Abstract
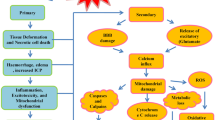
Numerous neurological disorders share a fatal pathologic process known as glutamate excitotoxicity. Among which, ischemic stroke is the major cause of mortality and disability worldwide. For a long time, the main idea of developing anti-excitotoxic neuroprotective agents was to block glutamate receptors. Despite this, there has been little successful clinical translation to date. After decades of “neuron-centered” views, a growing number of studies have recently revealed the importance of non-neuronal cells. Glial cells, cerebral microvascular endothelial cells, blood cells, and so forth are extensively engaged in glutamate synthesis, release, reuptake, and metabolism. They also express functional glutamate receptors and can listen and respond for fast synaptic transmission. This broadens the thoughts of developing excitotoxicity antagonists. In this review, the critical contribution of non-neuronal cells in glutamate excitotoxicity during ischemic stroke will be emphasized in detail, and the latest research progress as well as corresponding therapeutic strategies will be updated at length, aiming to reconceptualize glutamate excitotoxicity in a non-neuronal perspective.





Similar content being viewed by others
Data Availability
No datasets were generated or analyzed during the current study.
Abbreviations
- IS:
-
Ischemic stroke
- AIS:
-
Acute ischemic stroke
- FCI:
-
Focal cerebral ischemia
- tPA:
-
Tissue-type plasminogen activator
- Neu2000:
-
Nelonemdaz
- NA-1:
-
Nerinetide
- BBB:
-
Blood-brain barrier
- NMDAR:
-
NMDA receptor
- ROS:
-
Reactive oxygen species
- ECs:
-
Endothelial cells
- BMECs:
-
Brain microvascular endothelial cells
- MBMECs:
-
Mouse brain microvascular endothelial cells
- CNS:
-
Central nervous system
- EAAs:
-
Excitatory amino acids
- EAATs:
-
Excitatory amino acid transporters
- α-KG:
-
α-Ketoglutarate
- MCT-1:
-
Monocarboxylic acid transport 1
- GDH:
-
Glutamate dehydrogenase
- GLS:
-
Glutaminase
- ER:
-
Endoplasmic reticulum
- ICW:
-
Intracellular Ca2 + waves
- mGluRs:
-
Metabotropic glutamate receptors
- IP3:
-
Inositol 1,4,5-trisphosphate
- IP3R:
-
Inositol 1,4,5-trisphosphate receptor
- Gq-linked GPCR:
-
Gq-linked G protein-coupled receptor
- VGLUT:
-
Vesicular glutamate transporter
- VAMP:
-
Vesicle-associated membrane protein
- SNAP:
-
Synaptosomal-associated protein
- TREK-1:
-
TWIK-related K + channel 1
- Best-1:
-
Bestrophin-1
- HI:
-
Hypoxia-ischemia injury
- VRAC:
-
Volume-regulated anion channel
- MCAO:
-
Middle cerebral artery occlusion
- MCAO/R:
-
Middle cerebral artery occlusion/reperfusion
- pMCAO:
-
Permanent middle cerebral artery occlusion
- IClswell:
-
Swelling-activated Cl- current
- P2X7R:
-
Purinergic P2X7 receptors
- NLRP3:
-
Pyrin structural domain protein 3
- OGD:
-
Oxygen-glucose deprivation
- OGD/R:
-
Oxygen-glucose deprivation/reperfusion
- GJs:
-
Gap junctions
- GLAST:
-
Glutamate/aspartate transporter
- GLT-1:
-
Glutamate transporter-1
- rCCAs:
-
Rat cultured cortical astrocytes
- NCX:
-
Sodium/calcium exchanger
- OPCs:
-
Oligodendrocyte precursor cells
- CBX:
-
Carbenoxolone
- CEF:
-
Ceftriaxone
- SDH:
-
Succinate dehydrogenase
- OxAc:
-
Oxaloacetate
- GOT:
-
Glutamate-oxaloacetate transaminase
- hrGOT1:
-
Human recombinant GOT1
- Pyr:
-
Pyruvate
- GPT:
-
Glutamate-pyruvate transaminases
- PD:
-
Peritoneal dialysis
- NPCs:
-
Neural precursor cells
References
Feigin VL, Brainin M, Norrving B, Martins S, Sacco RL, Hacke W, Fisher M, Pandian J et al (2022) World Stroke Organization (WSO): global stroke fact sheet 2022. Int J Stroke 17:18–29. https://doi.org/10.1177/17474930211065917
Yamagata K (2021) Astrocyte-induced synapse formation and ischemic stroke. J Neurosci Res 99:1401–1413. https://doi.org/10.1002/jnr.24807
Walter K (2022) What is acute ischemic stroke? JAMA 327:885. https://doi.org/10.1001/jama.2022.1420
Wang F, Xie X, Xing X, Sun X (2022) Excitatory synaptic transmission in ischemic stroke: a new outlet for classical neuroprotective strategies. Int J Mol Sci 23:9381. https://doi.org/10.3390/ijms23169381
Lee JS, Lee JS, Gwag BJ, Choi DW, An CS, Kang HG, Song TJ, Ahn SH et al (2023) The rescue on reperfusion damage in cerebral infarction by nelonemdaz (RODIN) trial: protocol for a double-blinded clinical trial of nelonemdaz in patients with hyperacute ischemic stroke and endovascular thrombectomy. J Stroke 25:160–168. https://doi.org/10.5853/jos.2022.02453
Hill MD, Goyal M, Menon BK, Nogueira RG, McTaggart RA, Demchuk AM, Poppe AY, Buck BH et al (2020) Efficacy and safety of nerinetide for the treatment of acute ischaemic stroke (ESCAPE-NA1): a multicentre, double-blind, randomised controlled trial. Lancet 395:878–887. https://doi.org/10.1016/S0140-6736(20)30258-0
Su XT, Wang L, Ma SM, Cao Y, Yang NN, Lin LL, Fisher M, Yang JW et al (2020) Mechanisms of acupuncture in the regulation of oxidative stress in treating ischemic stroke. Oxid Med Cell Longev 2020:7875396. https://doi.org/10.1155/2020/7875396
Mira RG, Cerpa W (2021) Building a bridge between NMDAR-mediated excitotoxicity and mitochondrial dysfunction in chronic and acute diseases. Cell Mol Neurobiol 41:1413–1430. https://doi.org/10.1007/s10571-020-00924-0
Fan G, Liu M, Liu J, Huang Y (2023) The initiator of neuroexcitotoxicity and ferroptosis in ischemic stroke: glutamate accumulation. Front Mol Neurosci 16:1113081. https://doi.org/10.3389/fnmol.2023.1113081
Kaindl AM, Degos V, Peineau S, Gouadon E, Chhor V, Loron G, Le Charpentier T, Josserand J et al (2012) Activation of microglial N-methyl-D-aspartate receptors triggers inflammation and neuronal cell death in the developing and mature brain. Ann Neurol 72:536–549. https://doi.org/10.1002/ana.23626
Kim KS, Jeon MT, Kim ES, Lee CH, Kim DG (2022) Activation of NMDA receptors in brain endothelial cells increases transcellular permeability. Fluids Barriers CNS 19:70. https://doi.org/10.1186/s12987-022-00364-6
Andersen JV, Markussen KH, Jakobsen E, Schousboe A, Waagepetersen HS, Rosenberg PA, Aldana BI (2021) Glutamate metabolism and recycling at the excitatory synapse in health and neurodegeneration. Neuropharmacology 196:108719. https://doi.org/10.1016/j.neuropharm.2021.108719
Andersen JV, Schousboe A (2023) Milestone review: metabolic dynamics of glutamate and GABA mediated neurotransmission - the essential roles of astrocytes. J Neurochem 166:109–137. https://doi.org/10.1111/jnc.15811
Mahmoud S, Gharagozloo M, Simard C, Gris D (2019) Astrocytes maintain glutamate homeostasis in the CNS by controlling the balance between glutamate uptake and release. Cells 8:184. https://doi.org/10.3390/cells8020184
de Ceglia R, Ledonne A, Litvin DG, Lind BL, Carriero G, Latagliata EC, Bindocci E, Di Castro MA et al (2023) Specialized astrocytes mediate glutamatergic gliotransmission in the CNS. Nature 622:120–129. https://doi.org/10.1038/s41586-023-06502-w
Helms HC, Aldana BI, Groth S, Jensen MM, Waagepetersen HS, Nielsen CU, Brodin B (2017) Characterization of the L-glutamate clearance pathways across the blood-brain barrier and the effect of astrocytes in an in vitro blood-brain barrier model. J Cereb Blood Flow Metab 37:3744–3758. https://doi.org/10.1177/0271678X17690760
Kaplan-Arabaci O, Acari A, Ciftci P, Gozuacik D (2022) Glutamate scavenging as a neuroreparative strategy in ischemic stroke. Front Pharmacol 13:866738. https://doi.org/10.3389/fphar.2022.866738
Hinca SB, Salcedo C, Wagner A, Goldeman C, Sadat E, Aibar MMD, Maechler P, Brodin B et al (2020) Brain endothelial cells metabolize glutamate via glutamate dehydrogenase to replenish TCA-intermediates and produce ATP under hypoglycemic conditions. J Neurochem 157:1861–1875. https://doi.org/10.1111/jnc.15207
Pál B (2018) Involvement of extrasynaptic glutamate in physiological and pathophysiological changes of neuronal excitability. Cell Mol Life Sci 75:2917–2949. https://doi.org/10.1007/s00018-018-2837-5
Iovino L, Tremblay ME, Civiero L (2020) Glutamate-induced excitotoxicity in Parkinson’s disease: the role of glial cells. J Pharmacol Sci 144:151–164. https://doi.org/10.1016/j.jphs.2020.07.011
Xin W, Mironova YA, Shen H, Marino RAM, Waisman A, Lamers WH, Bergles DE, Bonci A (2019) Oligodendrocytes support neuronal glutamatergic transmission via expression of glutamine synthetase. Cell Rep 27:2262–2271. https://doi.org/10.1016/j.celrep.2019.04.094
Shen Z, Xiang M, Chen C, Ding F, Wang Y, Shang C, Xin L, Zhang Y et al (2022) Glutamate excitotoxicity: potential therapeutic target for ischemic stroke. Biomed Pharmacother 151:113125. https://doi.org/10.1016/j.biopha.2022.113125
Takeuchi H, Suzumura A (2014) Gap junctions and hemichannels composed of connexins: potential therapeutic targets for neurodegenerative diseases. Front Cell Neurosci 8:189. https://doi.org/10.3389/fncel.2014.00189
Takeuchi H, Jin S, Wang J, Zhang G, Kawanokuchi J, Kuno R, Sonobe Y, Mizuno T et al (2006) Tumor necrosis factor-alpha induces neurotoxicity via glutamate release from hemichannels of activated microglia in an autocrine manner. J Biol Chem 281:21362–21368. https://doi.org/10.1074/jbc.M600504200
Gao G, Li C, Zhu J, Wang Y, Huang Y, Zhao S, Sheng S, Song Y et al (2020) Glutaminase 1 regulates neuroinflammation after cerebral ischemia through enhancing microglial activation and pro-inflammatory exosome release. Front Immunol 7(11):161. https://doi.org/10.3389/fimmu.2020.00161
Gao G, Zhao S, Xia X, Li C, Li C, Ji C, Sheng S, Tang Y et al (2019) Glutaminase C regulates microglial activation and pro-inflammatory exosome release: relevance to the pathogenesis of Alzheimer’s disease. Front Cell Neurosci 13:264. https://doi.org/10.3389/fncel.2019.00264
Li H, Xie Y, Zhang N, Yu Y, Zhang Q, Ding S (2015) Disruption of IP3R2-mediated Ca2+ signaling pathway in astrocytes ameliorates neuronal death and brain damage while reducing behavioral deficits after focal ischemic stroke. Cell Calcium 58:565–576. https://doi.org/10.1016/j.ceca.2015.09.004
Alabi AA, Tsien RW (2013) Perspectives on kiss-and-run: role in exocytosis, endocytosis, and neurotransmission. Annu Rev Physiol 75:393–422. https://doi.org/10.1146/annurev-physiol-020911-153305
Zhang Q, Fukuda M, Van Bockstaele E, Pascual O, Haydon PG (2004) Synaptotagmin IV regulates glial glutamate release. Proc Natl Acad Sci USA 101:9441–9446. https://doi.org/10.1073/pnas.0401960101
Robinson IM, Ranjan R, Schwarz TL (2002) Synaptotagmins I and IV promote transmitter release independently of Ca2+ binding in the C2A domain. Nature 418:336–340. https://doi.org/10.1038/nature00915
Wang CT, Lu JC, Bai J, Chang PY, Martin TFJ, Chapman ER, Jackson MB (2003) Different domains of synaptotagmin control the choice between kiss-and-run and full fusion. Nature 424:943–947. https://doi.org/10.1038/nature01857
Sugita S, Han W, Butz S, Liu X, Fernández-Chacón R, Lao Y, Südhof TC (2001) Synaptotagmin VII as a plasma membrane Ca(2+) sensor in exocytosis. Neuron 30:459–473. https://doi.org/10.1016/S0896-6273(01)00290-2
Montana V, Ni Y, Sunjara V, Hua X, Parpura V (2004) Vesicular glutamate transporter-dependent glutamate release from astrocytes. J Neurosci 24:2633–2642. https://doi.org/10.1523/JNEUROSCI.3770-03.2004
Bezzi P, Gundersen V, Galbete JL, Seifert G, Steinhäuser C, Pilati E, Volterra A (2004) Astrocytes contain a vesicular compartment that is competent for regulated exocytosis of glutamate. Nat Neurosci 7:613–620. https://doi.org/10.1038/nn1246
Tao-Cheng JH, Pham A, Yang Y, Winters CA, Gallant PE, Reese TS (2014) Syntaxin 4 is concentrated on plasma membrane of astrocytes. Neuroscience 286:264–271. https://doi.org/10.1016/j.neuroscience.2014.11.054
Schubert V, Bouvier D, Volterra A (2011) SNARE protein expression in synaptic terminals and astrocytes in the adult hippocampus: a comparative analysis. Glia 59:1472–1488. https://doi.org/10.1002/glia.21190
Montana V, Liu W, Mohideen U, Parpura V (2009) Single molecule measurements of mechanical interactions within ternary SNARE complexes and dynamics of their disassembly: SNAP25 vs. SNAP23. J Physiol 587:1943–1960. https://doi.org/10.1113/jphysiol.2009.168575
Zhang Y, Chen K, Sloan SA, Bennett ML, Scholze AR, O’Keeffe S, Phatnani HP, Guarnieri P et al (2014) An RNA-sequencing transcriptome and splicing database of glia, neurons, and vascular cells of the cerebral cortex. J Neurosci 34:11929–11947. https://doi.org/10.1523/JNEUROSCI.1860-14.2014
Woo DH, Bae JY, Nam MH, An H, Ju YH, Won J, Choi JH, Hwang EM et al (2018) Activation of astrocytic μ-opioid receptor elicits fast glutamate release through TREK-1-containing K2P channel in hippocampal astrocytes. Front Cell Neurosci 12:319. https://doi.org/10.3389/fncel.2018.00319
Kim A, Jung HG, Kim SC, Choi M, Park JY, Lee SG, Hwang EM (2020) Astrocytic AEG-1 regulates expression of TREK-1 under acute hypoxia. Cell Biochem Funct 38:167–175. https://doi.org/10.1002/cbf.3469
Li F, Zhou SN, Zeng X, Li Z, Yang R, Wang XX, Meng B, Pei WL et al (2022) Activation of the TREK-1 potassium channel improved cognitive deficits in a mouse model of Alzheimer’s disease by modulating glutamate metabolism. Mol Neurobiol 59:5193–5206. https://doi.org/10.1007/s12035-022-02776-9
Wu X, Liu Y, Chen X, Sun Q, Tang R, Wang W, Yu Z, Xie M (2013) Involvement of TREK-1 activity in astrocyte function and neuroprotection under simulated ischemia conditions. J Mol Neurosci 49(3):499–506. https://doi.org/10.1007/s12031-012-9875-5
Zheng X, Yang J, Zhu Z, Fang Y, Tian Y, Xie M, Wang W, Liu Y (2022) The two-pore domain potassium channel TREK-1 promotes blood-brain barrier breakdown and exacerbates neuronal death after focal cerebral ischemia in mice. Mol Neurobiol 59:2305–2327. https://doi.org/10.1007/s12035-021-02702-5
Fan J, Du J, Zhang Z, Shi W, Hu B, Hu J, Xue Y, Li H et al (2022) The protective effects of hydrogen sulfide new donor methyl S-(4-fluorobenzyl)-N-(3,4,5-trimethoxybenzoyl)-l-cysteinate on the ischemic stroke. Molecules 27:1554. https://doi.org/10.3390/molecules27051554
Han KS, Woo J, Park H, Yoon BJ, Choi S, Lee CJ (2013) Channel-mediated astrocytic glutamate release via Bestrophin-1 targets synaptic NMDARs. Mol Brain 6:4. https://doi.org/10.1186/1756-6606-6-4
Park H, Han KS, Seo J, Lee J, Dravid SM, Woo J, Chun H, Cho S et al (2021) Channel-mediated astrocytic glutamate modulates hippocampal synaptic plasticity by activating postsynaptic NMDA receptors. Mol Brain 8:7. https://doi.org/10.1186/s13041-015-0097-y
Woo DH, Han KS, Shim JW, Yoon BE, Kim E, Bae JY, Oh SJ, Hwang EM et al (2012) TREK-1 and Best1 channels mediate fast and slow glutamate release in astrocytes upon GPCR activation. Cell 151:25–40. https://doi.org/10.1016/j.cell.2012.09.005
Oh SJ, Woo J, Lee YS, Cho M, Kim E, Cho NC, Park JY, Pae AN et al (2017) Direct interaction with 14–3-3γ promotes surface expression of Best1 channel in astrocyte. Mol Brain 10:51. https://doi.org/10.1186/s13041-017-0331-x
Owji AP, Yu K, Kittredge A, Wang J, Zhang Y, Yang T (2022) Bestrophin-2 and glutamine synthetase form a complex for glutamate release. Nature 611:180–187. https://doi.org/10.1038/s41586-022-05373-x
Golubinskaya V, Vontell R, Supramaniam V, Wyatt-Ashmead J, Gustafsson H, Mallard C, Nilsson H (2019) Bestrophin-3 expression in a subpopulation of astrocytes in the neonatal brain after hypoxic-ischemic injury. Front Physiol 10:23. https://doi.org/10.3389/fphys.2019.00023
Yang J, Vitery MDC, Chen J, Osei-Owusu J, Chu J, Qiu Z (2019) Glutamate-releasing SWELL1 channel in astrocytes modulates synaptic transmission and promotes brain damage in stroke. Neuron 102:813–827. https://doi.org/10.1016/j.neuron.2019.03.029
Wilson CS, Bach MD, Ashkavand Z, Norman KR, Martino N, Adam AP, Mongin AA (2019) Metabolic constraints of swelling-activated glutamate release in astrocytes and their implication for ischemic tissue damage. J Neurochem 151:255–272. https://doi.org/10.1111/jnc.14711
Balkaya M, Dohare P, Chen S, Schober AL, Fidaleo AM, Nalwalk JW, Sah R, Mongin AA (2023) Conditional deletion of LRRC8A in the brain reduces stroke damage independently of swelling-activated glutamate release. iScience 26:106669. https://doi.org/10.1016/j.isci.2023.106669
Schlichter LC, Mertens T, Liu B (2011) Swelling activated Cl- channels in microglia: biophysics, pharmacology and role in glutamate release. Channels (Austin) 5:128–137. https://doi.org/10.4161/chan.5.2.14310
Zhao YF, Tang Y, Illes P (2021) Astrocytic and oligodendrocytic P2X7 receptors determine neuronal functions in the CNS. Front Mol Neurosci 14:641570. https://doi.org/10.3389/fnmol.2021.641570
Pedata F, Dettori I, Coppi E, Melani A, Fusco I, Corradetti R, Pugliese AM (2016) Purinergic signalling in brain ischemia. Neuropharmacology 104:105–130. https://doi.org/10.1016/j.neuropharm.2015.11.007
Wang S, Wang B, Shang D, Zhang K, Yan X, Zhang X (2022) Ion channel dysfunction in astrocytes in neurodegenerative diseases. Front Physiol 13:814285. https://doi.org/10.3389/fphys.2022.814285
Sperlágh B, Zsilla G, Baranyi M, Illes P, Vizi ES (2007) Purinergic modulation of glutamate release under ischemic-like conditions in the hippocampus. Neuroscience 149:99–111. https://doi.org/10.1016/j.neuroscience.2007.07.035
Arbeloa J, Pérez-Samartín A, Gottlieb M, Matute C (2012) P2X7 receptor blockade prevents ATP excitotoxicity in neurons and reduces brain damage after ischemia. Neurobiol Dis 45:954–961. https://doi.org/10.1016/j.nbd.2011.12.014
Alves VS, da Silva JP, Rodrigues FC, Araújo SMB, Gouvêa AL, Leite-Aguiar R, Santos SACS, da Silva MSP et al (2023) P2X7 receptor contributes to long-term neuroinflammation and cognitive impairment in sepsis-surviving mice. Front Pharmacol 14:1179723. https://doi.org/10.3389/fphar.2023.1179723
Gu BJ, Wiley JS (2018) P2X7 as a scavenger receptor for innate phagocytosis in the brain. Br J Pharmacol 175:4195–4208. https://doi.org/10.1111/bph.14470
Wang Y, Zhu Y, Wang J, Dong L, Liu S, Li S, Wu Q (2023) Purinergic signaling: a gatekeeper of blood-brain barrier permeation. Front Pharmacol 14:1112758. https://doi.org/10.3389/fphar.2023.1112758
Ottestad-Hansen S, Hu QX, Follin-Arbelet VV, Bentea E, Sato H, Massie A, Zhou Y, Danbolt NC (2018) The cystine-glutamate exchanger (xCT, Slc7a11) is expressed in significant concentrations in a subpopulation of astrocytes in the mouse brain. Glia 66(5):951–970. https://doi.org/10.1002/glia.23294
Barger SW, Basile AS (2001) Activation of microglia by secreted amyloid precursor protein evokes release of glutamate by cystine exchange and attenuates synaptic function. J Neurochem 76:846–854. https://doi.org/10.1046/j.1471-4159.2001.00075.x
Satarker S, Bojja SL, Gurram PC, Mudgal J, Arora D, Nampoothiri M (2022) Astrocytic glutamatergic transmission and its implications in neurodegenerative disorders. Cells 11:1139. https://doi.org/10.3390/cells11071139
Rossi DJ, Oshima T, Attwell D (2000) Glutamate release in severe brain ischaemia is mainly by reversed uptake. Nature 403:316–321. https://doi.org/10.1038/35002090
Passlick S, Rose CR, Petzold GC, Henneberger C (2021) Disruption of glutamate transport and homeostasis by acute metabolic stress. Front Cell Neurosci 15:637784. https://doi.org/10.3389/fncel.2021.637784
Rao VL, Dogan A, Todd KG, Bowen KK, Kim BT, Rothstein JD, Dempsey RJ (2001) Antisense knockdown of the glial glutamate transporter GLT-1, but not the neuronal glutamate transporter EAAC1, exacerbates transient focal cerebral ischemia-induced neuronal damage in rat brain. J Neurosci 21:1876–1883. https://doi.org/10.1523/JNEUROSCI.21-06-01876.2001
Aizawa H, Sun W, Sugiyama K, Itou Y, Aida T, Cui W, Toyoda S, Terai H et al (2020) Glial glutamate transporter GLT-1 determines susceptibility to spreading depression in the mouse cerebral cortex. Glia 68(12):2631–2642. https://doi.org/10.1002/glia.23874
Liang Z, Wang X, Hao Y, Qiu L, Lou Y, Zhang Y, Ma D, Feng J (2020) The multifaceted role of astrocyte connexin 43 in ischemic stroke through forming hemichannels and gap junctions. Front Neurol 11:703. https://doi.org/10.3389/fneur.2020.00703
Socodato R, Portugal CC, Rodrigues A, Henriques J, Rodrigues C, Figueira C, Relvas JB (2018) Redox tuning of Ca2+ signaling in microglia drives glutamate release during hypoxia. Free Radic Biol Med 118:137–149. https://doi.org/10.1016/j.freeradbiomed.2018.02.036
Parkin GM, Udawela M, Gibbons A, Dean B (2018) Glutamate transporters, EAAT1 and EAAT2, are potentially important in the pathophysiology and treatment of schizophrenia and affective disorders. World J Psychiatry 8:51–63. https://doi.org/10.5498/wjp.v8.i2.51
Rao P, Yallapu MM, Sari Y, Fisher PB, Kumar S (2015) Designing novel nanoformulations targeting glutamate transporter excitatory amino acid transporter 2: implications in treating drug addiction. J Pers Nanomed 1:3–9
Hsu PC, Lan YJ, Chen CC, Lee LY, Chen WP, Wang YC, Lee YH (2022) Erinacine A attenuates glutamate transporter 1 downregulation and protects against ischemic brain injury. Life Sci 306:120833. https://doi.org/10.1016/j.lfs.2022.120833
Harvey BK, Airavaara M, Hinzman J, Wires EM, Chiocco MJ, Howard DB, Shen H, Gerhardt G et al (2011) Targeted over-expression of glutamate transporter 1 (GLT-1) reduces ischemic brain injury in a rat model of stroke. PLoS ONE 6:e22135. https://doi.org/10.1371/journal.pone.0022135
Rozyczka J, Figiel M, Engele J (2004) Endothelins negatively regulate glial glutamate transporter expression. Brain Pathol 14:406–614. https://doi.org/10.1111/j.1750-3639.2004.tb00084.x
Rodriguez-Kern A, Gegelashvili M, Schousboe A, Zhang J, Sung L, Gegelashvili G (2003) Beta-amyloid and brain-derived neurotrophic factor, BDNF, up-regulate the expression of glutamate transporter GLT-1/EAAT2 via different signaling pathways utilizing transcription factor NF-kappaB. Neurochem Int 43:363–370. https://doi.org/10.1016/s0197-0186(03)00023-8
Karki P, Webb A, Zerguine A, Choi J, Son DS, Lee E (2014) Mechanism of raloxifene-induced upregulation of glutamate transporters in rat primary astrocytes. Glia 62:1270–1283. https://doi.org/10.1002/glia.22679
Lee E, Sidoryk-Wegrzynowicz M, Yin Z, Webb A, Son DS, Aschner M (2012) Transforming growth factor-α mediates estrogen-induced upregulation of glutamate transporter GLT-1 in rat primary astrocytes. Glia 60:1024–1036. https://doi.org/10.1002/glia.22329
Autry AE, Grillo CA, Piroli GG, Rothstein JD, McEwen BS, Reagan LP (2006) Glucocorticoid regulation of GLT-1 glutamate transporter isoform expression in the rat hippocampus. Neuroendocrinology 83:371–379. https://doi.org/10.1159/000096092
Zorec R, Verkhratsky A, Rodríguez JJ, Parpura V (2016) Astrocytic vesicles and gliotransmitters: slowness of vesicular release and synaptobrevin2-laden vesicle nanoarchitecture. Neuroscience 323:67–75. https://doi.org/10.1016/j.neuroscience.2015.02.033
He X, Chen F, Zhang Y, Gao Q, Guan Y, Wang J, Zhou J, Zhai F, Boison D et al (2019) Upregulation of adenosine A2A receptor and downregulation of GLT1 is associated with neuronal cell death in Rasmussen’s encephalitis. Brain Pathol 30:246–260. https://doi.org/10.1111/bpa.12770
Hasel P, Dando O, Jiwaji Z, Baxter P, Todd AC, Heron S, Márkus NM, McQueen J et al (2017) Neurons and neuronal activity control gene expression in astrocytes to regulate their development and metabolism. Nat Commun 8:15132. https://doi.org/10.1038/ncomms15132
Lee ML, Martinez-Lozada Z, Krizman EN, Robinson MB (2017) Brain endothelial cells induce astrocytic expression of the glutamate transporter GLT-1 by a Notch-dependent mechanism. J Neurochem 143:489–506. https://doi.org/10.1111/jnc.14135
Martinez-Lozada Z, Robinson MB (2020) Reciprocal communication between astrocytes and endothelial cells is required for astrocytic glutamate transporter 1 (GLT-1) expression. Neurochem Int 139:104787. https://doi.org/10.1016/j.neuint.2020.104787
Sitcheran R, Gupta P, Fisher PB, Baldwin AS (2005) Positive and negative regulation of EAAT2 by NF-kappaB: a role for N-myc in TNFalpha-controlled repression. EMBO J 24:510–520. https://doi.org/10.1038/sj.emboj.7600555
Karki P, Webb A, Smith K, Johnson J Jr, Lee K, Son DS, Aschner M, Lee E (2014) Yin Yang 1 is a repressor of glutamate transporter EAAT2, and it mediates manganese-induced decrease of EAAT2 expression in astrocytes. Mol Cell Biol 34:1280–1289. https://doi.org/10.1128/MCB.01176-13
Helms HC, Aldana BI, Groth S, Jensen MM, Waagepetersen HS, Nielsen CU, Brodin B (2017) Characterization of the L-glutamate clearance pathways across the blood-brain barrier and the effect of astrocytes in an in vitro blood-brain barrier model. J Cereb Blood Flow Metab 37:3744–3758. https://doi.org/10.1177/0271678X17690760z
Castillo J, Loza MI, Mirelman D, Brea J, Blanco M, Sobrino T, Campos F (2016) A novel mechanism of neuroprotection: blood glutamate grabber. J Cereb Blood Flow Metab 36:292–301. https://doi.org/10.1177/0271678X15606721
Bonova P, Jachova J, Nemethova M, Bona M, Kollarova P, Gottlieb M (2021) Accelerated capacity of glutamate uptake via blood elements as a possible tool of rapid remote conditioning mediated tissue protection. Neurochem Int 142:104927. https://doi.org/10.1016/j.neuint.2020.104927
Hinca SB, Salcedo C, Wagner A, Goldeman C, Sadat E, Aibar MMD, Maechler P, Brodin B et al (2021) Brain endothelial cells metabolize glutamate via glutamate dehydrogenase to replenish TCA-intermediates and produce ATP under hypoglycemic conditions. J Neurochem 157:1861–1875. https://doi.org/10.1111/jnc.15207
Pitt D, Nagelmeier IE, Wilson HC, Raine CS (2003) Glutamate uptake by oligodendrocytes: implications for excitotoxicity in multiple sclerosis. Neurology 61:1113–1120. https://doi.org/10.1212/01.wnl.0000090564.88719.37
Hogan-Cann AD, Anderson CM (2016) Physiological roles of non-neuronal NMDA receptors. Trends Pharmacol Sci 37:750–767. https://doi.org/10.1016/j.tips.2016.05.012
Verkhratsky A, Chvátal A. NMDA receptors in astrocytes (2020) Neurochem Res 45(1):122–133. https://doi.org/10.1007/s11064-019-02750-3
Palygin O, Lalo U, Pankratov Y (2011) Distinct pharmacological and functional properties of NMDA receptors in mouse cortical astrocytes. Br J Pharmacol 163:1755–1766. https://doi.org/10.1111/j.1476-5381.2011.01374.x
Krebs C, Fernandes HB, Sheldon C, Raymond LA, Baimbridge KG (2003) Functional NMDA receptor subtype 2B is expressed in astrocytes after ischemia in vivo and anoxia in vitro. J Neurosci 23:3364–3372. https://doi.org/10.1523/JNEUROSCI.23-08-03364.2003
Zhou Y, Li HL, Zhao R, Yang LT, Dong Y, Yue X, Ma YY, Wang Z et al (2010) Astrocytes express N-methyl-D-aspartate receptor subunits in development, ischemia and post-ischemia. Neurochem Res 35:2124–2134. https://doi.org/10.1007/s11064-010-0325-x
Dzamba D, Honsa P, Valny M, Kriska J, Valihrach L, Novosadova V, Kubista M, Anderova M (2015) Quantitative analysis of glutamate receptors in glial cells from the cortex of GFAP/EGFP mice following ischemic injury: focus on NMDA receptors. Cell Mol Neurobiol 35:1187–1202. https://doi.org/10.1007/s10571-015-0212-8
de Oca M, Balderas P, Aguilera P (2015) A metabotropic-like flux-independent NMDA receptor regulates Ca2+ exit from endoplasmic reticulum and mitochondrial membrane potential in cultured astrocytes. PLoS ONE 10:e0126314. https://doi.org/10.1371/journal.pone.0126314
Ziemens D, Oschmann F, Gerkau NJ, Rose CR (2019) Heterogeneity of activity induced sodium transients between astrocytes of the mouse hippocampus and neocortex: mechanisms and consequences. J Neurosci 39:2620–2634. https://doi.org/10.1523/JNEUROSCI.2029-18.2019
Sultan S, Li L, Moss J, Petrelli F, Casse F, Gebara E, Lopatar J, Pfrieger FW et al (2015) Synaptic integration of adult-born hippocampal neurons is locally controlled by astrocytes. Neuron 88:957–972. https://doi.org/10.1016/j.neuron.2015.10.037
Papouin T, Dunphy JM, Tolman M, Dineley KT, Haydon PG (2017) Septal cholinergic neuromodulation tunes the astrocyte-dependent gating of hippocampal NMDA receptors to wakefulness. Neuron 94:840–854. https://doi.org/10.1016/j.neuron.2017.04.021
Bodner O, Radzishevsky I, Foltyn VN, Touitou A, Valenta AC, Rangel IF, Panizzutti R, Kennedy RT et al (2020) D-Serine signaling and NMDAR-mediated synaptic plasticity are regulated by system A-type of glutamine/D-serine dual transporters. J Neurosci 40:6489–6502. https://doi.org/10.1523/JNEUROSCI.0801-20.2020
Lalo U, Palygin O, Rasooli-Nejad S, Andrew J, Haydon PG, Pankratov Y (2014) Exocytosis of ATP from astrocytes modulates phasic and tonic inhibition in the neocortex. PLoS Biol 12:e1001747. https://doi.org/10.1371/journal.pbio.1001747
Boue-Grabot E, Pankratov Y (2017) Modulation of central synapses by astrocyte released ATP and postsynaptic P2X receptors. Neural Plast 2017:9454275. https://doi.org/10.1155/2017/9454275
Stenovec M, Lasič E, Božić M, Bobnar ST, Stout RF Jr, Grubišić V, Parpura V, Zorec R (2016) Ketamine inhibits ATP-evoked exocytotic release of brain-derived neurotrophic factor from vesicles in cultured rat astrocytes. Mol Neurobiol 53:6882–6896. https://doi.org/10.1007/s12035-015-9562-y
Verkhratsky A, Untiet V, Rose CR (2020) Ionic signalling in astroglia beyond calcium. J Physiol 598:1655–1670. https://doi.org/10.1113/JP277478
Hogan-Cann AD, Lu P, Anderson CM (2019) Endothelial NMDA receptors mediate activity-dependent brain hemodynamic responses in mice. Proc Natl Acad Sci USA 116:10229–10231. https://doi.org/10.1073/pnas.1902647116
Lu L, Hogan-Cann AD, Globa AK, Lu P, Nagy JI, Bamji SX, Anderson CM (2019) Astrocytes drive cortical vasodilatory signaling by activating endothelial NMDA receptors. J Cereb Blood Flow Metab 39:481–496. https://doi.org/10.1177/0271678X17734100
Mapelli L, Gagliano G, Soda T, Laforenza U, Moccia F, D’Angelo EU (2017) Granular layer neurons control cerebellar neurovascular coupling through an NMDA receptor/NO-dependent system. J Neurosci 37:1340–1351. https://doi.org/10.1523/JNEUROSCI.2025-16.2016
Mishra A, Reynolds JP, Chen Y, Gourine AV, Rusakov DA, Attwell D (2016) Astrocytes mediate neurovascular signaling to capillary pericytes but not to arterioles. Nat Neurosci 19:1619–1627. https://doi.org/10.1038/nn.4428
Epping L, Schroeter CB, Nelke C, Bock S, Gola L, Ritter N, Herrmann AM, Räuber S et al (2022) Activation of non-classical NMDA receptors by glycine impairs barrier function of brain endothelial cells. Cell Mol Life Sci 79:479. https://doi.org/10.1007/s00018-022-04502-z
Saab AS, Tzvetavona ID, Trevisiol A, Baltan S, Dibaj P, Kusch K, Mobius W, Goetze B et al (2016) Oligodendroglial NMDA receptors regulate glucose import and axonal energy metabolism. Neuron 91:119–132. https://doi.org/10.1016/j.neuron.2016.05.016
Karadottir R, Cavelier P, Bergersen LH, Attwell D (2005) NMDA receptors are expressed in oligodendrocytes and activated in ischaemia. Nature 438:1162–1166. https://doi.org/10.1038/nature04302
Micu I, Jiang Q, Coderre E, Ridsdale A, Zhang L, Woulfe J, Yin X, Trapp BD et al (2006) NMDA receptors mediate calcium accumulation in myelin during chemical ischaemia. Nature 439:988–992. https://doi.org/10.1038/nature04474
Cao N, Yao ZX (2013) Oligodendrocyte N-methyl-D-aspartate receptor signaling: insights into its functions. Mol Neurobiol 47:845–856. https://doi.org/10.1007/s12035-013-8408-8
Li C, Xiao L, Liu X, Yang W, Shen W, Hu C, Yang G, He C (2013) A functional role of NMDA receptor in regulating the differentiation of oligodendrocyte precursor cells and remyelination. Glia 61:732–749. https://doi.org/10.1002/glia.22469
De Biase LM, Kang SH, Baxi EG, Fukaya M, Pucak ML, Mishina M, Calabresi PA, Bergles DE (2011) NMDA receptor signaling in oligodendrocyte progenitors is not required for oligodendrogenesis and myelination. J Neurosci 31:12650–12662. https://doi.org/10.1523/JNEUROSCI.2455-11.2011
Murugan M, Sivakumar V, Lu J, Ling EA, Kaur C (2011) Expression of N-methyl D-aspartate receptor subunits in amoeboid microglia mediates production of nitric oxide via NF-κB signaling pathway and oligodendrocyte cell death in hypoxic postnatal rats. Glia 59:521–539. https://doi.org/10.1002/glia.21121
Todd L, Palazzo I, Suarez L, Liu X, Volkov L, Hoang TV, Campbell WA, Blackshaw S et al (2019) Reactive microglia and IL1β/IL-1R1-signaling mediate neuroprotection in excitotoxin-damaged mouse retina. J Neuroinflammation 16:118. https://doi.org/10.1186/s12974-019-1505-5
Mazella J, Pétrault O, Lucas G, Deval E, Béraud-Dufour S, Gandin C, El-Yacoubi M, Widmann C et al (2010) Spadin, a sortilin-derived peptide, targeting rodent TREK-1 channels: a new concept in the antidepressant drug design. PLoS Biol 8:e1000355. https://doi.org/10.1371/journal.pbio.1000355
Pietri M, Djillani A, Mazella J, Borsotto M, Heurteaux C (2019) First evidence of protective effects on stroke recovery and post-stroke depression induced by sortilin-derived peptides. Neuropharmacology 158:107715. https://doi.org/10.1016/j.neuropharm.2019.107715
Moha Ou Maati H, Veyssiere J, Labbal F, Coppola T, Gandin C, Widmann C, Mazella J, Heurteaux C et al (2012) Spadin as a new antidepressant: absence of TREK-1-related side effects. Neuropharmacology 62:278–288. https://doi.org/10.1016/j.neuropharm.2011.07.019
Deng ZH, Liao J, Zhang JY, Liang C, Song CH, Han M, Wang LH, Xue H et al (2014) Inhibition of the connexin 43 elevation may be involved in the neuroprotective activity of leptin against brain ischemic injury. Cell Mol Neurobiol 34:871–879. https://doi.org/10.1007/s10571-014-0066-5
Ma D, Feng L, Cheng Y, Xin M, You J, Yin X, Hao Y, Cui L et al (2018) Astrocytic gap junction inhibition by carbenoxolone enhances the protective effects of ischemic preconditioning following cerebral ischemia. J Neuroinflammation 15:198. https://doi.org/10.1186/s12974-018-1230-5
Yin X, Feng L, Ma D, Yin P, Wang X, Hou S, Hao Y, Zhang J et al (2018) Roles of astrocytic connexin-43, hemichannels, and gap junctions in oxygen-glucose deprivation/reperfusion injury induced neuroinflammation and the possible regulatory mechanisms of salvianolic acid B and carbenoxolone. J Neuroinflammation 15:97. https://doi.org/10.1186/s12974-018-1127-3
Li X, Zhao H, Tan X, Kostrzewa RM, Du G, Chen Y, Zhu J, Miao Z et al (2015) Inhibition of connexin43 improves functional recovery after ischemic brain injury in neonatal rats. Glia 63:1553–1567. https://doi.org/10.1002/glia.22826
Marsh SR, Williams ZJ, Pridham KJ, Gourdie RG (2021) Peptidic Connexin43 therapeutics in cardiac reparative medicine. J Cardiovasc Dev Dis 8:52. https://doi.org/10.3390/jcdd8050052
Abulseoud OA, Alasmari F, Hussein AM, Sari Y (2022) Ceftriaxone as a novel therapeutic agent for hyperglutamatergic states: bridging the gap between preclinical results and clinical translation. Front Neurosci 16:841036. https://doi.org/10.3389/fnins.2022.841036
Rao PS, Saternos H, Goodwani S, Sari Y (2015) Effects of ceftriaxone on GLT1 isoforms, xCT and associated signaling pathways in P rats exposed to ethanol. Psychopharmacology 232:2333–2342. https://doi.org/10.1007/s00213-015-3868-3
Shen Y, He P, Fan YY, Zhang JX, Yan HJ, Hu WW, Ohtsu H, Chen Z (2010) Carnosine protects against permanent cerebral ischemia in histidine decarboxylase knockout mice by reducing glutamate excitotoxicity. Free radical bio med 48:727–735. https://doi.org/10.1016/j.freeradbiomed.2009.12.021
Jain S, Kim ES, Kim D, Burrows D, De Felice M, Kim M, Baek SH, Ali A et al (2020) Comparative cerebroprotective potential of d- and l-carnosine following ischemic stroke in mice. Int J Mol Sci 21:3053. https://doi.org/10.3390/ijms21093053
Melani A, Dettori I, Corti F, Cellai L, Pedata F (2015) Time-course of protection by the selective A2A receptor antagonist SCH58261 after transient focal cerebral ischemia. Neurol Sci 36:1441–1448. https://doi.org/10.1007/s10072-015-2160-y
Zhou Y, Zeng X, Li G, Yang Q, Xu J, Zhang M, Mao X, Cao Y et al (2019) Inactivation of endothelial adenosine A2A receptors protects mice from cerebral ischaemia-induced brain injury. Br J Pharmacol 176:2250–2263. https://doi.org/10.1111/bph.14673
Han BR, Lin SC, Espinosa K, Thorne PR, Vlajkovic SM (2019) Inhibition of the adenosine A2A receptor mitigates excitotoxic injury in organotypic tissue cultures of the rat cochlea. Cells 8:877. https://doi.org/10.3390/cells8080877
Lin Z, Huang P, Huang S, Guo L, Xu X, Shen X, Xie B, Zhong Y (2018) Effect of adenosine and adenosine receptor antagonists on retinal Müller cell inwardly rectifying potassium channels under exogenous glutamate stimulation. Biomed Res Int 2018:2749257. https://doi.org/10.1155/2018/2749257
Liu Y, Chu S, Hu Y, Yang S, Li X, Zheng Q, Ai Q, Ren S et al (2021) Exogenous adenosine antagonizes excitatory amino acid toxicity in primary astrocytes. Cell Mol Neurobiol 41:687–704. https://doi.org/10.1007/s10571-020-00876-5
Peng M, Ling X, Song R, Gao X, Liang Z, Fang F, Cang J (2019) Upregulation of GLT-1 via PI3K/Akt pathway contributes to neuroprotection induced by dexmedetomidine. Front Neurol 10:1041. https://doi.org/10.3389/fneur.2019.01041
Taheri F, Sattari E, Hormozi M, Ahmadvand H, Bigdeli MR, Kordestani-Moghadam P, Anbari K, Milanizadeh S et al (2022) Dose-dependent effects of astaxanthin on ischemia/reperfusion induced brain injury in MCAO model rat. Neurochem Res 47:1736–1750. https://doi.org/10.1007/s11064-022-03565-5
Zhang X, Shi M, Bjørås M, Wang W, Zhang G, Han J, Liu Z, Zhang Y et al (2013) Ginsenoside Rd promotes glutamate clearance by up-regulating glial glutamate transporter GLT-1 via PI3K/AKT and ERK1/2 pathways. Front Pharmacol 4:152. https://doi.org/10.3389/fphar.2013.00152
Ferreira RS, Teles-Souza J, Dos Santos Souza C, Pereira ÉPL, de Araújo FM, da Silva AB, Castro E Silva JH, Nonose Y, et al (2021) Rutin improves glutamate uptake and inhibits glutamate excitotoxicity in rat brain slices. Mol Biol Rep 48:1475-1483https://doi.org/10.1007/s11033-021-06145-y
Song X, Gong Z, Liu K, Kou J, Liu B, Liu K (2020) Baicalin combats glutamate excitotoxicity via protecting glutamine synthetase from ROS-induced 20S proteasomal degradation. Redox Biol 34:101559. https://doi.org/10.1016/j.redox.2020.101559
Dopico-López A, Pérez-Mato M, da Silva-Candal A, Iglesias-Rey R, Rabinkov A, Bugallo-Casal A, Sobrino T, Mirelman D et al (2021) Inhibition of endogenous blood glutamate oxaloacetate transaminase enhances the ischemic damage. Transl Res 230:68–81. https://doi.org/10.1016/j.trsl.2020.10.004
Pérez-Mato M, Ramos-Cabrer P, Sobrino T, Blanco M, Ruban A, Mirelman D, Menendez P, Castillo J et al (2014) Human recombinant glutamate oxaloacetate transaminase 1 (GOT1) supplemented with oxaloacetate induces a protective effect after cerebral ischemia. Cell Death Dis 5:e992. https://doi.org/10.1038/cddis.2013.507
Zaghmi A, Dopico-López A, Pérez-Mato M, Iglesias-Rey R, Hervella P, Greschner AA, Bugallo-Casal A, da Silva A et al (2020) Sustained blood glutamate scavenging enhances protection in ischemic stroke. Commun Biol 3:729. https://doi.org/10.1038/s42003-020-01406-1
Frank D, Kuts R, Tsenter P, Gruenbaum BF, Grinshpun Y, Zvenigorodsky V, Shelef I, Natanel D et al (2019) The effect of pyruvate on the development and progression of post-stroke depression: a new therapeutic approach. Neuropharmacology 155:173–184. https://doi.org/10.1016/j.neuropharm.2019.05.035
Godino Mdel C, Romera VG, Sánchez-Tomero JA, Pacheco J, Canals S, Lerma J, Vivancos J, Moro MA et al (2013) Amelioration of ischemic brain damage by peritoneal dialysis. J Clin Invest 123:4359–4363. https://doi.org/10.1172/JCI67284
Davies S, Lally F, Satchithananda D, Kadam U, Roffe C (2014) Extending the role of peritoneal dialysis: can we win hearts and minds? Nephrol Dial Transplant 29:1648–1654. https://doi.org/10.1093/ndt/gfu001
Bacigaluppi M, Russo GL, Peruzzotti-Jametti L, Rossi S, Sandrone S, Butti E, De Ceglia R, Bergamaschi A et al (2016) Neural stem cell transplantation induces stroke recovery by upregulating glutamate transporter GLT-1 in astrocytes. J Neurosci 36:10529–10544. https://doi.org/10.1523/JNEUROSCI.1643-16.2016
Pérez-Mato M, Iglesias-Rey R, Vieites-Prado A, Dopico-López A, Argibay B, Fernández-Susavila H, da Silva-Candal A, Pérez-Díaz A et al (2019) Blood glutamate EAAT2-cell grabbing therapy in cerebral ischemia. EBioMedicine 39:118–131. https://doi.org/10.1016/j.ebiom.2018.11.024
Funding
This study was supported by the key projects of Shandong (China) Natural Science Fund [grant number ZR2020KH003] (Sponsor: Bing-bing Han) and the Student Innovation and Entrepreneurship Training Program of Shandong Province [grant number 2022083] (Sponsor: Tian-he Fang).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Literature collection and summarization were performed by Hao Yu, Jia-xin Li, Na Li, Chong Li, Dong-han Xu, Hao Zhang, and Tian-he Fang. The first draft of the manuscript was written by Xiao-man Yang. Review and editing were done by Shi-jun Wang, Pei-yu Yan, and Bing-bing Han. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiao-man Yang and Hao Yu are the co-first authors.
Shi-jun Wang and Pei-yu Yan are the co-corresponding authors; the main corresponding author is Bing-bing Han.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, Xm., Yu, H., Li, Jx. et al. Excitotoxic Storms of Ischemic Stroke: A Non-neuronal Perspective. Mol Neurobiol (2024). https://doi.org/10.1007/s12035-024-04184-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12035-024-04184-7