Abstract
Objectives
Despite various methodological concerns, previous studies mainly use questionnaires to assess mindfulness. Following a multi-measurement approach, the present study aimed to evaluate the added value of an experience-sampling measure in the context of posttraumatic stress disorder (PTSD) and depression.
Method
Data were collected in a PTSD group, depression group, and control group (each n = 33). The Mindful-Breathing Exercise (MBE) was used as an experience-sampling method and the Five Facet Mindfulness Questionnaire (FFMQ) as a mindfulness questionnaire. Clinical variables included PTSD and depressive symptoms.
Results
Scores from the MBE and the FFMQ were positively correlated in the control group (r = 0.48) and the depression group (r = 0.28), while a non-significant correlation emerged for the PTSD group. On the level of FFMQ facets, results were heterogeneous among the three groups. The MBE predicted hyperarousal (β = − 0.41) and intrusions (β = − 0.32) in the PTSD group, whereas the FFMQ predicted depressive symptoms in the depression group (β = − 0.41) and the control group (β = − 0.65). Compared to the control group, the PTSD group (d = 1.88) and the depression group (d = 1.67) demonstrated lower FFMQ scores. In terms of the MBE, there was a trend towards higher scores in the control group than either clinical group.
Conclusions
Findings hint at conceptual overlaps and distinctive features of both measurement approaches. With respect to the clinical context, results suggest an added value of the MBE to questionnaire-based assessments of mindfulness with respect to its predictive value for hyperarousal and intrusions.
Preregistration
This study is not pre-registered.
Similar content being viewed by others
Historically, mindfulness can be traced back to 2500-year-old Buddhist teachings and represents an essential internal attitude in Eastern meditation practice (Bodhi, 2011). In Western psychological literature, various definitions of mindfulness exist focusing on different aspects (for an overview, see Medvedev et al., 2022). One of the most common definitions was introduced by Kabat-Zinn (1994), who describes mindfulness as a non-judgmental, nonreactive, and open-hearted moment-by-moment focus of attention. Mindfulness seems to be an important beneficial factor in the context of mental health (Tomlinson et al., 2018). Therefore, it has become more popular in both psychological practice and research and has evolved into a broad concept during the last decades (Bravo et al., 2022). This development has resulted, on the one hand, in a critical debate about discrepancies between the Western understandings of mindfulness and its original Buddhist conceptualization (e.g., Baer, 2019; Feng et al., 2018) and, on the other hand, in a lack of consensus regarding the conceptualizations of mindfulness in general (van Dam et al., 2018).
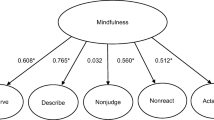
The distinct conceptual understandings are also reflected in different approaches to operationalize mindfulness. As a result, a large number of mindfulness questionnaires were published that are based on a different idea of dimensionality of the construct (for an overview, see Bergomi et al., 2013; Sauer et al., 2013). Two of the most commonly used questionnaires are the Mindful Attention and Awareness Scale (MAAS; Brown & Ryan, 2003) and the Five Facet Mindfulness Questionnaire (FFMQ; Baer et al., 2006). While the MAAS is based on a unidimensional understanding of mindfulness, Baer et al. (2006) considered mindfulness to be a multidimensional construct. This is based on the factor analytical development of the FFMQ which comprises the following facets: “observing” (tendency to notice or attend to internal and external experiences), “describing” (tendency to label internal and external experiences with words), “acting with awareness” (full awareness and undivided attention of current experiences), “nonjudging of experience” (viewing internal experiences with a non-evaluative stance), and “nonreactivity to inner experience” (tendency to allow thoughts, emotions, and bodily sensations to come and go).
Besides the different operationalizations and conflicting underlying definitions of mindfulness, further methodological concerns regarding the validity of mindfulness assessed by questionnaires need to be considered (van Dam et al., 2018). Firstly, empirical findings suggested an unstable factor structure of the FFMQ depending on the general experience with mindfulness or meditation (Baer et al., 2006; Baer et al., 2008; Williams et al., 2014), the participation in a mindfulness-based intervention (Gu et al., 2016), or the psychopathology of the examined sample (Curtiss & Klemanski, 2014). Secondly, recent findings stated that FFMQ scores did not differ between groups receiving a mindfulness intervention compared to control conditions (Goldberg et al., 2016; Isbel et al., 2020), and showed no significant association with duration or frequency of actual mindfulness practice (Falkenström, 2010; Manuel et al., 2017). These results indicate discrepancies between how mindful individuals consider themselves in their ratings in questionnaires and how mindful they really seem to be. One main explanation is that the semantic understanding of mindfulness items (e.g., “I rush through activities without being really attentive to them.” from the FFMQ) seems to depend on one’s individual experience with and understanding of mindfulness practices (Grossman, 2008; van Dam et al., 2018). As mindfulness practice enhances self-awareness of one’s actual mindlessness, it may then result in lower mindfulness self-reports (van Dam et al., 2018).
In a recent psychometric review, Lecuona et al. (2020) recommended the development and evaluation of alternative assessment tools measuring mindfulness. Common alternative approaches to mindfulness questionnaires are experience-sampling methods during a meditative practice: the Mindful-Breathing Exercise (MBE; Burg & Michalak, 2011), the Breath-Counting Test (BCT; Levinson et al., 2014), and the Meditation Breath Attention Scores (MBAS; Frewen et al., 2008). They are also based on self-reports but do not use a semantic approach. Instead, they assess the ability to maintain one’s attention to the breath (e.g., without mind wandering) during a 15–20-min sitting meditation.
Another major aspect in terms of the conceptionalization and operationalization of mindfulness is the distinction between trait and state: While most definitions consider mindfulness to be a dispositional long-lasting trait (Brown & Ryan, 2003), it can also be understood as a current state (Lau et al., 2006). Trait mindfulness is defined by a “general tendency of being mindful” in daily life, whereas state mindfulness rather comprises “the degree of mindfulness at any particular point in time or context” (Bravo et al., 2022, p. 4). The majority of the established questionnaires conceptualized mindfulness as a trait only (Lau et al., 2006). Therefore, experience-sampling approaches have the potential to become an important addition in the assessment of mindfulness as they represent more state-like qualities of mindfulness, i.e., the capacity to cultivate a state of mindfulness during meditative practice.
The MBE seems to be particularly suitable as an experience-sampling method because it follows a naturalistic approach of just mindfully observing the breathing. Burg and Michalak (2011) examined the convergent validity of the MBE in a sample of undergraduates and found positive correlations with mindfulness questionnaire facets of “acting with awareness” and “accepting without judgment.” Further results indicated positive correlations of the MBE with self-regulation (Burg et al., 2012) and self-esteem (Burg & Michalak, 2012).
Just as mindfulness has been shown to be related to aspects of positive mental health, it also seems to constitute an essential protective and psychological resilience factor for mental disorders like posttraumatic stress disorder (PTSD; R. W. Thompson et al., 2011) and depression (e.g., Schut & Boelen, 2017). Concerning PTSD, chronic avoidance of trauma-related memories, thoughts, and feelings highly contributes to the etiology and maintenance of the disorder (e.g., Orsillo & Batten, 2005; Walser & Hayes, 2006). In contrast, a mindful, non-judgmental awareness of painful memories and trauma-related thoughts and feelings counteracts avoidance behaviors and diminishes the risk of PTSD after a traumatic experience (Thompson et al., 2011). In the context of depression, one explanation is that mindfulness promotes a detached, decentered relationship with negative feelings and thoughts, which, in turn, leads to increased disengagement from ruminative processing (Teasdale et al., 2002; van der Velden et al., 2015). Hence, mindfulness is essential in preventing the exacerbation of negative thinking patterns (Ma & Teasdale, 2004).
Various correlational findings and group comparisons provide empirical evidence for the above-mentioned theoretical considerations regarding lower levels of self-reported mindfulness in patients diagnosed with PTSD or depression. In terms of PTSD, questionnaire-based measurements of mindfulness were negatively associated with overall PTSD symptomology (Carpenter et al., 2019), with its symptom clusters of intrusions and hyperarousal (Martin et al., 2018), as well as with that of avoidance (Thompson & Waltz, 2010). Additionally, Boughner et al. (2016) found that lower levels of self-reported mindfulness partially mediated the association between increased traumatic experiences and PTSD overall symptomology. Questionnaire-based measurements of mindfulness have also shown negative associations with depression symptom severity in trauma-exposed patients (Barr et al., 2019), and patients with PTSD (Schoorl et al., 2015) and with depressive disorders (Argus & Thompson, 2008; Solem et al., 2015), as well as in non-clinical samples (e.g., Freudenthaler et al., 2017; López et al., 2016). Regarding experience-sampling methods, Burg and Michalak (2011) found a negative association of the MBE with depressive symptoms, rumination, and repetitive negative thinking in a non-clinical sample.
As known so far, results of group comparisons indicated that traumatized patients with PTSD have lower mindfulness scores in questionnaires compared to traumatized individuals without PTSD and healthy controls (Basharpoor et al., 2015; Wahbeh et al., 2011). Nevertheless, the amount of group comparisons in relation to PTSD is sparse, and experience-sampling approaches have not yet been used with PTSD patients. In terms of depression, patients diagnosed with a current depressive episode had significantly lower mindfulness scores in questionnaires than patients in remission (Solem et al., 2015) and healthy controls (Crowe & McKay, 2016; Didonna et al., 2019). Rohde et al. (2014) showed that patients with depression had lower MBE scores in comparison to never-depressed controls and had significantly higher self-reported self-criticism after mind wandering during the MBE.
In the light of these findings, an ever-growing number of mindfulness-based programs has been developed in the clinical context (Baminiwatta & Solangaarachchi, 2021). However, valid and reliable measurements of mindfulness are required in order to assess the effectiveness of these programs (Isbel et al., 2020; Medvedev et al., 2022). Against the background of the described methodological limitations of mindfulness questionnaires (van Dam et al., 2018), it seems important to implement psychometrically solid additional measurement approaches of mindfulness. Various studies delivered promising results using self-report-based experience-sampling approaches to assess more state-like aspects of mindfulness during a meditation task (e.g., Burg & Michalak, 2011; Frewen et al., 2008; Levinson et al., 2014). In the context of depressive symptoms, experience-sampling methods for assessing mindfulness have been examined in non-clinical samples (Burg & Michalak, 2011; Frewen et al., 2011) and in patients diagnosed with depression (Rohde et al., 2014). However, apart from that, these approaches are not well established in clinical research yet. Up until now, only few studies have used them to measure mindfulness as an outcome variable in the evaluation of mindfulness-based interventions, e.g., one with healthy individuals (Isbel et al., 2020) and one with PTSD patients (Müller-Engelmann et al., 2019). Furthermore, systematic studies examining experience-sampling methods for mindfulness in the context of PTSD seem to be lacking entirely, which we consider a major issue, given the recently increasing presence of mindfulness in traumatic stress research (e.g., Hopwood & Schutte, 2017; Taylor et al., 2020).
Therefore, the present study pursued the main goal of evaluating the added value of an experience-sampling method as an additional measurement approach to mindfulness questionnaires. The combination of these two self-report-based operationalizations of mindfulness is ideally suited to triangulate these assessments in the clinical context. In the context of depressive symptoms, a lot of research has focused on mindfulness measured by questionnaires and first results exist with regard to experience-sampling. Therefore, it seems particularly promising to examine both measurement approaches in PTSD patients not only in reference to healthy individuals, but also in reference to patients diagnosed with depression. Until now, studies comparing different clinical groups with respect to mindfulness were based on questionnaires only (e.g., Crowe & McKay, 2016; Didonna et al., 2019). In contrast, the present study followed a multi-measurement approach using the MBE as an experience-sampling method to assess state aspects of mindfulness in combination with questionnaire-based measurements of mindfulness covering trait aspects.
As a first step, we examined associations of the two measurement approaches separately in three different samples: PTSD group, depression group, and control group (Hypothesis I). Next, we examined the relationship of experience-sampling and questionnaire-based measurements of mindfulness with clinical variables (Hypothesis II). Last, we performed group comparisons between the three groups (Hypothesis III). Our hypotheses were as follows: (I) We expected to find positive correlations of experience-sampling and questionnaire-based measurements of mindfulness in all three samples. (II) We expected both measurement approaches to be negatively associated with all three PTSD symptom clusters (intrusions, avoidance, and hyperarousal) in the PTSD group. Furthermore, we predicted negative associations with depressive symptoms in all three groups. In addition, we examined to which extent mindfulness, assessed by experience-sampling, predicts unique variance above and beyond questionnaire-based measurements of mindfulness in the PTSD symptom clusters (only the PTSD group) and in the depressive symptoms (the depression and control group). (III) We expected the PTSD and depression groups to show lower levels of mindfulness in both measurement approaches compared to the control group. We further compared both clinical groups, which might allow the discovery of disorder-specific characteristics in mindfulness.
Method
Participants
The overall sample (N = 99) in this study was made up of three samples (PTSD group, depression group, and control group; each sample n = 33). The PTSD and depression group were recruited from the waiting list of our outpatient treatment center at Goethe-University Frankfurt, and half of the data of the PTSD group (n = 16) were collected from another associated therapy study (Müller-Engelmann et al., 2019). The control group was recruited via different public channels.
For all participants, inclusion criteria were an age between 18 and 65 years and informed consent. In the PTSD group, we included patients having a primary diagnosis of PTSD and allowed for additional Axis I diagnoses, as in most patients there are high comorbidities in clinical practice (e.g., Nichter et al., 2019; Nickerson et al., 2017). Consequently, the PTSD group also comprised PTSD patients suffering from comorbid depression. In contrast, in the depression group, we only included patients with a single major depressive episode, recurrent depressive disorders, or persistent depressive disorders while not having any further Axis I diagnosis. We consider the two clinical samples (PTSD group vs. depression group) as conceptually distinct even though depression was not an exclusion criterion in the PTSD group since groups did differ in terms of their primary diagnosis and their potential focus of psychopathology. An advantage of the described inclusion criteria is that we recruited the patients in a naturalistic setting, and that the samples are close to clinical reality. In the control group, we only included participants who were characterized by an absence of any current mental disorder.
In all samples, the following factors were defined as exclusion criteria: current psychotherapeutic treatment, lifetime diagnosis of schizophrenia or bipolar disorder, intellectual disability, current substance addiction, suicide attempt in the last 12 months or current high suicide risk, and a body mass index lower than 16.
Procedures
After a brief telephone screening, suitable participants received an invitation to our laboratory where they gave written informed consent and sociodemographic data were collected. Inclusion and exclusion criteria were assessed with the Structured Clinical Interview for DSM-IV (SCID-I; German version: Wittchen et al., 1997). Then, participants completed the MBE (Burg & Michalak, 2011) and filled out the questionnaires electronically using Unipark (QuestBack GmbH). The whole procedure lasted about 3 hr including a half-hour break, and all participants received monetary compensation. The samples were matched to achieve comparable groups in terms of gender and age. In total, we screened 184 participants on the phone (72 for the PTSD group, 60 for the depression group, 52 for the control group), conducted the SCID-I with 119 participants (44 for the PTSD group, 41 for the depression group, 34 for the control group), and included 99 participants (33 in each group) in the final sample.
Measures
The SCID-1 (Wittchen et al., 1997) was used to assess present Axis I diagnoses. As no German DSM-5-based structured clinical interviews existed at the start of the study, we assessed Axis I diagnoses according to the DSM-IV. In all groups, traumatic events were recorded during the SCID-I interview and if present, the occurrence of posttraumatic stress symptoms was assessed. In the PTSD group, traumatic events were additionally identified with the Life Events Checklist (LEC-5; Weathers et al., 2013), which is a self-report measure that assesses exposure to 17 different traumatic events.
Depression symptoms over the past 2 weeks were assessed using the Beck Depression Inventory (BDI-II; Beck et al., 1996; German version: Hautzinger et al., 2006) in the two clinical groups. The BDI-II consists of 21 items that are answered on a 4-point scale with at least four options of increasing intensity to choose from. The German version of the BDI-II is a reliable and valid measure for depression (Hautzinger et al., 2006). In the present study, internal consistency for the BDI-II was good (Cronbach’s α = 0.93 and McDonald’s ω = 0.93).
The Davidson Trauma Scale (DTS; Davidson et al., 1997) was used as a self-rating scale to assess the frequency and severity of posttraumatic stress symptoms in the PTSD group. It consists of 17 items that are rated on a 5-point scale ranging from 0 (not at all) to 4 (every day) for frequency and from 0 (not at all distressing) to 4 (extremely distressing) for severity. In the present study, results are reported for the three subscales (intrusions, avoidance, and hyperarousal). The DTS shows good reliability and validity (Davidson et al., 1997). In the present study, internal consistency was good for all three subscales (intrusions: Cronbach’s α = 0.89 and McDonald’s ω = 0.87; avoidance: Cronbach’s α = 0.88 and McDonald’s ω = 0.86; hyperarousal: Cronbach’s α = 0.89 and McDonald’s ω = 0.87).
We used the Five Facet Mindfulness Questionnaire (FFMQ; Baer et al., 2006; German Version: Michalak et al., 2016) to measure mindfulness by questionnaire. The FFMQ consists of 39 items, which assess five facets of mindfulness (see above). Items are rated on a 5-point scale ranging from 1 (never or very rarely true) to 5 (very often or always true). The psychometric properties and the construct validity of the FFMQ were found to be good for both the English (Baer et al., 2008) and the German version (Michalak et al., 2016). However, factor analyses suggest that the “observing” subscale should not be part of the overarching mindfulness construct among non-meditators (Baer et al., 2006; Gu et al., 2016; Williams et al., 2014) and in the context of clinical samples (Curtiss & Klemanski, 2014; Williams et al., 2014). Thus, we report results for a FFMQ total score without the “observing” scale and internal consistency was good in the present study (Cronbach’s α = 0.92 and McDonald’s ω = 0.93).
As an experience-sampling measure, we used the Mindful-Breathing Exercise (MBE; Burg & Michalak, 2011). In this exercise, participants were asked to stay in contact with their breath for 18 min. Acoustic signals were given at irregular intervals, and participants were asked to indicate by mouse click whether they are still in contact with their breath or whether their mind is wandering. Additionally, they were asked to indicate whenever they notice that their mind is wandering during the intervals between the signals. The MBE consisted of 22 phases of different lengths (20 to 80 s) that end with a signal tone. A score for the MBE was calculated by considering all phases of the MBE without mind wandering indicated during and at the end of the phase. A high score corresponds to many phases in the MBE without mind wandering.
Data Analyses
There were no missing values. To avoid confounding of the results by age and gender, we used a matched group design. Simple ANOVAs and chi-square tests were performed to detect group differences regarding sociodemographic data.
To test for associations between the MBE and the FFMQ total score (without “observing”) and FFMQ facets (Hypothesis I), we computed separate Pearson product-moment correlations (one-tailed) for all three groups.
To test for associations of the MBE and the FFMQ total score (without “observing”) with clinical variables (Hypothesis II), in a first step we computed Pearson product-moment correlations (one-tailed) of the MBE and the FFMQ with the DTS symptom clusters in the PTSD group, and with the BDI-II in the depression and control group. In order to assess incremental validity of the MBE, we performed multiple linear regressions entering both the MBE and the FFMQ simultaneously into the model predicting all three DTS symptom clusters in the PTSD group and the BDI-II in the depression and control group. As 81.9% of the PTSD group suffered from a comorbid depressive disorder, depression could function as a confounding variable. Therefore, we computed Pearson product-moment correlations of the MBE and the FFMQ with the BDI-II in the PTSD group. Furthermore, in order to control statistically for comorbid depressive symptoms in the PTSD group, we added the BDI-II as control variable into the model. We applied Cohen’s conventions (1988) to interpret the size of the correlations (r ≥ 0.10 small association; r ≥ 0.30 moderate association; r ≥ 0.50 large association). We found no violations of the assumptions regarding Pearson product-moment correlations for Hypotheses I and II. Regarding the performed regression models (Hypothesis II), we did not detect any violations in terms of outlying values, nonlinearity, heteroscedasticity, auto-correlations among predictors, or multicollinearity. We found one violation to the normality assumption in the prediction of the BDI-II in the control group. However, in line with recommendations by Schmidt and Finan (2018), we decided against any outcome transformations, especially as regression models seem to be relatively robust to violations of the normality assumption.
To test for group differences (Hypothesis III), we conducted two separate ANOVAs (in-between design) for the MBE and the FFMQ total score (without “observing”) as dependent variables and the three groups as independent variables. Simple contrasts were used for pairwise comparisons. To counteract the problem of multiple comparisons, Bonferroni correction was used. Effect sizes were assessed via Cohen’s d (Cohen, 1988; d = 0.20 small effect, d = 0.50 medium effect, d = 0.80 large effect). No violation of ANOVA assumptions was found in the Shapiro-Wilk test and Levene’s test.
Results
Sample Characteristics
Sociodemographic data for the three groups are presented in Table 1. In terms of group differences, the control group had higher levels of education than the two clinical groups. Furthermore, the control group had lower levels of depressive symptoms (BDI-II) than the two clinical groups, while the two clinical groups did not differ significantly. Compared to the PTSD group, the proportion of those who experienced a traumatic event in the past was lower in the depression group and in the control group. For prior experiences of mindfulness, results showed significant differences between the three groups with the highest percentage of prior mindfulness experience in the PTSD group and the lowest in the control group.
PTSD patients showed different index traumas: childhood sexual and/or physical abuse (14 patients, 42.4%), physical and/or sexual violence in adulthood (14 patients, 42.2%), witnessing a violent assault or sudden death of a close relative (3 patients, 6.1%), severe car or work accident (2 patients, 6.1%). The average number of traumatic event types experienced, as reported in the LEC, was 5.50 (SD = 2.93, range 1–10). The average duration of PTSD was 9.29 years (SD = 11.02, range 0.3–42). Thirty-one patients (93.93%) fulfilled the criteria for comorbid disorders according to the SCID-I interview. The average number of comorbid Axis I disorders was 1.94 (SD = 1.39, range 0–7). The most frequent Axis I diagnoses in addition to PTSD were depressive disorders (a total of 81.9% of patients, which is divided as follows: current episode/dysthymia/double depression: 60.7%; recurrent depressive disorder, currently in remission: 21.2%).
In the depression group, seven patients (21.2%) suffered from a first major depressive episode, 24 patients (72.7%) had a recurrent depressive disorder with an average of 5.12 episodes in the past (SD = 4.98, range 2–20), and two patients (6.1%) suffered from a double depression. According to SCID-I diagnostic, six patients (18.2%) were classified as having currently a mild episode, 21 patients (63.6%) as having a moderate episode, and six patients (18.2%) as having a severe episode. The average duration of the current depressive episode was 4.76 months (SD = 4.02, range 1–14).
Hypothesis I: Associations Between MBE and FFMQ
Table 2 shows correlations of the MBE with the FFMQ total score (without “observing”) and the FFMQ facets separately for all three groups. Regarding associations between the MBE and the FFMQ total score, analyses revealed no significant result in the PTSD group, a marginal significant moderate positive correlation in the depression group, and a highly significant moderate positive correlation in the control group. With regard to the FFMQ facets, in the PTSD group we found a significant moderate negative association with “nonjudging” and a significant moderate positive association with “nonreactivity.” In the depression group, marginal significant positive associations emerged for “acting with awareness” and “nonjudging.” In the control group, the MBE showed significant moderate positive correlations with all FFMQ facets except for “observing.”
Hypothesis II: Associations of MBE and FFMQ with Clinical Variables
Table 3 displays correlations of the MBE and the FFMQ total score (without “observing”) with clinical variables in all three groups. In the PTSD group, the MBE and the FFMQ showed a significant moderate negative correlation with DTS hyperarousal and a marginal significant small to moderate negative correlation with DTS intrusions while no significant correlations emerged with DTS avoidance. Furthermore, we found a moderate significant negative correlation of the BDI-II with the FFMQ in the PTSD group, while no association emerged with the MBE. In the depression group, analyses revealed significant moderate negative correlations of the MBE and the FFMQ with the BDI-II. In the control group, we found significant moderate to large negative correlations of both the MBE and the FFMQ with the BDI-II.
In a next step, we performed linear multiple regressions to predict the clinical variables based on the MBE and the FFMQ. Results are shown in Table 4. In the PTSD group, we performed regressions on the DTS symptom clusters of intrusions, avoidance, and hyperarousal and controlled statistically for the BDI-II since comorbidity of depression was high in the PTSD group. In the PTSD group, all three regression models were significant (DTS intrusions: F (3, 29) = 4.09, p = 0.015; DTS avoidance: F (3, 29) = 5.08, p = 0.006; DTS hyperarousal: F (3, 29) = 9.80, p < 0.001). The BDI-II as a control variable significantly contributed to the prediction of all three DTS symptom clusters. The MBE was a marginally significant predictor of DTS intrusions and a significant predictor of DTS hyperarousal, while the FFMQ was not significantly associated with these outcomes. In the depression and control group, we performed regressions on the BDI-II. Significant overall models emerged in both groups (depression group: F (2, 30) = 5.06, p = 0.013; control group: F (2, 30) = 14.39, p < 0.001) with the FFMQ as the only significant predictor.
Hypothesis III: MBE and FFMQ Group Differences
Means and standard deviations of the MBE and the FFMQ for the three groups are presented in Table 5. We found significant univariate group effects for the MBE (F (2, 96) = 3.21, p = 0.045) and the FFMQ (F (2, 96) = 38.22, p < 0.001). Table 5 presents the results of the pairwise comparisons and the corresponding effect sizes. Post hoc tests revealed that the PTSD and depression group had marginal significantly lower MBE and FFMQ scores compared to the control group. No significant differences were found between the two clinical groups in the MBE and the FFMQ.
Discussion
Various methodological concerns challenge the validity of questionnaire-based assessments of mindfulness and hint at the necessity of alternative assessment approaches, e.g., other self-report measures such as experience-sampling or behavioral assessments. Hence, the main goal of this study was to evaluate the potential added value of an experience-sampling approach in the clinical context of PTSD and depression. Therefore, we used the MBE (Burg & Michalak, 2011), which measures the capacity to cultivate a state of mindful awareness during a breathing meditation exercise. The MBE covers rather state-like aspects of mindfulness while the FFMQ assesses trait aspects and comprises multiple facets of mindfulness, e.g., “nonjudging” or “acting with awareness” (Baer et al., 2006).
We separately examined the associations between the MBE and the FFMQ for patients with PTSD and depression as well as for healthy individuals. The fact that we did not find a significant association between the MBE and the FFMQ total score in the PTSD group might be explained by PTSD-typical symptoms such as hyperarousal and intrusions, which might affect performance more during a meditative exercise like the MBE than in a retrospective self-report like the FFMQ. In contrast, in the depression group, the MBE showed a moderate correlation with the FFMQ total score. In the control group, this association turned out to be even moderate to large. Assuming that the MBE assesses rather state-like aspects and the FFMQ trait-like aspects of mindfulness, the results of the present study make an important contribution to the respective literature as previous findings actually indicated that state and trait mindfulness are not strongly related (Bravo et al., 2018; Tanay & Bernstein, 2013; Thompson & Waltz, 2007). However, these results were obtained in non-clinical samples only, and state mindfulness was assessed with retrospective questionnaires.
Regarding convergent validity, in the PTSD group, the MBE seems to assess unique aspects of mindfulness, which are not fully covered by the FFMQ. However, we did find a significant moderate positive correlation between the MBE and the FFMQ facet “nonreactivity.” Nonetheless, the FFMQ facet “nonjudging” showed a negative moderate association with the MBE which was unexpected. We attribute this paradoxical finding to our small sample size. Although we did not find any statistically relevant outliers, scatterplots revealed extreme values in the MBE for few PTSD patients which led to considerable changes in the correlation found with the FFMQ. Therefore, one alternative explanation for the non-significant association between the MBE and the FFMQ could be that self-assessments and self-perceptions of PTSD patients might be biased due to their symptomology.
In contrast to the correlational results obtained in the PTSD group, in the depression and in the control group, the positive associations between the MBE and the FFMQ total score indicate a certain conceptual overlap. In the depression group, “acting with awareness” and “nonjudging” seemed to be crucial for this finding as they were the only FFMQ facets which showed a marginal significant moderate negative association with the MBE. In the control group, all FFMQ facets except “observing” showed significant moderate positive correlations with the MBE. In previous studies with non-clinical samples, Burg and Michalak (2011) only found “acting with awareness” and “accepting without judgment” to positively correlate with the MBE, while results of Frewen et al. (2014) indicate that only “acting with awareness” reliably correlates with the MBAS. However, in line with our findings, a study by Levinson et al. (2014) delivered moderate positive correlations of the BCT with all mindfulness facets except “observing” in two different non-clinical samples as well.
Overall, the results of the present study make an important contribution to former results regarding associations between experience-sampling and questionnaire-based approaches of mindfulness. Nevertheless, the findings are quite heterogeneous. Additionally, despite certain similarities between MBE, MBAS, and BCT, these measurement approaches are not equivalent as they differ in terms of length, setting, and instructions given. Therefore, future research is needed to draw solid conclusions.
A further step of the study was to look at the association of the MBE and the FFMQ with clinical variables. In the PTSD group, no significant correlation emerged for the MBE and the BDI-II. However, in line with previous results (Barr et al., 2019; Schoorl et al., 2015), we found a significant negative moderate correlation of the FFMQ with the BDI-II. Furthermore, both the MBE and the FFMQ showed a moderate negative correlation with hyperarousal, which supports previous results regarding the FFMQ (Martin et al., 2018). Remarkably, in the regression analysis predicting hyperarousal while controlling for depression, the MBE remained significant, whereas the FFMQ did not significantly contribute to the prediction of hyperarousal. For intrusions, we found a marginally significant small to moderate negative correlation with the MBE. In contrast to previous results (Martin et al., 2018), the correlation with the FFMQ was not significant. Regression analysis predicting intrusions showed that when controlling for depression, again only the MBE was a marginally significant predictor. To sum up, the MBE seemed to be superior to the FFMQ in terms of its predictive value for hyperarousal and intrusions.
Compared to healthy controls, PTSD patients in our study showed reduced levels of mindfulness in both the MBE and the FFMQ, which is in line with previous research assessing mindfulness with questionnaires (e.g., Basharpoor et al., 2015). We extended these findings following a multi-measurement approach using both the MBE and the FFMQ, which allowed us to gain more specific insights: Whereas impairments in the FFMQ in the PTSD group seem to be associated with comorbid depressive symptoms, impairments in the MBE might be associated with PTSD-specific symptomology. Thus, an elevated level of arousal and reactivity (e.g., hypervigilance, problems with concentration, and sleep disturbances; American Psychiatric Association, 2013) seems to impair patients’ abilities in a naturalistic meditative exercise such as the MBE. In this context, increased intrusions might be associated with difficulties focusing on one’s breathing due to more mind wandering and distractions caused by distressing trauma-related thoughts, feelings, and memories.
In contrast to our hypothesis, we found no association of the MBE and the FFMQ with avoidance in the PTSD group. This is surprising as previous studies indicated associations of several mindfulness facets with avoidance (Thompson & Waltz, 2010), and also from a theoretical point of view, avoiding trauma-related feelings, memories, and thoughts seems to be opposed to a mindful coping strategy. Further research is needed to clarify potential associations between PTSD-specific avoidance and mindfulness.
In the depression and control group, analyses yielded negative moderate associations of the MBE with the BDI-II. With this, we replicated findings of Burg and Michalak (2011) showing a similar association in a non-clinical sample, and extended them to a clinical sample of patients diagnosed with depression. Additionally, the FFMQ and the BDI-II showed negative correlations in both groups, which is in accordance with previous findings in samples of patients with depression (Argus & Thompson, 2008; Solem et al., 2015) and in samples of healthy individuals (e.g., Freudenthaler et al., 2017; López et al., 2016). Surprisingly, in regression models for both groups, the FFMQ turned out to be the only significant predictor. Thus, in these two groups, the MBE did not predict any unique variance of depressive symptoms above and beyond the FFMQ. The significant group differences in both measurement approaches between the depression and the control group are in line with previous findings concerning the FFMQ (e.g., Didonna et al., 2019) and the MBE (Rohde et al., 2014). The larger effect size we found for the FFMQ in this group comparison suggests that impairments in depressed patients might be more relevant in trait qualities of mindfulness assessed via questionnaires than in state aspects assessed with experience-sampling. One explanation might be that depressed patients’ evaluations of their abilities are negatively biased (e.g., Petersen et al., 2019; Serra-Blasco et al., 2019), which might result in an underestimation of their mindfulness skills in questionnaires.
Lastly, although we found distinct association patterns of the MBE and the FFMQ with psychopathology in the PTSD and depression group, we did not find differences between the two clinical groups in terms of their levels of mindfulness in both measurement approaches. The result with respect to the FFMQ might be explained by the high percentage of PTSD patients with comorbid depression in our sample. The results suggest that both clinical groups could benefit from mindfulness-based intervention, and we consider the findings of the present study to be quite notable for future evaluations of such interventions. Our findings emphasize the added value of the MBE to questionnaire-based assessments of mindfulness with respect to its predictive value for hyperarousal and intrusions. Future studies addressing mechanisms of change in PTSD symptomology might thus benefit from including the MBE in addition to questionnaire-based assessments of mindfulness. Nevertheless, the regression coefficients in the present study were still quite small and other factors explaining PTSD symptomology should be considered as well.
Limitations and Future Research
Our study has some limitations. Firstly, all our statistical analyses would have gained from a larger sample size; therefore, the results must be interpreted with due caution. In addition, Pearson product-moment correlations are relatively prone to outliers, which can be particularly relevant in the case of our small sample size leading to over- or underestimations of the actual associations.
Another limitation is the high comorbidity with depressive disorders in the PTSD group and the high self-reported level of depression in the BDI-II. However, the PTSD group we studied is representative of clinical reality where comorbidity with depression is particularly frequent (e.g., Nichter et al., 2019; Nickerson et al., 2017). In addition, 28.8% of the depression group and 12.1% of the control group had experienced past trauma, which is in line with the prevalence rate of traumatic life events in the general population (e.g., around 20%, Hauffa et al., 2011). Furthermore, the majority of the PTSD and depression group had prior experience with mindfulness, mostly due to participating in mindfulness group sessions during inpatient treatment. In contrast, in the control group only about 20% reported previous experience in mindfulness. This may have impaired the validity of the results of the group comparison: The differences between the two clinical groups and the control group might have turned out to be larger due to the patients’ prior experiences with mindfulness practice. Following van Dam et al. (2018), deficits could be perceived more strongly with increasing prior experience in mindfulness and thus lead to a lower FFMQ score. In contrast, inexperienced beginners, like the majority of the control group, might have a more naïve comprehension of the concept and therefore be prone to overestimating their mindfulness skills (Sauer et al., 2013).
A very important limitation of the present study is the absence of a questionnaire-based measurement approach of state mindfulness such as the Toronto Mindfulness Scale (TMS; Lau et al., 2006) or the State Mindfulness Scale (SMS; Tanay & Bernstein, 2013). Various previous studies followed a two-step protocol to measure state mindfulness: first, the completion of a short meditation exercise, and afterwards, the assessment of state mindfulness during the exercise via questionnaire-based self-reports (e.g., Bravo et al., 2018; Thompson & Waltz, 2007). In contrast to this procedure, we used the MBE, where participants are instructed to rate their current state of mindfulness directly during the meditation exercise, which avoids retrospective biases. Nevertheless, the present study would have benefitted from the inclusion of a questionnaire-based measure of state mindfulness additional to the MBE. This would have allowed us to empirically test our theoretical assumptions that the MBE captures rather state than trait-like aspects of mindfulness.
With respect to experience-sampling approaches, one major shortcoming lies in the fact that reporting one’s own experience during a meditation exercise is still based on self-reports (Csikszentmihalyi & Larson, 2014), which can lead to common biases (e.g., social desirability; Tracey, 2016). Furthermore, just like the FFMQ, the MBE is also prone to the contradictory effect of increased self-awareness leading to decreased mindfulness ratings: Being more aware of one’s absent-mindedness and more sensitive to mind wandering can still result in lower MBE scores. In contrast to the FFMQ, the MBE avoids any kind of semantic understanding of mindfulness concepts since participants only rate their current state of mindfulness by a simple mouse click. Therefore, self-ratings during the MBE might depend less on previous individual experience with mindfulness than self-ratings in questionnaires. In addition, the MBE avoids retrospective biases due to an immediate assessment of mindfulness during a meditation exercise in a task environment. Therefore, the MBE seems to be reliable and sensitive to measure attention-related aspects of mindfulness. Nevertheless, one disadvantage of the MBE is that it does not assess the attitudes of nonjudging, nonreactivity, and friendly curiosity that are often described as essential to mindfulness (Kabat-Zinn, 2015) and are assessed with the FFMQ. To sum up, the MBE and the FFMQ both have their specific benefits and shortcomings.
For future research, it would be of great interest to compare other existing experience-sampling approaches for mindfulness such as the BCT (Levinson et al., 2014) and the MBAS (Frewen et al., 2008), with the MBE (Burg & Michalak, 2011). Furthermore, future studies might examine the association of mindfulness based on experience-sampling with questionnaire-based measurements of both state (e.g., TMS; Lau et al., 2006) and trait mindfulness (such as the FFMQ). In the present study, we conducted analyses based on cross-sectional data, which do not allow any conclusions in terms of causality. Therefore, longitudinal analysis methods are required to interpret the direction of the association between mindfulness and psychopathology. Lastly, the present study has demonstrated different correlational patterns of the MBE and the FFMQ in the three groups, thus showing that results based on non-clinical samples cannot be generalized to patient groups. Therefore, future research on different measurement approaches of mindfulness might be advised to shift its focus more to clinical samples.
Data Availability
The dataset generated and analyzed during the current study is available from the corresponding author on reasonable request.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Argus, G., & Thompson, M. (2008). Perceived social problem solving, perfectionism, and mindful awareness in clinical depression: An exploratory study. Cognitive Therapy and Research, 32(6), 745–757. https://doi.org/10.1007/s10608-006-9102-1
Baer, R. A. (2019). Assessment of mindfulness by self-report. Current Opinion in Psychology, 28, 42–48. https://doi.org/10.1016/j.copsyc.2018.10.015
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27–45. https://doi.org/10.1177/1073191105283504
Baer, R. A., Smith, G. T., Lykins, E., Button, D., Krietemeyer, J., Sauer, S., Walsh, E., Duggan, D., & Williams, J. M. G. (2008). Construct validity of the Five Facet Mindfulness Questionnaire in meditating and nonmeditating samples. Assessment, 15(3), 329–342. https://doi.org/10.1177/1073191107313003
Baminiwatta, A., & Solangaarachchi, I. (2021). Trends and developments in mindfulness research over 55 years: A bibliometric analysis of publications indexed in web of science. Mindfulness, 12(9), 2099–2116. https://doi.org/10.1007/s12671-021-01681-x
Barr, N., Keeling, M., & Castro, C. (2019). Associations between mindfulness, PTSD, and depression in combat deployed post-9/11 military veterans. Mindfulness, 10(11), 2403–2414. https://doi.org/10.1007/s12671-019-01212-9
Basharpoor, S., Shafiei, M., & Daneshvar, S. (2015). The comparison of experimental avoidance, mindfulness and rumination in trauma-exposed individuals with and without posttraumatic stress disorder (PTSD) in an Iranian sample. Archives of Psychiatric Nursing, 29(5), 279–283. https://doi.org/10.1016/j.apnu.2015.05.004
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). BDI-II: Beck Depression Inventory: Manual (2nd ed.). Psychological corporation; Harcourt Brace.
Bergomi, C., Tschacher, W., & Kupper, Z. (2013). The assessment of mindfulness with self-report measures: Existing scales and open issues. Mindfulness, 4(3), 191–202. https://doi.org/10.1007/s12671-012-0110-9
Bodhi, B. (2011). What does mindfulness really mean? A canonical perspective. Contemporary Buddhism, 12(1), 19–39. https://doi.org/10.1080/14639947.2011.564813
Boughner, E., Thornley, E., Kharlas, D., & Frewen, P. (2016). Mindfulness-related traits partially mediate the association between lifetime and childhood trauma exposure and PTSD and dissociative symptoms in a community sample assessed online. Mindfulness, 7(3), 672–679. https://doi.org/10.1007/s12671-016-0502-3
Bravo, A. J., Lindsay, E. K., & Pearson, M. R. (2022). Nature, assessment, and mechanisms of mindfulness. In O. N. Medvedev, C. U. Krägeloh, R. J. Siegert, & N. N. Singh (Eds.), Handbook of assessment in mindfulness research (pp. 1–12). Springer. https://doi.org/10.1007/978-3-030-77644-2_2-1
Bravo, A. J., Pearson, M. R., Wilson, A. D., & Witkiewitz, K. (2018). When traits match states: Examining the associations between self-report trait and state mindfulness following a state mindfulness induction. Mindfulness, 9(1), 199–211. https://doi.org/10.1007/s12671-017-0763-5
Brown, K. W., & Ryan, R. M. (2003). The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84(4), 822–848. https://doi.org/10.1037/0022-3514.84.4.822
Burg, J. M., & Michalak, J. (2011). The healthy quality of mindful breathing: Associations with rumination and depression. Cognitive Therapy and Research, 35(2), 179–185. https://doi.org/10.1007/s10608-010-9343-x
Burg, J. M., & Michalak, J. (2012). Achtsamkeit, Selbstwert und Selbstwertstabilität. Zeitschrift für Klinische Psychologie und Psychotherapie, 41, 1–8. https://doi.org/10.1026/1616-3443/a000111
Burg, J. M., Wolf, O. T., & Michalak, J. (2012). Mindfulness as self-regulated attention: Associations with heart rate variability. Swiss Journal of Psychology, 71(3), 135–139. https://doi.org/10.1024/1421-0185/a000080
Carpenter, J. K., Conroy, K., Gomez, A. F., Curren, L. C., & Hofmann, S. G. (2019). The relationship between trait mindfulness and affective symptoms: A meta-analysis of the Five Facet Mindfulness Questionnaire (FFMQ). Clinical Psychology Review, 74, 101785. https://doi.org/10.1016/j.cpr.2019.101785
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Lawrence Earlbaum Associates.
Crowe, K., & McKay, D. (2016). Mindfulness, obsessive–compulsive symptoms, and executive dysfunction. Cognitive Therapy and Research, 40(5), 627–644. https://doi.org/10.1007/s10608-016-9777-x
Csikszentmihalyi, M., & Larson, R. (2014). Validity and reliability of the experience-sampling method. In M. Csikszentmihalyi (Ed.), Flow and the foundations of positive psychology: The collected works of Mihaly Csikszentmihalyi (pp. 35–54). Springer. https://doi.org/10.1007/978-94-017-9088-8_3
Curtiss, J., & Klemanski, D. H. (2014). Factor analysis of the Five Facet Mindfulness Questionnaire in a heterogeneous clinical sample. Journal of Psychopathology and Behavioral Assessment, 36(4), 683–694. https://doi.org/10.1007/s10862-014-9429-y
Davidson, J. R. T., Book, S. W., Colket, J. T., Tupler, L., Roth, S., David, D., Hertzberg, M., Mellman, T., Beckham, J. C., Smith, R. C., Davison, R. M., Kratz, R., & Feldmann, M. E. (1997). Assessment of a new self-rating scale for post-traumatic stress disorder. Psychological Medicine, 27(1), 153–160. https://doi.org/10.1017/S0033291796004229
Didonna, F., Rossi, R., Ferrari, C., Iani, L., Pedrini, L., Rossi, N., Xodo, E., & Lanfredi, M. (2019). Relations of mindfulness facets with psychological symptoms among individuals with a diagnosis of obsessive-compulsive disorder, major depressive disorder, or borderline personality disorder. Psychology and Psychotherapy, 92(1), 112–130. https://doi.org/10.1111/papt.12180
Falkenström, F. (2010). Studying mindfulness in experienced meditators: A quasi-experimental approach. Personality and Individual Differences, 48(3), 305–310. https://doi.org/10.1016/j.paid.2009.10.022
Feng, X. J., Krägeloh, C. U., Billington, D. R., & Siegert, R. J. (2018). To what extent is mindfulness as presented in commonly used mindfulness questionnaires different from how it is conceptualized by senior ordained Buddhists? Mindfulness, 9(2), 441–460. https://doi.org/10.1007/s12671-017-0788-9
Freudenthaler, L., Turba, J. D., & Tran, U. S. (2017). Emotion regulation mediates the associations of mindfulness on symptoms of depression and anxiety in the general population. Mindfulness, 8(5), 1339–1344. https://doi.org/10.1007/s12671-017-0709-y
Frewen, P., Evans, E. M., Maraj, N., Dozois, D. J. A., & Partridge, K. (2008). Letting go: Mindfulness and negative automatic thinking. Cognitive Therapy and Research, 32(6), 758–774. https://doi.org/10.1007/s12671-011-0069-y
Frewen, P., Lundberg, E., MacKinley, J., & Wrath, A. (2011). Assessment of response to mindfulness meditation: Meditation breath attention scores in association with subjective measures of state and trait mindfulness and difficulty letting go of depressive cognition. Mindfulness, 2(4), 254–269. https://doi.org/10.1007/s12671-011-0069-y
Frewen, P. A., Unholzer, F., Logie-Hagan, K. R. J., & MacKinley, J. D. (2014). Meditation Breath Attention Scores (MBAS): Test–retest reliability and sensitivity to repeated practice. Mindfulness, 5, 161–169.
Goldberg, S. B., Wielgosz, J., Dahl, C., Schuyler, B., MacCoon, D. S., Rosenkranz, M., Lutz, A., Sebranek, C. A., & Davidson, R. J. (2016). Does the Five Facet Mindfulness Questionnaire measure what we think it does? Construct validity evidence from an active controlled randomized clinical trial. Psychological Assessment, 28(8), 1009–1014. https://doi.org/10.1037/pas0000233
Grossman, P. (2008). On measuring mindfulness in psychosomatic and psychological research. Journal of Psychosomatic Research, 64(4), 405–408. https://doi.org/10.1016/j.jpsychores.2008.02.001
Gu, J., Strauss, C., Crane, C., Barnhofer, T., Karl, A., Cavanagh, K., & Kuyken, W. (2016). Examining the factor structure of the 39-item and 15-item versions of the Five Facet Mindfulness Questionnaire before and after mindfulness-based cognitive therapy for people with recurrent depression. Psychological Assessment, 28(7), 791–802. https://doi.org/10.1037/pas0000263
Hauffa, R., Rief, W., Brähler, E., Martin, A., Mewes, R., & Glaesmer, H. (2011). Lifetime traumatic experiences and posttraumatic stress disorder in the German population: Results of a representative population survey. The Journal of Nervous and Mental Disease, 199(12), 934–939.
Hautzinger, M., Keller, F., & Kühner, C. (2006). Becks Depressions-Inventar (BDI-II). Hartcourt Test Services.
Hopwood, T. L., & Schutte, N. S. (2017). A meta-analytic investigation of the impact of mindfulness-based interventions on post traumatic stress. Clinical Psychology Review, 57, 12–20. https://doi.org/10.1016/j.cpr.2017.08.002
Isbel, B., Stefanidis, K., & Summers, M. J. (2020). Assessing mindfulness: Experimental support for the discriminant validity of breath counting as a measure of mindfulness but not self-report questionnaires. Psychological Assessment, 32(12), 1184–1190. https://doi.org/10.1037/pas0000957
Kabat-Zinn, J. (1994). Wherever you go, there you are: Mindfulness meditation in everyday life. Hyperion.
Kabat-Zinn, J. (2015). Mindfulness. Mindfulness, 6(6), 1481–1483. https://doi.org/10.1007/s12671-015-0456-x
Lau, M. A., Bishop, S. R., Segal, Z. V., Buis, T., Anderson, N. D., Carlson, L., Shapiro, S., & Carmody, J. (2006). The Toronto Mindfulness Scale: Development and validation. Journal of Clinical Psychology, 62(12), 1445–1467. https://doi.org/10.1002/jclp.20326
Lecuona, O., García-Garzón, E., García-Rubio, C., & Rodríguez-Carvajal, R. (2020). A psychometric review and conceptual replication study of the Five Facets Mindfulness Questionnaire latent structure. Assessment, 27(5), 859–872. https://doi.org/10.1177/1073191119873718
Levinson, D. B., Stoll, E. L., Kindy, S. D., Merry, H. L., & Davidson, R. J. (2014). A mind you can count on: Validating breath counting as a behavioral measure of mindfulness. Frontiers in Psychology, 5, 1202. https://doi.org/10.3389/fpsyg.2014.01202
López, A., Sanderman, R., & Schroevers, M. J. (2016). Mindfulness and self-compassion as unique and common predictors of affect in the general population. Mindfulness, 7(6), 1289–1296. https://doi.org/10.1007/s12671-016-0568-y
Ma, S. H., & Teasdale, J. D. (2004). Mindfulness-based cognitive therapy for depression: Replication and exploration of differential relapse prevention effects. Journal of Consulting and Clinical Psychology, 72(1), 31. https://doi.org/10.1037/0022-006X.72.1.31
Manuel, J. A., Somohano, V. C., & Bowen, S. (2017). Mindfulness practice and its relationship to the Five-Facet Mindfulness Questionnaire. Mindfulness, 8(2), 361–367. https://doi.org/10.1007/s12671-016-0605-x
Martin, C. E., Bartlett, B. A., Reddy, M. K., Gonzalez, A., & Vujanovic, A. A. (2018). Associations between mindfulness facets and PTSD symptom severity in psychiatric inpatients. Mindfulness, 9(5), 1571–1583. https://doi.org/10.1007/s12671-018-0904-5
Medvedev, O. N., Krägeloh, C. U., Siegert, R. J., & Singh, N. N. (2022). An introduction to assessment in mindfulness research. In O. N. Medvedev, C. U. Krägeloh, R. J. Siegert, & N. N. Singh (Eds.), Handbook of assessment in mindfulness research (pp. 1–11). Springer. https://doi.org/10.1007/978-3-030-77644-2_1-1
Michalak, J., Zarbock, G., Drews, M., Otto, D., Mertens, D., Ströhle, G., Schwinger, M., Dahme, B., & Heidenreich, T. (2016). Erfassung von Achtsamkeit mit der deutschen Version des Five Facet Mindfulness Questionnaires (FFMQ-D). Zeitschrift für Gesundheitspsychologie, 24(1), 1–12. https://doi.org/10.1026/0943-8149/a000149
Müller-Engelmann, M., Schreiber, C., Kümmerle, S., Heidenreich, T., Stangier, U., & Steil, R. (2019). A trauma-adapted mindfulness and loving-kindness intervention for patients with PTSD after interpersonal violence: A multiple-baseline study. Mindfulness, 10(6), 1105–1123. https://doi.org/10.1007/s12671-018-1068-z
Nichter, B., Norman, S., Haller, M., & Pietrzak, R. H. (2019). Psychological burden of PTSD, depression, and their comorbidity in the US veteran population: Suicidality, functioning, and service utilization. Journal of Affective Disorders, 256, 633–640. https://doi.org/10.1016/j.jad.2019.06.072
Nickerson, A., Schick, M., Schnyder, U., Bryant, R. A., & Morina, N. (2017). Comorbidity of posttraumatic stress disorder and depression in tortured, treatment-seeking refugees. Journal of Traumatic Stress, 30(4), 409–415. https://doi.org/10.1002/jts.22205
Orsillo, S. M., & Batten, S. V. (2005). Acceptance and commitment therapy in the treatment of posttraumatic stress disorder. Behavior Modification, 29(1), 95–129. https://doi.org/10.1177/0145445504270876
Petersen, J. Z., Porter, R. J., & Miskowiak, K. W. (2019). Clinical characteristics associated with the discrepancy between subjective and objective cognitive impairment in depression. Journal of Affective Disorders, 246, 763–774. https://doi.org/10.1016/j.jad.2018.12.105
Rohde, K., Adolph, D., Dietrich, D. E., & Michalak, J. (2014). Mindful attention regulation and non-judgmental orientation in depression: A multi-method approach. Biological Psychology, 101, 36–43. https://doi.org/10.1016/j.biopsycho.2014.06.009
Sauer, S., Walach, H., Schmidt, S., Hinterberger, T., Lynch, S., Büssing, A., & Kohls, N. (2013). Assessment of mindfulness: Review on state of the art. Mindfulness, 4(1), 3–17. https://doi.org/10.1007/s12671-012-0122-5
Schmidt, A. F., & Finan, C. (2018). Linear regression and the normality assumption. Journal of Clinical Epidemiology, 98, 146–151. https://doi.org/10.1016/j.jclinepi.2017.12.006
Schoorl, M., van Mil-Klinkenberg, L., & van der Does, W. (2015). Mindfulness skills, anxiety sensitivity, and cognitive reactivity in patients with posttraumatic stress disorder. Mindfulness, 6(5), 1004–1011. https://doi.org/10.1007/s12671-014-0346-7
Schut, D. M., & Boelen, P. A. (2017). The relative importance of rumination, experiential avoidance and mindfulness as predictors of depressive symptoms. Journal of Contextual Behavioral Science, 6(1), 8–12. https://doi.org/10.1016/j.jcbs.2016.11.008
Serra-Blasco, M., Torres, I. J., Vicent-Gil, M., Goldberg, X., NavarraVentura, G., Aguilar, E., Via, E., Portella, M. J., Figuereo, I., Palao, D., Lam, R. W., & Cardoner, N. (2019). Discrepancy between objective and subjective cognition in major depressive disorder. European Neuropsychopharmacology, 29(1), 46–56. https://doi.org/10.1016/j.euroneuro.2018.11.1104
Solem, S., Hagen, R., Wang, C. E. A., Hjemdal, O., Waterloo, K., Eisemann, M., & Halvorsen, M. (2015). Metacognitions and mindful attention awareness in depression: A comparison of currently depressed, previously depressed and never depressed individuals. Clinical Psychology & Psychotherapy, 24(1), 94–102. https://doi.org/10.1002/cpp.1983
Tanay, G., & Bernstein, A. (2013). State Mindfulness Scale (SMS): Development and initial validation. Psychological Assessment, 25(4), 1286–1299. https://doi.org/10.1037/a0034044
Taylor, J., McLean, L., Korner, A., Stratton, E., & Glozier, N. (2020). Mindfulness and yoga for psychological trauma: Systematic review and meta-analysis. Journal of Trauma & Dissociation, 21(5), 536–573. https://doi.org/10.1080/15299732.2020.1760167
Teasdale, J. D., Moore, R. G., Hayhurst, H., Pope, M., Williams, S., & Segal, Z. V. (2002). Metacognitive awareness and prevention of relapse in depression: Empirical evidence. Journal of Consulting and Clinical Psychology, 70(2), 275–287. https://doi.org/10.1037/0022-006X.70.2.275
Thompson, B. L., & Waltz, J. (2007). Everyday mindfulness and mindfulness meditation: Overlapping constructs or not? Personality and Individual Differences, 43(7), 1875–1885. https://doi.org/10.1016/j.paid.2007.06.017
Thompson, B. L., & Waltz, J. (2010). Mindfulness and experiential avoidance as predictors of posttraumatic stress disorder avoidance symptom severity. Journal of Anxiety Disorders, 24(4), 409–415. https://doi.org/10.1016/j.janxdis.2010.02.005
Thompson, R. W., Arnkoff, D. B., & Glass, C. R. (2011). Conceptualizing mindfulness and acceptance as components of psychological resilience to trauma. Trauma, Violence, & Abuse, 12(4), 220–235. https://doi.org/10.1177/1524838011416375
Tomlinson, E. R., Yousaf, O., Vittersø, A. D., & Jones, L. (2018). Dispositional mindfulness and psychological health: A systematic review. Mindfulness, 9(1), 23–43. https://doi.org/10.1007/s12671-017-0762-6
Tracey, T. J. G. (2016). A note on socially desirable responding. Journal of Counseling Psychology, 63(2), 224–232. https://doi.org/10.1037/cou0000135
Van Dam, N. T., van Vugt, M. K., Vago, D. R., Schmalzl, L., Saron, C. D., Olendzki, A., Meissner, T., Lazar, S. W., Kerr, C. E., Gorchov, J., Fox, K. C. R., Field, B. A., Britton, W. B., & Meyer, D. E. (2018). Mind the hype: A critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspectives on Psychological Science, 13(1), 36–61. https://doi.org/10.1177/1745691617709589
van der Velden, A. M., Kuyken, W., Wattar, U., Crane, C., Pallesen, K. J., Dahlgaard, J., Fjorback, L., & Piet, J. (2015). A systematic review of mechanisms of change in mindfulness-based cognitive therapy in the treatment of recurrent major depressive disorder. Clinical Psychology Review, 37, 26–39. https://doi.org/10.1016/j.cpr.2015.02.001
Wahbeh, H., Lu, M., & Oken, B. (2011). Mindful awareness and non-judging in relation to posttraumatic stress disorder symptoms. Mindfulness, 2(4), 219–227. https://doi.org/10.1007/s12671-011-0064-3
Walser, R. D., & Hayes, S. C. (2006). Acceptance and commitment therapy in the treatment of posttraumatic stress disorder. Cognitive-Behavioral Therapies for Trauma, 2, 146–172.
Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013). The Life Events Checklist for DSM-5 (LEC-5). Instrument available from the National Center for PTSD at www.ptsd.va.gov
Williams, M. J., Dalgleish, T., Karl, A., & Kuyken, W. (2014). Examining the factor structures of the Five Facet Mindfulness Questionnaire and the Self-Compassion Scale. Psychological Assessment, 26(2), 407–418. https://doi.org/10.1037/a0035566
Wittchen, H. U., Wunderlich, U., Gruschwitz, S., & Zaudig, M. (1997). SCID I - Manual of the German version. Hogrefe.
Acknowledgements
We thank Anne Wagner, Madeleine Graef, Corinna Schreiber, Maria van Recum, and Felix Kolb for their cooperation and help.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
S.K.: designed and executed the study, analyzed the data, and wrote the paper. T.H.: collaborated with the design of the study and the editing of the final manuscript. M.M.-E.: designed the study, collaborated with the writing of the paper and editing of the final manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in this study were in accordance with the ethical standards of the institution and with the 1964 Helsinki Declaration and its later amendments. The ethics committee of Goethe-University of Frankfurt am Main approved this study (reference number: 210/16).
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kümmerle, S., Heidenreich, T. & Müller-Engelmann, M. Beyond Mindfulness Assessed by Questionnaires: The Mindful-Breathing Exercise as an Additional Approach in PTSD and Depression. Mindfulness 14, 919–932 (2023). https://doi.org/10.1007/s12671-023-02093-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-023-02093-9