Abstract
Parkinson's disease (PD), the second-most prevalent neurodegenerative disorder, is characterized by the aberrant deposition of α-synuclein (α-Syn) aggregation in neurons. Recent reports have shown that retinoic acid (RA) ameliorates motor deficits. However, the underlying molecular mechanisms remain unclear. In this article, we investigated the effects of RA on cellular and animal models of PD. We found that RA is beneficial for neuronal survival in PD-associated models. In α-Syn preformed fibrils-treated mice, RA administration relieved the formation of intracellular inclusions, dopaminergic neuronal loss, and behavioral deficits. α-Syn preformed fibrils-treated SH-SY5Y cells manifested decreased cell viability, apoptosis, α-Syn aggregation, and autophagy defects. All these negative phenomena were alleviated by RA. More importantly, RA could inhibit the neurotoxicity via inhibiting α-Syn preformed fibrils-induced STAT1-PARP1 signaling, which could also be antagonized by IFN-γ. In conclusion, RA could hinder α-Syn preformed fibrils-induced toxicity by inhibiting STAT1-PARP1 signaling. Thus, we present new insight into RA in PD management.










Similar content being viewed by others
Data Availability
The authors declare that all data supporting the findings of this study are available within the article.
References
Dorsey ER, Bloem BR (2018) The Parkinson Pandemic-A Call to Action. JAMA Neurol 75(1):9–10. https://doi.org/10.1001/jamaneurol.2017.3299
Kalia LV, Lang AE (2015) Parkinson’s disease. Lancet 386(9996):896–912. https://doi.org/10.1016/S0140-6736(14)61393-3
Tysnes OB, Storstein A (2017) Epidemiology of Parkinson’s disease. J Neural Transm (Vienna) 124(8):901–905. https://doi.org/10.1007/s00702-017-1686-y
Winner B, Jappelli R, Maji SK, Desplats PA, Boyer L, Aigner S, Hetzer C, Loher T et al (2011) In vivo demonstration that alpha-synuclein oligomers are toxic. Proc Natl Acad Sci U S A 108(10):4194–4199. https://doi.org/10.1073/pnas.1100976108
Luk KC, Kehm V, Carroll J, Zhang B, O’Brien P, Trojanowski JQ, Lee VM (2012) Pathological alpha-synuclein transmission initiates Parkinson-like neurodegeneration in nontransgenic mice. Science 338(6109):949–953. https://doi.org/10.1126/science.1227157
Spillantini MG, Schmidt ML, Lee VM, Trojanowski JQ, Jakes R, Goedert M (1997) Alpha-synuclein in Lewy bodies. Nature 388(6645):839–840. https://doi.org/10.1038/42166
Kalia LV, Kalia SK, McLean PJ, Lozano AM, Lang AE (2013) alpha-Synuclein oligomers and clinical implications for Parkinson disease. Ann Neurol 73(2):155–169. https://doi.org/10.1002/ana.23746
Krishnakumar R, Kraus WL (2010) The PARP side of the nucleus: molecular actions, physiological outcomes, and clinical targets. Mol Cell 39(1):8–24. https://doi.org/10.1016/j.molcel.2010.06.017
Gupte R, Liu Z, Kraus WL (2017) PARPs and ADP-ribosylation: recent advances linking molecular functions to biological outcomes. Genes Dev 31(2):101–126. https://doi.org/10.1101/gad.291518.116
Szanto M, Bai P (2020) The role of ADP-ribose metabolism in metabolic regulation, adipose tissue differentiation, and metabolism. Genes Dev 34(5–6):321–340. https://doi.org/10.1101/gad.334284.119
Ke Y, Han Y, Guo X, Wen J, Wang K, Jiang X, Tian X, Ba X et al (2017) PARP1 promotes gene expression at the post-transcriptiona level by modulating the RNA-binding protein HuR. Nat Commun 8:14632. https://doi.org/10.1038/ncomms14632
Mao K, Chen J, Yu H, Li H, Ren Y, Wu X, Wen Y, Zou F et al (2020) Poly (ADP-ribose) polymerase 1 inhibition prevents neurodegeneration and promotes alpha-synuclein degradation via transcription factor EB-dependent autophagy in mutant alpha-synucleinA53T model of Parkinson’s disease. Aging Cell 19(6):e13163. https://doi.org/10.1111/acel.13163
Zhang H, Xie Z, Peng Y, Xie A, Fu C, Zheng D, Cai Z, Zhong J et al (2023) PARP1 promotes NLRP3 activation via blocking TFEB-mediated autophagy in rotenone-induced neurodegeneration. Ecotoxicol Environ Saf 252:114630. https://doi.org/10.1016/j.ecoenv.2023.114630
Puentes LN, Lengyel-Zhand Z, Reilly SW, Mach RH (2021) Evaluation of a Low-Toxicity PARP Inhibitor as a Neuroprotective Agent for Parkinson’s Disease. Mol Neurobiol 58(8):3641–3652. https://doi.org/10.1007/s12035-021-02371-4
Olsen AL, Feany MB (2019) PARP Inhibitors and Parkinson’s Disease. N Engl J Med 380(5):492–494. https://doi.org/10.1056/NEJMcibr1814680
Verhoeven Y, Tilborghs S, Jacobs J, De Waele J, Quatannens D, Deben C, Prenen H, Pauwels P et al (2020) The potential and controversy of targeting STAT family members in cancer. Semin Cancer Biol 60:41–56. https://doi.org/10.1016/j.semcancer.2019.10.002
Xu E, Boddu R, Abdelmotilib HA, Sokratian A, Kelly K, Liu Z, Bryant N, Chandra S et al (2022) Pathological alpha-synuclein recruits LRRK2 expressing pro-inflammatory monocytes to the brain. Mol Neurodegener 17(1):7. https://doi.org/10.1186/s13024-021-00509-5
Raspaglio G, Buttarelli M, Filippetti F, Battaglia A, Buzzonetti A, Scambia G, Gallo D (2021) Stat1 confers sensitivity to radiation in cervical cancer cells by controlling Parp1 levels: a new perspective for Parp1 inhibition. Cell Death Dis 12(10):933. https://doi.org/10.1038/s41419-021-04229-y
Cherng YG, Chu YC, Yadav VK, Huang TY, Hsieh MS, Lee KF, Lee WH, Yeh CT et al (2021) Induced mitochondrial alteration and dna damage via IFNGR-JAK2-STAT1-PARP1 pathway facilitates viral hepatitis associated hepatocellular carcinoma aggressiveness and stemness. Cancers (Basel) 13(11):2755. https://doi.org/10.3390/cancers13112755
Ziouzenkova O, Plutzky J (2008) Retinoid metabolism and nuclear receptor responses: New insights into coordinated regulation of the PPAR-RXR complex. FEBS Lett 582(1):32–38. https://doi.org/10.1016/j.febslet.2007.11.081
Germain P, Chambon P, Eichele G, Evans RM, Lazar MA, Leid M, De Lera AR, Lotan R et al (2006) International Union of Pharmacology LX Retinoic acid receptors. Pharmacol Rev 58(4):712–725. https://doi.org/10.1124/pr.58.4.4
Ono K, Yamada M (2007) Vitamin A potently destabilizes preformed alpha-synuclein fibrils in vitro: implications for Lewy body diseases. Neurobiol Dis 25(2):446–454. https://doi.org/10.1016/j.nbd.2006.10.010
Carta M, Stancampiano R, Tronci E, Collu M, Usiello A, Morelli M, Fadda F (2006) Vitamin A deficiency induces motor impairments and striatal cholinergic dysfunction in rats. Neuroscience 139(4):1163–1172. https://doi.org/10.1016/j.neuroscience.2006.01.027
Kitaoka K, Hattori A, Chikahisa S, Miyamoto K, Nakaya Y, Sei H (2007) Vitamin A deficiency induces a decrease in EEG delta power during sleep in mice. Brain Res 1150:121–130. https://doi.org/10.1016/j.brainres.2007.02.077
Kunzler A, Ribeiro CT, Gasparotto J, Petiz LL, da RosaSilva HT, da Silva JD Jr, Bortolin R, de Souza PO et al (2019) The effects of retinol oral supplementation in 6-hydroxydopamine dopaminergic denervation model in Wistar rats. Neurochem Int 125:25–34. https://doi.org/10.1016/j.neuint.2019.02.002
Spathis AD, Asvos X, Ziavra D, Karampelas T, Topouzis S, Cournia Z, Qing X, Alexakos P et al (2017) Nurr1:RXRalpha heterodimer activation as monotherapy for Parkinson’s disease. Proc Natl Acad Sci U S A 114(15):3999–4004. https://doi.org/10.1073/pnas.1616874114
Samad TA, Krezel W, Chambon P, Borrelli E (1997) Regulation of dopaminergic pathways by retinoids: activation of the D2 receptor promoter by members of the retinoic acid receptor-retinoid X receptor family. Proc Natl Acad Sci U S A 94(26):14349–14354. https://doi.org/10.1073/pnas.94.26.14349
Krezel W, Ghyselinck N, Samad TA, Dupe V, Kastner P, Borrelli E, Chambon P (1998) Impaired locomotion and dopamine signaling in retinoid receptor mutant mice. Science 279(5352):863–867. https://doi.org/10.1126/science.279.5352.863
Krezel W, Kastner P, Chambon P (1999) Differential expression of retinoid receptors in the adult mouse central nervous system. Neuroscience 89(4):1291–1300. https://doi.org/10.1016/s0306-4522(98)00342-x
Chiu HJ, Fischman DA, Hammerling U (2008) Vitamin A depletion causes oxidative stress, mitochondrial dysfunction, and PARP-1-dependent energy deprivation. FASEB J 22(11):3878–3887. https://doi.org/10.1096/fj.08-112375
Cai W, Wang J, Hu M, Chen X, Lu Z, Bellanti JA, Zheng SG (2019) All trans-retinoic acid protects against acute ischemic stroke by modulating neutrophil functions through STAT1 signaling. J Neuroinflammation 16(1):175. https://doi.org/10.1186/s12974-019-1557-6
Wu J, Zheng C, Wan X, Shi M, McMillan K, Maique J, Cao C (2020) Retinoic Acid Alleviates Cisplatin-Induced Acute Kidney Injury Through Activation of Autophagy. Front Pharmacol 11:987. https://doi.org/10.3389/fphar.2020.00987
Coleman MM, Basdeo SA, Coleman AM, Cheallaigh CN, Peral de Castro C, McLaughlin AM, Dunne PJ et al (2018) All-trans Retinoic Acid Augments Autophagy during Intracellular Bacterial Infection. Am J Respir Cell Mol Biol 59(5):548–556. https://doi.org/10.1165/rcmb.2017-0382OC
Rivero-Rios P, Madero-Perez J, Fernandez B, Hilfiker S (2016) Targeting the Autophagy/Lysosomal Degradation Pathway in Parkinson’s Disease. Curr Neuropharmacol 14(3):238–249. https://doi.org/10.2174/1570159x13666151030103027
Arotcarena ML, Teil M, Dehay B (2019) Autophagy in synucleinopathy: the overwhelmed and defective machinery. Cells 8(6):565. https://doi.org/10.3390/cells8060565
Park H, Kam TI, Dawson TM, Dawson VL (2020) Poly (ADP-ribose) (PAR)-dependent cell death in neurodegenerative diseases. Int Rev Cell Mol Biol 353:1–29. https://doi.org/10.1016/bs.ircmb.2019.12.009
Tang D, Kang R, Berghe TV, Vandenabeele P, Kroemer G (2019) The molecular machinery of regulated cell death. Cell Res 29(5):347–364. https://doi.org/10.1038/s41422-019-0164-5
Makvandi M, Pantel A, Schwartz L, Schubert E, Xu K, Hsieh CJ, Hou C, Kim H et al (2018) A PET imaging agent for evaluating PARP-1 expression in ovarian cancer. J Clin Invest 128(5):2116–2126. https://doi.org/10.1172/JCI97992
Karpova Y, Wu C, Divan A, McDonnell ME, Hewlett E, Makhov P, Gordon J et al (2019) Non-NAD-like PARP-1 inhibitors in prostate cancer treatment. Biochem Pharmacol 167:149–162. https://doi.org/10.1016/j.bcp.2019.03.021
Zhu H, Wei M, Xu J, Hua J, Liang C, Meng Q, Zhang Y, Liu J et al (2020) PARP inhibitors in pancreatic cancer: molecular mechanisms and clinical applications. Mol Cancer 19(1):49. https://doi.org/10.1186/s12943-020-01167-9
Jain PG, Patel BD (2019) Medicinal chemistry approaches of poly ADP-Ribose polymerase 1 (PARP1) inhibitors as anticancer agents - A recent update. Eur J Med Chem 165:198–215. https://doi.org/10.1016/j.ejmech.2019.01.024
Awasthi N, Liongue C, Ward AC (2021) STAT proteins: a kaleidoscope of canonical and non-canonical functions in immunity and cancer. J Hematol Oncol 14(1):198. https://doi.org/10.1186/s13045-021-01214-y
Shibata M, Pattabiraman K, Lorente-Galdos B, Andrijevic D, Kim SK, Kaur N, Muchnik SK, Xing X et al (2021) Regulation of prefrontal patterning and connectivity by retinoic acid. Nature 598(7881):483–488. https://doi.org/10.1038/s41586-021-03953-x
Bang YJ, Hu Z, Li Y, Gattu S, Ruhn KA, Raj P, Herz J, Hooper LV (2021) Serum amyloid A delivers retinol to intestinal myeloid cells to promote adaptive immunity. Science 373(6561):eabf9232. https://doi.org/10.1126/science.abf9232
Dai L, Wang J, He M, Xiong M, Tian Y, Liu C, Zhang Z (2021) Lovastatin Alleviates alpha-Synuclein Aggregation and Phosphorylation in Cellular Models of Synucleinopathy. Front Mol Neurosci 14:682320. https://doi.org/10.3389/fnmol.2021.682320
Acknowledgements
This study is supported by the Natural Science Foundation of Hubei Province (2020CFB737) and the Medical Science and Technology Development Program of Shandong Province (No. 202003081484).
Funding
This work was supported by the Natural Science Foundation of Hubei Province (No. 2020CFB737) to Xiang Gao, and the Medical and Health Development Project of Shandong Province (No. 202003081484) to Zengxia Ma.
Author information
Authors and Affiliations
Contributions
G.X. and M.Z. provided funding and supervision and reviewed and edited the manuscript. Z.L. designed and performed experiments, analyzed the data, and wrote the manuscript. All authors have read and approved the submitted version.
Corresponding authors
Ethics declarations
Ethics Approval
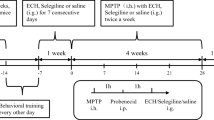
The Declaration of Helsinki and guidelines of Renmin Hospital, Wuhan University. was strictly followed during animal maintenance and experiments. The Animal Care and Use Committee of Renmin Hospital of Wuhan University reviewed and approved the protocol (20211104).
Consent to Participate
Not applicable.
Consent to Publish
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, L., Ma, Z. & Gao, X. Retinoic Acid Prevents α-Synuclein Preformed Fibrils-Induced Toxicity via Inhibiting STAT1-PARP1 Signaling. Mol Neurobiol 60, 4828–4841 (2023). https://doi.org/10.1007/s12035-023-03376-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-023-03376-x