Abstract
Introduction
The TROPHIES observational study enrolled patients with type 2 diabetes mellitus (T2DM) initiating their first injectable treatment with the glucagon-like peptide 1 receptor agonists (GLP-1 RAs) dulaglutide or liraglutide. This manuscript focuses on the study design, baseline characteristics of the enrolled population, and factors associated with GLP-1 RA choice.
Methods
TROPHIES is a prospective, observational, 24-month study conducted in France, Germany, and Italy. Inclusion criteria include adult patients with T2DM, naïve to injectable antihyperglycemic treatments, initiating dulaglutide or liraglutide per routine clinical practice. The primary outcome is the duration of treatment on dulaglutide or liraglutide without a significant treatment change.
Results
The analysis included 2181 patients (dulaglutide, 1130; liraglutide, 1051) (cutoff date May 15, 2019). The population was 56% male with mean [standard deviation (SD)] patient characteristics at baseline as follows: age, 59.2 (11.0) years; body mass index (BMI), 33.9 (6.6) kg/m2; T2DM duration, 8.5 (6.9) years; and glycated hemoglobin (HbA1c), 8.2 (1.3)%. Between-cohort demographic and clinical characteristics were balanced. The mean (SD) HbA1c and BMI values for French, German, and Italian patients were, respectively, 8.6 (1.4)%, 8.2 (1.4)%, 8.0 (0.8)%; 33.3 (6.1) kg/m2, 36.0 (7.2) kg/m2, and 32.6 (5.9) kg/m2.
Conclusion
This study analysis at baseline provides an opportunity to evaluate between-country differences in baseline HbA1c, weight, macrovascular complications, and factors driving GLP-1 RA selection for patients with T2DM in daily practice.
Plain Language Summary
Dulaglutide and liraglutide are medications that can help people with type 2 diabetes mellitus (T2DM) to control their blood sugar levels. These medications may also reduce body weight and reduce the risk of major cardiovascular disease. Given these treatment effects, it is essential to know how they are used in everyday clinical practice. Therefore, a study is being performed in three countries (France, Germany, and Italy) in people with T2DM who had a first-ever injectable therapy for T2DM with dulaglutide or liraglutide. Here, we present the study design, the patient characteristics at the start of treatment, and the factors driving the choice of one or the other medication. We analyzed data from 2181 people with T2DM. On average, it was shown that they were middle-aged and obese. On average, these people were diagnosed with T2DM 8.5 years before the start of dulaglutide or liraglutide and had high blood sugar levels when these medications were started. The patient characteristics were slightly different between the three countries. Country-specific factors driving the choice of either medication were also identified.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Glucagon-like peptide 1 receptor agonists (GLP-1 RAs) are recommended as the first injectable antihyperglycemic medication for selected adults with type 2 diabetes (T2DM). |
Observational studies provide valuable insight into patients’ prescription treatment patterns in routine clinical practice and complement randomized controlled trials. |
What did the study ask? |
This analysis presents baseline findings for the population enrolled in the TROPHIES study. |
This is an ongoing study assessing the real-world use of dulaglutide and liraglutide in GLP-1 RA-naïve patients with T2DM to provide information relating to the timing of and the reasons that underlie a significant treatment change in antihyperglycemic therapy after GLP-1 RA initiation; it will provide insights into patient management, prescribing, and clinical information relating to patients who initiate these agents in daily practice. |
What was learned from the study? |
This study included 2181 patients initiating treatment with dulaglutide (n = 1130) or liraglutide (n = 1051) (cutoff date May 15, 2019) from France, Germany, and Italy, with some notable numerical differences in the baseline characteristics of patients identified at the country level. |
These baseline characteristics provide insight into the population of patients with T2DM initiating GLP-1 RAs, as well as the factors driving GLP-1 RA selection, in normal clinical practice in these countries. |
Digital Features
This article is published with digital features, including a summary slide and plain language summary, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.14547270.
Introduction
The latest American Diabetes Association (ADA) and European Association for the Study of Diabetes (EASD) consensus report for the management of type 2 diabetes mellitus (T2DM) recommends glucagon-like peptide 1 receptor agonists (GLP-1 RAs) as the first injectable antihyperglycemic medication for adults with established atherosclerotic cardiovascular disease (CVD), patients without established CVD at high risk for major adverse cardiovascular events (MACE), and patients unable to meet glycated hemoglobin (HbA1c) targets with lifestyle modifications and metformin and who have a compelling need to minimize hypoglycemia or weight gain [1, 2].
Following glucagon-like peptide 1 receptor binding and activation, GLP-1 RAs enhance insulin secretion and inhibit glucagon release in a glucose-dependent manner [1, 3]. They also decrease gastric emptying, reduce body weight, and lower systolic blood pressure and the levels of some circulating lipoproteins and inflammatory markers [4]. Some drugs in this class can also be considered to reduce the risk for MACE [5,6,7].
Multiple agents are currently available in the GLP-1 RA class. Of these, once-weekly dulaglutide and once-daily liraglutide were widely used in a representative sample of European countries at the time when the observational TROPHIES study was initiated [8,9,10,11]. Observational studies provide valuable insight into patients’ prescription treatment patterns in routine clinical practice and complement randomized controlled trials [12,13,14], in spite of their limitations.
The TROPHIES study is assessing the real-world use of dulaglutide and liraglutide in GLP-1 RA-naïve patients with T2DM to estimate the duration of treatment with each of these drugs without a significant treatment change due to treatment- or diabetes-related factors. Additional study outcomes include description of the profiles of the patients who initiated each GLP-1 RA, glucose-lowering medication (GLM) treatments received before and at the time of GLP-1 RA initiation, persistence with the initial GLP-1 RA, reasons for first significant treatment change (as reported by the physician at the time of the change), patient factors at baseline that are associated with the first significant treatment change, clinical and patient-reported psychosocial outcomes, and use of healthcare resources associated with T2DM management. Recently, the TROPHIES patients’ perspectives at baseline, based on generic and disease-specific patient-reported outcomes (PROs), were published [15]. Here, we present the TROPHIES study design, the patients’ demographic and clinical profiles at GLP-1 RA initiation (baseline), their GLM regimens before and at baseline, and the factors associated with the initial choice of GLP-1 RA. We anticipate that TROPHIES will provide information relating to the timing of and the reasons that underlie a significant treatment change in antihyperglycemic therapy after GLP-1 RA initiation. Additionally, the study will provide insights into patient management, prescribing, and clinical information relating to patients who initiate dulaglutide or liraglutide in daily practice.
Methods
Study Design, Patients, and Treatment Details
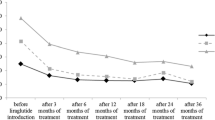
TROPHIES is a prospective, observational, two-cohort (dulaglutide and liraglutide), 24-month study conducted in France, Germany, and Italy. The study was initiated in July 2017, and completion is expected in mid-2021. This analysis includes patients enrolled up to May 15, 2019. Study visits (data collection points) were scheduled at baseline and approximately 6, 12, 18, and 24 months post-baseline as per routine clinical practice (observation period; Fig. 1).
Eligible patients were aged 18 years or older, had a diagnosis of T2DM (based on the investigators’ clinical judgment), were naïve to injectable treatment for T2DM (except for short-term [at most 4 weeks] use of insulin for acute conditions or insulin use during pregnancy), and were prescribed dulaglutide or liraglutide as their first injectable GLM by a physician during a routine healthcare visit. Patients initiating treatment with a GLP-1 RA in combination with insulin or those being treated with an investigational drug/procedure were excluded.
Dulaglutide and liraglutide were administered by subcutaneous injection as per label [16, 17]. The label-recommended dulaglutide dose is 1.5 mg once weekly as add-on therapy to other GLMs or 0.75 mg once weekly as monotherapy in patients for whom metformin is inappropriate because of intolerance or contraindications. For potentially vulnerable patients, a starting dose of 0.75 mg once weekly can be used. Per label, the liraglutide starting dose of 0.6 mg/day should be increased to 1.2 mg/day after at least 1 week and can be further increased to 1.8 mg/day after at least one additional week. Initiation of treatment and any subsequent treatment changes during the observation period were solely at the discretion of the treating physicians.
The study was conducted in accordance with the ethical principles of the Declaration of Helsinki [18] and the applicable laws and regulations of the three countries. Appropriate local bodies approved the study, and these are shown as supplementary material. All participants provided authorization for the use and disclosure of their personal health information covering the collection and release of data regarding treatment and its outcomes for the entire study period. Following the European Union General Data Protection Regulation 2016/679 (effective May 25, 2018), patients were asked to re-consent during a follow-up visit.
Study Objectives
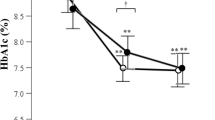
The primary objective is to estimate the duration of treatment with the patients’ first GLP-1 RA (dulaglutide or liraglutide) without a significant treatment change due to treatment- or diabetes-related factors [treatment changes due to factors not related to diabetes (e.g., hospitalization for reasons other than diabetes, pregnancy, or Ramadan) were not designated as treatment or diabetes related]. A significant treatment change comprised discontinuation of the first GLP-1 RA or intensification of GLM (Fig. 2). Discontinuation of the first GLP-1 RA was defined as stopping dulaglutide or liraglutide without initiating another GLM during the remaining observation period, or stopping dulaglutide or liraglutide and initiating treatment with insulin, an oral GLM not taken at baseline, or a different GLP-1 RA. Discontinuation did not include reduction of dulaglutide or liraglutide doses. Treatment intensification was defined as at least one of the following interventions occurring without discontinuing the first GLP-1 RA: increasing the dose of dulaglutide or liraglutide more than 90 days after baseline, adding insulin more than 30 days after baseline (insulin addition less than 30 days after baseline was considered as a simultaneous start; these patients were discontinued from the study and excluded from all analyses), or adding a new oral GLM more than 30 days after baseline.
Secondary objectives include description of patients’ demographic and baseline clinical characteristics (e.g., HbA1c levels, microvascular and macrovascular complications, other comorbidities, medical history), patients’ treatment patterns (persistence with GLP-1 RA treatment regardless of the addition or discontinuation of other GLMs, discontinuation, switching, and intensification), reasons underlying significant treatment changes (e.g., main reason for discontinuation, switching, or intensification), and changes in GLP-1 RA doses over time. Additional secondary objectives include evaluation of factors associated with the choice of the initial GLP-1 RA and those associated with the first significant treatment change. In addition, key clinical outcomes (e.g., HbA1c, body mass index [BMI], weight), PROs, including health-related quality of life (HRQoL), and use of resources associated with the treatment of T2DM will be evaluated in follow-up analyses.
Data Collection
Data collected at baseline included information about prescribing physicians and patient demographic and clinical characteristics. Data relating to clinical outcomes and study objectives were collected at baseline and at each post-baseline visit.
Physician information included specialty, number of years as a practicing physician, and type/location of the practice. Patient demographics included age, sex, race/ethnicity, height, weight, employment/educational status, and health behaviors (e.g., smoking status, alcohol consumption, exercise, and dietary habits). Patient clinical characteristics included date of initial T2DM diagnosis, the two most recent HbA1c measurements (the most recent was recorded as the baseline value), the HbA1c level targeted by the prescribing physician, and comorbidities. Comorbidities, either related or not to diabetes, were collected and categorized (macrovascular, microvascular, or other), and the Charlson Comorbidity Index [19] score was derived from relevant conditions.
Documentation of treatment with GLMs included agents and doses used, any changes made, and the reasons for start, change, and/or discontinuation of each medication. This information was collected for all oral and injectable GLMs taken before baseline and newly initiated at baseline/post-baseline, the GLP-1 RA initiated at baseline, and concomitant non-diabetes-related medications.
PROs assessed were treatment satisfaction using the Diabetes Treatment Satisfaction Questionnaire—Status [20]; perception of injection devices using the Diabetes Injection Device Experience Questionnaire [21]; HRQoL using the EQ-5D-5L questionnaire [22]; life and work productivity impairment using the Diabetes Productivity Measure [23]; and self-perception related to the patient’s body weight using the Impact of Weight on Self-Perceptions Questionnaire [24]. Healthcare utilization data, which covered the 6-month period before treatment initiation and the observation period, included number of visits to healthcare professionals; number and duration of hospital admissions, emergency room visits, and intensive care unit stays; and work days missed. Data relating to the time spent by healthcare professionals training patients how to use dulaglutide and liraglutide injection devices were also collected during the observation period. This manuscript focuses on the baseline TROPHIES clinical results, but information regarding the baseline PRO results has already been published [15].
Statistical Analyses
A sample size of ca. 350 patients in each treatment group, per country, was considered sufficient to provide good precision [95% confidence interval (CI) width, ca. 3 months] for estimation of the median time to first significant treatment change for each GLP-1 RA and to allow for descriptive analyses of each dose of dulaglutide (1.5 and 0.75 mg) and liraglutide (1.2 and 1.8 mg). This sample size was derived by simulation (2000 simulation runs), assuming a median time to first significant treatment change of 9 months (based on Divino et al. [25]), a 24-month observation period, and a dropout rate of 20–30%.
All patients who fulfilled the inclusion and exclusion criteria were included in the analyses. Analyses were performed for the entire study population and for each country-specific population, both overall and per treatment cohort. Baseline patient data were analyzed using descriptive statistics (continuous variables—mean values with standard deviations and median values with minimum, maximum, and quartiles; categorical variables—absolute numbers and relative frequencies).
Factors associated with treatment choice at baseline were explored using univariate analyses (to explore differences between treatment cohorts at baseline), and those with a p value less than 0.1 were entered in multivariate logistic regression models, with several models tested and goodness of fit assessed for each one. In multivariate logistic regression models, factors were considered significant if the p value was less than 0.05. The outcomes of this analysis are presented as estimates and odds ratios, each with corresponding 95% CI limits. Between-cohort comparisons, overall and per country, were performed using the χ2 test and the t test for categorical and continuous variables, respectively. Between-country comparisons were not performed, and p values were not adjusted for multiple testing. Missing data were not imputed for baseline analysis.
The primary outcome (i.e., duration of patients’ treatment on the first GLP-1 RA before a significant treatment change) and the factors associated with this change will be evaluated following the end of the observation period using Kaplan–Meier analysis and the Cox proportional hazard model, respectively. As part of the primary analysis, propensity scores from the logistic model, including factors associated with treatment choice identified at baseline, will be derived and used to compare cohorts, if possible.
Results
Patient Disposition and Baseline Demographic Characteristics
In total, 2181 patients (dulaglutide, 1130; liraglutide, 1051) were included in the analysis: 712 in France (dulaglutide, 377; liraglutide, 335), 727 in Germany (dulaglutide, 364; liraglutide, 363), and 742 in Italy (dulaglutide, 389; liraglutide, 353). Patients were enrolled by diabetologists [1709 (78.4%)], endocrinologists [974 (44.7%)], internists [672 (30.8%)], general practitioners (GPs) [201 (9.2%)], and other specialists [87 (4.0%)]; several physicians reported more than one specialty.
Table 1 shows the demographic characteristics of the dulaglutide and liraglutide cohorts. Patients were predominantly male (56.1%) and Caucasian (92.0%). Mean [standard deviation (SD)] patient age was 59.2 (11.0) years [France 58.5 (10.9); Germany 57.4 (11.5); Italy 61.6 (10.1)] (Table S1). The mean (SD) duration of T2DM from diagnosis to baseline was 8.5 (6.9) years [France 9.0 (7.2); Germany 6.8 (6.0); Italy 9.6 (7.2)] (Table S1).
Clinical and Biological Characteristics at Baseline
Table 2 shows the clinical characteristics of the dulaglutide and liraglutide cohorts at baseline, before treatment started. The overall mean (SD) HbA1c at baseline was 8.2 (1.3)%, with 50.9% of patients having HbA1c ≤ 8.0% and 46.9% of patients having HbA1c > 8.0%. The mean (SD) HbA1c target set by the treating physicians was 6.9 (0.4)%, and the most frequent HbA1c target ranges were ≥ 7.0 to < 8.0% (58.2%) and ≥ 6.5 to < 7.0 (38.3%). The actual mean (SD) HbA1c value was 1.4 (1.2)% higher than the target value. The mean (SD) HbA1c values of French, German, and Italian patients were 8.6 (1.4)%, 8.2 (1.4)%, and 8.0 (0.8)%, respectively (Fig. 3a; Table S1); the respective mean (SD) differences between actual and target HbA1c levels were 1.6 (1.4)%, 1.3 (1.3)%, and 1.2 (0.8)%. The proportions of patients with baseline HbA1c levels ≥ 7.5 and < 8.5% in France, Germany, and Italy were 34.0%, 34.1%, and 64.8%, respectively.
The overall mean (SD) weight and BMI was 96.7 (21.5) kg and 33.9 (6.6) kg/m2, respectively. The mean (SD) weight of French, German, and Italian patients was 93.4 (19.0), 106.8 (23.0), and 90.1 (18.9) kg, respectively (Table S1). The mean (SD) BMI values of French, German, and Italian patients were 33.3 (6.1), 36.0 (7.2), and 32.6 (5.9) kg/m2, respectively (see Fig. 3a for per cohort and per country BMI data). Overall, the mean (SD) systolic and diastolic blood pressures were 136.8 (17.5) and 80.7 (10.7) mmHg, respectively (see Table S1 for per country and per cohort values). Hypertension was reported by 73.2% of all patients (dulaglutide, 71.9%; liraglutide, 74.5%; Table 2). At the country level, the proportions of French, German, and Italian patients with hypertension were 66.2%, 79.2%, and 74.0%, respectively; the between-cohort difference in the proportion of patients with hypertension was highest in France (dulaglutide, 63.0%; liraglutide, 69.9%) (Table S1). Hyperlipidemia and liver disease were reported by 63.5% and 9.5% of all patients, respectively (Table 2) (see Table S1 for per country and per cohort values).
As regards diabetes-related comorbidities, 19.1% of all patients presented with at least one macrovascular condition (dulaglutide, 14.2%; liraglutide, 24.5%; p < 0.001) (Table 2). The between-cohort difference was explained by the numerically lower proportion of patients with myocardial infarction (MI) in the dulaglutide cohort in France (dulaglutide, 4.8% and liraglutide, 22.1%; Table S1), whereas in Germany and Italy no such difference in the proportion of patients with MI was observed. At least one microvascular condition was reported by 19.6% of all patients (dulaglutide, 20.2%; liraglutide, 18.9%; p = 0.442). The proportion of German patients with such conditions was higher in those receiving dulaglutide than liraglutide (27.5% and 18.7%, respectively; p = 0.004). This difference was driven primarily by neuropathy (16.2% and 10.7%, respectively). The between-cohort proportions of French and Italian patients with microvascular conditions did not differ (p > 0.05, both comparisons; Table S1).
Treatment Details at Baseline
In the overall population, 85.8% of patients received at least one oral GLM before or at the time of dulaglutide or liraglutide initiation (Table 2). The proportions of patients receiving one, two, and three or more oral GLMs were 56.5%, 26.3%, and 3.0%, respectively (Table 2). Metformin was the most frequently used oral GLM (either alone or in combination with other GLMs) in both treatment cohorts of all three countries. The proportions of patients receiving metformin alone in France, Germany, and Italy were 38.9%, 47.0%, and 65.4%, respectively (Table S1). The proportion of patients who reported receiving metformin and sulfonylurea in France, Germany, and Italy was 25.1%, 2.3%, and 12.5%, respectively (Table S1), and of those receiving sodium-glucose transporter 2 (SGLT2) inhibitors (alone or in combination) was 0%, 27.9%, and 0.5%, respectively (at the start of the study, SGLT2 inhibitors were not reimbursed in France; in Italy, they were not reimbursed in association with GLP-1 RA use). Proportions (%) of all patients on dulaglutide or liraglutide, respectively, were reported for lipid-lowering (50.1%, 51.7%), cardiovascular (69.8%, 72.4%), antithrombotic (29.5%, 36.2%), antiemetic (0.3%, 0.5%), and weight-lowering (0.2%, 0.1%) medications during the 6 months before baseline. Table 2 and Table S1 show patients’ cardiovascular medications.
Baseline Factors Associated with GLP-1 RA Choice
Table 3 shows the factors associated with GLP-1 RA treatment choice at baseline. In France, factors more likely to be associated with the initiation of liraglutide than dulaglutide included physician specialty other than diabetologist, endocrinologist, internist, or GP, presence versus absence of CVD, patients not exercising versus exercising, and those receiving versus not receiving antithrombotic treatment. Conversely, private versus public practice physicians and physicians with non-urban versus urban practices were more likely to prescribe dulaglutide than liraglutide. In Germany, private versus public physicians, internists, and GPs were more likely to prescribe liraglutide than dulaglutide. In contrast, German patients with higher versus lower than basic education and those consuming versus not consuming alcohol were more likely to be initiated with dulaglutide than liraglutide. In Italy, diabetologists versus other physician specialties and consuming versus not consuming alcohol were factors associated with the prescription of dulaglutide rather than liraglutide.
Discussion
The TROPHIES study focuses on patients with T2DM initiating their first injectable antihyperglycemic treatment with dulaglutide or liraglutide in the normal course of care in France, Germany, and Italy. For the overall population, enrolled patients were middle aged (ca. 60 years), more likely to be male, and obese (mean BMI ca. 34 kg/m2), with a mean disease duration of 8.5 years, a mean HbA1c of 8.2%, and a mean difference between actual and targeted HbA1c of 1.4%. These baseline characteristics provide insight into the population of patients with T2DM receiving GLP-1 RAs in normal clinical practice in these countries.
Additionally, our analysis identified some notable numerical differences at the country level. First, the duration of T2DM was numerically shorter in German than French or Italian patients. In all three countries, the guidelines for T2DM management allow GLP-1 RA prescription if glycemic control is not achieved with metformin [26,27,28]. Second, as German patients had a high mean weight and BMI, physicians in this country may be initiating treatment with GLP-1 RA earlier than French or Italian physicians because of the weight loss potential with these agents [4]. In fact, the current German T2DM management guidelines recommend using GLP-1 RAs in conjunction with oral GLMs (preferably metformin) in patients with substantial weight problems [29]. Our finding is supported by Qiao et al. [30], who reported that patients initiating GLP-1 RAs in Germany had a higher mean BMI than patients initiating other non-GLP-1 RA antihyperglycemic medications (36.1 vs 31.3 kg/m2, respectively). Third, the proportion of patients with baseline HbA1c levels ≥ 7.5% and < 8.5% in Italy was almost twofold higher than the respective proportions in France or Germany; this finding may be attributed to the fact that, in Italy, GLP-1 RAs were reimbursed only for patients with HbA1c levels of 7.5–8.5% at the time of patient enrollment in the TROPHIES study.
The mean BMI for French patients reported in this study is consistent with that reported for French patients with T2DM in the ObEpi (obesity epidemiology) 2012 survey (33.3 and 29.9 kg/m2, respectively) [31], and the mean BMI of the TROPHIES Italian patients is consistent with that reported for Italian patients with T2DM aged less than 65 years (32.6 and 30.7 kg/m2, respectively) [32]. Systolic blood pressure was numerically higher for German than for French or Italian patients, a factor that might align with the higher body weight of this population.
In France, the proportion of patients with macrovascular conditions, including MI, was significantly lower in the dulaglutide than the liraglutide cohort, which resulted in a corresponding difference observed at the overall study population level. This difference may be because, during the patient enrollment period for TROPHIES, the French Diabetes Society position statement recommended the administration of liraglutide to patients with T2DM who required secondary CVD prevention on the basis of the outcomes of the LEADER study [5, 33]. This supposition is supported by the analyses of factors associated with treatment choice at baseline that showed that the presence of macrovascular cardiovascular disease increased the likelihood of the patient receiving liraglutide in France. However, since the start of TROPHIES, other trials demonstrating cardiovascular benefit have been published, including REWIND for dulaglutide [7]. In 2019, the 2018 ADA/EASD consensus statement update recommended that GLP-1 RAs be considered in patients with T2DM with established CVD or without established CVD but with high risk factors to reduce MACE, and proposed the use of dulaglutide for the primary prevention of CVD, as it was supported by strong evidence that was lacking from other GLP-1 RAs [2]. As the TROPHIES study progresses, treatment modifications based on newly published data and updated guidance in this field will be monitored.
A numerically higher proportion of patients from Italy reported concomitant use of at least one GLM compared with patients from France or Germany. In France and Italy, GLP-1 RAs are reimbursed only if given concomitantly with metformin; thus, approximately two-thirds of patients were taking metformin, either alone or in combination with a sulfonylurea, at the time of GLP-1 RA initiation. Because SGLT2 inhibitors were not reimbursed in France, and in Italy they were not reimbursed in association with GLP-1 RAs when TROPHIES was initiated, no patients in France and only four in Italy reported using SGLT2 inhibitors alone or as part of combination therapy at baseline.
Limitations should be considered when interpreting these findings. At some sites, investigators may not have had patients’ complete treatment records, so the numbers and types of GLMs received before baseline are probably underestimated. Patient selection bias cannot be ruled out. Per protocol, patients who had previously received insulin were excluded, but this may not reflect the therapeutic history of all patients who initiate GLP-1 RAs in real-world practice in the countries in the study. Moreover, healthcare systems and patient care may vary across countries, so the findings of this study may not apply to other countries. For example, in Italy, all physicians were specialists, as Italian GPs are not allowed to prescribe GLP-1 RAs. Likewise, in France, almost all physicians enrolling patients were diabetes specialists; however, GPs in France can also initiate treatment with GLP-1 RAs in patients with T2DM. This may have influenced the profile of the French patients included in TROPHIES, as patients treated by specialists may have a more advanced and complex disease profile than those treated by GPs.
Conclusions
This observational study will improve our understanding of the treatment patterns associated with two widely prescribed GLP-1 RAs in three large European countries, including reasons for therapeutic changes. Valuable clinical data from patients will also be obtained. The current report shows how the design of the study will address multiple questions and highlights how patient characteristics differ among cohorts and countries. The similarities and differences identified may be explained by the study design or by local patient factors, prescribing habits, and guidelines.
References
Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41:2669–2701
Buse JB, Wexler DJ, Tsapas A, et al. 2019 update to: management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2020;43:487–493. https://doi.org/10.2337/dci19-0066.
Nauck MA, Meier JJ. Incretin hormones: their role in health and disease. Diabetes Obes Metab. 2018;20(Suppl 1):5–21. https://doi.org/10.1111/dom.13129.
Nauck MA, Meier JJ, Cavender MA, Abd El Aziz M, Drucker DJ. Cardiovascular actions and clinical outcomes with glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors. Circulation. 2017;136:849–870. https://doi.org/10.1161/CIRCULATIONAHA.117.028136.
Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375:311–22.
Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375:1834–1844. https://doi.org/10.1056/NEJMoa1607141.
Gerstein HC, Colhoun HM, Dagenais GR, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet. 2019;394:121–30. https://doi.org/10.1016/S0140-6736(19)31149-3.
Divino V, DeKoven M, Khan FA, Boye KS, Sapin H, Norrbacka K. GLP-1 RA treatment patterns among type 2 diabetes patients in five European countries. Diabetes Ther. 2017;8:115–28. https://doi.org/10.1007/s13300-016-0224-5.
Divino V, Boye KS, Lebrec J, DeKoven M, Norrbacka K. GLP-1 RA treatment and dosing patterns among type 2 diabetes patients in six countries: a retrospective analysis of pharmacy claims data. Diabetes Ther. 2019;10:1067–88. https://doi.org/10.1007/s13300-019-0615-5.
Otto T, Myland M, Jung H, Lebrec J, Richter H, Norrbacka K. Utilization patterns of glucagon-like peptide-1 receptor agonists in patients with type 2 diabetes mellitus in Germany: a retrospective cohort study. Curr Med Res Opin. 2019;35:893–901. https://doi.org/10.1080/03007995.2018.1538011.
Federici MO, McQuillan J, Biricolti G, et al. Utilization patterns of glucagon-like peptide-1 receptor agonists in patients with type 2 diabetes mellitus in Italy: a retrospective cohort study. Diabetes Ther. 2018;9:789–801. https://doi.org/10.1007/s13300-018-0396-2.
Chatterjee S, Davies MJ, Khunti K. What have we learnt from “real world” data, observational studies and meta-analyses. Diabetes Obes Metab. 2018;20(Suppl 1):47–58. https://doi.org/10.1111/dom.13178.
Carls GS, Tuttle E, Tan RD, et al. Understanding the gap between efficacy in randomized controlled trials and effectiveness in real-world use of GLP-1 RA and DPP-4 therapies in patients with type 2 diabetes. Diabetes Care. 2017;40:1469–78. https://doi.org/10.2337/dc16-2725.
He Z, Wang S, Borhanian E, Weng C. Assessing the collective population representativeness of related type 2 diabetes trials by combining public data from ClinicalTrials.gov and NHANES. Stud Health Technol Inform. 2015; 216:569–573.
Boye KS, Sapin H, García-Pérez LE, et al. The real-world observational prospective study of health outcomes with dulaglutide and liraglutide in type 2 diabetes patients (TROPHIES): baseline patient-reported outcomes. Diabetes Ther. 2020;11:2383–99. https://doi.org/10.1007/s13300-020-00908-9.
European Medicines Agency. Trulicity SPC. https://www.ema.europa.eu/en/documents/product-information/trulicity-epar-product-information_en.pdf. Accessed Jun 22, 2020.
European Medicines Agency. Victoza SPC. https://www.ema.europa.eu/en/documents/product-information/victoza-epar-product-information_en.pdf. Accessed Jun 22, 2020.
World Medical Association. Declaration of Helsinki. Recommendations guiding physicians in biomedical research involving human subjects. JAMA. 1997;277(11):925–926.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Bradley C, Lewis KS. Measures of psychological well-being and treatment satisfaction developed from the responses of people with tablet-treated diabetes. Diabet Med. 1990;7:445–51. https://doi.org/10.1111/j.1464-5491.1990.tb01421.x.
Matza LS, Boye KS, Stewart KD, Paczkowski R, Jordan J, Murray LT. Development of the diabetes injection device experience questionnaire (DID-EQ) and diabetes injection device preference questionnaire (DID-PQ). J Patient Rep Outcomes. 2018;2:43. https://doi.org/10.1186/s41687-018-0068-z.
EuroQol Group. https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/. Accessed Jun 22, 2020.
Brod M, Skovlund SE, Wittrup-Jensen KU. Measuring the impact of diabetes through patient report of treatment satisfaction, productivity and symptom experience. Qual Life Res. 2006;15:481–91. https://doi.org/10.1007/s11136-005-1624-6.
Hayes RP, DeLozier AM. Reliability, validity, and responsiveness of the impact of weight on self-perceptions questionnaire (IW-SP) in individuals with type 2 diabetes and obesity. Diabetes Technol Ther. 2015;17:210–4.
Divino V, DeKoven M, Hallinan S, et al. Glucagon-like peptide-1 receptor agonist treatment patterns among type 2 diabetes patients in six European countries. Diabetes Ther. 2014;5:499–520.
Landgraf R, Kellerer M, Aberle J, et al. Therapie des Typ-2-Diabetes. Diabetologie. 2019;14(Suppl 2):S167–87.
Haute Autorité de Santé. Stratégie médicamenteuse du contrôle glycémique du diabète de type 2, 2013. https://www.has-sante.fr/upload/docs/application/pdf/2013-02/10irp04_reco_diabete_type_2.pdf. Accessed Jun 22, 2020.
Associazione Medici Diabetologi (AMD). Standard Italiani per la Cura del Diabete Mellito 2018. https://aemmedi.it/wp-content/uploads/2009/06/AMD-Standard-unico1.pdf. Accessed October 12, 2020.
Nationale VersorgungsLeitlinien 2013. https://extranet.who.int/ncdccs/Data/DEU_D1_Type%202%20Diabetes.pdf. Accessed Jun 22, 2020.
Qiao Q, Grandy S, Hiller J, Kostev K. Clinical and patient-related variables associated with initiating glp-1 receptor agonist therapy in type 2 diabetes patients in primary care in Germany. PLoS One. 2016;11:e0152281.
Eschwege E, Basdevant A, Crine A, Moisan C, Charles M-A. Type 2 diabetes mellitus in France in 2012: results from the ObEpi Survey. Diabetes Metab. 2015;41:55–61. https://doi.org/10.1016/j.diabet.2014.11.007.
Monographie degli Annali AMD, 2017. https://aemmedi.it/wp-content/uploads/2018/06/Monografia_AMD-protetto.pdf. Accessed Jun 22, 2020.
Darmon P, Bauduceau B, Bordier L, et al. Prise de position de la Société Francophone du Diabète (SFD) sur la prise en charge médicamenteuse de l’hyperglycémie du patient diabétique de type 2. Méd Mal Métabol. 2017;11:577–93.
Acknowledgements
The authors thank the participants, caregivers, and investigators at the study centers across France, Germany, and Italy. The authors are grateful to IQVIA for their help in the recruitment and the running of the TROPHIES study.
Funding
This article and the journal’s Rapid Service Fee was sponsored by Eli Lilly and Company, Indianapolis, IN, USA.
Medical Writing and Editorial Assistance
The authors thank Ioannis Nikas and Janet Douglas (Rx Communications, Mold, UK) for providing writing and editorial assistance (funding provided by Eli Lilly and Company).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Luis-Emilio García-Pérez has made substantial contributions to the conception of the work, the design of the work, the interpretation of data, and critical revision of the manuscript. Kristina Boye has made substantial contributions to the conception of the work, the design of the work, the acquisition of data, the interpretation of data, and critical revision of the manuscript. Myriam Rosilio has made substantial contributions to the acquisition of data, the analysis of data, the interpretation of data, and critical revision of the manuscript. Heike Jung has made substantial contributions to the conception of the work, the design of the work, the interpretation of data, and critical revision of the manuscript. Elke Heitmann has made substantial contributions to the design of the work, the interpretation of data, and critical revision of the manuscript. Kirsi Norrbacka has made substantial contributions to the conception of the work, the design of the work, the interpretation of data, and critical revision of the manuscript. Marco Orsini Federici has made substantial contributions to the interpretation of data and critical revision of the manuscript. Raffaella Gentilella has made substantial contributions to the interpretation of data and critical revision of the manuscript. Bruno Guerci has made substantial contributions to the interpretation of data, the analysis of data, and critical revision of the manuscript. Francesco Giorgino has made substantial contributions to the conception of the work, the design of the work, the acquisition of data, the interpretation of data, the analysis of data, the drafting of the manuscript, and critical revision of the manuscript. Ulrich Aigner has made substantial contributions to the acquisition of data, the interpretation of data, and critical revision of the manuscript. Hélène Sapin has made substantial contributions to the conception of the work, the design of the work, the acquisition of data, the interpretation of data, the analysis of data, and critical revision of the manuscript. Luis-Emilio García-Pérez, Kristina Boye, Myriam Rosilio, Heike Jung, Elke Heitmann, Kirsi Norrbacka, Marco Orsini Federici, Raffaella Gentilella, Bruno Guerci, Francesco Giorgino, Ulrich Aigner, and Hélène Sapin give final approval of the manuscript to be submitted and have participated sufficiently in the work to agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Prior Presentation
Part of the data from this study analysis were presented at ISPOR Europe 2019, held in November 2–7, 2019, in Copenhagen, Denmark.
Disclosures
Bruno Guerci has participated in scientific advisory boards for Sanofi, Eli Lilly, Novo Nordisk, Novartis, GSK, MSD, Boehringer Ingelheim, AstraZeneca, Abbott, Medtronic, and Roche Diagnostics. He is also a Clinical investigator for Sanofi, Eli Lilly, Novo Nordisk, GSK, BMS, AstraZeneca, Medtronic, Abbott, Roche Diagnostics, MSD, Novartis, Janssen, and Boehringer Ingelheim and has received research support from Medtronic, VitalAire, Sanofi, Eli Lilly, and Novo Nordisk. Francesco Giorgino has participated in scientific advisory boards and received consulting fees from AstraZeneca, Boehringer Ingelheim, Eli Lilly, MSD, Novo Nordisk, Roche Diabetes Care, and Sanofi. Ulrich Aigner has no disclosures to declare. Luis-Emilio García-Pérez, Kristina Boye, Myriam Rosilio, Heike Jung, Elke Heitmann, Kirsi Norrbacka, Marco Orsini Federici, and Hélène Sapin are employees and minor shareholders of Eli Lilly and Company. Raffaella Gentilella is a former employee of Eli Lilly & Company Italia SpA and is currently an employee of Jazz Pharmaceuticals—Jazz Healthcare Italy s.r.l. and a minor shareholder of Eli Lilly.
Compliance with Ethics Guidelines
The study was conducted in accordance with the ethical principles of the Declaration of Helsinki and the applicable laws and regulations of the three countries [18]. Appropriate local bodies approved the study, and these are shown as supplementary material. All participants provided authorization for the use and disclosure of their personal health information covering the collection and release of data regarding treatment and its outcomes for the entire study period. Following the European Union General Data Protection Regulation 2016/679 (effective May 25, 2018), patients were asked to re-consent during a follow-up visit.
Data Availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
García-Pérez, LE., Boye, K.S., Rosilio, M. et al. The Real-World Observational Prospective Study of Health Outcomes with Dulaglutide and Liraglutide in Type 2 Diabetes Patients (TROPHIES): Design and Baseline Characteristics. Diabetes Ther 12, 1929–1946 (2021). https://doi.org/10.1007/s13300-021-01076-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-021-01076-0