Abstract
Around the world, undernutrition causes more than half of all deaths in children under 5 years of age. It also increases children's vulnerability to common diseases, impairs recovery, and stunts their physical and mental development. This paper investigates the state of child health and the assessment of health inequalities in children under 5 years, utilising Multiple Indicators Cluster Surveys across 36 districts in Punjab, Pakistan. We suggest a new household-based health index to identify health disparities and to help policymakers implement more successful domestic policies to offset inequalities. Additionally, this study estimates the health disparities for robustness checks applying the Palma ratio and Gini coefficient. The study's findings revealed that every second child in Punjab is malnourished and that 51% of children in Punjab had not received all of their recommended vaccinations. The results also show that health disparities in low-income districts are worse than in high-income districts. The findings further demonstrate that important contributors to health disparities include parental illiteracy, poverty, and political backwardness. This study recommends a multifaceted policy intervention to address child immunization, undernutrition, and infectious disease legislation, as well as income inequality, to reduce health disparities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Health disparities place a heavy weight on society, decelerating economic growth, labour productivity and causing income losses (Acemoglu & Johnson, 2007). Over the past few decades, the concerns surrounding health disparities have drawn attention in the fields of policymaking and academic research, primarily in wealthy countries but increasingly also in developing ones (Fotso, 2006; Gwatkin, 2017). Examples include the Black report from the 1980s, the Whitehall Studies from the 1960s, the final report of the Commission on Social Determinants of Health from the World Health Organization in 2008 and the 2030 plan for Sustainable Development (SDGs). The 2030 SDGs agenda's health-related goals placed a strong emphasis on health equity under SDG3: "ensure healthy lifestyles and promote well-being for all at all ages." A country can assess its progress toward SDG 3 and other health-related targets by addressing its health disparities, which also guarantees that underprivileged populations are not left behind.
All countries experience health disparities between demographic groups, although the severity of these inequalities varies between developed and developing countries in terms of size (Ataguba & Ataguba, 2020). Social and economic factors such as housing, income, education, political literacy, and access to state-provided healthcare are pivotal determinants impacting health indicators and are recognised as fundamental causes of health disparities (Braveman & Gottlieb, 2014; Nandy & Miranda, 2008). For instance, many studies have shown that the primary cause of malnutrition in developing countries is social factors, such as poverty, which results in a low nutritional status throughout generations and impedes social improvement and justice (Karaoğlan & Saraçoğlu, 2018; Sen & Mondal, 2012; Worku et al., 2018).
Over the last decade, Pakistan has made considerable progress in various health sectors, notably in improving maternal and child health, reducing child mortality and undernutrition. Significant achievements also include improved child vaccination and the eradication of diseases like malaria, tuberculosis, and hepatitis. Despite this Pakistan is ranked 149 out of 179 countries in terms of maternal mortality rates; 39% of the population is multidimensionally poor (Saleem et al., 2021); only 20% of Pakistan's entire population has availability to clean drinking water and only 22% of the population can obtain natural gas as a clean cooking fuel (Rahut et al., 2020). According to Ali et al. (2022) and Micha (2021), in Pakistan, about 37.6% children under 5 years age are stunted that is higher than the average in Asia (21.8%) and accounts for almost 22 million of the country's children who do not attend schools.
Pakistan needs to declare a health emergency in order to reach its health-related goals and develop a globally competitive workforce. This requires sufficient funding for health departments, improved health facilities, and focused efforts on the most vulnerable populations. To enhance health indicators, it's crucial to measure valid, reliable health indicators and develop a composite health index at the household level. Additionally, these indicators can help assess spatial health inequalities within and across Pakistan's districts. In order to track the accomplishments of the health-related SDGs, the World Health Organization [WHO] (2017) developed a five-step framework for examining health disparities. These procedures involve choosing the proper health-related indicators, gathering the necessary data, doing sophisticated analysis, presenting the findings, and determining the areas that need to be addressed first (Hosseinpoor et al., 2018). Furthermore, a framework provided by the UK Office for National Statistics (ONS) (2018) suggests that the construction of reliable health index should encompass key domains related to health status measurement., e.g., physiological risk factors, protective measures, and physical health conditions.
In light of the above, this study constructs the health index based on frameworks formulated by the World Health Organization (WHO) in 2017 and the Office for National Statistics (ONS) of the UK in 2018. The main purpose of the health index is to uncover the causes and factors of intra-district health disparities in Punjab's health infrastructure. Further, this study is designed to expose the disparities in health among children below the age of 5 years and to explore their relationship with socioeconomic factors that affect child health, utilising the Multifunctional Indicators Cluster Survey (MICS) microdata across 36 districts in Punjab, Pakistan.
The objectives of this paper are as follows: (a) measure and analyse the three health-related indicators: the composite index of anthropometric failure (CIAF), the cough, hepatitis, and tuberculosis index (CHTI), and the immunization rate; (b) examine the relationship between socioeconomic status and health indicators; (c) compute the health index to determine health disparities for all districts and their associations with socioeconomic status; and (d) offer recommendations for enhancing public health practises in addressing health disparities. Considering the foregoing, we developed a new household health index, representing the weighted average of three health related factors: the immunization rate (preventative measures); the CIAF (physiological risk factors); and the CHTI (physical health conditions).
This paper uniquely contributes in a number of ways to the public health and child health policy sectors: 1) it constructs a new household-based health index by including child and adult health-related variables for district-level analysis of health conditions; 2) it ensures the construct validity by finding indicators’ expected empirical relationship with the household-based asset index; 3) it applies a methodological option for the formation of the household-based health index and describes the health disparities in 36 districts applying the Gini coefficient and the Palma ratio to perform robustness checks; 4) it validates the Palma ratio method's central tenet that the middle 50% of the distribution can be disregarded because of its low variability; 5) it endorses the disparity measurement methods through finding a nearly perfect fit between Gini and Palma; 6) it interprets the role of economic and social disparities in explaining the health disparities within Punjab districts. Finally, we demonstrated the resilience of this health index using a range of robustness checks with multiple empirical methods. This research would recommend policy changes to the public health sector and provincial governments to improve access to vaccination facilities and nutrition education for children under the age of five. It would also assist policymakers in identifying district-specific socioeconomic factors that contribute to child health disparities.
The remainder of the essay is organised as follows: Section 2 presents a critical analysis of child health and the factors that contribute to child health disparities. A brief methodological explanation of how each component of the health index is measured is provided in Section 3. The empirical results are presented in Section 3.1. Finally, some concluding remarks, discussion of the results and policy implications are provided in Section 3.1.1.
2 Review of the Literature on the Determinants of Health Disparities
This section aims to offer a detailed review of the existing literature on constructing health indices, child undernutrition, health disparities, and the theoretical framework of the study. Global agencies (e.g., WHO, UN agencies) and academic institutions estimate key health indicators to track trends over time (Boerma et al., 2010; Chan et al., 2010) and to make comparisons between societies by obtaining a comprehensive picture of causes of death (Mathers et al., 2009; Tate et al., 2012), burden of disease, or risk factors. A wide range of health indicators at a global and/or country level are published to assess the health status of the population. Commonly used indicators are life expectancy, health facilities, maternal health, communicable and non-communicable diseases, food and nutrition, and mortality levels (Aburto et al., 2020). Specifically, certain studies have focused on different aspects of health measurement: Santos et al. (2008) examined morbidity and the coverage of interventions or immunizations, Piqueras et al. (2021) analysed anthropometric indicators, and Grépin et al. (2020) explored financial indicators, such as total health expenditures, to assess health disparities. The United Nations Development Program (UNDP) launched the first human development report in 1990. The human development index (HDI) is comprised by of three dimensions; 1) a long and healthy life, 2) knowledge acquirement, and 3) a decent standard of living. The life expectancy at birth, an aggregate indicator, is used as proxy variable for estimating health situation (current mortality conditions) of the population to measure the national HDI level. The life expectancy index is an effective way for comparing the health situations of various countries. However, for estimating health disparities within a single country, it may not be as useful. This is because life expectancy is not directly measurable at the household level (Harttgen & Klasen, 2012). Although household-base mortality data can be used to generate household-level life expectancy index by employing some imputation or simulation techniques (Grimm et al., 2008; Harttgen & Klasen, 2012), the objective of this paper is not to estimate human development index at household level but rather to construct a household-based health index specifically for estimating health disparities. In 2003, the UNDP developed a district health index for Pakistan using two indicators: (1) child survival rates and (2) immunization rates. Later, the 2017 report updated this index by using (1) immunization rates and (2) health facilities as the key indicators (Kahane et al., 2003; UNDP, 2017).
Alternatively, a number of studies around the world have proposed health indicators to build a household-based health index. For example, the World Health Organisation (WHO) has introduced 100 core health indicators (WHO, 2015) covering topics such as service coverage, risk factors (such as nutrition, child immunization, and communicable diseases), and health status. Additionally, the World Health Organisation has created a methodology (WHO, 2017) for tracking health disparities within a country and for building health indices. Later, in 2018, the UK's Office for National Statistics released a report with a methodology illustration for estimating a composite health index for England. This report provides detailed information on variables to consider when developing a health index, such as protective measures, physiological risk factors and physical health conditions.
There is also a lot of evidence in the empirical literature for calculating health indexes using indicators other than life expectancy. Pelletier et al. (1995) have investigated the effect of malnutrition on child mortality by using data of developing countries. The results of the study explicitly explain that 56% of child mortality is associated to malnutrition of children. This study strongly suggests that health outcomes are closely linked to child nutrition. However, its limitation lies in using only the child weight-for-age indicator to represent malnutrition. This approach fails to address other critical dimensions of undernutrition, namely height-for-age and weight-for-height.Gurung and Sapkota (2009) have analysed the factors associated to the undermatron in Nepal. They have estimated the stunting, wasting and under-weight for under-five children by using cross-sectional data. The results reveal that children belonging to poor families have four times higher risk of being underweight than the children from rich families. Similar indicators of undernutrition (stunting, wasting, and underweight) are calculated in the following studies (Gurung & Sapkota, 2009; Padmapriyadarsini et al., 2009). The limitations of these studies include that they do not collect information from a single undernutrition score; rather, they explain the results separately for each facet of undernutrition.
The CIAF is single value index of undernutrition that explains the information of all three dimensions of undernutrition (stunting, wasting and underweight). Svedberg introduced the CIAF in 2000, and Nandy improved it in 2005. A number of studies have used the CIAF to explain undernutrition predictors and the association between undernutrition, mortality, illness, and poverty (Nandy & Miranda, 2008; Nandy & Svedberg, 2012; Nandy et al., 2005). Overall, these studies provide useful information about health-nutrition indicators, but they do not provide a comprehensive picture of people's health since they miss several critical features (immunisation, infectious diseases etc.) recommended by WHO (2015) and the framework provided by UK ONS (2018) and WHO (2017). A reliable health index needs to cover fundamental domains concerning the measurement of health status, e.g., physiological risk factors, protective measures, and physical health conditions (WHO, 2017).
In developing countries, data adequacy is a problem, as data on all health variables is unavailable for study. To address data limitations, this study chose the most appropriate indicators from the defined domains for the available household-based survey data. The CIAF is employed to evaluate physiological risk factors by examining a child's nutritional status, focusing specifically on anthropometric failure and health disparities. All children who display even one of the following: underweight, wasting, or stunting, are included in the CIAF. To represent the domain of preventive measures, the proportion of children who have received their prescribed vaccines is used as an indicator, as outlined in Al-lela et al. (2014).SDG 3.b.1 clearly states that vaccinations are required. TB, hepatitis, and cough are examples of infectious illnesses that are utilised to diagnose physical health issues. Thus, this study measures a health index that includes adult and child health indicators in order to investigate health disparities and their causes differently than past research.
The health analysis performed in this study is unique from the existing literature on health disparities in Pakistan for various reasons. Specifically, it develops a systematic and methodical methodology to select reliable and valid indicators for constructing a household-based health index. We also seek to construct a comprehensive picture of health indicators, despite data limitations that prevent the addition of some additional dimensions (e.g., maternal health indicators, access to health facilities in the country, satisfaction with health facilities, etc.). This includes indicators related to child health (e.g., the immunization rate, stunting, wasting, and underweight), adult health (such as TB, hepatitis, chronic cough, and fever In contrast to other studies that mention Pakistan, these studies are restricted to one or a small number of health-related indicators. Additionally, this study places a strong emphasis on estimating health disparities through the application of the Gini-coefficient and Palma-ratio approaches. It also offers a thorough comparison of the outcomes generated by Gini and Palma and verifies that the district rank ordering for Pakistan's Underline Province is the same using both advanced methodologies. We develop the following hypotheses for our subsequent analyses based on the theoretical considerations and empirical evidence described in this section:
-
H1: As we expect that health-related indicators depends on socioeconomic factors, we hypothesize that households with lower incomes have lower rates of vaccination, poorer physical health, and undernutrition.
-
H2: As the health disparities also depends on socioeconomic factors, we hypothesize that health disparities are greater in districts with higher rates of income and education disparities.
3 Description of the Data and Statistical Methods
The Pakistan Bureau of Statistics (PBS) collected data for the United Nations Children's Fund through the Punjab MICS05 survey, which was used in this study (UNICEF).Footnote 1 The Pakistan MICS survey is a nationally representative survey that uses multistage cluster sampling to obtain information on a variety of women and child health topics including as vaccination, education, child and maternal health, family planning, and HIV/AIDS knowledge. Standardised questionnaires were used to collect information from children under the age of 5 in the selected households. The survey's institutions were responsible for gaining ethical approval. The objective of the survey is to evaluate and examine the health situation of the population by giving the government of Pakistan with authentic and up-to-date health indicators for men and women aged 15–49 and children under 5. Pakistan's administrative units are four provinces: Punjab, Sindh, Khyber Pakhtunkhwa, and Balochistan. The MICS survey, in reference to Pakistan, is unique in that it gives a population representative sample for each province independently. Furthermore, by incorporating updated global and regional data in each round of the MICS survey, this study provides a more comprehensive view of the long-term income (assets), education, and child health of the sampled population. Punjab is the province with the most population, accounting for 53% of Pakistan's overall population (Pakistan Economic Survey, 2016–17). On other hand, Punjab hosts one-fourth of Pakistan's poorest people (Naveed & Khan, 2018). The Punjab-MICS5 was carried out in 36 districts throughout the province, with a sample sizeFootnote 2 of 38,405 households and a 98% response rate. The survey's response rate is considered to be a key indicator of the data's quality and authenticity, since it reflects findings that would have come from the entire population. Higher response rates have been shown to increase the likelihood of including all subgroups that might differ systematically in the attitudes, opinions, or other prosperities of the data (Groves & Peytcheva, 2008). Additionally, 53,668 women between the ages of 15 and 49 were interviewed to address issues specific to women, and 27,495 mothers or carers were questioned to report on issues specific to children under the age of 5 years. The survey data specifically covers child-related topics, including education, immunization, nutrition, child development, and mortality rates. Table 1 provides detailed information regarding the division-wise district level sample of mix survey. It shows that there are nine divisions of Punjab, where division is sub-administrative units of the province of Pakistan. Each division is comprised by number of districts.
3.1 The Construction of the Household Health Index
The health index offers a single health value that can be used to compare health between districts or over time. This study mostly adopts the methods suggested by the UK's ONS annual report (2018) and the WHO’s (2017) strategy for the selection of health-related indicators to construct a composite household-based health index. Additionally, Sen and Mondal (2012), Berkley (2015) and the WHO served as inspirations for the selection of indicators (2017). The three domains that make up the health index are, in general, preventative measures, physiological risk factors, and physical health states. The ONS has also developed the procedures to build a health index for the analysis of the UK's health status using more or less comparable domains and indicators. In this section, the three health-related variables (immunization rate, CIAF, and the prevalence of CHT) are explained and put into formulas. Additionally, we clarify and support the asset index,Footnote 3 which is used as a validator to ensure that each indicator, dimension, and final health index are accurate.
3.1.1 Estimating Child Health
Computating Immunization Rate
The immunization rate is one of the metrics used in the protective measures area. A child is deemed fully immunized in accordance with the immunized rate if they have got a minimum of one dose of the BCG vaccine, three oral polio vaccination doses, the Penta vaccination in three doses (which contains DPT, HepB, and HiB),Footnote 4 and a single measles-I vaccination dose (Hasan et al., 2010). According to the survey, Pakistan's overall complete immunization rate ranges from 47 to 57% (Owais et al., 2011). A comprehensive part on immunization is covered by the MICS5 data for Punjab-Pakistan, which includes questions from IM1 to IM19 in the questionnaire. In this study, the full immunization rate for children under the age of 5 was estimated using MICS5 SPSSFootnote 5 syntax. To do this, the immunization rate (Irate_h) of each household is calculated using Eq. (1), where Irate_h is the proportion of the total number of completely immunized children aged 12 to 35 months in each household (TCFIM_h) to the total number of children in the household (TCMH h). The official present:
3.1.2 Composite Anthropometric Failure Index
In underdeveloped countries in particular, undernutrition is regarded as the leading cause of illness and child mortality (Pelletier et al., 1995). It is determined by factors including age, height, and weight. For example, a child under the age of 5 is considered underweight if they are underweighted for their height and age, wasting when their weight is low for their height, and stunting when their height is low for their age. Stunting is thought to be a reflection of chronic illness or persistent food deprivation, while wasting is thought to be a consequence of more recent illness or food scarcity and acute undernutrition. Additionally, chronic and acute underweight are implicitly measured using the composite index of underweight (Nandy & Miranda, 2008). To standardise anthropometric measurements, the NCHS/WHO international reference standards are employed. Experts in nutrition study typically use Z-scores; with this methodology, the mean and standard deviation for a group of children's Z-scores can be computed. The Z-score in Eq. (2) is defined as the difference between an individual's value and the median value of the reference population for the same age or height, divided by the standard deviation of the reference population.
where OF denotes the observed value, MV is the median reference value, and \(\sigma\) denotes the reference population's standard error. In addition, the percentage of the median (PM) is defined as the difference between the observed value (OV) in the individual and the median value (MV) of reference data for people of the same age or height and sex. Equations (2) and (3), respectively, give the equations for the Z-score and the median percentage.
The most popular Z-score cut-off for all markers is -2 SD, which can be used to detect children who are stunted, wasting, or underweight. In other words, a child will be deemed undernourished for a specific indicator if their Z-score for stunting, wasting, or underweight is below -2 standard deviation; children below -3 standard deviation are referred to as seriously undernourished. See WHO Child Growth StandardsFootnote 6 (De Onis, 2017) for a thorough explanation of how Z-scores are determined, and get Anthro-Plus Software.Footnote 7 Each of these three indices offers highly helpful details on both chronic and acute malnutrition (WHO, 2017), however they are unable to quantify children's overall undernutrition as a whole (Nandy & Svedberg, 2012). The CIAF was introduced by Svedberg (2000) as a general indicator of undernutrition. He stated that anthropometric failure is underestimated by stunting, wasting, or being underweight, hence he proposes CIAF as a remedy. According to Nandy et al. (2005), children with anthropometric failure fall into the following categories.
As shown in Table 2, the CIAF assesses the proportion of children under 5 with a broad overview of anthropometric failure that reflects health deprivation (Nandy & Miranda, 2008; Nandy & Svedberg, 2012; Nandy et al., 2005). Hence, in order to assess the nutritional status of children under the age of 5, we applied an anthropometric accomplishment index. As a result, the CIAF offers a thorough assessment of anthropometric failure that indicates health deprivation. An anthropometric accomplishment is CIAF's opposite. This index's formal measurement is the percentage of children under 5 who do not have any anthropometric issues. A higher percentage indicates a healthier society with a higher predicted life expectancy. The index is presented more formally in Eq. (4):
where TCH5 is the total number of children under the age of 5 in the family, TC5NAF is the total number of children under the age of 5 without any anthropometric failure, and NAFh is the "no anthropometric failure index".
Calculating the Index for Cough, Hepatitis, and Tuberculosis:
The prevalence of CHT are utilised as indicators for the physical health conditions domain when computing the health index. The MICS5 survey statistics include the following three questions about the frequency of infectious diseases: (1) HL16A: Has the family member had a fever and a cough for the previous three weeks? (2) HL16B: Has the member received a tuberculosis diagnosis during the last 12 months? (3) HL16C: Has the member had a hepatitis diagnosis within the last 12 months? The following is the formal Eq. (5) for estimating stage three physical health conditions (PHCh):
where TNMF denotes the overall number of family members in the household and NFNCTH denotes the number of family members who do not have a prevalence of CHT. The PHCh is the proportion of a family free of infectious illnesses at the time of the survey. This index's value increases with the level of society's health and productivity.
3.1.3 The Health Index Calculation Approach
The health index \({(H}_{h})\) is a composite index made up of three domains: preventative measures, physiological risk factors, and physical health conditions. Each of these domains is measured by one of the following three subindices: immunization rate, anthropometric failure index, and physical health conditions index. The method of measurement for each index was described in the sections before this one. The health index is created using the Eq. (6) after these three indices have been determined for each household.
A household-specific health index is Hh in this case. It calculates the proportion of children who are properly immunized, have no anthropometric failure, and are free from infectious diseases among all household members. A more productive and healthy society is indicated by a higher index value. Also, a higher health index may reflect higher economic well-being, either as a result of having a higher income that allows them to afford better food, housing, and medical care or because they are healthier and therefore don't need to spend as much on medications and medical care (Farooq & Masud, 2021). Table 3 provides a summary of health index indicators and target posts.
3.2 Calculating Household Level Asset Index
This study used a household-based asset index as a proxy variable for household income, offering a better representation of long-term income, as assets accumulate over time and embody a multidimensional aspect of household living standards (Howe et al., 2008). A robust analytical framework is necessary for the construction of the asset index itself; specifically, we have selected a modified version of the deprivation measurement index that has been certified by the European Union. The reader can access additional, methodical information about how the household-base asset index is constructed from Naveed et al. (2021). The following procedures are used to construct the household level asset index: 1) Tetrachoric Principal-Component Analysis and Exploratory Factor Analysis are used to ascertain the dimensional structure of the assets, 2) we have employed Item-Response Theory and Classical Test Theory models to identify the best subset of assets in order to minimise systematic and random errors. These models help in assessing the construct's validity and reliability. Additionally, they support the use of equated household income as a validator for the asset index, presuming that households with higher incomes will possess more assets and earn more money over the long run. The OECD square root equalisation scale approach is used to calculate equalised household income.
Following the implementation of the outlined procedures, the research finds that a selection of just 22 itemsFootnote 8 from a total of 30 assets can construct a highly reliable scale. The household asset index is constructed by applying equal weights to each item in the final index, as shown in the equation below.
Here, 𝐴𝑖 stands for the household-specific asset index and ŷ denotes specific weights for each asset possessed by the household. The term \({a}_{in}\) refers to the respective asset of \({i}^{th}\) household recorded as a dichotomous variable in Punjab MICS05 data sets. We obtain an estimated normalized index by merging the asset index elements, which may range from 0 to 1.
3.3 Education Index
Exploring whether districts in Punjab with greater educational disparities also exhibit higher health disparities would be insightful. To facilitate this investigation, we have estimated a household-based education index using data from the MICS05 survey. The following numbers to 0indicators are used to estimate the education index: 1) expected years of education (EYS) for children enrolled in school, 2) literacy skills, and 3) mean years of schooling (MYS) for individuals 25 years of age and older. Using modified version of the UNDP framework, the following equation is used to estimate the composite education index at the household level.
where \({{\text{E}}}^{{\text{h}}}\) is the household-specific education index, \({MYS}^{{\text{h}}}\) is the estimated adult mean years of schooling index, \({EYS}^{{\text{h}}}\) is the expected years of schooling index, \({Ra}^{{\text{h}}}\) is the reading ability household index, and \({Wa}^{{\text{h}}}\) is the writing ability index. Finally, education disparities are measured by calculating the Gini coefficient of the composite education index.
3.4 Methods for Calculating Health Disparities
There are numerous estimating methods available for measuring disparities (De Maio, 2007). The Gini coefficient is one of many methods for estimating disparities that is frequently cited. The Gini coefficient approach is established on the Lorenz curve formation. It has been employed in existing studies to assess income disparities and health disparities (Raskall & Matheson, 1992; Eyal et al., 2013). It is a relative scale with a value ranging from 0 (no disparity) to 1 (the greatest disparity). The Gini coefficient's index (0–1) has no intuitive significance on its own, but when multiplied by two, it represents the percentage of the projected mean difference between two randomly selected people in the population (Eyal et al., 2013). For example, if two households are chosen at random from the population distribution and the disparities in their health or income shares is expressed as a fraction of the mean, the deviation is equal to twice the Gini coefficient's value. This implies that with a Gini coefficient of 0.2, there's an expected 40% difference in the average health or income share between the two randomly chosen households. The Palma ratio is another widely used method for assessing disparities. Hence, inequality can be meaningfully quantified by comparing the top 10% of households with the richest share of households to the bottom 40% of households, or the poorest (Cobham & Sumner, 2013). The Palma ratio axiom states that the lowest and highest tails of the distribution are mostly unaffected by changes in income distributions (Palma, 2011, 2016). Furthermore, it has been asserted that across time and between countries, the middle 50% largely maintains its stability.
The Sustainable Development Goals (SDG) 2030 programme by the United Nations includes the Palma ratio. "By 2030, progressively achieve and sustain income growth of the bottom 40% of the population at a rate higher than the national average," states Sustainable Development Goal 10.1. The UNDP, numerous other nations, and UN agencies have all made extensive use of the Palma ratio. In conclusion, the Palma ratio is incorporated by the UN into the SDGs and suggested by numerous research studies, including Doyle and Stiglitz (2014), and Palma (2011, 2016)).
The Gini coefficient is an effective measure of disparities since it adheres to Lorenz-consistent. It also satisfies the four essential assumptions of inequality measureme: symmetry, replication invariance, scale invariance, and transfers (Bellù and Liberati (2006); Lisker, 2008). While the Palma Ratio can contradict the transfer axiom (where there is a transfer inside the lowest 40%, richest 10%, or 50% in the middle). It can be considered more intuitive, this does not stem from its normative approach, which contradicts the established axiomatic literature on inequality measurement (Van Puyenbroeck, 2008). In this study, the Gini coefficient and Palma ratio are computed using the composite health index to determine health disparities. Similarly, the Gini coefficient is calculated using the asset index to measure income disparities.
4 Results and Discussion
The results of the health indicators and health disparities in Punjab, Pakistan, are presented in this section per district.
4.1 Upshots of Child Health
In this subsection, we present that three health-related indicators which are used to compute the composite health index. These three health-related indicators are CIAF, chronic CHT and child immunization present.
4.1.1 Immunization Rate Estimation and its Association with the Asset Index
Many studies applied the income and mother educations as validators for immunization rate (Lucyk et al., 2019; Naveed et al., 2021). The immunization rate is predicted to be positively correlated with household income and mothers' level of education (Shah et al., 2021). This is accomplished by establishing a link between the household-based asset index and the vaccination rate, and then using the asset index as a proxy for household income as a validator for immunization achievement.
Table 4 shows the immunization rates of children under the age of 5 by gender and district. The Gujrat district performed best when it came to immunizing children under the age of 5; around 91% of the youngsters were fully immunized. Places second and third, with 89% and 87% respectively, go to the districts of Narowal and Jhelum. The lowest immunization rates are found in the Southern Punjab region, specifically in the division of Dera Gazi Khan, which comprises the districts of Dera Gazi Khan, Muzaffargarh, and Rajanpur. These districts' immunization rates are 28%, 37%, and 42%, respectively. In general, among the nine divisions of Punjab, Dera Gazi Khan has the worst performance. This could be because the majority of the poorest people live in the Dera Ghazi Khan division, which has the lowest literacy rate in the country (less than 40%; Pakistan Social and Living Standard Measurement 2013 (PSLM), 2013), inadequate infrastructure, discrimination against women, political backwardness Ali et al., 2022, poverty, and unequal access to human capital (Shah et al., 2021).
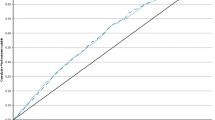
The low immunization rate is related to household poverty (Ye, 2021). According to Fig. 1, there is a strong correlation between the immunization rate and the household-based asset index in Punjab. We employed Naveed et al. (2021)'s estimation of a valid and accurate asset index at the household level as a validator to confirm the accuracy of the immunization rate index results. It also demonstrates the favourable correlation between the household-level asset index and the immunization index for children under the age of 5, offering valuable ex-post authentication of the immunization index. It displays the 95% confidence interval of the mean and the quantiles of the asset index for each immunization score.
The findings support the underlying hypothesis that households with low permanent incomes would have lower child immunization rates and households with high incomes would have higher immunization rates; this connection is non-linear. Our findings are in line with those provided by Wiysong et al. (2012) for developing countries, which demonstrate an association among income of the household and the child immunization rate.
4.1.2 An Empirical Estimation of the Anthropometric Undernourishment Composite Index and its Association to the Asset Index
The WHO Child Growth Standards are used in this study as a guide for the weight and height distribution of children under 5.
Table 5 indicates that approximately 34% of children are stunted, 17% are wasting, and 34% are underweight. The Composite Index of Anthropometric Failure (CIAF) suggests that around 48% of children are underprivileged, with only 52% of children having no reported anthropometric problems, as shown in Table 6. In Pakistan, malnutrition affects about one in two children. Our findings are consistent with those in the Pakistan Demographic and Health 2017–18 (PDHS) Survey and the National Nutrition Survey by UNICEF (2018). Regrettably, Pakistan's performance on measures relating to children is unsatisfactory. For instance, one of the highest rates in the world for child mortality is 74.9 deaths per 1000 live births. Also, around 22 million children do not attend school, 50% experience iron deficiency, and in some regions of Pakistan, more than 70% of children are undernourished. Additionally, about 44% of children experience chronic malnutrition, 33% experience acute malnutrition, and 15% experience both chronic and acute malnutrition.
Table 7 shows Punjab's less-than-5-year-old children's anthropometric status by district. Dera Ghazi Khan has the highest percentage of anthropometric failure in the CIAF, with 64%, Muzaffargarh has 60%, and Rahim Yar Khan has 59%. In contrast, the three districts with the lowest rates are Rawalpindi (31%), Attock (35%), and Jhelum (35%). As validators for all CIAF indicators, Naveed et al. (2021)'s asset index quintiles are used.Footnote 9
Figure 2 shows the connection between family income and the subgroup of anthropometric failure and the undernutrition that plagues the children of low-income families. It demonstrates the negative correlation between the CIAF and the household-based asset index, offering a valuable ex-post validation of the construct. Child undernutrition is axiomatically predicted to be inversely correlated with household permanent income (Worku et al., 2018).
The findings in Fig. 3 support the hypothesis that families in the lowest quintiles of assets experience the highest incidence of undernutrition and households in the highest quintiles of income experience the lowest anthropometric failure. An overall assessment of children's health is provided by the immunization rate and anthropometric achievement index.
4.1.3 An Empirical Estimation of the Cough, Tuberculosis, and Hepatitis Composite Index and its Association to the Asset Index
Physical health conditions are measured by the frequency of infectious diseases that can be fatal as the third domain of the health index. According to Table 8 findings, there are 49 cases of physical health deprivation (deficiency), 4 cases of tuberculosis, 15 cases of hepatitis, and 32 cases of chronic cough reported in Punjab for every 1000 people. A higher index value indicates worse physical health circumstances. The physical health deprivation index also displays a negative number of health-related variables. Therefore, in addition to the immunization rate and the anthropometric achievement index, the inverse of physical health deprivation is employed to produce the health index. In other words, a higher health index value indicates improved preventative measures, better diet, and better physical health conditions.
Figure 4 displays the district-level physical health conditions index. The overall health achievement indicator shows that Bhakkar, Khushab, and Mianwali perform the top, whereas Hafizabad and Muzaffargarh perform the worst. In Pakistan, hepatitis is one of the diseases that is spreading, with millions of people having HCV infection (Waheed et al., 2009). Hepatitis in Pakistan is spread through infected surgical and barbering devices, blood transfusions, and tainted drinking water (Kane et al., 1999; Rahut et al., 2020).
Lack of awareness and unavailability of medical tests for hepatitis for all household members may be the reason for this low perceived proportion of hepatitis in Punjab. In reality, the hepatitis number is expected to be much higher (Umar & Bilal, 2012). Figure 5 displays the error bar for the asset index and the physical health conditions index. Figure 6 represents the error bar for no prevalence of CHT individually, and the asset index. The relationship between the index of physical health conditions and the household asset index is clearly seen to be strongly positive in both Figures. Overall, the estimates of the health index are valid and reliable because high-income households experience quality living standards, good food, improved sanitation, and access to health facilities that prevent them from infectious diseases.
This study empirically confirmed that districts with higher education and income disparities have greater health disparities. Specifically, the Southern districts of Punjab have been found to have high levels of deprivation in child-related indicators such as malnutrition and immunization. These districts are made up of the province's most scattered and impoverished people (Khan & Hussain, 2020; Naveed & Khan, 2018). Access to child health facilities becomes more difficult when districts lack resources, and the population is scattered (Khan et al, 2023; Saleem et al., 2021). These districts' household earnings are primarily tied to agriculture. These districts are prone to flooding. As a result, household income resources and asset accumulation are highly fragile, having a negative impact on children's food and nutrition. Along with a lack of economic resources, political backwardness is a contributing factor to the health sector's underdevelopment (Ali et al, 2022). In Punjab's southern regions, poor infrastructure and a lack of safe drinking water are severe challenges. Poor sanitation and unclean drinking water are major causes of child malnutrition; also, a low immunization rate traps children in a vicious circle of infections (Rahut et al., 2020). Poor health and income pulled the people of these districts down the human development ladder. There should be a stronger emphasis on child poverty alleviation, particularly on enhancing children's education and health care (Shah et al., 2021; Wiysong et al., 2012).
4.2 District-level Health Index: The Results Reveals the Poor are Sick
The general health position of Punjab is highly positive despite reduced budgetary support for health, subpar medical facilities, and poor departmental coordination because at the moment, a sizable majority of Pakistan's population is young (Ali et al, 2022). Based on immunization rates, CIAF scores, and physical health status, each district in Punjab has achieved better health outcomes than other socioeconomic factors like income and education. According to Fig. 7, the health index places Dera Ghazi Khan, Rajanpur, and Muzaffargarh at the bottom, while Jhelum, Chakwal, and Gujrat are at the top. The physical health conditions index is generally lowering the health index and overstating the state of health in 36 districts. It won't be as high as it is now for each district's health index currently if it only includes the immunization rate and anthropometric accomplishment indices, but in that case, the health index would only be dependent on child health indicators (Khan & Hussain, 2020). We are unable to include access to general healthcare facilities and high-quality healthcare services in the formulation of a health index due to the data shortage.
To evaluate the construct's validity, the correlation between the household asset index and the health index is calculated. The household-based asset index deciles and the household-level health index have a substantial positive correlation, as shown in Fig. 8. It clearly shows that when the household-based health index is evaluated, the physical health condition index raises both the immunization index and the anthropometric achievement index. Figure 8 displays the deciles of the asset index and the 95% confidence band around the mean for the scores on household health. It supports the hypothesis that high-income families would have a high level of health index and low-income households would have a lower level. This connection has been demonstrated in much of the existing literature (Boen et al., 2021). We have created a household-level health index that is objectively valid based on the significant correlation between assets and health scores shown in Fig. 8. Also, it gives us assurance that it is okay for us to apply this index to calculate the health inequalities in 36 districts.
4.3 Using Alternative Methods to Estimate Punjab's Health Disparities
We illustrate the persistence of health disparities using multiple empirical methodologies and a variety of robustness checks. In this section of the investigation, the Palma ratio and Gini coefficient approaches are utilised to describe the health disparities among the 36 districts. Additionally, we analyse the relationship between socioeconomic factors and health disparities.
4.3.1 Health Disparities: The Estimates of Gini and Palma
The Gini-coefficient and Palma-ratio are estimated from the household based composite health index to compute health disparities in 36 districts of Punjab province of Pakistan.
Table 9, presented below, shows the distribution of health shares, the Palma ratio, and the Gini coefficient comparing the lowest 40% and the highest 10% within each district of Punjab. According to Table 9, of Punjab's 36 districts, Dera Gazi Khan (0.23), Rajanpur (0.21), and Muzaffargarh have the largest health inequalities (0.20). Jhelum (0.079), Chakwal (0.08), and Gujrat are the districts with the lowest health inequalities (0.09). The findings show that Southern Punjab districts have worse health inequalities than Central or Northern Punjab areas. The division of Dera Gazi Khan has the three districts with the biggest health inequalities, while Rawalpindi's division includes the three with the lowest. For instance, the Dera Gazi Khan district has the most unequal distribution of health index scores, with a Gini coefficient of 0.23 and the lowest 22% of the health share going to the bottom 40% of the population. In addition, the Dera Gazi Khan division's districts are all mostly underdeveloped, backward, and made up primarily of rural areas. The majority of Punjab's poor people live in this division, which also has substantial educational disparities, significant income disparities, and subpar socioeconomic indices like child mortality, employment, school enrolment, and human development.
The Dera Ghazi Khan district has the largest level of health disparities of all 36 districts, with the bottom 40% of the population receiving just 22% of the lowest health share and the top 10% receiving 15% of the highest. As a result, the Palma ratio of 0.64 is highest in the Dera Ghazi Khan district as compared to others, and the health index distribution is highly unequal. In contrast, the Palma ratio in Jhelum district is 0.32, with 34% of the health share going to the bottom 40% of the population Thus, the Jhelum district exhibits the minimal health disparities. Concordance between the Palma ratio and Gini coefficient regarding health disparities supports and confirms our analytical findings.
4.3.2 Between the Gini and Palma Techniques
The Gini coefficient and the Palma ratio indices are generally anticipated to be highly correlated. The Palma ratio does not include the middle 50% of the distribution in the analysis, while the Gini coefficient is responsive to the distribution's midpoint. But when it comes to district-level health index disparities, both approaches basically yield the same outcomes. This supports the Palma ratio approach's fundamental premise that the 50% in the middle of the distribution can be disregarded as a result of its low level of inconsistency (Palma, 2011, 2016). Figure 9's scatter plot shows that the Gini coefficient and Palma ratio have a very strong connection The relationship between the Palma ratio and the Gini coefficient is closely approximated by an exponential relationship.
We performed a regression analysis between the Gini coefficient and the two Palma ratio components in order to further confirm our results. Table 10 shows that the Palma components (the top 10% and bottom 40% of households' share of health) account for 99.8% of variations in the Gini coefficient. The positive sign for the top 10% indicates that Punjab's inequality would rise as the proportion of top 10% recipients rises. A rise in the percentage of the poorest 40% of individuals would result in a decrease in overall inequality, according to the negative sign for the lowest 40% of the population.
Figure 10 displays the relationship between the Gini coefficient and the percentage of health in the top 10% and bottom 40% of households. The findings are similar to Table 9 and Fig. 9. Hence, the volatility in the Gini coefficient efficiently explains the variation in the top 10% and lowest 40% of household health shares. Our findings are in line with those of Cobham and Sumner (2013) and Naveed et al. (2021), who found that the top 10% share is positively correlated with the Gini coefficient while the bottom 40% share is inversely related to estimates of Gini inequality.
The Palma ratio is considered the good indicator of inequality because of it simplicity. For instance, if the Gini coefficient index value is 0.5, it denotes a major inequality issue but has no immediate meaning to a non-technical audience. Conversely, if the Palma ratio is 5, it is clear that the richest 10% have 5 times as much as the poorest 40%.
4.3.3 The Illiterate Poor are Sick!
Low living standards and inadequate educational opportunities are linked to health risks. According to Mackenbach et al. (2014) and Karaoğlan and Saraçoğlu (2018), income of the household has a higher impact on a person's health status than medical services or facilities do. Public health facilities in Pakistan are insufficient in both quantity and quality (Khan et al., 2023). This section examines the connection between health disparities and socioeconomic factor disparities in order to verify the validity of our findings. In pursuit of this objective, we employed the Gini Coefficient to quantify health, income, and education disparities among districts using health, asset, and education indices, respectively. Figure 11a illustrates the correlation between health and education disparities, and Fig. 11b shows the relationship between income and health disparities. Figure 11a shows a substantial positive relationship between health and education disparities, and these disparities are greater in districts with higher poverty and illiteracy. Similarly, the findings in Fig. 11b are consistent with those in Fig. 11a regarding the strong association between income and health inequality. Figures 11a–b show that the districts in Southern Punjab, such as Dera Gazi G Khan, Muzaffargarh, Rajanpur, and Rahim Yar Khan, have higher income (asset) and education disparities, as well as higher health disparities. Health-related disparities are also less prevalent in the districts with lower economic disparities, such as Chakwal, Jhelum, and Gujrat. Similar results were seen for health and education gaps. Our results are in line with those in Dong et al. (2022), Karaoğlan and Saraçoğlu (2018), who provide evidence that the socioeconomic factors play key roles in health inequalities. This section comes to the conclusion that health disparities in Punjab province cannot be investigated in isolation and are instead explained by household-based economic disparities and education-related disparities. It is established that health disparities exist and that there is an association between socioeconomic characteristics like income and education and individual health outcomes (Braveman & Gottlieb, 2014).
5 Conclusions, Discussion and Policy Recommendations
In conclusion, this paper attempts to create a methodical discourse on the development of a household-based health index by taking into account numerous imperative health domains and empirically evaluating the construct's validity for the 36 districts of Punjab province. This study explicitly investigates the disparities in child health and whether these disparities differ amongst Punjab subregion districts. We make sure that we can use the results for this discussion by confirming all of our findings using a number of robustness checks. For instance, one of the goals of this paper is to estimate health disparities across all districts applying the Palma ratio and Gini coefficient and also to contrast the two approaches. Collectively, the findings provide robust evidence that child health inequalities are caused by unequal distribution of major socioeconomic variables (income and education disparities etc.) across different demographic groups. There is strong evidence that child health inequalities rise in districts with higher poverty and education gaps.
Our study reveals noteworthy patterns in the differences between the districts' rates of stunting underweight and wasting. According to the CIAF, 48% of children in Punjab experience anthropometric failure, with significantly higher rates exceeding 60% observed in districts located in Southern Punjab. This study's findings further underscore the poor state of Punjab's health sector, revealing that one in every two children under the age of five is affected by malnutrition, and over half of the children are not receiving the necessary immunizations.
A number of studies have found that socioeconomic variables play a significant influence in causing disparities in health outcomes (Braveman & Gottlieb, 2014; Karaoğlan & Saraçoğlu, 2018; Sen & Mondal, 2012). We also find significant disparities in child malnutrition in the Southern regions (e.g., in the districts of Dera Gazi Khan, Muzaffargarh, and Rajanpur etc.) compared to other regions. It is further evident that low vaccination rates were recorded in the areas with comparable higher poverty and lower literacy rates. The analysis also supports the prediction that families in the lowest quintiles of assets have the highest incidence of undernutrition and immunization rate and households in the top quintiles of income have the lowest undernutrition and immunization rate. This supports our hypothesis and other studies that households with low permanent incomes would have lower child immunization rates and undernutrition (Nandy et al., 2005; Shah et al., 2021; Worku et al., 2018; Ye, 2021). We suggest that reducing disparities in childhood malnutrition is significantly influenced by personal socio-economic factors such wealth status, parental illiteracy, and degree of knowledge regarding child nutrition and immunization.
A household with a high income is more likely to have adequate living circumstances, good food, improved sanitation, and access to health facilities that can protect them against infectious diseases (Dean & Fenton, 2010; O'Boyle & O'Boyle, 2012). In terms of physical health disparities, we observe a larger proportion of cough, tuberculosis, and hepatitis outcomes among low-income households, with differences varying among districts. According to the estimates, physical health conditions and asset index have a substantial positive association, implying that higher income districts may have less physical diseases such as cough, tuberculosis, and hepatitis than high poverty districts.
The empirical analysis revealed that the composite health index was significantly higher in the Central or Northern Punjab than Southern Punjab. This validates our initial findings from the health indicates, which show that there are significant health disparities between Punjab districts. To test the robustness of the findings, we calculated child health disparities using the Gini coefficient and the Palma ratio, as well as assessing their relationship with the asset index. We conclude that the greatest health disparities are seen in three districts of Southern Punjab: Dera Gazi Khan, Muzaffargarh, and Rajanpur districts. The district of Dera Gazi Khan, in particular, has the most unequal distribution of health index scores, with a lower Gini coefficient and the lowest health share going to the poorest 40% of the population. The results of this study also concluded a significant correlation between the Gini coefficient and the Palma ratio's constituent parts (Cobham & Sumner, 2013, Naveed et al., 2021). We find that, in districts with higher rates of poverty and illiteracy, the lowest 40% of households receive a smaller proportion of health care, which may lead to a rise in total health disparity in the children.
In order to provide additional support for our results, our study used the Gini coefficient approach to calculate three disparity measures: income, health, and education. The results imply a strong correlation between health, income, and education disparities and indicate that districts with higher rates of poverty and illiteracy also have higher health disparities. The aforementioned findings suggest that the observed disparities in child health in the Southern Punjab districts may be attributed to specific regional factors, such as low parental education, low socioeconomic status of the household, and varying levels of awareness regarding child nutrition and immunization (Ali et al., 2022; PSLM, 2013; Shah et al., 2021).
The findings imply that policymakers should focus on district-specific factors to reduce inequality in income distribution, education and health facilities, child nutrition, and immunization. For example, increasing water and sanitation coverage has the potential to alleviate malnutrition and nutrition inequality in rural regions, but only if complete populations are served (Mkupete et al., 2022). To further prevent health disparities, policymakers should work to raise the health share of the lowest 40% of the population. Particularly, in districts where access to healthcare is still disproportionately concentrated among the wealthy, policy initiatives can concentrate on expanding the availability of health services and raising public awareness of them (Khan et al., 2023). Health policymakers should conduct a survey designed specifically to measure child poverty as well as a public awareness campaign for child nutrition and immunization. It may be possible to lessen the disparity in children’s health by implementing well-thought-out policies that raise household per capita income and the level of education of family heads (Dong et al., 2022). These variables can only be handled on a big scale at the national level by policymakers and will most likely have an influence only in the long run, after sufficient resources are mobilised to achieve these goals. It is highly suggested that Southern Punjab implement these child health-related activities.
Despite its significant contributions to the literature, we acknowledge that our work suffers from limitations. Significant elements of health are not included in the composite household-based health index due to data restrictions, such as access to quality health services, satisfaction with services received, proportion share of income for health expenditures. The health analysis in this study is confined to Punjab, one province of Pakistan. In our subsequent project, we plan to expand the analysis to encompass all four provinces of the country. Although the estimates are confined to a cross-sectional examination of health disparities, a time trend estimation of health indicators and health disparities can be acquired by gathering data from different rounds of DHS and MICS surveys. Additionally, this paper's estimations are restricted to identifying health disparities and contrasting Gini & Palma's findings; yet, determining the socioeconomic, political, and geographic causes of health disparities would be a valuable addition to the subject.
Data Availability
We have used UNICEF data with their permission that is available online and some one may collect it by requesting UNICEF (link is given below), and we might not have the rights to share it without their permission. The link for online data https://mics.unicef.org/surveys.
Notes
The authors acknowledge the UNICEF for providing access to MICS05 datasets.
The asset index is used as proxy variable to measure long-term household income. The details on construction of asset index at household level are given in upcoming sections.
https://link.springer.com/article/10.1007/s11205-020-02594-3
Diphtheria-pertussis-tetanus (DPT), Hepatitis B (HepB) and Haemophilus influenza type B (HiB).
The following is a list of the assets: refrigerator, washing machine, air conditioner, car, computer, cater filter, stove, iron, motorbike, pump, mobile, watch, fan, bicycle, radio, electricity, phone, gas and financial assets (bank deposits).
References
Aburto, J. M., Villavicencio, F., Basellini, U., Kjærgaard, S., & Vaupel, J. W. (2020). Dynamics of life expectancy and life span equality. Proceedings of the National Academy of Sciences, 117(10), 5250–5259.
Acemoglu, D., & Johnson, S. (2007). Disease and development: The effect of life expectancy on economic growth. Journal of Political Economy, 115(6), 925–985.
Ali, H. A., Hartner, A. M., Echeverria-Londono, S., et al. (2022). Vaccine equity in low and middle income countries: A systematic review and meta-analysis. International Journal Equity Health, 21, 82.
Al-lela, O. Q. B., Bahari, M. B., Salih, M. R., Al-Abbassi, M. G., Elkalmi, R. M., & Jamshed, S. Q. (2014). Factors underlying inadequate parents’ awareness regarding pediatrics immunization: Findings of cross-sectional study in Mosul-Iraq. BMC Pediatrics, 14(1), 1–7.
Ataguba, O. A., & Ataguba, J. E. (2020). Social determinants of health: The role of effective communication in the COVID-19 pandemic in developing countries. Global Health Action, 13(1), 1788263.
Bellù, L. G., & Liberati, P. (2006). Inequality analysis: The Gini index. FAO, EASYPol Module, 40.
Berkley, S. (2015). Make vaccine coverage a key UN health indicator. Nature, 526(7572), 165–165.
Boen, C., Keister, L. A., & Graetz, N. (2021). Household wealth and child body mass index: Patterns and mechanisms. The Russell Sage Foundation Journal of the Social Sciences, 7(3), 80–100.
Boerma, J. T., Mathers, C., & Abou-Zahr, C. (2010). WHO and global health monitoring: The way forward. PLoS Medicine, 7(11), e1000373.
Braveman, P., & Gottlieb, L. (2014). The social determinants of health: It’s time to consider the causes of the causes. Public Health Reports, 129(1), 19–31.
Chan, M., Kazatchkine, M., Lob-Levyt, J., Obaid, T., Schweizer, J., Sidibe, M., . . . Yamada, T. (2010). Meeting the demand for results and accountability: A call for action on health data from eight global health agencies. PLoS Medicine, 7(1), e1000223.
Cobham, A., & Sumner, A. (2013). Putting the Gini Back in the Bottle? “The Palma” as a policy-relevant measure of inequality. Mimeograph, London: King’s College London.
De Maio, F. G. (2007). Income inequality measures. Journal of Epidemiol Community Health, 61(10), 849–852.
De Onis, M. (2017). World Health Organization child growth standards. Nutrition and Health in a Developing World, 119–141.
Dean, H. D., & Fenton, K. A. (2010). Addressing social determinants of health in the prevention and control of HIV/AIDS, viral hepatitis, sexually transmitted infections, and tuberculosis. Public Health Reports, 125(4), 1–5.
Dong, Y., Deng, Q., & Li, S. (2022). The health inequality of children in China: A regression-based decomposition analysis. Child Indicators Research, 15, 137–159.
Doyle, M., & Stiglitz, J. (2014). Eliminating extreme inequality: A sustainable development goal, 2015–2030. Ethics and International Affairs, 28(10), 1–7.
Eyal, N., Hurst, S., Norheim, O. F., & Wikler, D. (2013). Health inequality, Health Inequity and Health Spending. Inequalities in Health: Concepts, Measures, and Ethics (pp. 27–36). Oxford University Press.
Farooq, S., & Masud, F. (2021). Catastrophic health expenditure and poverty in Pakistan. The Pakistan Development Review, 60(1), 27–48.
Fotso, J. C. (2006). Child health inequities in developing countries: Differences across urban and rural areas. International Journal for Equity in Health, 5(1), 1–10.
Grépin, K. A., Irwin, B. R., & SasTrakinsky, B. (2020). On the measurement of financial protection: An assessment of the usefulness of the catastrophic health expenditure indicator to monitor progress towards universal health coverage. Health Systems & Reform, 6(1), e1744988.
Grimm, M., Harttgen, K., Klasen, S., & Misselhorn, M. (2008). A human development index by income groups. World Development, 36(12), 2527–2546.
Groves, R. M., & Peytcheva, E. (2008). The impact of nonresponse rates on nonresponse bias: A meta-analysis. Public Opinion Quarterly, 72(2), 2–31.
Gurung, C., & Sapkota, V. (2009). Prevalence and predictors of underweight, stunting and wasting in under-five children. Journal of Nepal Health Research Council, 7(15), 120–126.
Gwatkin, D. R. (2017). Trends in health inequalities in developing countries. The Lancet Global Health, 5(4), e371–e372.
Harttgen, K., & Klasen, S. (2012). A household-based human development index. World Development, 40(5), 878–899.
Hasan, Q., Bosan, A., & Bile, K. (2010). A review of EPI progress in Pakistan towards achieving coverage targets: Present situation and the way forward. EMHJ-Eastern Mediterranean Health Journal, 16(1), 31–38.
Hosseinpoor, A. R., Bergen, N., Schlotheuber, A., & Boerma, T. (2018). National health inequality monitoring: Current challenges and opportunities. Bulletin of the World Health Organization, 96(9), 654–659.
Howe, L. D., Hargreaves, J. R., & Huttly, S. R. A. (2008). Issues in the construction of wealth indices for the measurement of socio-economic position in low-income countries. Emerging Themes in Epidemiology, 5(3), 1–14.
Kahane, M., Hrynkiewicz, J., Supinska, J., Herbst, I., Bratkowski, A., Pawlisz, M. (2003) Human development report 2003: Millennium development goals: a compact among nations to end human poverty. New York
Kane, A., Lloyd, J., Zaffran, M., Simonsen, L., & Kane, M. (1999). Transmission of Hepatitis B, Hepatitis C and human immunodeficiency viruses through unsafe injections in the developing world: Model-based regional estimates. Bulletin of the World Health Organization, 77(10), 801–807.
Karaoğlan, D., & Saraçoğlu, D. S. (2018). Socio-economic factors affecting early childhood health: The case of Turkey. Child Indicators Research, 11(1), 1051–1075.
Khan, S. J., Asif, M., Aslam, S., Khan, W. J., & Hamza, S. A. (2023). Pakistan’s healthcare system: A review of major challenges and the first comprehensive universal health coverage initiative. Cureus, 15(9).
Khan, S. U., & Hussain, I. (2020). Inequalities in health and health-related indicators: A spatial geographic analysis of Pakistan. BMC Public Health, 20(1), 1–9.
Lisker, T. (2008). Is the Gini coefficient a stable measure of galaxy structure? The Astrophysical Journal, 179, 319–325.
Lucyk, K., Simmonds, K. A., Lorenzetti, D. A., Drews, S. J., & Svenson, M. L. R. (2019). The association between influenza vaccination and socioeconomic status in high income countries varies by the measure used: A systematic review. BMC Medical Research Methodology, 19(153), 1–23.
Mackenbach, J. P., Kulhanova, I., Menvielle, G., Bopp, M., Borrell, C., Costa, G., Deboosere, P., Esnaola, S., Kalediene, R., & Kovacs, K. (2014). Trends in inequalities in premature mortality: A study of 3.2 million deaths in 13 European countries. Journal of Epidemiology and Community Health, 69, 207–217.
Mathers, C. D., Boerma, T., & Ma Fat, D. (2009). Global and regional causes of death. British Medical Bulletin, 92(1), 7–32.
Micha, R. (2021). Global Nutrition Report: The State of Global Nutrition. Development Initiatives.
Mkupete, M. J., Fintel, D. V., & Burger, R. (2022). Decomposing inequality of opportunity in child health in Tanzania: The role of access to water and sanitation. Health Economics, 31(11), 2287–2511.
Nandy, S., & Miranda, J. J. (2008). Overlooking undernutrition? Using a composite index of anthropometric failure to assess how underweight misses and misleads the assessment of undernutrition in young children. Social Science & Medicine, 66(9), 1963–1966.
Nandy, S., Irving, M., Gordon, D., Subramanian, S., & Smith, G. D. (2005). Poverty, child undernutrition and morbidity: New evidence from India. Bulletin of the World Health Organization, 83, 210–216.
Nandy, S., & Svedberg, P. (2012). The Composite Index of Anthropometric Failure (CIAF): An alternative indicator for malnutrition in young children. Handbook of Anthropometry (pp. 127–137). Springer.
Naveed, T. A., Gordon, D., Ullah, S., & Zhang, M. (2021). The construction of an asset index at household level and measurement of economic disparities in Punjab (Pakistan) by using MICS-Micro data. Social Indicators Research, 155(1), 73–95.
Naveed, A., & Khan, S. A. (2018). Widening Disparities: public sector spending and poverty across districts in Punjab. Research Brief, Pakistan Poverty. Available http://www.ppaf.org.pk/doc/PolicyBriefs/25.Widening%20Disparities%20in%20Punjab.pdf. Accessed 24 June 2021
O’Boyle, E., & O’Boyle, M. P. (2012). Global poverty, hunger, death, and disease. International Journal of Social Economics, 39, 4–17.
Office for National Statistics (2018). Annual report of the Chief Medical Officer, 2018 Health 2040-better health within reach. https://assets.publishing.service.gov.uk/media/5c1ccb75ed915d730364be7c/Annual_report_of_the_Chief_Medical_Officer_2018_-_health_2040_-_better_health_within_reach.pdf
Owais, A., Hanif, B., Siddiqui, A. R., Agha, A., & Zaidi, A. K. M. (2011). Does improving maternal knowledge of vaccines impact infant immunization rates? A community-based randomized-controlled trail in Karachi, Pakistan. BMC Public Health, 11, 239.
Padmapriyadarsini, C., Pooranagangadevi, N., Chandrasekaran, K., Subramanyan, S., Thiruvalluvan, C., Bhavani, P., & Swaminathan, S. (2009). Prevalence of underweight, stunting, and wasting among children infected with human immunodeficiency virus in South India. International Journal of Pediatrics, 2009, 1–5.
Pakistan Bureau of Statistics GoP. Pakistan Social and Living Standard Measurement (2013). Available at https://aserpakistan.org/document/learning_resources/2014/PSLM/Findings%20PSLM%202012-2013.pdf
Pakistan Economic Survey (2016-17). Finance Division, Government of Pakistan, Islamabad. http://111.68.102.42:8080/xmlui/handle/123456789/15929?show=full
Palma, J. G. (2011). Homogeneous middles vs. heterogeneous tails, and the end of the ‘Inverted-U’: It’s All about the share of the rich. Development and Change, 42(1), 87–153.
Palma, J. G. (2016). Do nations just get the inequality they deserve? The 'Palma Ratio' Re-Examined. Inequality and Growth: Patterns and Policy, 35–97.
Pelletier, L. G., Vallerand, R. J., Green-Demers, I., Brière, N. M., & Blais, M. R. (1995). Leisure and mental health: Relationship between leisure involvement and psychological well-being. Canadian Journal of Behavioural Science, 27(2), 214–225.
Piqueras, P., Ballester, A., Durá-Gil, J. V., Martinez-Hervas, S., Redón, J., & Real, J. T. (2021). Anthropometric Indicators as a tool for diagnosis of obesity and other health risk factors: A literature review. Frontiers in Psychology, 12, 631179.
Rahut, D. B., Ali, A., Mottaleb, K. A., & Aryal, J. P. (2020). Understanding households’ choice of cooking fuels: Evidence from urban households in Pakistan. Asian Development Review, 37(1), 185–212.
Raskall, P., & Matheson, G. (1992). Understanding Gini Coefficient. SPRC Newsletter, 46.
Saleem, H., Shabbir, M. S., & Khan, B. (2021). Re-examining multidimensional poverty in Pakistan: A new assessment of regional variations. Global Business Review, 22(6), 1441–1458.
Santos, L. M. P., Paes-Sousa, R., Silva Junior, JBd., & Victora, C. G. (2008). National immunization day: A strategy to monitor health and nutrition indicators. Bulletin of the World Health Organization, 86, 474–479.
Sen, J., & Mondal, N. (2012). Socio-economic and demographic factors affecting the composite index of anthropometric failure (CIAF). Annals of Human Biology, 39(2), 129–136.
Shah, S. Z. A., Chaudhry, I. S., & Farooq, F. (2021). Poverty human capital and economic development Nexus: A case study of Multan division. Sustainable Business and Society in Emerging Economics, 3(1), 461–469.
Svedberg, P. (2000). Poverty and undernutrition: Theory, measurement, and policy. Clarendon Press.
Tate, J. E., Burton, A. H., Boschi-Pinto, C., Steele, A. D., Duque, J., & Parashar, U. D. (2012). 2008 estimate of worldwide rotavirus-associated mortality in children younger than 5 years before the introduction of universal rotavirus vaccination programmes: A systematic review and meta-analysis. The Lancet Infectious Diseases, 12(2), 136–141.
Umar, M., & Bilal, M. (2012). Hepatitis C, a Mega Menace: A Pakistani perspective. Journal Pakistan Medical Students, 2(2), 68–72.
UNICEF (2018). National Nutrition Survey 2018: Key Findings Report. https://www.unicef.org/pakistan/media/1951/file/Final%20Key%20Findings%20Report%202019.pdf
United Nations Development Programme. (2017). National Human Development Report 2017: Pakistan. New York.
Van Puyenbroeck, T. (2008). Proportional representation, Gini coefficients, and the principle of transfers. Journal of Theoretical Politics, 20, 498–526.
Waheed, Y., Shafi, T., Safi, S. Z., & Qadri, I. (2009). Hepatitis C virus in Pakistan: A systematic review of prevalence, genotypes and risk factors. World Journal of Gastroenterology, 15(45), 5647–5653.
Wiysong, C. S., Uthman, O. A., Ndumbe, P. M., & Hussey, G. D. (2012). Individual and contextual factors associated with low childhood immunisation coverage in Sub-Saharan Africa: A multilevel analysis. PLoS ONE, 7(5), e37905.
Worku, B. N., Abessa, T. G., Wondafrash, M., Vanvuchelen, M., Bruckers, L., Kolsteren, P., & Granitzer, M. (2018). The relationship of undernutrition/psychosocial factors and developmental outcomes of children in extreme poverty in Ethiopia. BMC Pediatrics, 45, 18–45.
World Health Organization. (2015). Global Reference list of 100 Core Health Indicators. WHO. https://apps.who.int/iris/bitstream/10665/173589/1/WHO_HIS_HSI_2015.3_eng.pdf?ua=1
World Health Organization. (2017). National health inequality monitoring: A step-by-step manual. WHO. https://apps.who.int/iris/handle/10665/255652
Ye, X. (2021). Exploring the relationship between Political Partisanship and COVID-19 vaccination rate. Journal of Public Health, fdab364.
Acknowledgements
The authors extend their appreciation to the anonymous referees, production department, and the editor for their valuable comments and suggestions on a previous draft of this article, which greatly contributed to its enhancement. Special gratitude is also expressed to Cyrus Zarrebini for providing proofreading assistance. Furthermore, the authors would like to acknowledge the University of Bath for managing the publication fee associated with the journal.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Tanveer Ahmed Naveed (TAN) Imran Hussain Shah (HIS) “Conceptualization, TAN, HIS: Methodology, TAN, HIS; validation, TAN, HIS; formal analysis, TAN, HIS; investigation, TAN, HIS; writing—original draft preparation, TAN, HIS.; data, TAN; writing—review and editing, TAN, HIS, ARAA; visualization, TAN, HIS, project administration, HIS; TAN, All authors have read, own and agreed to the published version of the manuscript.”
Corresponding author
Ethics declarations
Declarations
The authors declare that this manuscript has not be submitted to any other journal for simultaneous consideration.
Research Involving Human Participants and/or Animals
Not applicable.
Informed Consent
Not applicable.
Conflicts of Interest
I have no conflicts of interest to disclose.
Disclosure
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Naveed, T.A., Shah, I.H. Assessing Child Health Disparities: Evidence from a Household-Based Health Index in Punjab, Pakistan. Child Ind Res 17, 779–814 (2024). https://doi.org/10.1007/s12187-024-10103-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12187-024-10103-y