Abstract
Objectives
We aimed to evaluate the risk factors for moderate-to-severe bronchopulmonary dysplasia (BPD) and focus on discussing its relationship with the duration of initial invasive mechanical ventilation (IMV) in very preterm neonates less than 32 weeks of gestational age (GA).
Methods
We performed a prospective cohort study involving infants born at 23–31 weeks of GA who were admitted to 47 different neonatal intensive care unit (NICU) hospitals in China from January 2018 to December 2021. Patient data were obtained from the Sina-northern Neonatal Network (SNN) Database.
Results
We identified 6538 very preterm infants, of whom 49.5% (3236/6538) received initial IMV support, and 12.6% (823/6538) were diagnosed with moderate-to-severe BPD symptoms. The median duration of initial IMV in the moderate-to-severe BPD group was 26 (17–41) days, while in the no or mild BPD group, it was 6 (3–10) days. The incidence rate of moderate-to-severe BPD and the median duration of initial IMV were quite different across different GAs. Multivariable logistic regression analysis showed that the onset of moderate-to-severe BPD was significantly associated with the duration of initial IMV [adjusted odds ratio (AOR): 1.97; 95% confidence interval (CI): 1.10–2.67], late-onset neonatal sepsis (LONS), and patent ductus arteriosus (PDA).
Conclusion
In this multicenter cohort study, the duration of initial IMV was still relatively long in very premature infants, and the longer duration of initial IMV accounts for the increased risk of moderate-to-severe BPD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
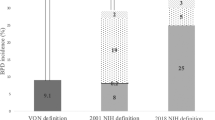
With the increasing survival rates of preterm infants, the incidence of bronchopulmonary dysplasia (BPD) has remained steady or increasing [1, 2]. Moderate-to-severe BPD brings about serious respiratory morbidity and neurosensory impairment, thus impacting the quality of life in affected pediatric and even adult patients [3, 4]. BPD was first described in 1967 and is considered the result of over-aggressive invasive mechanical ventilation (IMV) of relatively mature lungs (≥ 32 weeks of gestation) with an excessively high peak pressure of the supplemental gas mixture containing a higher proportion of oxygen and lacking surfactant [5]. However, the histology and pathogenesis of BPD have changed with a rise in the survival rates of premature infants at smaller gestational ages and weight. In 2001, the National Institute of Child Health and Human Development (NICHD) proposed the “New BPD” based on the severity and postmenstrual age (PMA), which is used most widely now [6]. Moreover, the NICHD Neonatal Research Network proposed a new evidence-based and severity-based definition of BPD in 2018 [7, 8]. The new definition of BPD focuses more on alveolar developmental arrest; nevertheless, whether the application status of initial invasive mechanical ventilation (IMV) still plays an important role in the occurrence and development of BPD still deserves our attention.
Series of guidelines such as the 2014 American Academy of Pediatrics guidelines [9] and 2019 European consensus guidelines [10] on the management of respiratory distress syndrome highly recommend the early use of pulmonary surfactant and the avoidance and minimization of IMV. We established the Sina-northern Neonatal Network (SNN) database and its online website (www.snn-med.com), and our previous study showed that about 41.9% of preterm infants [< 32 weeks of gestational age (GA)] received initial IMV. The incidence of BPD in the noninvasive ventilation failure group of very preterm infants can reach up to 37.6% [11]. The difference is statistically significant compared with that of the successful noninvasive ventilation receiving subjects, suggesting that the respiratory management of preterm infants may be related to the occurrence of BPD. In recent years, with the improvement of the treatment ability of very preterm infants, an increasing number of infants with smaller GAs and birth weight survive, and we urgently need multicenter large-scale research to reassess the effect of iatrogenic factors, especially the duration of initial IMV, in addition to alveolar arrest, on the development of moderate-to-severe BPD.
The main objectives of this study were to (1) investigate the incidence of moderate-to-severe BPD and the duration of initial IMV for different GAs in very preterm infants and (2) analyze the prenatal and in-hospital characteristics and identify the risk factors of moderate-to-severe BPD in very preterm neonates, especially its relationship with the duration of initial IMV.
Methods
Data source and study population
We performed a multicenter prospective cohort study of very preterm infants (GA: 23–31 weeks) in 47 neonatal intensive care units (NICUs) of level II or level III in China from January 1, 2018, through December 31, 2021. Patient records were obtained from the SNN database. SNN is a clinical research database in China and has strict data entry and quality-control standards. Trained data abstractors prospectively collected infant information at each NICU and electronically shared it each time among all provincial NICUs. All 47 hospitals collected data on very preterm infants using the SNN database with standardized definitions during the three-year study period. Written informed consents were obtained from all parents of the infants at each participating institution. Data on live-born infants were collected prospectively until discharge or death. Infants whose data were missing, with severe congenital heart and lung malformations, who transferred out, and those who died before 36 weeks of PMA were excluded from this study. The patterns of the initial IMV included both pressure support ventilation and volume control mode.
Study definitions
BPD was defined as the use of supplemental oxygen for more than 28 days of life and further stratified as mild, moderate, or severe according to the NICHD consensus-2001 [6]. Moderate-to-severe BPD was defined as any infant requiring continuous supplemental oxygen at 36 weeks of PMA or at hospital discharge, whichever occurred earlier. Small for gestational age (SGA) was defined as birth weight less than the 10th percentile for GA based on the Fenton growth curve [12]. Neonatal respiratory distress syndrome (NRDS) was diagnosed based on the presence of signs of respiratory distress in a typical chest X-ray and/or the need for surfactant. The patent ductus arteriosus (PDA) was diagnosed depending on signs of a murmur, bounding pulses, active precordium, and echocardiography. The presence of intraventricular hemorrhage (IVH) symptoms was diagnosed by evaluating a head ultrasound performed before 14 days of life and graded according to the Papile classification [13]. The diagnosis of necrotizing enterocolitis (NEC) was performed based on Bell’s modified staging criteria. Early-onset neonatal sepsis (EONS) was defined as premature rupture of the placental membrane more than 18 h before delivery, infectious disease development in neonates within 72 h of live birth, and abnormal values for two or more nonspecific infection indicators. If blood or cerebrospinal fluid (CSF) culture was positive for microbial infections, culture-positive septicaemia was diagnosed [14, 15]. Late-onset neonatal sepsis (LONS) was diagnosed by the clinical manifestations of systemic infection after three days of birth as well as abnormal values for two or more of the following nonspecific infection indicators: white blood cell (WBC) count < 5 × 109/L or > 20 × 109/L, C-reactive protein (CRP) ≥ 10 mg/L, platelets (PLTs) ≤ 100 × 109/L, and procalcitonin (PCT) > 2 ng/mL. Likewise, if the blood or CSF culture was positive, culture-positive septicaemia was diagnosed [16].
Statistical analysis
SPSS software version 25 (IBM Corp., NY, USA) and SAS version 9.3 software (SAS Institute, Inc., Cary, NC) were used for data analysis. Categorical variables are presented as percentages, and numerical data are presented as medians with 25th and 75th percentiles (interquartile range, IQR) and were compared by rank-sum tests. Standard descriptive analyses of the demographic and clinical data were performed by using Student’s t test, Mann–Whitney U test, or chi-squared (χ2) test, as appropriate. A P value of less than 0.05 was considered statistically significant. The odds ratio (OR) was calculated using multivariable logistic regression (MLR), with adjustment for factors that had a P value of < 0.05 in the univariable analyses. The MLR model, including all covariates, allowed us to assess the independent risk for the primary outcome of the individual patient. Receiver operating characteristic (ROC) curve analysis was performed to determine the cut-off value for continuous variables. The area under the ROC curve (AUC) was considered a measure of cut-off point accuracy. AUC values ≥ 0.90, 0.80–0.89, 0.70–0.79, and < 0.70 were considered excellent, good, reasonable, and poor, respectively.
Results
After excluding ineligible subjects, the study cohort finally included 6538 preterm infants with GA ranging from 23 to 31 weeks who were born at 47 different Chinese hospitals. Of these infants, 823 (12.6%) developed moderate-to-severe BPD, while 5715 (87.4%) were classified as having no or mild BPD (Fig. 1). The incidences of moderate-to-severe BPD in very preterm infants showed a decreasing trend with increasing GA, from 68.4% (13/19) at 23–24 weeks to 3.9% (74/1875) at 31 weeks of GA (Table 1).About 49.5% (3236/6538) of patients required initial IMV support, while that in moderate-to-severe BPD cases was 89.1% (733/823). The median duration of initial IMV in the moderate-to-severe BPD group was 26 (17–41) days and that in the no or mild BPD group was 6 (3–10) days. There were significant differences between the median duration of initial IMV support between moderate-to-severe and no or mild BPD groups as well as among different GAs. The median duration of initial IMV of GA at 23–31 weeks ranged from 19 to 28 days in the moderate-to-severe BPD group (Fig. 2).
All the included infants were allocated to the moderate-to-severe and no or mild BPD groups. The baseline characteristics of these subjects are described in Table 2. Among the infants with moderate-to-severe BPD, the median GA was 27.3 (26.1–28.6) weeks, and birth weight (BW) was 862 (780–940) g. Among them, 733 (89.1%) infants received initial support of IMV, and 744 (90.4%) had an initial fraction of inspired oxygen (FiO2) ≥ 30%. Compared with the no or mild BPD group, infants in the moderate-to-severe BPD group had lower GA and BW. There were statistically significant differences between these two groups in cesarean section, chorioamnionitis, male sex, SGA, APGAR scores for one and five minutes, surfactant treatment, initial FiO2 ≥ 30%, the median duration of initial IMV (days), the median duration of initial noninvasive ventilation, and postnatal dexamethasone treatment (Table 2).
The 6538 subjects were divided into two groups, namely, the case group and the control group, at 1:2 stratification (case group n = 823, control group n = 1646; Fig. 1) matched with GA (± 1 week), BW (± 100 g), and mode of initial respiratory support (initial IMV or initial noninvasive ventilation). Characteristics of GA, BW, and initial respiratory support were completely matched between the two groups. At the same time, there were no differences in cesarean section, chorioamnionitis, SGA, or APGAR scores (all P > 0.05). Notably, there was a significant difference in gender between the two groups (P < 0.05). Following stratification matching, neonates in the case group had significantly higher incidence rates of LONS, IVH grade 3–4, PDA, and retinopathy of prematurity (ROP) ≥ grade 3. They were more likely to receive postnatal dexamethasone treatment, as well as a relatively longer duration of initial IMV and noninvasive ventilation. At discharge, individuals in the case group had been hospitalized longer, had a higher body weight and were older than those in the control group (Table 2).
To evaluate the effect of these risk factors on the occurrence of moderate-to-severe BPD, we included gender, duration of initial IMV (days), duration of initial noninvasive ventilation (days), LONS, PDA, and IVH grade 3–4 for the MLR analysis (Table 3), and we adjusted the treatment of postnatal dexamethasone. Time of noninvasive ventilation, gender, and IVH grade 3–4 were found to have no correlation with the occurrence of moderate-to-severe BPD (all P > 0.05). The duration of initial IMV [adjusted odds ratio (AOR) = 1.97, 95% confidence interval (CI) = 1.10–2.67], LONS (AOR = 2.07, 95% CI = 1.54–3.26), and PDA (AOR = 1.45, 95% CI = 1.07–2.11) might have increased the risk of moderate-to-severe BPD onset (Table 3).
The cut-off value of the initial IMV time was set to 22 days through the ROC curve (sensitivity: 81.0%; specificity: 70.1%; area = 0.87; 95% CI: 0.74 to 0.92; P = 0.000) (Fig. 3). After 22 days of IMV, the risk of moderate-to-severe BPD was found to increase 1.97 times for each additional day of IMV (Table 3).
Discussion
This cohort study included 6538 very preterm infants with GA of 23–31 weeks. Among them, 8.2% of infants had a GA of ≤ 26 weeks. We identified that 49.5% of enrolled infants were prescribed initial IMV support, and 12.6% developed moderate-to-severe BPD. The median duration of initial IMV in the moderate-to-severe BPD group was 26 (17–41) days, while in no or mild BPD, it was 6 (3–10) days. This study suggests the current status of initial IMV support and exhaustively describes the relationship between prolonged duration of initial IMV and occurrence of moderate-to-severe BPD in a large-sample prospective cohort. The findings of this investigation emphasize the severity of a longer duration of initial IMV and the urgent need for quality improvement of respiratory management in neonates, which are crucial for guiding clinical practice on the prevention of moderate-to-severe BPD in Chinese NICUs.
In the present study, the incidence rate of moderate-to-severe BPD was 12.6% in neonates born at 23–31 weeks of gestation. According to the Vermont Oxford Network (VON), about 10% of infants born with GA between 22 and 29 weeks died before 36 weeks of PMA; 36.9% developed grade 1 or 2 BPD, and 3.7% presented grade 3 BPD in the United States [3]. In total, 59% of infants were born at ≤ 26 weeks of GA, compared with 8.2% of infants in the present cohort. Restricting our data set to infants who were born at ≤ 26 weeks of GA and survived to 36 weeks of PMA, we found higher BPD rates in these two studies. Furthermore, Torchin et al. reported in the EPIPAGE-2 cohort study in France [17] that the incidence rate of moderate-to-severe BPD in preterm infants with GA of 23–31 weeks was 11.1% and that at ≤ 26 weeks of GA was 38.5%. In this cohort study, the incidence rate of moderate-to-severe BPD at ≤ 26 weeks of GA was 40.1%, indicating a relatively higher occurrence rate in our case, which deserves further attention from clinicians.
In this study, preterm infants with moderate-to-severe BPD were associated with more complicated adverse outcomes, including a longer length of hospital stay, an older GA, and greater body weight at discharge. According to the published literature, middle- and long-term follow-up of moderate-to-severe BPD showed poor health and neurodevelopmental outcomes compared with preterm peers without or with mild BPD. Schmidt et al. found that preterm infants with BPD have more than doubled odds of late death or neurodevelopmental disability when compared with preterm infants without BPD [18,19,20]. Moreover, Jensen et al. [3] identified that greater BPD severity could be associated with more frequent development of major neonatal morbidities, in-hospital mortality, and the use of supplemental respiratory support at discharge. Therefore, early prevention and detection of moderate-to-severe BPD are extremely important.
The American Academy of Pediatrics Guidelines-2014 for respiratory support at birth and the European Guidelines-2016 for the prevention and treatment of NRDS have strongly recommended the implementation of preventive continuous positive airway pressure (CPAP) immediately after birth with subsequent selective surfactant administration in very preterm infants; if a ventilator is needed, rapid extubation is preferred to prolonged ventilation. The proportion of very preterm infants requiring initial IMV support was 49.5% in the whole cohort and 89.1% in moderate-to-severe BPD subjects. A retrospective cohort study from Spain between 2015 and 2019 reported that the proportion of preterm infants with GA of < 32 weeks requiring initial IMV support was approximately 31.8% [21]. In this study, the median duration of initial IMV in the moderate-to-severe BPD group was 26 (17–41) days and that in the no or mild BPD group was 6 (3–10) days. Moreover, Dassios et al. reported in a whole-population study with infants at < 28 weeks of gestation who were admitted to a neonatal unit in England between 2014 and 2018 that the duration of ventilation in the BPD group was 18 (7–35) days and that in the no BPD group was 4 (2–10) days [22]. Although the median GA of our cohort was relatively larger, the initial IMV duration was longer, suggesting that prolonged IMV duration could initiate secondary health complications. Therefore, a higher proportion of initial IMV and prolonged IMV duration pinpoints that there are gaps in the implementation of international guidelines in our region, which means further quality improvement of respiratory management of premature infants is urgently needed.
The comparison of baseline data between our study and previous studies confirmed that GA, BW, and effective initial resuscitation were significant risk factors for developing moderate-to-severe BPD [23]. After matching by GA, BW, and initial respiratory support, we found that the duration of initial IMV was consistently an important disease-modulatory factor related to the onset of moderate-to-severe BPD. Studies have shown that among infants with extremely low birth weight (ELBW), a longer cumulative duration of IMV largely accounts for the increased risk of chronic respiratory diseases associated with re-initiation of IMV [24]. Despite the life-saving benefits of IMV, Choi et al. reported the downside of mechanical ventilation in inducing moderate-to-severe BPD in very preterm neonates, especially when applied for a longer duration [25]. Several studies have reported similar consequences and suggested seriously considering the actual necessity of prolonged IMV support in preterm neonates [26,27,28]. Likewise, our study results also suggest that clinicians should consider an optimized mechanical ventilation strategy to minimize the incidence of moderate-to-severe BPD in very preterm neonates. An efficient strategy should include weaning from the ventilator as soon as clinically possible, following early extubation, and noninvasive ventilator support whenever possible.
Furthermore, we found that LONS and PDA increased the risk of moderate-to-severe BPD, which was consistent with previous reports. In a retrospective, population-based cohort study, Lapcharoensap et al. detected a reduction in rates of nosocomial infections associated with declining rates of BPD [29]. Many studies have indicated that there could be a pathophysiological relationship between sepsis and BPD. It is particularly important to control the occurrence of LONS to reduce the rate of BPD [30, 31]. PDA has been historically implicated in the development of BPD, which may be medically treated or surgically closed [32]. Recently, several studies have confirmed that prophylactic surgical ligation of PDA could not improve the incidence of BPD onset [33]. Additional studies are warranted to determine the weightage of benefits versus risks of non-intervention for hemodynamically significant PDA in premature infants. It is suggested that clinicians first manage PDA to strengthen the prevention and control of nosocomial infections, resulting in a reduced rate of occurrence of moderate-to-severe BPD.
The major strengths of our study are as follows. This was a large prospective cohort involving very preterm infants with a GA of 23–31 weeks. This study showed the incidence of moderate-to-severe BPD and the multicenter application status of initial IMV, demonstrating the causal relationship between the incidence of moderate-to-severe BPD and the duration of initial IMV at different GAs. Furthermore, the results of this study suggest that in addition to alveolar developmental arrest of premature infants leading to “new BPD”, iatrogenic factors still affect the occurrence and development of BPD, which should not be ignored. The occurrence of moderate-to-severe BPD is still related to NICU management, especially respiratory management, implying that clinicians still need to pay attention to and optimize respiratory management in very preterm infants and shorten the duration of initial IMV as much as possible. In addition, our study was based on a clinical research database that collected data according to internationally standardized definitions. Hence, our data source was reliable and strictly quality controlled, ensuring the accuracy of the variables in this study.
However, our study also suffers from several limitations. First, the NICHD consensus in 2001 was followed to define different stages of BPD severity and to exclude those infants who died before 36 weeks of PMA, which might have included some infants with severe BPD, thereby introducing selection bias to this study. Second, we did not analyze variations in IMV applications among different NICUs. We are planning to implement a survey on initial respiratory management strategies in multicenter NICUs to identify possible reasons for the application of prolonged IMV while exploring optimized respiratory management to prevent the occurrence of moderate-to-severe BPD. In addition, the specific modes and parameters of invasive mechanical ventilation were not analyzed in this study. We plan to conduct in-depth analysis and discussion on different ventilator modes and parameters in the following study.
In conclusion, the duration of initial IMV was relatively longer in very preterm infants in this regional multicenter study. A longer duration of initial IMV was associated with significantly higher incidences of moderate-to-severe BPD. Optimization of early respiratory management in very premature infants may play an important role in reducing the occurrence of moderate-to-severe BPD, which deserves further study. Next, we will explore the possible reasons for the longer duration of initial IMV, analyze the potential influencing factors of self-exposure and NICU management, and strive to carry out continuous quality improvement of NICU management factors.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA. 2015;314:1039–51.
Horbar JD, Carpenter JH, Badger GJ, Kenny MJ, Soll RF, Morrow KA, et al. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics. 2012;129:1019–26.
Jensen EA, Edwards EM, Greenberg LT, Soll RF, Ehret DEY, Horbar JD. Severity of bronchopulmonary dysplasia among very preterm infants in the United States. Pediatrics. 2021;148:e2020030007.
Allen J, Zwerdling R, Ehrenkranz R, Gaultier C, Geggel R, Greenough A, et al. Statement on the care of the child with chronic lung disease of infancy and childhood. Am J Respir Crit Care Med. 2003;168:356–96.
Northway WH, Rosan RC, Porter DY. Pulmonary disease following respirator therapy of hyaline-membrane disease, bronchopulmonary dysplasia. N Engl J Med. 1967;276:357–68.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Higgins RD, Jobe AH, Koso-Thomas M, Bancalari E, Viscardi RM, Hartert TV, et al. Bronchopulmonary dysplasia: executive summary of a workshop. J Pediatr. 2018;197:300–8.
Isayama T, Lee SK, Yang J, Lee D, Daspal S, Dunn M, et al. Canadian neonatal network and Canadian neonatal follow-up network investigators. revisiting the definition of bronchopulmonary dysplasia: effect of changing panoply of respiratory support for preterm neonates. JAMA Pediatr. 2017;171:271–9.
Committee on Fetus and Newborn, American Academy of Pediatrics. Respiratory support in preterm infants at birth. Pediatrics. 2014;133:171–4.
Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Te Pas A, et al. European consensus guidelines on the management of respiratory distress syndrome—2019 Update. Neonatology. 2019;115:432–50.
Wang L, Li JH, Yu YH, Huang L, Huang XY, Fan XF, et al. Initial respiratory support modality and outcome in preterm infants with less than 32 weeks of gestation in China: a multicentre retrospective cohort study. Paediatr Perinat Epidemiol. 2022;36:390–8.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013;13:59.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500 gm. J Pediatr. 1978;92:529–34.
Verani JR, McGee L. Schrag SJPrevention of perinatal group B streptococcal disease–revised guidelines from CDC, 2010. MMWR Recomm Rep. 2010;59:1–36.
Schlapbach LJ, Graf R, Woerner A, Fontana M, Zimmermann-Baer U, Glauser D, et al. Pancreatic stone protein as a novel marker for neonatal sepsis. Intensive Care Med. 2013;39:754–63.
Caffrey OE, Prentice P. NICE clinical guideline: antibiotics for the prevention and treatment of early-onset neonatal infection. Arch Dis Child Educ Pract Ed. 2014;99:98–100.
Torchin H, Ancel PY, Goffinet F, Hascoët JM, Truffert P, Tran D, et al. Placental complications and bronchopulmonary dysplasia: EPIPAGE-2 cohort study. Pediatrics. 2016;137:e20152163.
Schmidt B, Asztalos EV, Roberts RS, Robertson CM, Sauve RS, Whitfifield MF, et al. Impact of bronchopulmonary dysplasia, brain injury, and severe retinopathy on the outcome of extremely low-birth-weight infants at 18 months: results from the trial of indomethacin prophylaxis in preterms. JAMA. 2003;289:1124–9.
Schmidt B, Roberts RS, Davis PG, Doyle LW, Asztalos EV, Opie G, et al. Prediction of late death or disability at age 5 years using a count of 3 neonatal morbidities in very low birth weight infants. J Pediatr. 2015;167:982–6.
Turunen R, Nupponen I, Siitonen S, Repo H, Andersson S. Onset of mechanical ventilation is associated with rapid activation of circulating phagocytes in preterm infants. Pediatrics. 2006;117:448–54.
Avila-Alvarez A, Zozaya C, Pértega-Diaz S, Sanchez-Luna M, Iriondo-Sanz M, Elorza MD, et al. Temporal trends in respiratory care and bronchopulmonary dysplasia in very preterm infants over a 10 year period in Spain. Arch Dis Child Fetal Neonatal Ed. 2022;107:143–9.
Dassios T, Williams EE, Hickey A, Greenough A. Duration of mechanical ventilation and prediction of bronchopulmonary dysplasia and home oxygen in extremely preterm infants. Acta Paediatr. 2021;110:2052–8.
Kim SH, Han YS, Chun J, Lee MH, Sung TJ. Risk factors that affect the degree of bronchopulmonary dysplasia: comparison by severity in the same gestational age. PLoS ONE. 2020;15:e0235901.
Jensen EA, DeMauro SB, Kornhauser M, Aghai ZH, Greenspan JS, Dysart KC. Effects of multiple ventilation courses and duration of mechanical ventilation on respiratory outcomes in extremely low-birth-weight infants. JAMA Pediatr. 2015;169:1011–7.
Choi YB, Lee J, Park J, Jun YH. Impact of Prolonged mechanical ventilation in very low birth weight infants: results from a national cohort study. J Pediatr. 2018;194:34–9.
Fischer HS, Bührer C. Avoiding endotracheal ventilation to prevent bronchopulmonary dysplasia: a meta-analysis. Pediatrics. 2013;132:e1351–60.
Hwang JS, Rehan VK. Recent advances in bronchopulmonary dysplasia: pathophysiology, prevention, and treatment. Lung. 2018;196:129–38.
Escobar V, Soares DS, Kreling J, Ferrari LSL, Felcar JM, Camillo CAM, et al. Influence of time under mechanical ventilation on bronchopulmonary dysplasia severity in extremely preterm infants: a pilot study. BMC Pediatr. 2020;20:241.
Lapcharoensap W, Gage SC, Kan P, Profit J, Shaw GM, Gould JB, et al. Hospital variation and risk factors for bronchopulmonary dysplasia in a population-based cohort. JAMA Pediatr. 2015;169:e143676.
Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics. 2002;110:285–91.
Jung E, Lee BS. Late-onset sepsis as a risk factor for bronchopulmonary dysplasia in extremely low birth weight infants: a nationwide cohort study. Sci Rep. 2019;9:15448.
Ansems SM, Kirpalani H, Mercer-Rosa L, Wang Y, Hopper RK, Fraga MV, et al. Patent ductus arteriosus and the effects of its late closure in preterm infants with severe bronchopulmonary dysplasia. Neonatology. 2019;116:236–43.
Clyman RI, Hills NK, Liebowitz M, Johng S. Relationship between duration of infant exposure to a moderate-to-large patent ductus arteriosus shunt and the risk of developing bronchopulmonary dysplasia or death before 36 weeks. Am J Perinatol. 2020;37:216–23.
Acknowledgements
We sincerely appreciate all the clinical medical experts, epidemiological experts, statistics experts, and study participants of the Sino-northern neonatal network (SNN) and the CARE-Preterm cohort study group for their contributions to data collection and quality control, research design and data analysis.
Funding
This work was supported by the Project of “2021 Shandong Medical Association Clinical Research Fund (Qilu Special Project, YXH2022DZX0200X) and Shandong Key Research and Development Project (2018GSF118163).
Author information
Authors and Affiliations
Contributions
YYH: contributed to conceptualization, methodology, and supervision. DC: contributed to data curation, formal analysis, and writing of original draft. ZQC, QJH, HL, DYJ, YDJ, LL, LD, WXK, WY, QX, ZX, ZBJ, JHY and LZL: participated in conceptualization, data curation and formal analysis. RS: contributed to writing–review and editing. All the authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article. The authors have no conflict of interest to declare.
Ethical approval
The research protocol has been registered in the Chinese Clinical Trial Registration Center (ID: ChiCTR1900025234) and has been ethically reviewed by the Ethics Committee of the Provincial Hospital Affiliated to Shandong First Medical University (LCYJ: No. 2019-132). Informed consent to participate in the study have been obtained from participants’ parent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dou, C., Yu, YH., Zhuo, QC. et al. Longer duration of initial invasive mechanical ventilation is still a crucial risk factor for moderate-to-severe bronchopulmonary dysplasia in very preterm infants: a multicentrer prospective study. World J Pediatr 19, 577–585 (2023). https://doi.org/10.1007/s12519-022-00671-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-022-00671-w