Abstract
Various lymphocyte subpopulations, including NK cells as well as γδ T cells, have been considered an important element in the pathogenesis of autoimmune, inflammatory, rheumatic diseases, such as rheumatoid arthritis (RA) and ankylosing spondylitis (AS). The aim of this study was to assess the potential role of polymorphic variations in the genes coding for three NK and γδ T cell receptors: NCR3, FCγR3A, and DNAM-1 (rs1052248, rs396991, and rs763361, respectively) in the disease susceptibility and the efficacy of treatment with TNF inhibitors. The study included 461 patients with RA, 168 patients with AS, and 235 voluntary blood donors as controls. The NCR3 rs1052248 AA homozygosity prevailed in RA in patients lacking rheumatoid factor (p = 0.044) as well as in those who manifested the disease at a younger age (p = 0.005) and had higher CRP levels after 12 weeks of anti-TNF therapy (p = 0.021). The FCγR3A rs396991 polymorphism was associated with pain visual analogue scale (VAS) values before the initiation of anti-TNF treatment. Lower VAS values were observed in the GG homozygous RA patients (p = 0.024) and in AS patients with the TT genotype (p = 0.012). Moreover, AS heterozygous patients with the TG genotype presented higher CRP levels in the 12th week of anti-TNF treatment (p = 0.021). The findings suggest that the NCR3 rs1052248 AA homozygosity may have an adverse effect on RA, while the T allele potentially plays a protective role in the development of AS. Moreover, the rs1052248 T allele and TT genotype appear to have a favorable impact on the response to anti-TNF therapy in RA patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) and ankylosing spondylitis (AS) belong to the commonly diagnosed autoimmune rheumatic diseases. It is estimated that rheumatic diseases affect about 0.9–1.5% of the world’s population [1]. Their perpetuation or implemented treatment can contribute to the development of comorbidities such as cardiovascular disease, cancer, lung disease, gastrointestinal ulcers, and various infections, and even lead to premature death [2,3,4,5,6,7,8,9,10,11,12].
The development of RA and AS is influenced by various risk factors, including environmental factors, lifestyle choices, history of infectious diseases, and socio-economic dimensions. Geo-epidemiological differences are also apparent, which may suggest the importance of factors related to patient ethnicity [13] and associated genetic variation.
One of the well-known and extensively studied genetic factors in RA is the so-called shared epitope (SE) which is a four-amino acid sequence (70–74 position) in the human leukocyte antigen (HLA)-DRB1 molecule. The presence of the shared epitope has a significant impact on the development and severity of RA [14] due to its potential role in CD4 + T lymphocyte activation. Simultaneously, HLA-B27 has been implicated in AS susceptibility. HLA-B27 belongs to HLA class I molecules and its main role is the presentation of antigens to CD8 + T lymphocytes leading to their activation. One of the widely accepted theories of HLA-B27’s role in the pathogenesis of AS is that HLA-B27 presents external bacterial antigens that resemble human antigens. As a result, CD8 + lymphocytes may be activated by self-antigens and propagate inflammation [15]. Both types of HLA molecules interact with αβ T cell receptors (TCR).
γδ T lymphocytes and natural killer (NK) cells have been implicated in the pathogenesis of rheumatic diseases, alongside T helper (CD4 +) and cytotoxic (CD8 +) cells [1, 16,17,18,19]. The role of γδ T cells in rheumatic diseases remains unclear and requires further exploration, although some reports suggest that they play a key role in disease pathogenesis. For instance, patients with RA have shown elevated levels of γδ T cells in synovial fluid compared to healthy individuals [20]. Furthermore, γδ T cells are known to produce interleukin (IL)-17, a cytokine involved in the pathogenesis of inflammatory diseases [16].
On the other hand, the role of NK cells in the development of rheumatic diseases has already been quite well described [18, 19]. It is known that the beneficial or detrimental effect of NK cell activity results from the balance of inhibitory and activating receptors on the surface of these cells.
Among a wide repertoire of surface receptors, there are three which have the ability to stimulate both γδ T cells as well as NK cells, namely NCR3, FCγ3R, and DNAM-1. These receptors are involved in the synergistic pathway of NK cell activation [21, 22].
The natural cytotoxicity triggering receptor 3 (NCR3) belongs to the immunoglobulin superfamily (IgSF) and is also referred to as a cluster of differentiation 337 (CD337) or natural killer protein 30 (NKp30) [23]. The gene for NCR3 is located on the human chromosome 6. Rusakiewicz et al. showed that NCR3 is a very important element in the mechanism of action of interferon-gamma (IFNγ), which has been identified as an important element in the pathogenesis of some autoimmune diseases, including RA [24,25,26]. In RA patients, increased levels of NCR3 were detected in the synovium, which was associated with more severe inflammation within the joints [26].
The A form of the FCγ3R receptor (encoded by FCγR3A) is one of the six-member human FCRs family, each with varying affinities for IgG immunoglobulins. FCγ3R is considered a low-affinity receptor [27] and is encoded by two genes FCγR3A and FCγR3B located on chromosome 1q23 sequentially along with other low-affinity FCR molecules. The FCR family has recently attracted considerable research interest due to their involvement in the development of various autoimmune and inflammatory diseases [28,29,30]. However, the exact role of FCRs in the development of rheumatic diseases has not been exhaustively described to date. FCRs are mostly produced by monocytes, macrophages, neutrophils, and NK cells involved in cytotoxicity, phagocytosis, and mediating pro-inflammatory molecule production [31, 32]. These receptors are also expressed on the surface of osteoclasts, which may suggest a role in the erosion of bone and cartilage structures within affected joints [33, 34]. One of the more recent studies discussing the mouse equivalent of FCγ3RA indicates its function in inducing the production of S100A8/S100A9 inflammation-mediating molecules that have been detected in the synovial fluid of arthritic joints [33]. They are mainly produced by neutrophils in whose activation FCγR3A is involved [35].
The DNAX accessory molecule-1 (DNAM-1), known also as Cluster of Differentiation 226 (CD226), is an activating receptor that is primarily involved in NK cell–dependent antitumor reaction and is also a very important element in the antiviral immune response [36,37,38,39]. It has been reported that the interaction between DNAM-1 and its ligand CD155 (also often described as poliovirus receptor, PVR, or Nectin-like molecule-5, Necl5) supports the polarization of T cells towards the Th1 subpopulation and the development of inflammation. On the other hand, the action of DNAM-1 results in inhibiting the JAK-STAT pathway by preventing phosphorylation, which reduces the Th2 lymphocyte response [40]. In addition, stimulated DNAM-1 can cooperate with the NCR3 receptor. Together, they enable communication between NK cells and dendritic cells and are involved in the proliferation of mature dendritic cells [41]. Moreover, previous studies have linked DNAM-1 with predispositions to rheumatic diseases, including RA [42,43,44].
The aim of our present study was to investigate the role of polymorphic variants within the genes encoding NCR3, FCγR3A, and DNAM-1 receptors in the development of inflammatory rheumatic diseases and the outcome of biological treatment with tumor necrosis factor (TNF) inhibitors. For this purpose, RA and AS patients and unrelated healthy controls were genotyped for two non-synonymous single nucleotide polymorphisms (SNPs): (I) a T to G substitution (rs396991) within the FCγR3A gene resulting in phenylalanine (Phe) to valine (Val) amino acid exchange in position 158 (Phe158Val), and (II) a C to T substitution (rs763361) within the DNAM-1 gene resulting with glycine (Gly) to serine (Ser) amino acid exchange in position 307 (Gly307Ser), as well as (III) a T to A substitution (rs1052248) in the 3′ UTR of the NCR3 gene. To our knowledge, the role of these SNPs has not been previously investigated in Polish patients with RA and AS.
Materials and methods
Patients and controls — inclusion and exclusion criteria
A total of 461 RA patients and 168 AS patients were investigated. The basic condition for qualifying rheumatic patients for the study was high disease activity at the time of classification, non-response for treatment with the use of at least two conventional synthetic disease-modifying anti-rheumatic drugs (csDMARDs) for RA or non-steroidal anti-inflammatory drugs (NSAIDs) for AS patients. As a result, those patients were enrolled in the treatment program with TNF inhibitors. RA and AS activity was determined based on the American College of Rheumatology (ACR)/European League Against Rheumatism (EULAR) from 2010 and 1984 modified New York Criteria, respectively [45, 46]. Biological material was obtained in cooperation with the Department of Rheumatology and Internal Medicine, University Clinical Hospital in Wroclaw, Poland, and the Department of Rheumatology and Connective Tissue, Jan Biziel University Hospital No. 2 in Bydgoszcz, Poland.
All participants had to be over 18 years old, of Polish ethnicity, and lack other autoimmune and cancer diseases in their medical review. Moreover, they should be willing to cooperate. Failure to meet any of the above criteria resulted in the exclusion of the patient from the study group.
The control group consisted of 235 healthy voluntary blood donors. These individuals were over the age of 18 and belonged to the Polish ethnic group. The controls were not related to each other and had no medical history of immunological or hematologic diseases. All participants were of Caucasian ancestry. The study protocol was approved by the Wroclaw Medical University Ethics Committee.
Selection of therapy and assessment of treatment effectiveness
Classified RA and AS patients were treated with one of the approved biological drugs that inhibit the effects of TNF. The dosage administered was determined by the doctor in accordance with the recommended guidelines for the respective medication. Additionally, methotrexate (MTX) was utilized as the primary first-line therapy for RA, and NSAIDs for AS were permitted for use.
Demographic data, including gender, age, and BMI, were collected from the patients. Clinical data such as C-reactive protein (CRP), rheumatoid factor (RF), and anti-cyclic citrullinated peptide (anti-CCP) antibodies (for RA patients) levels, as well as HLA-B27 status (for AS patients), were obtained through medical examinations prior to the initiation of TNF inhibitor therapy. Disease activity was assessed using the Disease Activity Score 28 (DAS28) for RA patients and the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) for AS patients. Additionally, patients self-reported their level of pain on a visual analogue scale (VAS). Subsequent medical examinations took place at 12 and 24 weeks after the initiation of TNF inhibitor therapy. During these medical appointments, additional clinical data were collected, and anti-TNF treatment effectiveness was assessed based on EULAR response criteria.
The condition of the patients was characterized by collecting and analyzing the parameters given in Table 1.
Polymorphisms selection
The FCγR3A rs396991 polymorphism is located on the 1st human chromosome in the low-affinity IIIA Fc fragment. It is a substitution from T to G which leads to changing phenylalanine (F) to valine (V) and is described also as T > G, Phe158Val, F176V, or F158V. This change probably leads to functional modifications related to the affinity of the FCγR3A receptor for IgG [47]. Literature data have shown the relationship of this polymorphism with autoimmune diseases and their treatment [48,49,50,51,52,53].
The NCR3 rs1052248 substitution is found on the 6th chromosome in the 3′ UTR gene sequence. The difference in variants is the change from T to A. This polymorphism has been quite poorly examined in the context of rheumatic diseases, but the changing level of NCR3 protein during joint inflammation has been reported [26].
DNAM-1 rs763361 is also described as Gly307Ser (C/T) in the CD226 gene located on the 18th chromosome in humans. Its relationship to rheumatic diseases has been pointed out in several papers, mainly in multiple sclerosis, rheumatoid arthritis, and systemic lupus as well [54,55,56,57]. Moreover, this polymorphism is likely involved in cellular signaling through the TCR pathway and activation of naïve T lymphocytes for proliferation and differentiation [58].
Genotyping of receptor genes
Peripheral blood samples were collected on EDTA from RA and AS patients as well as from voluntary blood donors. DNA was isolated from the peripheral blood using the column isolation method (QIAamp DNA Blood Midi/Maxi Kit, Qiagen, Germany). The DNA samples were further subjected to analysis of three SNPs: FCγR3A rs396991 (T > G; Phe158Val); DNAM-1 rs763361 (C > T; Gly307Ser); and NCR3 rs1052248 (A > T). All selected polymorphisms were characterized with minor allele frequency (MAF) > 0.05, and are non-synonymous or are located within regulatory regions. Genotyping was performed with the use of commercial LightSNP kits employing real-time PCR (TIB MOLBIOL, Germany). Amplifications were carried out on the Real-Time PCR Instrument 480 (Roche Diagnostics, Switzerland).
Statistical analysis
All non-normally distributed continuous data were subjected to analysis using the Mann–Whitney U-test. For data with a normal distribution, the parametric Student T-test with Welch’s correction for unpaired features was employed. Quantitative data were evaluated using Fisher’s test. Distribution was assessed using the Shapiro–Wilk test.
Statistical calculations and analyses were performed using GraphPad Prism 8.0.1 software, with results deemed statistically significant if the p-value was below 0.05.
Results
Genotype and allele distributions of investigated polymorphisms in RA and AS patients and control cohort
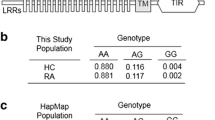
The distribution of alleles and genotypes for all selected polymorphisms was tested to check if they are in Hardy–Weinberg equilibrium (HWE). All groups satisfied the conditions of Hardy–Weinberg equilibrium.
Similarly, no significant difference was observed between both groups of the RA and AS patients and the controls concerning the DNAM-1 rs763361 polymorphism.
However, an interesting difference was observed in the distribution of particular alleles/genotypes of the NCR3 rs1052248 polymorphism between the group of patients suffering from AS and the control cohort. The TT genotype has not been identified among AS patients, whereas it occurred in healthy individuals with a frequency of approximately 10% (p < 0.0001; OR = 0.028, Table 2) suggesting a potential protective effect of this homozygous genotype against AS susceptibility. This relationship was not observed for RA patients.
Association of NCR3 rs1052248 polymorphism with clinical parameters in RA and AS patients
Statistical analysis of results obtained from genotyping rs1052248 polymorphisms for the NCR3 gene in relation to RA patients’ clinical parameters showed some significant relationships (Fig. 1).
The onset of RA was observed to be earlier in patients with the NCR3 rs1052248 AA genotype than in carriers of the T allele (p = 0.005). Furthermore, the age of RA development was found to be affected by the presence of both AA and TT homozygous genotypes compared to AT heterozygosity, with AA and TT homozygous patients having onset at a younger age (p = 0.026) (Fig. 1A and B).
Moreover, AA homozygosity of the rs1052248 SNP was found to be associated with higher C-reactive protein (CRP) levels after 12 weeks of anti-TNF therapy (p = 0.021), while patients with the heterozygous AT genotype exhibited significantly lower blood CRP levels than homozygotes (p = 0.040) (Fig. 1C and D).
Additionally, the AA genotype was more frequently observed among RF-negative patients compared to patients with the TT/AT genotypes (p = 0.044, Fig. 1E).
No significant relationship was detected between the NCR3 genetic variants and clinical parameters in patients with AS.
Relationship between FCγR3A rs396991 polymorphism and VAS scale in RA and AS patients
No association was observed between the FCyR3A rs396991 polymorphism and the risk of developing either RA or AS. However, some relationship was noted for this polymorphism concerning the VAS values before the initiation of anti-TNF therapy in both studied diseases. In the RA group, lower VAS values were observed in the GG homozygous patients than in those with other genotypes before starting anti-TNF therapy (p = 0.024, Fig. 2A). In the AS group, patients with the G allele marked higher pain values on the VAS scale than TT genotype carriers (p = 0.012, Fig. 2B). Moreover, among the group AS patients, the presence of heterozygous TG genotype was associated with higher CRP level than at the 12th week from the start of anti-TNF treatment as compared to patients carrying either TT or GG FCγR3A rs396991 homozygous genotype (p = 0.021, Fig. 2C).
Associations between FCγR3A rs396991 variants and clinical parameters in RA and AS patients. Significant relationships between FCγR3A polymorphism and VAS values before initiation of anti-TNF treatment in RA (A) and AS patients (B), as well as CRP levels after 12 weeks of the anti-TNF treatment in patients with AS (C)
Similarly to the NCR3 rs1052248 and FCγR3A rs396991 polymorphism, the presence of the DNAM-1 rs763361 genetic variant was tested for various clinical parameters in patients suffering from RA and AS. However, no significant relationships were observed.
Discussion
The current state of knowledge highlights the significant role of NK cells and γδ lymphocytes in the pathogenesis and progression of rheumatic diseases [1, 18]. Intriguingly, these two cell types constitute an innate lymphoid population capable of producing inflammatory mediators and exerting cytotoxic activity. Furthermore, NK and γδ cells share surface receptors and transcription factors [59]. Therefore, we embarked on a study to investigate the impact of polymorphic variants in NCR3, FCγR3A, and DNAM-1 genes, which are common to NK and γδ cells. Our objective was to explore their association with the development, progression, and response to TNF inhibitor treatment in patients diagnosed with rheumatoid arthritis and ankylosing spondylitis.
Our key findings concern the rs1052248 polymorphism of the NRC3 receptor gene that was found to play a significant role in both groups of patients we examined. As mentioned earlier, it can be inferred from our study that the presence of the T allele seems to act as a protective factor of disease development, as observed for AS and RF-negative RA. This genetic variant was also less frequent among patients who developed RA at a younger age. Importantly, a more favorable impact of the rs1052248 T allele was also seen in RA patients concerning the anti-TNF treatment outcome, additionally confirming its beneficial effect. Notably, the rs1052248 polymorphism has been described for both the NCR3 and LTS1 genes, which are located close to each other and partially overlap, albeit they are transcribed in opposite directions on the complementary strands. These genes are situated within the MHC class III region, specifically in the Ltab-Ncr3 conserved haplotype, which has a significant association with arthritis pathogenesis and progression [60, 61]. Studies conducted on a rat model have demonstrated that increased NCR3 expression and decreased LST1 expression contribute to reducing the severity of RA. Similar results were obtained by the researchers when examining a group of 32 patients with RA [61].
The rs1052248 polymorphism within LST1/NCR3 was also investigated in an intriguing study conducted by Wu et al. focusing on genome-wide interaction analysis in psoriasis, which is also an autoimmune disorder. While the primary aim of their work was to introduce a novel approach to the analysis of locus interactions, the findings presented demonstrate that the rs1052248 polymorphism in LST1/NCR3 interacts with other polymorphisms, including the rs3131636 and rs3132468 single nucleotide substitutions in the MICB gene. Furthermore, the rs1052248 polymorphic site serves as a binding site for microRNA miR-324-3p [62]. It is noteworthy that different types of MIC family genes and miR-324 molecules have been linked in the literature to arthritis [63,64,65,66].
According to the literature data, the rs1052248 polymorphism of the NCR3 gene has been very poorly investigated to date and there are no publications enabling us to compare the results of our present study with other cohorts of patients suffering from RA, AS, or other autoimmune diseases. In one of the published studies concerning the rs1052248 polymorphism, the authors examined its association with susceptibility to malaria in malaria-risk regions; however, no significant relationship was observed [67].
Nevertheless, numerous studies have shed light on the significant involvement of NCR3 in the progression of autoimmune conditions and the cytotoxic capabilities of cells [24, 68], undoubtedly contributing to the pathogenesis of RA and AS. Furthermore, the impact of the NCR3 protein has been observed in various other diseases, such as Sjögren’s syndrome and cancer-related disorders [24, 69].
In our present study, we also genotyped our RA and AS patients for the FCγR3A rs396991 polymorphism. The FCγR family of molecules has been associated with the pathogenesis of rheumatic diseases in many different studies [30, 70]. The primary role of FCγR molecules in the disease process is to recognize immune complexes and stimulate cells to produce inflammatory mediators in arthritic joints, which can further lead to the development of pain. Interestingly, our analyses showed some associations between the rs396991 polymorphism in the gene encoding the FCγR3A receptor and VAS scores in both groups of patients investigated, although their results are not consistent when comparing RA and AS patients. One study reported results quite similar to our own. Its authors pointed out that the presence of FCγR3A rs396991 A allele, as well as lower VAS values on the baseline, is in relation to better response to treatment by abatacept in RA patients. However, it is important to note that the VAS pain scale score is based on a subjective assessment determined by the patient [71]. Moreover, the results regarding the rs396991 FCγR3A polymorphism should be considered preliminary in nature as they are based on a small patient group. Nevertheless, these findings may provide insight into potential associations between genotype and clinical parameters in patients, particularly in the AS subgroup. It would be interesting to repeat this study on a larger patient cohort.
Furthermore, as in our study, the existing literature provides divergent perspectives on the identification of a beneficial variant of the rs396991 polymorphism in FCγR3A [50].
A meta-analysis conducted by Lee et al. demonstrated an association between the presence of the GG genotype and the occurrence of RA among Europeans but not Asians [72]. Several studies have examined the relationship between the polymorphism in the FCγR3A gene and the response to treatment with TNF inhibitors. It has been suggested that individuals with the homozygous dominant TT genotype have slower drug metabolism, leading to therapeutic benefits [73]. Similar findings were reported by Tutuncu et al. in a mixed American population [74] and Márquez Pete et al. in a Spanish population [71]. On the other hand, no association between treatment response and the specific polymorphic variant was found in either Swedish individuals [75] or in the Dutch population [76]. However, in our AS patients, the FCγR3A rs396991 heterozygosity seems to have an unfavorable impact on anti-TNF treatment with no effect of the FCγR3A rs396991 SNP in the RA patient group. In Spanish patients with AS, the G allele was reported to be associated with a better response to anti-TNF treatment. In the same study, Morales-Lara et al. also examined patients with RA and PsA, but the results did not align with those for AS, leading the authors to conclude that the drug’s impact may vary among different types of arthritic diseases, which we agree with [77].
The results of the third SNP studied, rs763361 polymorphism in the DNAM-1 gene, did not show any significant association in either RA or AS patients of Polish origin. Nevertheless, in many other populations, this polymorphism has also not been unequivocally identified as a diagnostic or clinically significant factor, both in the diseases we investigated (RA and AS) and other autoimmune disorders [78,79,80]. One study involving an Iranian population suggests a possible negative association of the T allele, which increases the risk of developing RA [81], and meta-analyses encompassing diverse populations indicate some probability of autoimmune disease prediction, including for RA, using the rs763361 polymorphism in the DNAM-1 gene [82, 83]. Furthermore, the study by Tan et al. indicates an association between the rs763361 polymorphism of DNAM-1 and the response to TNF inhibitor treatment in RA [56]. However, our findings do not confirm this association.
Conclusion
In summary, our results represent the first research study investigating the significance of the rs1052248 NCR3, rs396991 FCγR3A, and rs763361 DNAM-1 polymorphisms in the pathogenesis, progression, and response to therapy with TNF inhibitors in Polish patients with rheumatoid arthritis and ankylosing spondylitis. To the best of our knowledge, the most promising results of our current study regarding the NCR3 gene polymorphism provide new insights not only in the context of the Polish population but also as the only published results of their kind. We believe that all the polymorphisms we investigated are worth further attention and analysis, with a special focus on the rs1052248 NCR3 polymorphism, which has the potential to become a prognostic factor for the more severe RA, as well as a predictor for AS, as observed in our Polish population.
Data Availability
The data supporting the findings of this study are available within the article and available from the corresponding author on request.
References
Bank I. The role of gamma delta T cells in autoimmune rheumatic diseases. Cells. 2020;9(2):462. https://doi.org/10.3390/cells9020462.
Maradit-Kremers H, Nicola PJ, Crowson CS, Ballman KV, Gabriel SE. Cardiovascular death in rheumatoid arthritis: a population-based study. Arthritis Rheum. 2005;52(3):722–32. https://doi.org/10.1002/art.20878.
Maradit-Kremers H, Crowson CS, Nicola PJ, et al. Increased unrecognized coronary heart disease and sudden deaths in rheumatoid arthritis: a population-based cohort study. Arthritis Rheum. 2005;52(2):402–11. https://doi.org/10.1002/art.20853.
Baecklund E, Iliadou A, Askling J, et al. Association of chronic inflammation, not its treatment, with increased lymphoma risk in rheumatoid arthritis. Arthritis Rheum. 2006;54(3):692–701. https://doi.org/10.1002/art.21675.
Simon TA, Thompson A, Gandhi KK, Hochberg MC, Suissa S. Incidence of malignancy in adult patients with rheumatoid arthritis: a meta-analysis [published correction appears in Arthritis Res Ther. 2016;18(1):100]. Arthritis Res Ther. 2015;17(1):212. https://doi.org/10.1186/s13075-015-0728-9.
Wolfe F, Caplan L, Michaud K. Rheumatoid arthritis treatment and the risk of severe interstitial lung disease. Scand J Rheumatol. 2007;36(3):172–8. https://doi.org/10.1080/03009740601153774.
Fewins HE, McGowan I, Whitehouse GH, Williams J, Mallya R. High definition computed tomography in rheumatoid arthritis associated pulmonary disease. Br J Rheumatol. 1991;30(3):214–6. https://doi.org/10.1093/rheumatology/30.3.214.
Garcia Rodríguez LA, Hernández-Díaz S. The risk of upper gastrointestinal complications associated with nonsteroidal anti-inflammatory drugs, glucocorticoids, acetaminophen, and combinations of these agents. Arthritis Res. 2001;3(2):98–101. https://doi.org/10.1186/ar146.
Simon LS, Weaver AL, Graham DY, et al. Anti-inflammatory and upper gastrointestinal effects of celecoxib in rheumatoid arthritis: a randomized controlled trial. JAMA. 1999;282(20):1921–8. https://doi.org/10.1001/jama.282.20.1921.
Doran MF, Crowson CS, Pond GR, O’Fallon WM, Gabriel SE. Frequency of infection in patients with rheumatoid arthritis compared with controls: a population-based study. Arthritis Rheum. 2002;46(9):2287–93. https://doi.org/10.1002/art.10524.
Schneeweiss S, Setoguchi S, Weinblatt ME, et al. Anti-tumor necrosis factor alpha therapy and the risk of serious bacterial infections in elderly patients with rheumatoid arthritis. Arthritis Rheum. 2007;56(6):1754–64. https://doi.org/10.1002/art.22600.
Gabriel SE, Michaud K. Epidemiological studies in incidence, prevalence, mortality, and comorbidity of the rheumatic diseases. Arthritis Res Ther. 2009;11(3):229. https://doi.org/10.1186/ar2669.
Abdel-Kader Martín N, Cardiel MH. Geographical factors in rheumatoid arthritis. Int J Clin Rheumatol. 2011;6(3):259–61.
Del Rincón I, Battafarano DF, Arroyo RA, Murphy FT, Fischbach M, Escalante A. Ethnic variation in the clinical manifestations of rheumatoid arthritis: role of HLA-DRB1 alleles. Arthritis Rheum. 2003;49(2):200–8. https://doi.org/10.1002/art.11000.
Garrido-Mesa J, Brown MA. T cell repertoire profiling and the mechanism by which HLA-B27 causes ankylosing spondylitis. Curr Rheumatol Rep. 2022;24(12):398–410. https://doi.org/10.1007/s11926-022-01090-6.
Gaur P, Misra R, Aggarwal A. Natural killer cell and gamma delta T cell alterations in enthesitis related arthritis category of juvenile idiopathic arthritis. Clin Immunol. 2015;161(2):163–9. https://doi.org/10.1016/j.clim.2015.07.012.
Nguyen CT, Maverakis E, Eberl M, Adamopoulos IE. γδ T cells in rheumatic diseases: from fundamental mechanisms to autoimmunity. Semin Immunopathol. 2019;41(5):595–605. https://doi.org/10.1007/s00281-019-00752-5.
Hojjatipour T, Aslani S, Salimifard S, et al. NK cells - Dr. Jekyll and Mr. Hyde in autoimmune rheumatic diseases. Int Immunopharmacol. 2022;107:108682. https://doi.org/10.1016/j.intimp.2022.108682.
Shegarfi H, Naddafi F, Mirshafiey A. Natural killer cells and their role in rheumatoid arthritis: friend or foe? ScientificWorldJournal. 2012;2012:491974. https://doi.org/10.1100/2012/491974.
Liu MF, Yang CY, Chao SC, Li JS, Weng TH, Lei HY. Distribution of double-negative (CD4- CD8-, DN) T subsets in blood and synovial fluid from patients with rheumatoid arthritis. Clin Rheumatol. 1999;18(3):227–31. https://doi.org/10.1007/s100670050089.
MacFarlane AW 4th, Campbell KS. Signal transduction in natural killer cells. Curr Top Microbiol Immunol. 2006;298:23–57. https://doi.org/10.1007/3-540-27743-9_2.
Pazina T, Shemesh A, Brusilovsky M, Porgador A, Campbell KS. Regulation of the functions of natural cytotoxicity receptors by interactions with diverse ligands and alterations in splice variant expression. Front Immunol. 2017;8:369. https://doi.org/10.3389/fimmu.2017.00369.
Kruse PH, Matta J, Ugolini S, Vivier E. Natural cytotoxicity receptors and their ligands. Immunol Cell Biol. 2014;92(3):221–9. https://doi.org/10.1038/icb.2013.98.
Rusakiewicz S, Nocturne G, Lazure T, et al. NCR3/NKp30 contributes to pathogenesis in primary Sjogren’s syndrome. Sci Transl Med. 2013;5(195):195–6. https://doi.org/10.1126/scitranslmed.3005727.
Villanueva J, Lee S, Giannini EH, et al. Natural killer cell dysfunction is a distinguishing feature of systemic onset juvenile rheumatoid arthritis and macrophage activation syndrome. Arthritis Res Ther. 2005;7(1):R30-37. https://doi.org/10.1186/ar1453.
Mulcahy H, O’Rourke KP, Adams C, Molloy MG, O’Gara F. LST1 and NCR3 expression in autoimmune inflammation and in response to IFN-gamma LPS and microbial infection. Immunogenetics. 2006;57(12):893–903. https://doi.org/10.1007/s00251-005-0057-2.
Nimmerjahn F, Ravetch JV. Fcgamma receptors: old friends and new family members. Immunity. 2006;24(1):19–28. https://doi.org/10.1016/j.immuni.2005.11.010.
Gillis C, Gouel-Chéron A, Jönsson F, Bruhns P. Contribution of human FcγRs to disease with evidence from human polymorphisms and transgenic animal studies. Front Immunol. 2014;5:254. https://doi.org/10.3389/fimmu.2014.00254.
Li X, Gibson AW, Kimberly RP. Human FcR polymorphism and disease. Curr Top Microbiol Immunol. 2014;382:275–302. https://doi.org/10.1007/978-3-319-07911-0_13.
Ben Mkaddem S, Benhamou M, Monteiro RC. Understanding Fc receptor involvement in inflammatory diseases: from mechanisms to new therapeutic tools. Front Immunol. 2019;10:811. https://doi.org/10.3389/fimmu.2019.00811.
Sandor M, Lynch RG. The biology and pathology of Fc receptors. J Clin Immunol. 1993;13(4):237–46. https://doi.org/10.1007/BF00919382.
Wijngaarden S, van de Winkel JG, Jacobs KM, Bijlsma JW, Lafeber FP, van Roon JA. A shift in the balance of inhibitory and activating Fcgamma receptors on monocytes toward the inhibitory Fcgamma receptor IIb is associated with prevention of monocyte activation in rheumatoid arthritis. Arthritis Rheum. 2004;50(12):3878–87. https://doi.org/10.1002/art.20672.
Di Ceglie I, Ascone G, Cremers NAJ, et al. Fcγ receptor-mediated influx of S100A8/A9-producing neutrophils as inducer of bone erosion during antigen-induced arthritis. Arthritis Res Ther. 2018;20(1):80. https://doi.org/10.1186/s13075-018-1584-1.
Zuo Y, Deng GM. Fc Gamma receptors as regulators of bone destruction in inflammatory arthritis. Front Immunol. 2021;12:688201. https://doi.org/10.3389/fimmu.2021.688201.
Nacken W, Roth J, Sorg C, Kerkhoff C. S100A9/S100A8: myeloid representatives of the S100 protein family as prominent players in innate immunity. Microsc Res Tech. 2003;60(6):569–80. https://doi.org/10.1002/jemt.10299.
Fuchs A, Colonna M. The role of NK cell recognition of nectin and nectin-like proteins in tumor immunosurveillance. Semin Cancer Biol. 2006;16(5):359–66. https://doi.org/10.1016/j.semcancer.2006.07.002.
Welch MJ, Teijaro JR, Lewicki HA, Colonna M, Oldstone MB. CD8 T cell defect of TNF-α and IL-2 in DNAM-1 deficient mice delays clearance in vivo of a persistent virus infection. Virology. 2012;429(2):163–70. https://doi.org/10.1016/j.virol.2012.04.006.
Nabekura T, Kanaya M, Shibuya A, Fu G, Gascoigne NR, Lanier LL. Costimulatory molecule DNAM-1 is essential for optimal differentiation of memory natural killer cells during mouse cytomegalovirus infection. Immunity. 2014;40(2):225–34. https://doi.org/10.1016/j.immuni.2013.12.011.
de Andrade LF, Smyth MJ, Martinet L. DNAM-1 control of natural killer cells functions through nectin and nectin-like proteins. Immunol Cell Biol. 2014;92(3):237–44. https://doi.org/10.1038/icb.2013.95.
Lozano E, Joller N, Cao Y, Kuchroo VK, Hafler DA. The CD226/CD155 interaction regulates the proinflammatory (Th1/Th17)/anti-inflammatory (Th2) balance in humans. J Immunol. 2013;191(7):3673–80. https://doi.org/10.4049/jimmunol.1300945.
Balsamo M, Zambello R, Teramo A, et al. Analysis of NK cell/DC interaction in NK-type lymphoproliferative disease of granular lymphocytes (LDGL): role of DNAM-1 and NKp30. Exp Hematol. 2009;37(10):1167–75. https://doi.org/10.1016/j.exphem.2009.06.010.
Elhai M, Chiocchia G, Marchiol C, et al. Targeting CD226/DNAX accessory molecule-1 (DNAM-1) in collagen-induced arthritis mouse models. J Inflamm (Lond). 2015;12:9. https://doi.org/10.1186/s12950-015-0056-5.
Du Y, Tian L, Shen LX, et al. Association of the CD226 single nucleotide polymorphism with systemic lupus erythematosus in the Chinese Han population. Tissue Antigens. 2011;77(1):65–7. https://doi.org/10.1111/j.1399-0039.2010.01568.x.
Avouac J, Elhai M, Tomcik M, et al. Critical role of the adhesion receptor DNAX accessory molecule-1 (DNAM-1) in the development of inflammation-driven dermal fibrosis in a mouse model of systemic sclerosis. Ann Rheum Dis. 2013;72(6):1089–98. https://doi.org/10.1136/annrheumdis-2012-201759.
Aletaha D, Neogi T, Silman AJ, et al. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010;62(9):2569–81. https://doi.org/10.1002/art.27584.
van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 1984;27(4):361–68. https://doi.org/10.1002/art.1780270401.
Murphy KE, Niederer HA, King KS, Harris EC, Glass SM, Cox CJ. Accurate interrogation of FCGR3A rs396991 in European and Asian populations using a widely available TaqMan genotyping method. Pharmacogenet Genomics. 2015;25(11):569–72. https://doi.org/10.1097/FPC.0000000000000175.
Lee YH, Ji JD, Song GG. Associations between FCGR3A polymorphisms and susceptibility to rheumatoid arthritis: a metaanalysis. J Rheumatol. 2008;35(11):2129–35. https://doi.org/10.3899/jrheum.080186.
Latiano A, Palmieri O, Valvano MR, et al. Evaluating the role of the genetic variations of PTPN22, NFKB1, and FcGRIIIA genes in inflammatory bowel disease: a meta-analysis. Inflamm Bowel Dis. 2007;13(10):1212–9. https://doi.org/10.1002/ibd.20185.
Radstake TR, Petit E, Pierlot C, van de Putte LB, Cornelis F, Barrera P. Role of Fcgamma receptors IIA, IIIA, and IIIB in susceptibility to rheumatoid arthritis. J Rheumatol. 2003;30(5):926–33.
Kim DH, Jung HD, Kim JG, et al. FCGR3A gene polymorphisms may correlate with response to frontline R-CHOP therapy for diffuse large B-cell lymphoma. Blood. 2006;108(8):2720–5. https://doi.org/10.1182/blood-2006-01-009480.
Cartron G, Dacheux L, Salles G, et al. Therapeutic activity of humanized anti-CD20 monoclonal antibody and polymorphism in IgG Fc receptor FcgammaRIIIa gene. Blood. 2002;99(3):754–8. https://doi.org/10.1182/blood.v99.3.754.
Zhang W, Gordon M, Schultheis AM, et al. FCGR2A and FCGR3A polymorphisms associated with clinical outcome of epidermal growth factor receptor expressing metastatic colorectal cancer patients treated with single-agent cetuximab. J Clin Oncol. 2007;25(24):3712–8. https://doi.org/10.1200/JCO.2006.08.8021.
Hafler JP, Maier LM, Cooper JD, et al. CD226 Gly307Ser association with multiple autoimmune diseases. Genes Immun. 2009;10(1):5–10. https://doi.org/10.1038/gene.2008.82.
International Multiple Sclerosis Genetics Consortium (IMSGC). The expanding genetic overlap between multiple sclerosis and type I diabetes. Genes Immun. 2009;10(1):11–14. https://doi.org/10.1038/gene.2008.83.
Tan RJ, Gibbons LJ, Potter C, et al. Investigation of rheumatoid arthritis susceptibility genes identifies association of AFF3 and CD226 variants with response to anti-tumour necrosis factor treatment [published correction appears in Ann Rheum Dis. 2011;70(8):1519]. Ann Rheum Dis. 2010;69(6):1029–35. https://doi.org/10.1136/ard.2009.118406.
Löfgren SE, Delgado-Vega AM, Gallant CJ, et al. A 3′-untranslated region variant is associated with impaired expression of CD226 in T and natural killer T cells and is associated with susceptibility to systemic lupus erythematosus. Arthritis Rheum. 2010;62(11):3404–14. https://doi.org/10.1002/art.27677.
Shirakawa J, Shibuya K, Shibuya A. Requirement of the serine at residue 329 for lipid raft recruitment of DNAM-1 (CD226). Int Immunol. 2005;17(3):217–23. https://doi.org/10.1093/intimm/dxh199.
Al-Mossawi MH, Ridley A, Kiedel S, Bowness P. The role of natural killer cells, gamma delta T-cells and other innate immune cells in spondyloarthritis. Curr Opin Rheumatol. 2013;25(4):434–9. https://doi.org/10.1097/BOR.0b013e3283620163.
Yau AC, Holmdahl R. Rheumatoid arthritis: identifying and characterising polymorphisms using rat models. Dis Model Mech. 2016;9(10):1111–23. https://doi.org/10.1242/dmm.026435.
Yau AC, Tuncel J, Haag S, et al. Conserved 33-kb haplotype in the MHC class III region regulates chronic arthritis. Proc Natl Acad Sci USA. 2016;113(26):E3716–24. https://doi.org/10.1073/pnas.1600567113.
Wu X, Dong H, Luo L, et al. A novel statistic for genome-wide interaction analysis. PLoS Genet. 2010;6(9):e1001131. https://doi.org/10.1371/journal.pgen.1001131.
Wang Y, Li S, Chen C, et al. MICB*002 and MICB*014 protect against rheumatoid arthritis, whereas MICA*009 and MICA*A6 are associated with rheumatoid arthritis in a Hainan Han Chinese population. Int J Rheum Dis. 2019;22(1):90–5. https://doi.org/10.1111/1756-185X.13302.
López-Arbesu R, Ballina-García FJ, Alperi-López M, et al. MHC class I chain-related gene B (MICB) is associated with rheumatoid arthritis susceptibility. Rheumatology (Oxford). 2007;46(3):426–30. https://doi.org/10.1093/rheumatology/kel331.
Woods S, Barter MJ, Elliott HR, et al. miR-324-5p is up regulated in end-stage osteoarthritis and regulates Indian Hedgehog signalling by differing mechanisms in human and mouse. Matrix Biol. 2019;77:87–100. https://doi.org/10.1016/j.matbio.2018.08.009.
Wielińska J, Crossland RE, Łacina P, et al. Exploring the extracellular vesicle microRNA expression repertoire in patients with rheumatoid arthritis and ankylosing spondylitis treated with TNF inhibitors. Dis Markers. 2021;2021:2924935. https://doi.org/10.1155/2021/2924935.
Randall LM, Kenangalem E, Lampah DA, et al. A study of the TNF/LTA/LTB locus and susceptibility to severe malaria in Highland Papuan children and adults. Malar J. 2010;9:302. https://doi.org/10.1186/1475-2875-9-302.
Pende D, Parolini S, Pessino A, et al. Identification and molecular characterization of NKp30, a novel triggering receptor involved in natural cytotoxicity mediated by human natural killer cells. J Exp Med. 1999;190(10):1505–16. https://doi.org/10.1084/jem.190.10.1505.
Pinheiro PF, Justino GC, Marques MM. NKp30 - A prospective target for new cancer immunotherapy strategies. Br J Pharmacol. 2020;177(20):4563–80. https://doi.org/10.1111/bph.15222.
Chalayer E, Gramont B, Zekre F, et al. Fc receptors gone wrong: a comprehensive review of their roles in autoimmune and inflammatory diseases. Autoimmun Rev. 2022;21(3):103016. https://doi.org/10.1016/j.autrev.2021.103016.
Márquez Pete N, Maldonado Montoro MDM, Pérez Ramírez C, et al. Influence of the FCGR2A rs1801274 and FCGR3A rs396991 polymorphisms on response to abatacept in patients with rheumatoid arthritis. J Pers Med. 2021;11(6):573. https://doi.org/10.3390/jpm11060573.
Lee YH, Bae SC, Song GG. FCGR2A, FCGR3A, FCGR3B polymorphisms and susceptibility to rheumatoid arthritis: a meta-analysis. Clin Exp Rheumatol. 2015;33(5):647–54.
Cañete JD, Suárez B, Hernández MV, et al. Influence of variants of Fc gamma receptors IIA and IIIA on the American College of Rheumatology and European League Against Rheumatism responses to anti-tumour necrosis factor alpha therapy in rheumatoid arthritis. Ann Rheum Dis. 2009;68(10):1547–52. https://doi.org/10.1136/ard.2008.096982.
Tutuncu Z, Kavanaugh A, Zvaifler N, Corr M, Deutsch R, Boyle D. Fcgamma receptor type IIIA polymorphisms influence treatment outcomes in patients with inflammatory arthritis treated with tumor necrosis factor alpha-blocking agents. Arthritis Rheum. 2005;52(9):2693–6. https://doi.org/10.1002/art.21266.
Kastbom A, Bratt J, Ernestam S, et al. Fcgamma receptor type IIIA genotype and response to tumor necrosis factor alpha-blocking agents in patients with rheumatoid arthritis. Arthritis Rheum. 2007;56(2):448–52. https://doi.org/10.1002/art.22390.
Dávila-Fajardo CL, van der Straaten T, Baak-Pablo R, et al. FcGR genetic polymorphisms and the response to adalimumab in patients with rheumatoid arthritis. Pharmacogenomics. 2015;16(4):373–81. https://doi.org/10.2217/pgs.14.178.
Morales-Lara MJ, Conesa-Zamora P, García-Simón MS, et al. Association between the FCGR3A V158F polymorphism and the clinical response to infliximab in rheumatoid arthritis and spondyloarthritis patients. Scand J Rheumatol. 2010;39(6):518–20. https://doi.org/10.3109/03009741003781969.
Mohamed RA, Abd Elazeem MI. Genetic influence of DNAM-1 (DNAX accessory molecule-1) gene polymorphism (rs 763361) on susceptibility and disease activity of systemic lupus erythematosus and rheumatoid arthritis in Egyptian patients. Comp Clin Pathol. 2017;26:543–52. https://doi.org/10.1007/s00580-017-2406-6.
Hinks A, Eyre S, Ke X, et al. Association of the AFF3 gene and IL2/IL21 gene region with juvenile idiopathic arthritis. Genes Immun. 2010;11(2):194–8. https://doi.org/10.1038/gene.2009.105.
Reinards TH, Albers HM, Brinkman DM, et al. CD226 (DNAM-1) is associated with susceptibility to juvenile idiopathic arthritis. Ann Rheum Dis. 2015;74(12):2193–8. https://doi.org/10.1136/annrheumdis-2013-205138.
Hashemi M, Zakeri Z, Eskandari-Nasab E, et al. CD226 rs763361 (Gly307Ser) polymorphism is associated with susceptibility to rheumatoid arthritis in Zahedan Southeast Iran. Iran Biomed J. 2013;17(4):194–9. https://doi.org/10.6091/ibj.1205.2013.
Bai L, Jiang J, Li H, Zhang R. Role of CD226 Rs763361 polymorphism in susceptibility to multiple autoimmune diseases. Immunol Invest. 2020;49(8):926–42. https://doi.org/10.1080/08820139.2019.1703737.
Maiti AK, Kim-Howard X, Viswanathan P, et al. Non-synonymous variant (Gly307Ser) in CD226 is associated with susceptibility to multiple autoimmune diseases. Rheumatology (Oxford). 2010;49(7):1239–44. https://doi.org/10.1093/rheumatology/kep470.
Funding
This work was supported by grants from the National Science Centre (Poland): 2016/21/B/NZ5/01901 and 2022/47/B/NZ3/01980.
Author information
Authors and Affiliations
Contributions
SB performed genotyping studies and statistical analyses and drafted and finalized the manuscript; MI contributed to the conception and design of the study and drafted the manuscript; JS, KK, and SJ provided patients’ clinical samples and clinical data; JW contributed to DNA isolation and revised the manuscript; KBK conceived and designed the study, drafted and finalized the manuscript, and provided funding. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Biały, S., Iwaszko, M., Świerkot, J. et al. Genetic variability of three common NK and γδ T cell receptor genes (FCγ3R, NCR3, and DNAM-1) and their role in Polish patients with rheumatoid arthritis and ankylosing spondylitis. Immunol Res (2024). https://doi.org/10.1007/s12026-024-09488-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12026-024-09488-3