Abstract
Inhaled nitric oxide (iNO) is considered standard therapy for pediatric postcardiac surgical pulmonary hypertension (PH). Limited data suggest that inhaled iloprost (inIlo), an aerosolized prostacyclin, may be a feasible and more affordable therapeutic alternative. The goal of this study was to determine if significant hemodynamic change or adverse events would occur in postoperative congenital heart surgery (CHS) patients with PH after their transition from iNO to inIlo. This retrospective review investigated CHS patients with postoperative PH (mean pulmonary artery pressure [mPAP] >25 mmHg) between January 1, 2010 and December 31, 2011 who transitioned from iNO to inIlo. By protocol, CHS patients receiving stable doses of iNO were gradually transitioned to inIlo. After full transition, the patients received inIlo every 2 h, with a final dosing range of 1.25–5 μg/dose. Both PAP and systemic arterial pressure (SAP) were invasively measured during the transition period. Seven patients ages 10 days to 1.5 years completed the protocol. Measurements of mPAP (p = 0.27) and systolic PAP (p = 0.25) did not differ between iNO and inIlo therapy alone. No serious adverse events or complications (bleeding or thrombocytopenia) occurred. The ratio of systolic PAP to SAP decreased in all patients receiving inIlo alone (p = 0.03). Pulmonary hypertension in postoperative CHS patients can be managed successfully with inIlo, and the measured hemodynamics with this agent are similar to those observed with iNO. For the management of postoperative PH, inIlo may be a reasonable alternative, thus reducing the need for costly iNO. Larger confirmatory studies would more robustly facilitate its integration into standard care.
Similar content being viewed by others
Introduction
Pulmonary hypertension (PH) is a rare postoperative complication that can occur with congenital heart surgery (CHS) patients. Children who experience PH are at substantial risk of postoperative morbidity and mortality, with death occurring in up to 12 % of cases [4]. Currently, inhaled nitric oxide (iNO) is used routinely in the management of PH during the postoperative period. To date, limited studies have been performed to confirm the efficacy of iNO in the postoperative CHS population, although clinical experience supports its continued use [9]. Given its unproven benefit, risk of rebound phenomenon, toxic metabolites, and cost, many centers are seeking an alternative to iNO for postoperative CHS patients with PH [12, 16].
Inhaled iloprost (inIlo), an aerosolized prostacyclin, may be a feasible and more affordable therapeutic alternative based on the limited pediatric studies completed to date. Similar to iNO, inIlo is a selective pulmonary vasodilator with few systemic adverse effects but with the additional advantages of simple delivery, minimal toxicity, and pulmonary vasodilation through a different cellular mechanism [2, 16, 17]. In multiple clinical settings, including vasoreactivity testing, inIlo has been demonstrated to improve hemodynamic measures and clinical outcomes [6, 10–12]. However, few studies have evaluated the role of inIlo in the postoperative management of CHS patients with PH. Although these studies suggest that inIlo may be as effective as iNO in selectively lowering pulmonary vascular resistance [7, 8, 14], the hemodynamic responses during the transition from iNO to inIlo have not been clinically assessed to date.
A protocol was implemented at our institution to transition postoperative CHS patients with PH from iNO to inIlo. This study retrospectively reviewed the clinical and hemodynamic responses of postoperative CHS patients with PH who completed the inIlo transition protocol to assess for adverse events associated with inIlo therapy. We hypothesized that hemodynamic measures including mean pulmonary arterial pressure (mPAP), systolic PAP, and ratio of systolic PAP to systemic arterial pressure (SAP) would not differ significantly after transition to inhaled iloprost.
Methods
We conducted a retrospective review of the CHS patients with postoperative PH who completed the iNO-to-inIlo transition protocol at our institution from January 1, 2010 to December 31, 2011. Study approval with waiver of written informed consent was obtained from our Institutional Review Board. All patients younger than 18 years who completed the transition protocol were reviewed. Pulmonary hypertension was defined as a mPAP higher than 25 mmHg in the initial postoperative period determined by invasive PAP monitoring.
For all cases, the medical record was reviewed, with demographic and postoperative clinical data recorded. The clinical data included systolic, mean, and diastolic PAP with simultaneous systemic systolic, diastolic, and mean arterial pressure; transcutaneous oxygen saturation (SpO2); central venous pressure (CVP); heart rate; arterial blood gas measures; hematocrit; and serum platelets. Dosages of iNO and inIlo, delivered concentration of oxygen (FiO2), sedation score, and use of neuromuscular blockade also were recorded. Both pulmonary and SAP measures were obtained from invasive monitoring lines. The systolic PAP:SAP ratio was calculated using simultaneous pressure measurements. The time points assessed during the transition protocol included baseline (iNO therapy alone), first dose of inIlo (after administration), iNO wean (50 % iNO dose), iNO off, and 2, 4, 6, 12, and 24 h after discontinuation of iNO.
Overview of InIlo Transition Protocol
A pediatric inIlo transition protocol was created and approved by the Pharmacy and Therapeutics Committee at our institution. All members of the committee including representatives from specialty pharmacy, cardiac intensive care, and pediatric cardiology reviewed the protocol. All postoperative patients in the pediatric cardiac intensive care unit (CICU) who were anticipated to require inhaled vasodilator therapy for more than 12 h were considered for the protocol.
For postoperative monitoring purposes, all the patients had systemic arterial lines. Pulmonary arterial pressure lines were placed in the operating room at the discretion of the surgeon and not for the sole purpose of the transition protocol. At our institution, invasive PAP monitoring is used conservatively. These lines are placed primarily in high-risk patients based on preoperative hemodynamic assessment or difficulties separating from cardiopulmonary bypass due to elevated PAP, particularly if associated with right ventricle (RV) dysfunction. Patients without an invasive pulmonary arterial monitoring line were not eligible to participate in the study.
The starting dose of inIlo was determined based on patient weight (Table 1). The drug dose was diluted to a 3-mL volume with normal saline to facilitate drug delivery. InIlo was aerosolized during 10–15 min using an Aeroneb Professional Nebulizer system (Aerogen, Galway, Ireland). The second dose of inIlo was administered 1 h after the first dose, and subsequent doses were given every 2 h.
Once inIlo therapy was initiated, iNO was weaned to allow the patients to transition to inIlo alone. The patients were monitored continuously, and at frequent predetermined intervals, clinical measures, hemodynamic parameters, and arterial blood gases were documented. The iNO wean was continued only if the patient met the iNO weaning criteria (systolic PAP:SAP ratio ≤0.75 or systolic PAP ≤baseline systolic PAP with iNO therapy alone, ≤10 % decrease in SpO2, <20-torr decrease in measured dissolved oxygen [PaO2]).
If a clinical decline occurred, defined as inability to meet the iNO weaning criteria, baseline iNO was restarted, and the inIlo dose was increased to the high dose (Table 1) before another iNO wean attempt. If the iNO wean was unsuccessful with the high dose of inIlo, then the transition protocol was discontinued.
All the patients participating in the transition protocol received otherwise standard postoperative care. During the postoperative period, the patients were managed with intravenous inotropic infusions including epinephrine, dopamine, and milrinone for hemodynamic support. Appropriate levels of sedation and analgesia were maintained. Neuromuscular blockade was not used routinely but was available for acute management of PH crises. Mechanical ventilation parameters were adjusted to maintain adequate oxygenation (SpO2 >95 %) and mild respiratory alkalosis (pH goal, 7.4–7.45).
Statistical Analysis
The postoperative clinical measurements for each patient at each time point of interest are displayed in graphic format. The Wilcoxon signed rank test was used to evaluate changes in the measures from baseline to 24 h off iNO therapy for each postoperative variable using SAS version 9.3 (SAS Institute, Cary, NC, USA). All p values lower than 0.05 were considered statistically significant.
Results
Patients
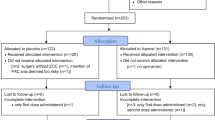
From January 1, 2010 to December 31, 2011, the iNO-to-inIlo transition protocol was initiated for 10 patients. Only seven patients completed the transition protocol because three patients were removed from the protocol after a diagnosis of residual anatomic pulmonary arterial or pulmonary venous obstruction was determined by cardiac catheterization or echocardiogram during the postoperative period. Five of seven patients underwent surgical repair of an atrioventricular septal defect or an anomalous pulmonary venous return. Two patients had a genetic diagnosis of trisomy 21, and one patient was known to have a 22q11 deletion.
The median age at surgery was 2.8 months (range, 0.3–18.4 months), and the median weight was 3.5 kg (range, 2.5–8.4 kg). The transition protocol was initiated most frequently on postoperative day (POD) 1 (range, POD 0–3). Demographic and clinical data including baseline iNO and final inIlo dose for each patient are presented in Table 2.
Hemodynamic Data
Median values showed no significant change in mPAP (24 vs 22 mmHg; p = 0.27) or systolic PAP (45 vs 34 mmHg; p = 0.25) when baseline measurements during iNO administration were compared with those of inIlo alone after iNO had been discontinued for 24 h. The mPAP measurements for each patient during the transition protocol are detailed in Fig. 1. Patients 5 and 6 showed an initial elevation in mPAP after iNO wean but improved after sedation and ventilation were optimized. Neuromuscular blockade was not required.
The ratio of systolic PAP to SAP decreased after transition from iNO to inIlo (0.61 vs 0.49; p = 0.03). Although variability in the ratio was noted for each patient through the transition protocol, no individual patient was found to have a ratio greater than baseline after completing the transition (Fig. 2).
All other clinical measurements including SpO2 (97 vs 96 %; p = 0.47), PaO2 (97 vs 73 torr; p = 0.31), CVP (10.5 vs 8.5 mmHg; p = 0.13), pH (7.41 vs 7.44; p = 0.69) measured dissolved carbon dioxide (pCO2) (38 vs 41 torr; p = 1.00) and heart rate (139 vs 140 beats per minute; p = 1.00) showed no significant change when measurements during iNO administration and after transition to inIlo were compared. Oxygen requirements decreased for all the patients through the transition protocol, and none required an FiO2 greater than 60 %.
Adverse Events
No serious adverse events including death or cardiopulmonary arrest occurred during the transition protocol. Similarly, no complications such as bleeding or thrombocytopenia with initiation of inIlo were observed.
Two episodes of transient hypoxemia and hypotension without additional evidence of clinical instability were documented. The episodes were associated with unplanned extubation (patient 2) or suboptimal sedation during a bedside procedure (patient 4). For both episodes, a decision was made by the attending physician to increase the iNO dose due to the acute change in hemodynamic measures. Neuromuscular blockade was used only to facilitate reintubation (patient 2). For both episodes, iNO wean was reinitiated after hemodynamic measures had returned to baseline. Both episodes were short in duration and did not preclude eventual full transition to inIlo.
All the patients were dependent on mechanical ventilation for the majority of the transition protocol. Bronchospasm related to inIlo administration, an adverse reaction documented with outpatient inIlo PH therapy [6], was not observed.
InIlo Delivery and Dosing
Aerosolized delivery of inIlo was well tolerated by all the patients. No errors occurred with the delivery device. An additional filter was placed in the expiratory limb of the ventilator circuit, which was changed daily and as needed. The proximal flow sensor was removed, and the iNO analyzer line was bypassed during inIlo administration to facilitate medication delivery and to maintain the integrity of the flow sensor. According to the transition protocol, all the patients were initiated with the starting inIlo dose for weight (Table 1), and four of the seven patients required escalation to a high dose during the protocol.
Patient Outcomes
After successful transition, inIlo was continued with all seven patients for a median of 3 days. Thereafter, three of the six patients who failed attempts to wean inIlo were transitioned to pulmonary vasodilatory therapy (sildenafil) dosed at 6.3 mg/kg/day (mean dose) before their transfer from the CICU. Three other patients normalized their PAP measured either by an invasive pulmonary arterial monitoring line or by echocardiographic assessment. The overall average CICU and hospital stays were 18 and 31 days, respectively. One patient died late during her CICU course due to chronic lung disease (with probable lymphangiectasia) and refractory PH.
InIlo Cost Data
The cost of inIlo was $9.69 per 1.25-μg dose, which increased incrementally to $38.75 per 5-μg dose. The patients transitioned to inIlo received a median of 38 total doses (range, 10–55 doses) during 3 days. The median unadjusted cost was $533 (range, $213–$1,317). The cost of iNO for an equivalent period was $9,504 ($3,168 per day). For the patient group in this study, a 3-day cost savings of approximately $9,000 per patient would be estimated for those successfully transitioned from iNO to inIlo.
Discussion
Pulmonary hypertension remains a significant postoperative complication for patients with congenital heart defects. New therapeutic options that become available for the management of pediatric PH should be considered for use in the critical care setting because they may be advantageous and more affordable.
InIlo, a prostacyclin analog, offers many advantages over iNO. When delivered as an inhaled agent, inIlo causes selective pulmonary vasodilation, minimizing the risk of systemic vasodilation while optimizing drug delivery to ventilated regions of the lung [5, 12, 14, 18]. Aerosolized delivery also avoids the risks associated with intravenous or subcutaneous prostacyclin administration. Additional advantages of inIlo therapy pertinent to the critical care setting include no documented risks of rebound phenomenon, less potential for toxicity, and greater ease of administration [12, 16].
The results from this small series of patients who completed an iNO to inIlo transition protocol demonstrate that postoperative CHS patients with PH can be transitioned successfully from iNO to inIlo without a significant change in hemodynamic or clinical measures and without serious adverse events, suggesting that inIlo may be a reasonable and cost-saving alternative to iNO.
A small number of pediatric studies, each with limited patient numbers, have evaluated the use of inIlo in the postoperative management of CHS patients with PH. A prospective randomized pilot study by Loukanov et al. [8] demonstrated that inIlo was as effective as iNO in the management of postoperative PH experienced by CHS patients, with comparable PAP measures and frequency of PH crises. However their study included only patients who had undergone repair of left-to-right shunt lesions. A study completed in a medical center with limited access to iNO also showed inIlo to be an effective alternative to iNO, but this study evaluated its use only as a rescue agent for postoperative PH crises [7]. In a case series of pediatric patients with PH who were sequentially treated with iNO followed by inIlo, both therapies were equipotent and equally selective in lowering pulmonary vascular resistance, but therapeutic effectiveness was assessed only for a 10-min period [14].
Our results are consistent with the conclusions of these studies, but the design of our study provided additional insight into the use of inIlo in the critical care setting because it included a longer period of clinical observation, a variety of postoperative CHS diagnoses including anomalous pulmonary venous return, and evaluated hemodynamic changes during a transition period. The hemodynamic stability sustained during transition from iNO to inIlo through the initial postoperative period demonstrated that inIlo may be an effective alternative to iNO in the care of postoperative CHS patients.
By successful transition of patients between pulmonary vasodilatory therapies, our results provide a unique perspective on the role of inIlo in the critical care setting. We demonstrated that CHS patients at risk for PH can be safely and feasibly transitioned to inIlo after initial stabilization using iNO.
Institutional protocols for weaning iNO in the care of postoperative CHS patients are variable. At our institution, an iNO weaning protocol is initiated in the postoperative period based at the discretion of the attending physician. Continuation of the iNO wean is based on hemodynamic stability. In our experience, CHS patients with PH often require a prolonged iNO wean unless an alternative pulmonary vasodilatory therapy is initiated.
Because the introduction of any therapeutic alternative is accompanied by a degree of uncertainty, we demonstrate that inIlo not only may be a practical alternative for the initial management of PH but also can be integrated into transition protocols for the postoperative management of PH in CHS patients. Its use in transition protocols would allow physicians to take advantage of the therapeutic benefits of inIlo with patients for whom a prolonged pulmonary vasodilatory therapy is anticipated, thereby reducing the use of iNO.
Because inIlo is a more stable prostacyclin with a longer elimination time and an effective pharmacologic half-life in the pulmonary vasculature of 21–25 min [2, 13], it also offers the advantage of intermittent dosing. We found that intermittent administration of pulmonary vasodilatory therapy rather than continuous delivery as required for iNO (or inhaled epoprostenol) was an unexpected advantage during the postoperative period because it was less cumbersome for patient care and made transport for urgent imaging or procedures safer and easier to facilitate.
Studies have proven inIlo to have a favorable safety profile in the management of outpatient pediatric PH. Common side effects include headache, cough, and flushing, whereas more serious but less common side effects may include thrombocytopenia, peripheral edema, and bronchoconstriction [2, 6, 13]. Although the majority of our patients were mechanically ventilated for the transition protocol, none experienced bronchospasm with inIlo administration. We observed no serious adverse events associated with inIlo therapy during the transition protocol, supporting its use as a safe pulmonary vasodilatory therapy for postoperative care.
As described in the review by Mulligan and Beghetti [12], the dose, delivery mechanism, and dosing interval for inIlo in the critical care setting remain unclearly defined. Among adults, inIlo dosing has varied from 10 to 20 μg/dose when used in postoperative care or to facilitate weaning from cardiopulmonary bypass [1, 19]. In the small number of pediatric studies focusing on acute care, the inIlo dose has varied from 0.5 to 2 μg/kg/dose, with the dosing interval varying from 30 min to 2 h [7, 8]. Based on the pharmacokinetic profile, the dosing recommendation for outpatient use of inIlo is 2.5–5 μg per dose administered five to nine times daily up to a maximum dose of 45 μg (5 μg per dose 9 times daily) [6]. With our transition protocol, the initial dose for all the patients was 0.25–0.5 μg/kg, and four patients required escalation to the higher dose of 0.5–1.0 μg/kg (Table 1), suggesting that 0.5–1.0 μg/kg per dose may be a more optimal dosing for postoperative CHS patients.
A variety of inIlo delivery devices have been described in published pediatric studies [6–8, 14]. In the acute care setting, device selection should allow easy incorporation into the inspiratory limb of the ventilator circuit. For our patients, we found aerosolized inIlo delivery using a nebulizer system to be uncomplicated and less cumbersome than the iNO delivery system. Although all patients were successfully transitioned using our inIlo dosing strategy and no change in hemodyanamics was observed after complete transition to inIlo, the pharmacokinetics of any drug are unpredictable in pediatric postoperative patients, and further studies are indicated to define better the optimal inIlo dose and administration in the CHS population.
At medical centers in which iNO is easily accessible, iNO has become the first-line agent for the management of postoperative PH, and physicians have developed a familiarity with its use despite a lack of supporting evidence. Coupled with the clinical advantages discussed previously [6, 12, 17], inIlo also may have a cost–benefit advantage. A small number of adult studies evaluating the cost effectiveness of prostacyclin outpatient therapy have suggested that although PH therapy should be individualized, iloprost is a less costly alternative with a good effectiveness profile [3, 15].
Although our study did not include a comprehensive cost-effectiveness analysis, the cost differential between iNO and inIlo therapy warrants brief discussion. During the study period, the institutional acquisition cost for a 10-μg vial of iloprost for inhaled therapy was approximately $80, which provided two to six pediatric doses depending on patient weight. In comparison, the cost of iNO was $132 per hour (daily cost of $3,168). If a range of $116–$465 for a 24-h dosing period of inIlo (depending on drug amount/dose) is used, the cost differential ranges between $2,700 and $3,000 per day. If two patients per month in each weight group (Table 1) treated with inIlo versus iNO are considered, the estimated annual cost savings could approach $975,000. Thus, inIlo is a substantially more affordable option than iNO and easily available in most countries. This finding may be especially relevant because the use of iNO typically imposes a significant financial burden on institutions and families because as a non-approved therapy for CHS patients, it generally is not a drug benefit covered by private or governmental payers.
Study Limitations
This study had several limitations. Because it was a retrospective review, the data set remained limited to the variables collected for the purpose of clinical management. Because invasive pulmonary arterial lines were infrequently used in our institution, only a limited number of patients completed the transition protocol, and thus our statistical analysis should be cautiously interpreted. Due to our conservative institutional practice, with placement of invasive PAP monitoring lines only for high-risk patients, those who completed the transition protocol were primarily patients with more severe disease. Despite a potential sampling bias, the results remain valuable because they demonstrate that even high-risk patients can be successfully transitioned to inIlo.
Some adult studies have suggested that a synergistic interaction can occur with simultaneous administration of iNO and inIlo [19]. This interaction has not been described in the pediatric population [14], but a potential interaction between iNO and inIlo during the transition cannot be excluded with these data. Hemodynamic measurements 24 h after discontinuation of iNO were used for comparison in our study to allow for complete metabolism of any residual iNO. Although larger pediatric studies are needed, this study remains unique because it describes the hemodynamic changes by invasive monitoring through a pulmonary vasodilatory transition protocol during the initial postoperative period.
Conclusion
Postoperative CHS patients with PH can be transitioned successfully from iNO to inIlo without a significant change in hemodynamic measurements or adverse events. Our results suggest that inIlo may be a reasonable and more affordable alternative for the management of postoperative PH in CHS patients.
We also have shown that inIlo can be integrated into transition protocols to reduce iNO use. Although a growing body of pediatric literature encourages the use of inIlo in the critical care setting, barriers that may prevent its integration into standard care include variable dosing strategies and a lack of familiarity with its clinical use and delivery system. Given the limited access to iNO in some medical centers and increasing economic pressures, inIlo may be a very practical alternative to iNO for postoperative CHS patients. Larger confirmatory studies are needed to facilitate its integration into standard care.
References
Antoniou T, Koletsis EN, Prokakis C, Rellia P, Thanopoulos A, Theodoraki K, Zarkalis D, Sfyrakis P (2013) Hemodynamic effects of combination therapy with inhaled nitric oxide and iloprost in patients with pulmonary hypertension and right ventricular dysfunction after high-risk cardiac surgery. J Cardiothorac Vasc Anesth 27:459–466
Baker SE, Hockman RH (2005) Inhaled iloprost in pulmonary arterial hypertension. Ann Pharmacother 39:1265–1274
Garin MC, Clark L, Chumney EC, Simpson KN, Highland KB (2009) Cost-utility of treatments for pulmonary arterial hypertension: a Markov state-transition decision analysis model. Clin Drug Invest 29:635–646
Gorenflo M (2010) Perioperative care in patients with pulmonary hypertension after cardiac surgery: clinical management, outcome, and future clinical research: results from an expert meeting. Cardiology 116:1–2
Ivy DD (2010) Prostacyclin in the intensive care setting. Pediatr Crit Care Med 11:S41–S45
Ivy DD, Doran AK, Smith KJ, Mallory GB Jr, Beghetti M, Barst RJ, Brady D, Law Y, Parker D, Claussen L, Abman SH (2008) Short- and long-term effects of inhaled iloprost therapy in children with pulmonary arterial hypertension. J Am Coll Cardiol 51:161–169
Limsuwan A, Wanitkul S, Khosithset A, Attanavanich S, Samankatiwat P (2008) Aerosolized iloprost for postoperative pulmonary hypertensive crisis in children with congenital heart disease. Int J Cardiol 129:333–338
Loukanov T, Bucsenez D, Springer W, Sebening C, Rauch H, Roesch E, Karck M, Gorenflo M (2011) Comparison of inhaled nitric oxide with aerosolized iloprost for treatment of pulmonary hypertension in children after cardiopulmonary bypass surgery. Clin Res Cardiol 100:595–602
Macrae DJ, Field D, Mercier JC, Moller J, Stiris T, Biban P, Cornick P, Goldman A, Gothberg S, Gustafsson LE, Hammer J, Lonnqvist PA, Sanchez-Luna M, Sedin G, Subhedar N (2004) Inhaled nitric oxide therapy in neonates and children: reaching a European consensus. Intensive Care Med 30:372–380
Muller M, Scholz S, Kwapisz M, Akinturk H, Thul J, Hempelmann G (2003) Use of inhaled iloprost in a case of pulmonary hypertension during pediatric congenital heart surgery. Anesthesiology 99:743–744
Muller M, Scholz S, Maxeiner H, Brenck F, Valeske K, Thul J, Akinturk H (2011) Efficacy of inhaled iloprost in the management of pulmonary hypertension after cardiopulmonary bypass in infants undergoing congenital heart surgery: a case series of 31 patients. HSR Proc Intensive Care Cardiovasc Anesth 3:123–130
Mulligan C, Beghetti M (2012) Inhaled iloprost for the control of acute pulmonary hypertension in children: a systematic review. Pediatr Crit Care Med 13:472–480
Olschewski H, Rohde B, Behr J, Ewert R, Gessler T, Ghofrani HA, Schmehl T (2003) Pharmacodynamics and pharmacokinetics of inhaled iloprost, aerosolized by three different devices, in severe pulmonary hypertension. Chest 124:1294–1304
Rimensberger PC, Spahr-Schopfer I, Berner M, Jaeggi E, Kalangos A, Friedli B, Beghetti M (2001) Inhaled nitric oxide versus aerosolized iloprost in secondary pulmonary hypertension in children with congenital heart disease: vasodilator capacity and cellular mechanisms. Circulation 103:544–548
Roman A, Barbera JA, Escribano P, Sala ML, Febrer L, Oyaguez I, Sabater E, Casado MA (2012) Cost effectiveness of prostacyclins in pulmonary arterial hypertension. Appl Health Econ Health Policy 10:175–188
Tissot C, Beghetti M (2009) Review of inhaled iloprost for the control of pulmonary artery hypertension in children. Vasc Health Risk Manag 5:325–331
Tissot C, Ivy DD, Beghetti M (2010) Medical therapy for pediatric pulmonary arterial hypertension. J Pediatr 157:528–532
Walmrath D, Schneider T, Pilch J, Grimminger F, Seeger W (1993) Aerosolised prostacyclin in adult respiratory distress syndrome. Lancet 342:961–962
Winterhalter M, Simon A, Fischer S, Rahe-Meyer N, Chamtzidou N, Hecker H, Zuk J, Piepenbrock S, Struber M (2008) Comparison of inhaled iloprost and nitric oxide in patients with pulmonary hypertension during weaning from cardiopulmonary bypass in cardiac surgery: a prospective randomized trial. J Cardiothorac Vasc Anesth 22:406–413
Disclosures
None.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vorhies, E.E., Caruthers, R.L., Rosenberg, H. et al. Use of Inhaled Iloprost for the Management of Postoperative Pulmonary Hypertension in Congenital Heart Surgery Patients: Review of a Transition Protocol. Pediatr Cardiol 35, 1337–1343 (2014). https://doi.org/10.1007/s00246-014-0933-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-014-0933-3