla-300 was much lower than that in the global ORION study, i.e., 0.9% versus 2.2% pre-Ramadan, 0.9% versus 2.6% during Ramadan, and 0% versus 0.2% post-Ramadan, indicating a very low incidence of hypoglycemia in this population. This lower risk of hypoglycemia observed in the ORION study population and specifically in the South Asian participants in the present subgroup analysis may have enabled the maximum number of participants to fast for the entire duration of Ramadan. One of the possible reasons for the lower incidence of hypoglycemia in this subgroup analysis of ORION study could be due to all individuals in this analysis receiving Gla-300. In a meta-analysis evaluating Gla-300 versus Gla-100 in participants with T2DM, the results showed that Gla-300 offers equivalent glycemic control with fewer hypoglycemic events than Gla-100 [22]. On the contrary, both the CREED and DAR-MENA studies may have included first-generation insulins or intermediate-acting insulins in the study, as the insulin type studied in these both studies was not specified [13, 14].
Overall, this subgroup analysis of participants from the South Asia region who were included in the ORION study, provides important clinical evidence for the effectiveness and safety of Gla-300 in people with T2DM who chose to fast during Ramadan. The finding that most study participants fasted for almost the entire month of Ramadan further adds to the relevance of the study. However, the ORION study and, hence, this subgroup analysis have a number of limitations. It should be noted that only those participants who intended to fast for ≥ 15 days during the Ramadan period were included in the study. Also, the included population may be representative of people with T2DM who believed they were well enough to fast for the entire month of Ramadan. Thus, the observed results may not be reflective of people with more severe illness and should be interpreted with caution. In addition, the majority of participants in the study fell into the moderate/low category of complications when fasting, according to IDF-DAR guidelines [12]; hence, these data may not fully reflect the safety of Gla-300 in a high-risk population as categorized by IDF-DAR guidelines. Other inherent limitations include the lack of randomization to control for unknown confounders and the lack of a comparator arm, which is required for comparison; in the current study, comparison is done only with participant baseline data, which is reflective of the real nature of observational study.
Conclusion
In the current subgroup analysis of the ORION study, which enrolled those participants with T2DM from the South Asia region who were treated with Gla-300 and fasted during the Ramadan, there were few reported symptomatic hypoglycemic events, of which none were severe, and glycemic control also improved. The majority of the participants treated with Gla-300 were able to complete ≥ 25 days of fasting during the month of Ramadan. Hence, Gla-300 could be an appropriate treatment option for people with T2DM who plan to fast during Ramadan and are in need of a basal insulin for managing their diabetes. These results will enable physicians to better manage people with diabetes who choose to fast during Ramadan and could help frame future guidelines for managing T2DM in patients who fast for cultural or religious reasons.
References
Trepanowski JF, Bloomer RJ. The impact of religious fasting on human health. Nutr J. 2010;9:57.
Ahmed WN, Arun CS, Koshy TG, et al. Management of diabetes during fasting and COVID-19—challenges and solutions. J Family Med Prim Care. 2020;9:3797–806.
Hassanein M, Al-Arouj M, Hamdy O, et al. Diabetes and Ramadan: practical guidelines. Diabetes Res Clin Pract. 2017;126:303–16.
Jaleel MA, Raza SA, Fathima FN, et al. Ramadan and diabetes: as-Saum (the fasting). Indian J Endocrinol Metab. 2011;15:268–73.
Azizi F. Islamic fasting and health. Ann Nutr Metab. 2010;56:273–82.
Al-Arouj M, Assaad-Khalil S, Buse J, et al. Recommendations for management of diabetes during Ramadan: update 2010. Diabetes Care. 2010;33:1895–902.
Babineaux SM, Toaima D, Boye KS, et al. Multi-country retrospective observational study of the management and outcomes of patients with Type 2 diabetes during Ramadan in 2010 (CREED). Diabet Med. 2015;32:819–28.
Salti I, Bénard E, Detournay B, et al. A Population-based study of diabetes and its characteristics during the fasting month of Ramadan in 13 countries results of the Epidemiology of Diabetes and Ramadan 1422/2001 (EPIDIAR) study. Diabetes Care. 2004;27:2306–11.
Basit A, Fawwad A, Qureshi H, Shera AS; NDSP Members. Prevalence of diabetes, pre-diabetes and associated risk factors: second National Diabetes Survey of Pakistan (NDSP), 2016–2017. BMJ Open. 2018;8:e020961.
Haddad M. Ramadan 2021: Fasting hours around the world. 2021. https://www.aljazeera.com/news/2021/4/7/ramadan-2021-fasting-hours-around-the-world. Accessed 1 Feb 2022.
Dabral S, Mukherjee S, Saha N, Manjavkar S, Kohli S. A survey of fasting practices and acceptance of an intervention for achieving control in diabetes during Ramadan. Natl Med J India. 2020;33:5–9.
International Diabetes Federation and the DAR International Alliance. Diabetes and Ramadan: practical guidelines. Brussels. 2021. https://www.daralliance.org/daralliance/idf-dar-practical-guidelines-2021/. Accessed 1 Feb 2022.
Jabbar A, Hassanein M, Beshyah SA, et al. CREED study: Hypoglycaemia during Ramadan in individuals with type 2 diabetes mellitus from three continents. Diabetes Res Clin Pract. 2017;132:19–26.
Hassanein M, Al Awadi FF, El Hadidy KES, et al. The characteristics and pattern of care for the type 2 diabetes mellitus population in the MENA region during Ramadan: an international prospective study (DAR-MENA T2DM). Diabetes Res Clin Pract. 2019;151:275–84.
Mauricio D, Hramiak I. Second-generation insulin analogues—a review of recent real-world data and forthcoming head-to-head comparisons. Eur Endocrinol. 2018;14:2–9.
Hassanein M, Akif-Buyukbese M, Malek R, et al. Real-world safety and effectiveness of insulin glargine 300 U/mL in participants with type 2 diabetes who fast during Ramada. Diabetes Res Clin Pract. 2020;166:108189.
Hassanein M, Al-Sifri S, Shaikh S, et al. A real-world study in patients with type 2 diabetes mellitus treated with gliclazide modified-release during fasting: DIA-RAMADAN. Diabetes Res Clin Pract. 2020;163:108154.
Riddle MC, Bolli GB, Ziemen M, et al. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 2 diabetes using basal and mealtime insulin: glucose control and hypoglycemia in a 6-month randomized controlled trial (EDITION 1). Diabetes Care. 2014;37(10):2755–62.
Yki-Jarvinen H, Bergenstal R, Ziemen M, et al. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 2 diabetes using oral agents and basal insulin: glucose control and hypoglycemia in a 6-month randomized controlled trial (EDITION 2). Diabetes Care. 2014;37:3235–43.
Hussein W, Elhadd T, Afandi B, et al. The free communications of the eighth clinical congress (Virtual) of the Gulf Chapter of the American Association of Clinical Endocrinologists; November 5–7, 2020. J Diabetes Endocr Pract. 2020;3:86–120.
Zainudin SB, Abu Bakar KNB, Abdullah SB, Hussain AB. Diabetes education and medication adjustment in Ramadan (DEAR) program prepares for self-management during fasting with tele-health support from pre-Ramadan to post- Ramadan. Ther Adv Endocrinol Metab. 2018;9:231–40.
Ritzel R, Roussel R, Bolli GB, et al. Patient-level meta-analysis of the EDITION 1, 2 and 3 studies: glycaemic control and hypoglycaemia with new insulin glargine 300 U/ml versus glargine 100 U/ml in people with type 2 diabetes. Diabetes Obes Metab. 2015;17:859–67.
Acknowledgements
All of the authors thank the participants, study investigators, and staff who participated in data collection for the study. The participating physicians from the South Asia region are listed in Appendix I of the Electronic Supplementary Material.
Funding
Sponsorship of the ORION study and journal Rapid Service Fee were funded by Sanofi.
Medical Writing Assistance
Manuscript writing support was provided by Amol Gujar, PhD, who is an employee of Sanofi, India.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work, and have given their approval for this version to be published.
Author Contributions
Mohamed Hassanein and Mubarak Naqvi were involved in the conception and design of the study. Mohamed Hassanein, Rakesh Sahay, Mohammad Imtiaz Hasan, Arshad Hussain, Vinod Mittal, Riyaz Mohammed, Zaman Shaikh, and Faraz Farishta substantially contributed to data acquisition for the work related to this document. All authors substantially contributed to the data analysis/interpretation of the results, critically reviewed and approved the final version for submission, and are accountable for the accuracy and integrity of this manuscript.
Prior Presentation
The ORION South Asia study data was partially presented at the 80th Virtual Scientific Sessions of American Diabetes Association (ADA-2020 congress), 12-16 June 2020.
Disclosures
Mohamed Hassanein is a member of the advisory board of Sanofi, Boehringer Ingelheim, and Novo Nordisk; received honorarium from Eli Lilly, Janssen, LifeScan, Merck Sharp and Dohme, Novo Nordisk, and Sanofi; and received lecture/other fees from Sanofi, Novo Nordisk, Eli Lilly, Merck Sharp and Dohme, Janssen, and LifeScan. Arshad Hussain has been speaker for Victoza and Rhyzodeg (Novo Nordisk) in pre-covid time, and also was part of the ORION trial and provided speaker services for Sanofi. Post-covid, Arshad Hussain has been key opinion leader and is part of advisory board for Ozempic (Novo Nordisk). Mohammad Imtiaz Hasan is a member of advisory Board of Sanofi, Novo Nordisk, Eli Lilly, Getz Pharma; and received speaker/lecture services for Sanofi, Novo Nordisk, Eli Lilly, and Getz Pharma. Zaman Shaikh is a member of the advisory Board of Novo Nordisk, Sanofi, Eli Lilly, and Aspin Pharma; and has also provided speaker services for Sanofi, Novo Nordisk, Eli Lilly, Getz, Hilton, Lundbeck, and Novartis Pharmaceuticals. Rakesh Sahay is member of advisory board for Boehringer Ingelheim, Dr Reddys Laboratories, Eli Lilly, and Sanofi; and is speaker for Boehringer Ingelheim, Eli Lilly, Novo Nordisk, and Sanofi. Faraz Farishta has received honorarium/other fees from Sanofi. Riyaz Mohammed and Vinod Mittal have nothing to disclose. Arjun Nair is an employee of Novo Nordisk Ltd, Bangalore, India, and may hold stock/shares. Mubarak Naqvi, Senthilnathan Mohanasundaram, and Zubair Ali are employees of Sanofi and may hold Sanofi stock/shares.
Compliance with Ethics Guidelines
This study was conducted in accordance with the guidelines for Good Epidemiology Practice and the Declaration of Helsinki of 1964 and subsequent amendments, and the study is registered with the World Health Organization International Clinical Trials Registry Platform, registration number CTRI/2019/02/017636. The ORION study protocol was reviewed and approved by the Institutional Review Board/Institutional Ethics Committee in accordance with the local regulations in each participating country/study center. All participants provided written informed consent.
Data Availability
Qualified researchers may request access to patient-level data and related documents including the clinical study report, study protocol with any amendments, blank case report form, statistical analysis plan, and dataset specifications. Patient-level data will be anonymized, and study documents will be redacted to protect the privacy of trial participants. Further details on Sanofi’s data sharing criteria, eligible studies, and process for requesting access can be found at https://www.vivli.org/.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hassanein, M., Sahay, R., Hasan, M.I. et al. A Real-World Observational Study of Gla-300 in Adults with Type 2 Diabetes Who Fast During Ramadan in the South Asia Region: A Subgroup Analysis of the ORION Study. Diabetes Ther 13, 747–759 (2022). https://doi.org/10.1007/s13300-022-01234-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-022-01234-y