Abstract
Purpose
Perioperative pulmonary hypertension (PH) is an independent risk factor for morbidity and mortality in cardiac surgery. While inhaled prostacyclins (iPGI2s) are an established treatment of chronic PH, data on the efficacy of iPGI2s in perioperative PH are scarce.
Methods
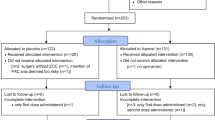
We searched PubMed, Embase, the Web of Science, CENTRAL, and the grey literature from inception until April 2021. We included randomized controlled trials investigating the use of iPGI2s in adult and pediatric patients undergoing cardiac surgery with an increased risk of perioperative right ventricle failure. We assessed the efficacy and safety of iPGI2s compared with placebo and other inhaled or intravenous vasodilators with random-effect meta-analyses. The primary outcome was mean pulmonary artery pressure (MPAP). Secondary outcomes included other hemodynamic parameters and mortality.
Results
Thirteen studies were included, comprising 734 patients. Inhaled prostacyclins significantly decreased MPAP compared with placebo (standardized effect size, 0.46; 95% confidence interval [CI], 0.11 to 0.87; P = 0.01) and to intravenous vasodilators (1.26; 95% CI, 0.03 to 2.49; P = 0.045). Inhaled prostacyclins significantly improved the cardiac index compared with intravenous vasodilators (1.53; 95% CI, 0.50 to 2.57; P = 0.004). In contrast, mean arterial pressure was significantly lower in patients treated with iPGI2s vs placebo (−0.39; 95% CI, −0.62 to 0.16; P = 0.001), but higher than in patients treated with intravenous vasodilators (0.81; 95% CI, 0.29 to 1.33; P = 0.002). With respect to hemodynamics, iPGI2s had similar effects as other inhaled vasodilators. Mortality was not affected by iPGI2s.
Conclusion
The results of this systematic review and meta-analysis show that iPGI2s improved pulmonary hemodynamics with similar efficacy as other inhaled vasodilators, but caused a significant small decrease in arterial pressure when compared with placebo, indicating spill-over into the systemic circulation. These effects did not affect clinical outcomes.
Study registration date
PROSPERO (CRD42021237991); registered 26 May 2021.
Résumé
Objectif
L’hypertension pulmonaire (HTAP) périopératoire est un facteur de risque indépendant de morbidité et de mortalité en chirurgie cardiaque. Bien que l’inhalation de prostacyclines (iPGI2) constitue un traitement établi de l’HTAP chronique, les données sur l’efficacité de ce traitement en cas d’HTAP périopératoire sont rares.
Méthode
Nous avons effectué des recherches dans les bases de données PubMed, Embase, Web of Science, CENTRAL et dans la littérature grise depuis leur création jusqu’en avril 2021. Nous avons inclus des études randomisées contrôlées portant sur l’utilisation de l’iPGI2 chez la patientèle adulte et pédiatrique bénéficiant d’une chirurgie cardiaque avec un risque accru d’insuffisance ventriculaire droite périopératoire. Nous avons évalué l’efficacité et l’innocuité des iPGI2 par rapport à un placebo et à d’autres vasodilatateurs inhalés ou intraveineux avec des méta-analyses à effets aléatoires. Le critère d’évaluation principal était la pression artérielle pulmonaire moyenne (PAPm). Les critères d’évaluation secondaires incluaient d’autres paramètres hémodynamiques et la mortalité.
Résultats
Treize études portant sur 734 patient·es ont été incluses. Les prostacyclines inhalées ont diminué de manière significative la PAPm par rapport au placebo (taille d’effet standardisée, 0,46; intervalle de confiance [IC] à 95 %, 0,11 à 0,87; P = 0,01) et aux vasodilatateurs intraveineux (1,26; IC 95 %, 0,03 à 2,49; P = 0,045). Les prostacyclines inhalées ont significativement amélioré l’index cardiaque par rapport aux vasodilatateurs intraveineux (1,53; IC 95 %, 0,50 à 2,57; P = 0,004). En revanche, la pression artérielle moyenne était significativement plus faible chez les patient·es traité·es par iPGI2 vs placebo (−0,39; IC 95 %, −0,62 à 0,16; P = 0,001), mais plus élevée que chez les personnes traitées par vasodilatateurs intraveineux (0,81; IC 95 %, 0,29 à 1,33; P = 0,002). En ce qui concerne l’hémodynamie, les iPGI2 ont eu des effets similaires à ceux des autres vasodilatateurs inhalés. La mortalité n’a pas été affectée par les iPGI2.
Conclusion
Les résultats de cette revue systématique et méta-analyse montrent que les iPGI2 ont amélioré l’hémodynamie pulmonaire avec une efficacité similaire à celle des autres vasodilatateurs inhalés, mais ont entraîné une diminution légère mais significative de la pression artérielle par rapport au placebo, indiquant un débordement dans la circulation systémique. Ces effets n’ont pas affecté les résultats cliniques.
Enregistrement de l’étude
PROSPERO (CRD42021237991); enregistrée le 26 mai 2021.


Similar content being viewed by others
References
Roques F, Nashef SA, Michel P, et al. Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg 1999; 15: 816–22. https://doi.org/10.1016/s1010-7940(99)00106-2
Dávila-Román VG, Waggoner AD, Hopkins WE, Barzilai B. Right ventricular dysfunction in low output syndrome after cardiac operations: assessment by transesophageal echocardiography. Ann Thorac Surg 1995; 60: 1081–6. https://doi.org/10.1016/0003-4975(95)00526-q
Levy D, Laghlam D, Estagnasie P, Brusset A, Squara P, Nguyen LS. Post-operative right ventricular failure after cardiac surgery: a cohort study. Front Cardiovasc Med 2021; 8: 667328. https://doi.org/10.3389/fcvm.2021.667328
Sarkar MS, Desai PM. Pulmonary hypertension and cardiac anesthesia: anesthesiologist's perspective. Ann Card Anaesth 2018; 21: 116–22. https://doi.org/10.4103/aca.aca_123_17
Kaplan JA, Finlayson DC, Woodward S. Vasodilator therapy after cardiac surgery: a review of the efficacy and toxicity of nitroglycerin and nitroprusside. Can Anaesth Soc J 1980; 27: 254–9. https://doi.org/10.1007/bf03007436
Wilkins MR, Wharton J, Grimminger F, Ghofrani HA. Phosphodiesterase inhibitors for the treatment of pulmonary hypertension. Eur Respir J 2008; 32: 198–209. https://doi.org/10.1183/09031936.00124007
Mandal B, Kapoor PM, Chowdhury U, Kiran U, Choudhury M. Acute hemodynamic effects of inhaled nitroglycerine, intravenous nitroglycerine, and their combination with intravenous dobutamine in patients with secondary pulmonary hypertension. Ann Card Anaesth 2010; 13: 138–44. https://doi.org/10.4103/0971-9784.62946
Olschewski H, Simonneau G, Galiè N, et al. Inhaled iloprost for severe pulmonary hypertension. N Engl J Med 2002; 347: 322–9. https://doi.org/10.1056/nejmoa020204
Rao V, Ghadimi K, Keeyapaj W, Parsons CA, Cheung AT. Inhaled nitric oxide (iNO) and inhaled epoprostenol (iPGI2) use in cardiothoracic surgical patients: is there sufficient evidence for evidence-based recommendations? J Cardiothorac Vasc Anesth 2018; 32: 1452–7. https://doi.org/10.1053/j.jvca.2017.12.014
Winterhalter M, Antoniou T, Loukanov T. Management of adult patients with perioperative pulmonary hypertension: technical aspects and therapeutic options. Cardiology 2010; 116: 3–9. https://doi.org/10.1159/000313863
Langer F, Wilhelm W, Tscholl D, et al. Intraoperative inhalation of the long-acting prostacyclin analog iloprost for pulmonary hypertension. J Thorac Cardiovasc Surg 2003; 126: 874–5. https://doi.org/10.1016/s0022-5223(03)00704-9
Rex S, Busch T, Vettelschoss M, de Rossi L, Rossaint R, Buhre W. Intraoperative management of severe pulmonary hypertension during cardiac surgery with inhaled iloprost. Anesthesiology 2003; 99: 745–7. https://doi.org/10.1097/00000542-200309000-00033
Lowson SM, Doctor A, Walsh BK, Doorley PA. Inhaled prostacyclin for the treatment of pulmonary hypertension after cardiac surgery. Crit Care Med 2002; 30: 2762–4. https://doi.org/10.1097/00003246-200212000-00023
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009; 339: b2700. https://doi.org/10.1136/bmj.b2700
Forrest P. Anaesthesia and right ventricular failure. Anaesth Intensive Care 2009; 37: 370–85. https://doi.org/10.1177/0310057x0903700314
Konstam MA, Kiernan MS, Bernstein D, et al. Evaluation and management of right-sided heart failure: a scientific statement from the American Heart Association. Circulation 2018; 137: e578–622. https://doi.org/10.1161/cir.0000000000000560
Haddad F, Doyle R, Murphy DJ, Hunt SA. Right ventricular function in cardiovascular disease, part II: pathophysiology, clinical importance, and management of right ventricular failure. Circulation 2008; 117: 1717–31. https://doi.org/10.1161/circulationaha.107.653584
Simonneau G, Gatzoulis MA, Adatia I, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol 2013; 62: D34–41. https://doi.org/10.1016/j.jacc.2013.10.029
Simonneau G, Montani D, Celermajer DS, et al. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J 2019; 53: 1801913. https://doi.org/10.1183/13993003.01913-2018
Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011; 343: d5928. https://doi.org/10.1136/bmj.d5928
Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 2018; 27: 1785–805. https://doi.org/10.1177/0962280216669183
DerSimonian R, Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials 2015; 45: 139–45. https://doi.org/10.1016/j.cct.2015.09.002
Haché M, Denault A, Bélisle S, et al. Inhaled epoprostenol (prostacyclin) and pulmonary hypertension before cardiac surgery. J Thorac Cardiovasc Surg 2003; 125: 642–9. https://doi.org/10.1067/mtc.2003.107
Kramm T, Eberle B, Guth S, Mayer E. Inhaled iloprost to control residual pulmonary hypertension following pulmonary endarterectomy. Eur J Cardiothorac Surg 2005; 28: 882–8. https://doi.org/10.1016/j.ejcts.2005.09.007
Xu Z, Zhu L, Liu X, Gong X, Gattrell W, Liu J. Iloprost for children with pulmonary hypertension after surgery to correct congenital heart disease. Pediatr Pulmonol 2015; 50: 588–95. https://doi.org/10.1002/ppul.23032
Winterhalter M, Rex S, Stoppe C, et al. Effect of iloprost inhalation on postoperative outcome in high-risk cardiac surgical patients: a prospective randomized-controlled multicentre trial (ILOCARD). Can J Anesth 2019; 66: 907–20. https://doi.org/10.1007/s12630-019-01309-8
Winterhalter M, Simon A, Fischer S, et al. Comparison of inhaled iloprost and nitric oxide in patients with pulmonary hypertension during weaning from cardiopulmonary bypass in cardiac surgery: a prospective randomized trial. J Cardiothorac Vasc Anesth 2008; 22: 406–13. https://doi.org/10.1053/j.jvca.2007.10.015
Loukanov T, Bucsenez D, Springer W, et al. Comparison of inhaled nitric oxide with aerosolized iloprost for treatment of pulmonary hypertension in children after cardiopulmonary bypass surgery. Clin Res Cardiol 2011; 100: 595–602. https://doi.org/10.1007/s00392-011-0284-5
Kirbas A, Yalcin Y, Tanrikulu N, Gürer O, Isik O. Comparison of inhaled nitric oxide and aerosolized iloprost in pulmonary hypertension in children with congenital heart surgery. Cardiol J 2012; 19: 387–94. https://doi.org/10.5603/cj.2012.0070
Abe S, Ishida K, Masuda M, et al. A prospective, randomized study of inhaled prostacyclin versus nitric oxide in patients with residual pulmonary hypertension after pulmonary endarterectomy. Gen Thorac Cardiovasc Surg 2017; 65: 153–9. https://doi.org/10.1007/s11748-016-0724-2
Hegazy N. Comparison of hemodynamic effects of inhaled milrinone and inhaled prostacyclin after adult cardiac surgery. J Appl Sci Res 2010; 6: 38–44.
Yurtseven N, Karaca P, Uysal G, et al. A comparison of the acute hemodynamic effects of inhaled nitroglycerin and iloprost in patients with pulmonary hypertension undergoing mitral valve surgery. Ann Thorac Cardiovasc Surg 2006; 12: 319–23.
Fattouch K, Sbraga F, Bianco G, et al. Inhaled prostacyclin, nitric oxide, and nitroprusside in pulmonary hypertension after mitral valve replacement. J Card Surg 2005; 20: 171–6. https://doi.org/10.1111/j.0886-0440.2005.200383w.x
Fattouch K, Sbraga F, Sampognaro R, et al. Treatment of pulmonary hypertension in patients undergoing cardiac surgery with cardiopulmonary bypass: a randomized, prospective, double-blind study. J Cardiovasc Med (Hagerstown) 2006; 7: 119–23. https://doi.org/10.2459/01.jcm.0000203850.97890.fe
Rex S, Schaelte G, Metzelder S, et al. Inhaled iloprost to control pulmonary artery hypertension in patients undergoing mitral valve surgery: a prospective, randomized-controlled trial. Acta Anaesthesiol Scand 2008; 52: 65–72. https://doi.org/10.1111/j.1399-6576.2007.01476.x
Theodoraki K, Tsiapras D, Tsourelis L, et al. Inhaled iloprost in eight heart transplant recipients presenting with post-bypass acute right ventricular dysfunction. Acta Anaesthesiol Scand 2006; 50: 1213–7. https://doi.org/10.1111/j.1399-6576.2006.01139.x
Theodoraki K, Rellia P, Thanopoulos A, et al. Inhaled iloprost controls pulmonary hypertension after cardiopulmonary bypass. Can J Anesth 2002; 49: 963–7. https://doi.org/10.1007/bf03016884
Price LC, Wort SJ, Finney SJ, Marino PS, Brett SJ. Pulmonary vascular and right ventricular dysfunction in adult critical care: current and emerging options for management: a systematic literature review. Crit Care 2010; 14: R169. https://doi.org/10.1186/cc9264
Elmi-Sarabi M, Deschamps A, Delisle S, et al. Aerosolized vasodilators for the treatment of pulmonary hypertension in cardiac surgical patients: a systematic review and meta-analysis. Anesth Analg 2017; 125: 393–402. https://doi.org/10.1213/ane.0000000000002138
Rex S, Missant C, Segers P, Rossaint R, Wouters PF. Epoprostenol treatment of acute pulmonary hypertension is associated with a paradoxical decrease in right ventricular contractility. Intensive Care Med 2008; 34: 179–89. https://doi.org/10.1007/s00134-007-0831-8
Rex S, Missant C, Claus P, Buhre W, Wouters PF. Effects of inhaled iloprost on right ventricular contractility, right ventriculo-vascular coupling and ventricular interdependence: a randomized placebo-controlled trial in an experimental model of acute pulmonary hypertension. Crit Care 2008; 12: R113. https://doi.org/10.1186/cc7005
Habler O, Kleen M, Zwissler B, et al. Inhalation of prostacyclin (PGI2) for 8 hours does not produce signs of acute pulmonary toxicity in healthy lambs. Intensive Care Med 1996; 22: 426–33. https://doi.org/10.1007/bf01712159
Hoeper MM, Olschewski H, Ghofrani HA, et al. A comparison of the acute hemodynamic effects of inhaled nitric oxide and aerosolized iloprost in primary pulmonary hypertension. German PPH study group. J Am Coll Cardiol 2000; 35: 176–82. https://doi.org/10.1016/s0735-1097(99)00494-5
McGinn K, Reichert M. A comparison of inhaled nitric oxide versus inhaled epoprostenol for acute pulmonary hypertension following cardiac surgery. Ann Pharmacother 2016; 50: 22–6. https://doi.org/10.1177/1060028015608865
Henke VG. Inhaled selective pulmonary vasodilator use after cardiac surgery: broader insights from a study describing significant changes in drug utilization and savings after implementation of a guideline favoring inhaled epoprostenol. J Cardiothorac Vasc Anesth 2022; 36: 1350–3. https://doi.org/10.1053/j.jvca.2022.01.024
Olschewski H, Rohde B, Behr J, et al. Pharmacodynamics and pharmacokinetics of inhaled iloprost, aerosolized by three different devices, in severe pulmonary hypertension. Chest 2003; 124: 1294–304. https://doi.org/10.1378/chest.124.4.1294
De Wet CJ, Affleck DG, Jacobsohn E, et al. Inhaled prostacyclin is safe, effective, and affordable in patients with pulmonary hypertension, right heart dysfunction, and refractory hypoxemia after cardiothoracic surgery. J Thorac Cardiovasc Surg 2004; 127: 1058–67. https://doi.org/10.1016/j.jtcvs.2003.11.035
Gavra P, Nguyen AQ, Beauregard N, Denault AY, Varin F. High-performance liquid chromatography assay using ultraviolet detection for urinary quantification of milrinone concentrations in cardiac surgery patients undergoing cardiopulmonary bypass. Biomed Chromatogr 2014; 28: 1084–9. https://doi.org/10.1002/bmc.3123
Nguyen AQ, Denault AY, Théoret Y, Perrault LP, Varin F. Inhaled milrinone in cardiac surgical patients: a pilot randomized controlled trial of jet vs. mesh nebulization. Sci Rep 2020; 10: 2069. https://doi.org/10.1038/s41598-020-58902-x
Krug S, Sablotzki A, Hammerschmidt S, Wirtz H, Seyfarth HJ. Inhaled iloprost for the control of pulmonary hypertension. Vasc Health Risk Manag 2009; 5: 465–74. https://doi.org/10.2147/vhrm.s3223
Loh E, Stamler JS, Hare JM, Loscalzo J, Colucci WS. Cardiovascular effects of inhaled nitric oxide in patients with left ventricular dysfunction. Circulation 1994; 90: 2780–5. https://doi.org/10.1161/01.cir.90.6.2780
Diaz-Rodriguez N, Nyhan SM, Kolb TM, Steppan J. How we would treat our own pulmonary hypertension if we needed to undergo cardiac surgery. J Cardiothorac Vasc Anesth 2022; 36: 1540–8. https://doi.org/10.1053/j.jvca.2021.09.030
Groves DS, Blum FE, Huffmyer JL, et al. Effects of early inhaled epoprostenol therapy on pulmonary artery pressure and blood loss during LVAD placement. J Cardiothorac Vasc Anesth 2014; 28: 652–60. https://doi.org/10.1053/j.jvca.2013.05.028
Hu X, Li X, Boggett S, et al. Routine intraoperative inhaled milrinone and iloprost reduces inotrope use in patients undergoing cardiac surgery: a retrospective cohort pilot study. Anesth Analg 2020; 131: 527–36. https://doi.org/10.1213/ane.0000000000004793
Weinberger B, Laskin DL, Heck DE, Laskin JD. The toxicology of inhaled nitric oxide. Toxicol Sci 2001; 59: 5–16. https://doi.org/10.1093/toxsci/59.1.5
Elmi-Sarabi M, Jarry S, Couture EJ, et al. Pulmonary vasodilator response of combined inhaled epoprostenol and inhaled milrinone in cardiac surgical patients. Anesth Analg 2023; 136: 282–94. https://doi.org/10.1213/ane.0000000000006192
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21: 1539–58. https://doi.org/10.1002/sim.1186
Author contributions
Berend Marcus and Steffen Rex helped in the study design, study conduction, data collection, data analysis, and manuscript preparation. Frederik Marynen helped in the study design, study conduction, data collection, and manuscript preparation. Steffen Fieuws helped in the study design, data analysis, and manuscript preparation. Dieter Van Beersel and Filip Rega helped with the data analysis and manuscript preparation.
Disclosures
Filip Rega has a research grant from Medtronic and is a consultant to AtriCure and Corcym. Steffen Rex has received speaking fees from Orion Pharma, Nordic Pharma, and Edwards Lifesciences. He has been member of advisory boards for Paion, Nordic Pharma, Orion Pharma, and Aerogen. He has received an unrestricted research grant from Nordic Pharma.
Funding statement
This research was solely funded by departmental sources and received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data availability statement
All data supporting the findings of this study are available within the article and in the Electronic Supplementary Material, and from the corresponding author on reasonable request. The protocol is available online on PROSPERO with the registration number CRD42021237991.
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Deputy Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marcus, B., Marynen, F., Fieuws, S. et al. The perioperative use of inhaled prostacyclins in cardiac surgery: a systematic review and meta-analysis. Can J Anesth/J Can Anesth 70, 1381–1393 (2023). https://doi.org/10.1007/s12630-023-02520-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-023-02520-4