Abstract
Purpose of Review
Leptomeningeal disease (LMD) is a rare, late complication of systemic cancer and is associated with significant neurological morbidity and high mortality. Here we provide an overview of this condition, summarizing key recent research findings and clinical practice trends in its diagnosis and treatment. We also review current clinical trials for LMD.
Recent Findings
Improved molecular diagnostic tools are in development to enable more sensitive detection of LMD, including circulating tumor cells and circulating tumor DNA. The use of targeted and CNS-penetrant therapeutics has shown survival improvements with tyrosine kinase inhibitors, antibody–drug conjugates, and select chemotherapy. However, these studies have primarily been phase I/II and retrospective analyses. There remains a dearth of clinical trials that include LMD patients.
Summary
The combination of patient-specific molecular information and novel therapeutic approaches holds significant promise for improving outcomes in patients with LMD.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kaplan JG, DeSouza TG, Farkash A, Shafran B, Pack D, Rehman F, et al. Leptomeningeal metastases: comparison of clinical features and laboratory data of solid tumors, lymphomas and leukemias. J Neurooncol. 1990;9:225–9.
Le Rhun E, Galanis E. Leptomeningeal metastases of solid cancer. Curr Opin Neurol. 2016;29:797–805.
Lamba N, Wen PY, Aizer AA. Epidemiology of brain metastases and leptomeningeal disease. Neuro Oncol. 2021;23:1447–56.
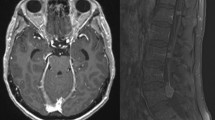
Singh SK, Leeds NE, Ginsberg LE. MR imaging of leptomeningeal metastases: Comparison of three sequences. Am J Neuroradiol. 2002;23:817–21.
Singh SK, Agris JM, Leeds NE, Ginsberg LE. Intracranial leptomeningeal metastases: comparison of depiction at FLAIR and contrast-enhanced MR imaging. Radiology. 2000;217:50–3.
Kleinschmidt-Demasters BK, Damek DM. The imaging and neuropathological effects of bevacizumab (Avastin) in patients with leptomeningeal carcinomatosis. J Neurooncol. 2010;96:375–84.
Harris P, Diouf A, Guilbert F, Ameur F, Letourneau-Guillon L, Ménard C, et al. Diagnostic reliability of leptomeningeal disease using magnetic resonance imaging. Cureus. 2019;11: e4416.
Clarke JL, Perez HR, Jacks LM, Panageas KS, Deangelis LM. Leptomeningeal metastases in the MRI era. Neurology. 2010;74:1449–54.
Le Rhun E, Taillibert S, Chamberlain M. Carcinomatous meningitis: leptomeningeal metastases in solid tumors. Surg Neurol Int. 2013;4:S265-288.
Glantz MJ, Cole BF, Glantz LK, Cobb J, Mills P, Lekos A, et al. Cerebrospinal fluid cytology in patients with cancer: minimizing false- negative results. Cancer. 1998;82:733–9.
Wasserstrom WR, Glass JP, Posner JB. Diagnosis and treatment of leptomeningeal metastases from solid tumors: experience with 90 patients. Cancer. 1982;49:759–72.
Chamberlain MC, Kormanik PA, Glantz MJ. A comparison between ventricular and lumbar cerebrospinal fluid cytology in adult patients with leptomeningeal metastases. Neuro Oncol. 2001;3:42–5.
Manne A, Paluri R. Biomarkers for carcinoma meningitis in solid tumors. J Adv Med Med Res. 2018;26:1–13.
Walbert T, Groves MD. Known and emerging biomarkers of leptomeningeal metastasis and its response to treatment. Future Oncol. 2010;6:287–97.
Corsini E, Bernardi G, Gaviani P, Silvani A, De Grazia U, Ciusani E, et al. Intrathecal synthesis of tumor markers is a highly sensitive test in the diagnosis of leptomeningeal metastasis from solid cancers. Clin Chem Lab Med. 2009;47:874–9.
Herrlinger U, Wiendl H, Renninger M, Förschler H, Dichgans J, Weller M. Vascular endothelial growth factor (VEGF) in leptomeningeal metastasis: diagnostic and prognostic value. Br J Cancer. 2004;91:219–24.
Reijneveld JC, Brandsma D, Boogerd W, Bonfrer JGM, Kalmijn S, Voest EE, et al. CSF levels of angiogenesis-related proteins in patients with leptomeningeal metastases. Neurology. 2005;65:1120–2.
Groves MD, Hess KR, Puduvalli VK, Colman H, Conrad CA, Gilbert MR, et al. Biomarkers of disease: cerebrospinal fluid vascular endothelial growth factor (VEGF) and stromal cell derived factor (SDF)-1 levels in patients with neoplastic meningitis (NM) due to breast cancer, lung cancer and melanoma. J Neurooncol. 2009;94:229–34.
Ashworth T. A case of cancer in which cells similar to those in the tumours were seen in the blood after death. Aust Med J. 1869;14:146–9.
Zhe X, Cher ML, Bonfil RD. Circulating tumor cells: finding the needle in the haystack. Am J Cancer Res. 2011;1:740–51.
Nagrath S, Sequist LV, Maheswaran S, Bell DW, Irimia D, Ulkus L, et al. Isolation of rare circulating tumour cells in cancer patients by microchip technology. Nature. 2007;450:1235–9.
Ghossein RA, Bhattacharya S, Rosai J. Molecular detection of micrometastases and circulating tumor cells in solid tumors. Clin Cancer Res. 1999;5:1950–60.
Le Rhun E, Massin F, Tu Q, Bonneterre J, Bittencourt MDC, Faure GC. Development of a new method for identification and quantification in cerebrospinal fluid of malignant cells from breast carcinoma leptomeningeal metastasis. BMC Clin Pathol. 2012;12:21.
Le Rhun E, Tu Q, De Carvalho BM, Farre I, Mortier L, Cai H, et al. Detection and quantification of CSF malignant cells by the Cell Search® technology in patients with melanoma leptomeningeal metastasis. Med Oncol. 2013;30:538.
van Bussel MTJ, Pluim D, Bol M, Beijnen JH, Schellens JHM, Brandsma D. EpCAM-based assays for epithelial tumor cell detection in cerebrospinal fluid. J Neurooncol. 2018;137:1–10.
•Van Bussel MTJ, Pluim Di, Milojkovic Kerklaan B, Bol M, Sikorska K, Linders DTC, et al. Circulating epithelial tumor cell analysis in CSF in patients with leptomeningeal metastases. Neurology. 2020;94:e521–8. Study that establishes the high sensitivity and specificity of CSF CTCs for the diagnosis of LMD.
Malani R, Fleisher M, Kumthekar P, Lin X, Omuro A, Groves MD, et al. Cerebrospinal fluid circulating tumor cells as a quantifiable measurement of leptomeningeal metastases in patients with HER2 positive cancer. J Neurooncol. 2020;148:599–606.
Moller P, Moldenhauer G, Hämmerling GJ. Immunohistochemical study of the expression of a Mr34, 000 human epithelium-specific surface glycoprotein in normal and malignant tissues. Cancer Res. 1987;47:2883–91.
Thiery JP. Epithelial-mesenchymal transitions in development and pathologies. Curr Opin Cell Biol. 2003;15:740–6.
••Pecot CV, Bischoff FZ, Mayer JA, Wong KL, Pham T, Bottsford-Miller J, et al. A novel platform for detection of CK + and CK - CTCs. Cancer Discov. 2011;1:580–6. This paper describes a novel assay for the detection of CTCs using both epithelial and mesenchymal markers.
Wan JCM, Massie C, Garcia-Corbacho J, Mouliere F, Brenton JD, Caldas C, et al. Liquid biopsies come of age: towards implementation of circulating tumour DNA. Nat Rev Cancer. 2017;17:223–38.
Phallen J, Sausen M, Adleff V, Leal A, Hruban C, White J, et al. Direct detection of early-stage cancers using circulating tumor DNA. Sci Transl Med. 2017;9:eaan2415.
Forshew T, Murtaza M, Parkinson C, Gale D, Tsui DWY, Kaper F, et al. Noninvasive identification and monitoring of cancer mutations by targeted deep sequencing of plasma DNA. Sci Transl Med. 2012;4:136ra68.
Leal A, van Grieken NCT, Palsgrove DN, Phallen J, Medina JE, Hruban C, et al. White blood cell and cell-free DNA analyses for detection of residual disease in gastric cancer. Nat Commun. 2020;11:525.
De Mattos-Arruda L, Mayor R, Ng CKY, Weigelt B, Martínez-Ricarte F, Torrejon D, et al. Cerebrospinal fluid-derived circulating tumour DNA better represents the genomic alterations of brain tumours than plasma. Nat Commun. 2015;6:8839.
Seoane J, De Mattos-Arruda L, Le RE, Bardelli A, Weller M. Cerebrospinal fluid cell-free tumour DNA as a liquid biopsy for primary brain tumours and central nervous system metastases. Ann Oncology. 2019;30:211–8.
Bettegowda C, Sausen M, Leary RJ, Kinde I, Wang Y, Agrawal N, et al. Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci Transl Med. 2014;6:224ra24.
Wang Y, Springer S, Zhang M, McMahon KW, Kinde I, Dobbyn L, et al. Detection of tumor-derived DNA in cerebrospinal fluid of patients with primary tumors of the brain and spinal cord. Proc Natl Acad Sci USA. 2015;112:9704–9.
•Zhao Y, He JY, Zou YL, Guo XS, Cui JZ, Guo L, et al. Evaluating the cerebrospinal fluid ctDNA detection by next-generation sequencing in the diagnosis of meningeal carcinomatosis. BMC Neurol. 2019;19:331. This study compared CSF ctDNA, cytology, and neuroimaging (MRI and CT) from 35 patients with meningeal carcinomatosis from various cancers and demonstrates the high sensitivity of ctDNA.
Ballester LY, Glitza Oliva IC, Douse DY, Chen MM, Lan C, Haydu LE, et al. Evaluating circulating tumor DNA from the cerebrospinal fluid of patients with melanoma and leptomeningeal disease. J Neuropathol Exp Neurol. 2018;77:628–35.
Ge M, Zhan Q, Zhang Z, Ji X, Zhou X, Huang R, et al. Different next-generation sequencing pipelines based detection of tumor DNA in cerebrospinal fluid of lung adenocarcinoma cancer patients with leptomeningeal metastases. BMC Cancer. 2019;19:143.
Jiang B-Y, Li Y, Chuai S, Zhang Z, Yang J-J, Zhong W, et al. NGS to reveal heterogeneity between cerebrospinal fluid and plasma ctDNA among non-small cell lung cancer patients with leptomeningeal carcinomatosis. J Clin Oncol. 2017;35:9022.
Choi W, Cho Y, Park SY, Hwang KH, Han JY, Lee Y. A nanowire-based liquid biopsy method using cerebrospinal fluid cell-free DNA for targeted management of leptomeningeal carcinomatosis. J Cancer Res Clin Oncol. 2021;147:213–22.
Zheng MM, Li YS, Tu HY, Jiang BY, Yang JJ, Zhou Q, et al. Genotyping of cerebrospinal fluid associated with osimertinib response and resistance for leptomeningeal metastases in EGFR-mutated NSCLC. J Thorac Oncol. 2021;16:250–8.
Stetson D, Ahmed A, Xu X, Nuttall BRB, Lubinski TJ, Johnson JH, et al. Orthogonal comparison of four plasma NGS tests with tumor suggests technical factors are a major source of assay discordance. JCO Precis Oncol. 2019;3:1–9.
Razavi P, Li BT, Brown DN, Jung B, Hubbell E, Shen R, et al. High-intensity sequencing reveals the sources of plasma circulating cell-free DNA variants. Nat Med. 2019;25:1928–37.
Fabian MR, Sonenberg N, Filipowicz W. Regulation of mRNA translation and stability by microRNAs. Annu Rev Biochem. 2010;79:351–79.
Volinia S, Calin GA, Liu CG, Ambs S, Cimmino A, Petrocca F, et al. A microRNA expression signature of human solid tumors defines cancer gene targets. Proc Natl Acad Sci USA. 2006;103:2257–61.
Teplyuk NM, Mollenhauer B, Gabriely G, Giese A, Kim E, Smolsky M, et al. MicroRNAs in cerebrospinal fluid identify glioblastoma and metastatic brain cancers and reflect disease activity. Neuro Oncol. 2012;14:689–700.
Toh WS, Lai RC, Zhang B, Lim SK. MSC exosome works through a protein-based mechanism of action. Biochem Soc Trans. 2018;46:843–53.
Zhou L, Lv T, Zhang Q, Zhu Q, Zhan P, Zhu S, et al. The biology, function and clinical implications of exosomes in lung cancer. Cancer Lett. 2017;407:84–92.
Jiang B-Y, Li Y, Wu X, Bao H, Ding Y, Yang J, et al. Identification of leptomeningeal metastasis-specific exosomal miRNA signature in cerebrospinal fluid of non-small-cell lung cancer patients. J Clin Oncol. 2018;13:S685.
Xu Q, Ye L, Huang L, Zhou L, Chen X, Ye M, et al. Serum exosomal miRNA might be a novel liquid biopsy to identify leptomeningeal metastasis in non-small cell lung cancer. Onco Targets Ther. 2021;14:2327–35.
McGranahan T, Nagpal S. A neuro-oncologist’s perspective on management of brain metastases in patients with EGFR mutant non-small cell lung cancer. Options in Oncol. 2017;18:22.
•Maillie L, Salgado LR, Lazarev S. A systematic review of craniospinal irradiation for leptomeningeal disease: past, present, and future. Clin Transl Oncol. 2021;23:2109–19. An excellent review on craniospinal irradiation in LMD, providing an overview of the research in the field, treatment, toxicities, and outcomes in 275 patients.
Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol. 2009;10:1037–44.
Yang TJ, Wijetunga NA, Yamada J, Wolden S, Mehallow M, Goldman DA, et al. Clinical trial of proton craniospinal irradiation for leptomeningeal metastases. Neuro Oncol. 2021;23:134–43.
Brown AP, Barney CL, Grosshans DR, McAleer MF, De Groot JF, Puduvalli VK, et al. Proton beam craniospinal irradiation reduces acute toxicity for adults with medulloblastoma. Int J Radiat Oncol Biol Phys. 2013;86:277–84.
Brown PD, Gondi V, Pugh S, Tome WA, Wefel JS, Armstrong TS, et al. Hippocampal avoidance during whole-brain radiotherapy plus memantine for patients with brain metastases: phase III trial NRG oncology CC001. J Clin Oncol. 2020;38:1019–29.
Jung TY, Chung WK, Oh IJ. The prognostic significance of surgically treated hydrocephalus in leptomeningeal metastases. Clin Neurol Neurosurg. 2014;119:80–3.
Su YH, Chiang CL, Yang HC, Hu YS, Chen YW, Luo YH, et al. Cerebrospinal fluid diversion and outcomes for lung cancer patients with leptomeningeal carcinomatosis. Acta Neurochir (Wien). 2022;164:459–67.
Nigim F, Critchlow JF, Kasper EM. Role of ventriculoperitoneal shunting in patients with neoplasms of the central nervous system: an analysis of 59 cases. Mol Clin Oncol. 2015;3:1381–6.
Omuro AMP, Lallana EC, Bilsky MH, DeAngelis LM. Ventriculoperitoneal shunt in patients with leptomeningeal metastasis. Neurology. 2005;64:1625–7.
Lassman AB, Abrey LE, Shah GD, Shah GG, Panageas KS, Begemann M, et al. Systemic high-dose intravenous methotrexate for central nervous system metastases. J Neurooncol. 2006;78:255–60.
Bazan F, Dobi E, Royer B, Curtit E, Mansi L, Menneveau N, et al. Systemic high-dose intravenous methotrexate in patients with central nervous system metastatic breast cancer. BMC Cancer. 2019;19:1029.
Cagney DN, Martin AM, Catalano PJ, Reitman ZJ, Mezochow GA, Lee EQ, et al. Impact of pemetrexed on intracranial disease control and radiation necrosis in patients with brain metastases from non-small cell lung cancer receiving stereotactic radiation. Radiother Oncol. 2018;126:511–8.
Kumthekar P, Grimm SA, Avram MJ, Kaklamani V, Helenowski I, Rademaker A, et al. Pharmacokinetics and efficacy of pemetrexed in patients with brain or leptomeningeal metastases. J Neurooncol. 2013;112:247–55.
Lu Y-S, Wei-Wu Chen T, Lin C-H, Yeh D-C, Tseng L-M, Wu P-F, et al. Cancer therapy: clinical bevacizumab preconditioning followed by etoposide and cisplatin is highly effective in treating brain metastases of breast cancer progressing from whole-brain radiotherapy. Clin Cancer Res. 2015;21:1851–8.
Wu PF, Lin CH, Kuo CH, Chen WW, Yeh DC, Liao HW, et al. A pilot study of bevacizumab combined with etoposide and cisplatin in breast cancer patients with leptomeningeal carcinomatosis. BMC Cancer. 2015;15:299.
Groves MD, Degroot J, Tremont I, Forman AD, Kang S, Pei B-L, et al. A pilot study of systemically administered bevacizumab in patients with neoplastic meningitis: imaging, clinical, CSF, and biomarker outcomes. Neuro Oncol. 2011;13:iii85–91.
Melisko ME, Assefa M, Hwang J, DeLuca A, Park JW, Rugo HS. Phase II study of irinotecan and temozolomide in breast cancer patients with progressing central nervous system disease. Breast Cancer Res Treat. 2019;177:401–8.
Morikawa A, De Stanchina E, Pentsova E, Kemeny MM, Li BT, Tang K, et al. Phase I study of intermittent high-dose lapatinib alternating with capecitabine for HER2-positive breast cancer patients with central nervous system metastases. Clin Cancer Res. 2019;25:3784–92.
Demeule M, Currie JC, Bertrand Y, Ché C, Nguyen T, Régina A, et al. Involvement of the low-density lipoprotein receptor-related protein in the transcytosis of the brain delivery vector Angiopep-2. J Neurochem. 2008;106:1534–44.
••Kumthekar P, Tang SC, Brenner AJ, Kesari S, Piccioni DE, Anders C, et al. ANG1005, a brain-penetrating peptide–drug conjugate, shows activity in patients with breast cancer with leptomeningeal carcinomatosis and recurrent brain metastases. Clin Cancer Res. 2020;26:2789–99. Phase II study of the peptide-drug conjugate ANG1005 (paclitaxel trevatide) in recurrent breast cancer brain metastasis patients, including 28 patients with LMD. This study demonstrated an intracranial control rate of 79% for the LMD patients.
Cross DAE, Ashton SE, Ghiorghiu S, Eberlein C, Nebhan CA, Spitzler PJ, et al. AZD9291, an irreversible EGFR TKI, overcomes T790M-mediated resistance to EGFR inhibitors in lung cancer. Cancer Discov. 2014;4:1046–61.
•Park S, Lee MH, Seong M, Kim ST, Kang JH, Cho BC, et al. A phase II, multicenter, two cohort study of 160 mg osimertinib in EGFR T790M-positive non-small-cell lung cancer patients with brain metastases or leptomeningeal disease who progressed on prior EGFR TKI therapy. Ann Oncol. 2020;31:1397–404. . Phase II study of the 3rd-generation TKI osimertinib in EGFR T70M NSCLC patients who had progressed on prior EGFR TKIs. The study showed promising survival benefit and safety profile, including in the LMD cohort of 17 patients.
Ross Camidge D, Kim DW, Tiseo M, Langer CJ, Ahn MJ, Shaw AT, et al. Exploratory analysis of brigatinib activity in patients with anaplastic lymphoma kinase-positive non–small-cell lung cancer and brain metastases in two clinical trials. J Clin Oncol. 2018;36:2693–701.
Solomon BJ, Besse B, Bauer TM, Felip E, Soo RA, Camidge DR, et al. Lorlatinib in patients with ALK-positive non-small-cell lung cancer: results from a global phase 2 study. Lancet Oncol. 2018;19:1654–67.
Gadgeel S, Peters S, Mok T, Shaw AT, Kim DW, Ou SI, et al. Alectinib versus crizotinib in treatment-naive anaplastic lymphoma kinase-positive (ALK+) non-small-cell lung cancer: CNS efficacy results from the ALEX study. Ann Oncol. 2018;29:2214–22.
Kim DW, Mehra R, Tan DSW, Felip E, Chow LQM, Camidge DR, et al. Activity and safety of ceritinib in patients with ALK-rearranged non-small-cell lung cancer (ASCEND-1): updated results from the multicentre, open-label, phase 1 trial. Lancet Oncol. 2016;17:452–63.
Chow LQ, Barlesi F, Bertino EM, van den Bent MJ, Wakelee H, Wen PY, et al. Results of the ASCEND-7 phase II study evaluating ALK inhibitor (ALKi) ceritinib in patients (pts) with ALK+ non-small cell lung cancer (NSCLC) metastatic to the brain. Ann Oncol. 2019;30:v602–3.
••Shaw AT, Bauer TM, de Marinis F, Felip E, Goto Y, Liu G, et al. First-line lorlatinib or crizotinib in advanced ALK-positive lung cancer. N Engl J Med. 2020;383:2018–29. Phase III trial comparing lorlatinib with crizotinib in 296 patients with advanced ALK-positive NSCLC with no prior systemic treatment for metastatic disease. Significantly higher PFS and intracranial response rates were seen with lorlatinib.
Lin NU, Borges V, Anders C, Murthy RK, Paplomata E, Hamilton E, et al. Intracranial efficacy and survival with tucatinib plus trastuzumab and capecitabine for previously treated HER2-positive breast cancer with brain metastases in the HER2CLIMB trial. J Clin Oncol. 2020;38:2610–9.
••Murthy RK, Loi S, Okines A, Paplomata E, Hamilton E, Hurvitz SA, et al. Tucatinib, trastuzumab, and capecitabine for HER2-positive metastatic breast cancer. N Engl J Med. 2020;382:597–609. Randomized controlled trial of patients with HER2-positive metastatic breast cancer who had been heavily pre-treated. Patients received trastuzumab, capecitabine, and either placebo or tucatinib, with improved PFS seen in the tucatinib containing cohort.
Stringer-Reasor EM, O’Brien BJ, Topletz-Erickson A, White JB, Lobbous M, Riley K, et al. Pharmacokinetic (PK) analyses in CSF and plasma from TBCRC049, an ongoing trial to assess the safety and efficacy of the combination of tucatinib, trastuzumab and capecitabine for the treatment of leptomeningeal metastasis (LM) in HER2 positive breast cancer. J Clin Oncol. 2021;39:1044–1044.
Madden R, Kosari S, Peterson GM, Bagheri N, Thomas J. Lapatinib plus capecitabine in patients with HER2-positive metastatic breast cancer: a systematic review. Int J of Clin Pharmacol Ther. 2018;56:72–80.
Freedman RA, Gelman RS, Anders CK, Melisko ME, Parsons HA, Cropp AM, et al. TBCRC 022: a phase II trial of neratinib and capecitabine for patients with human epidermal growth factor receptor 2-positive breast cancer and brain metastases. J Clin Oncol. 2019;37:1081–9.
Davies MA, Saiag P, Robert C, Grob J-J, Flaherty KT, Arance A, et al. Dabrafenib plus trametinib in patients with BRAF V600-mutant melanoma brain metastases (COMBI-MB): a multi-cohort, open-label, phase 2 trial. Lancet Oncol. 2017;18:863–73.
Long GV, Atkinson V, Lo S, Sandhu S, Guminski AD, Brown MP, et al. Combination nivolumab and ipilimumab or nivolumab alone in melanoma brain metastases: a multicentre randomised phase 2 study. Lancet Oncol. 2018;19:672–81.
•Brastianos PK, Lee EQ, Cohen JV, Tolaney SM, Lin NU, Wang N, et al. Single-arm, open-label phase 2 trial of pembrolizumab in patients with leptomeningeal carcinomatosis. Nat Med. 2020;26:1280–4. Manuscript presenting the data from the leptomeningeal cohort of a single-arm, phase II study of pembrolizumab in patients with metastatic disease, showing a 3-month OS of 60%.
Montemurro F, Delaloge S, Barrios CH, Wuerstlein R, Anton A, Brain E, et al. Trastuzumab emtansine (T-DM1) in patients with HER2-positive metastatic breast cancer and brain metastases: exploratory final analysis of cohort 1 from KAMILLA, a single-arm phase IIIb clinical trial. Ann Oncol. 2020;31:1350–8.
Jerusalem G, Park YH, Yamashita T, Hurvitz SA, Chen S, Cathcart J, et al. CNS metastases in HER2-positive metastatic breast cancer treated with trastuzumab deruxtecan: DESTINY-Breast01 subgroup analyses. Ann Oncol. 2020;31:S63–4.
Bardia A, Hurvitz SA, Tolaney SM, Loirat D, Punie K, Oliveira M, et al. Sacituzumab govitecan in metastatic triple-negative breast cancer. N Engl J Med. 2021;384:1529–41.
Brenner AJ, Pandey R, Chiou J, Floyd J, Surapreneni P, Kaklamani V, et al. Abstract PD13–05: delivery and activity of SN-38 by sacituzumab govitecan in breast cancer brain metastases. Cancer Res. 2021;81:PD13-05.
Bonneau C, Paintaud G, Trédan O, Dubot C, Desvignes C, Dieras V, et al. Phase I feasibility study for intrathecal administration of trastuzumab in patients with HER2 positive breast carcinomatous meningitis. Eur J Cancer. 2018;95:75–84.
Kumthekar P, Lassman AB, Lin N, Grimm S, Gradishar W, Pentsova E, et al. LPTO-02. Intrathecal (IT) trastuzumab for the treatment of leptomeningeal disease (LM) in patients (PTS) with human epidermal receptor-2 positive (HER2+) cancer: a multicenter phase 1/2 study. Neuro-Oncology Adv. 2019;1:6.
Glantz MJ, Jaeckle KA, Chamberlain MC, Phuphanich S, Recht L, Swinnen LJ, et al. A randomized controlled trial comparing intrathecal sustained-release cytarabine (DepoCyt) to intrathecal methotrexate in patients with neoplastic meningitis from solid tumors. Clin Cancer Res. 1999;5:3394–402.
Glantz MJ, LaFollette S, Jaeckle KA, Shapiro W, Swinnen L, Rozental JR, et al. Randomized trial of a slow-release versus a standard formulation of cytarabine for the intrathecal treatment of lymphomatous meningitis. J Clin Oncol. 1999;17:3110–6.
Jaeckle KA, Phuphanich S, Bent MJ, Aiken R, Batchelor T, Campbell T, et al. Intrathecal treatment of neoplastic meningitis due to breast cancer with a slow-release formulation of cytarabine. Br J Cancer. 2001;84:157–63.
Jaeckle KA, Batchelor T, O’Day SJ, Phuphanich S, New P, Lesser G, et al. An open label trial of sustained-release cytarabine (DepoCyt) for the intrathecal treatment of solid tumor neoplastic meningitis. J Neurooncol. 2002;57:231–9.
•Le Rhun E, Wallet J, Mailliez A, Le Deley MC, Rodrigues I, Boulanger T, et al. Intrathecal liposomal cytarabine plus systemic therapy versus systemic chemotherapy alone for newly diagnosed leptomeningeal metastasis from breast cancer. Neuro Oncol. 2020;22:524–38. One of the few phase III trials in the field evaluating the benefit of intrathecal cytarabine on patients with LMD.
Chamberlain MC, Tsao-Wei DD, Groshen S. Phase II trial of intracerebrospinal fluid etoposide in the treatment of neoplastic meningitis. Cancer. 2006;106:2021–7.
Grossman SA, Finkelstein DM, Ruckdeschel JC, Trump DL, Moynihan TT, Ettinger DS. Randomized prospective comparison of intraventricular methotrexate and thiotepa in patients with previously untreated neoplastic meningitis. J Clin Oncol. 1993;11:561–9.
Pan Z, Yang G, He H, Zhao G, Yuan T, Li Y, et al. Concurrent radiotherapy and intrathecal methotrexate for treating leptomeningeal metastasis from solid tumors with adverse prognostic factors: a prospective and single-arm study. Int J Cancer. 2016;139:1864–72.
Pan Z, Yang G, He H, Cui J, Li W, Yuan T, et al. Intrathecal pemetrexed combined with involved-field radiotherapy as a first-line intra-CSF therapy for leptomeningeal metastases from solid tumors: a phase I/II study. Ther Adv Med Oncol. 2020;12:1–14.
Pan Z, Yang G, Cui J, Li W, Li Y, Gao P, et al. A pilot phase 1 study of intrathecal pemetrexed for refractory leptomeningeal metastases from non-small-cell lung cancer. Front Oncol. 2019;30:838.
Fan C, Zhao Q, Li L, Shen W, Du Y, Teng C, et al. Efficacy and safety of intrathecal pemetrexed combined with dexamethasone for treating TKI-failed leptomeningeal metastases from EGFR-mutant NSCLC—a prospective open-label single-arm phase I/II clinical trial (unique identifier: ChiCTR1800016615). J Thorac Oncol. 2021;16:1359–68.
Bleyer WA, Pizzo PA, Spence AM, Platt WD, Benjamin DR, Kolins J, et al. The Ommaya reservoir. Newly recognized complications and recommendations for insertion and use. Cancer. 1978;41:2431–7.
Li J, Li X, Tong X, Liu J, Huang B, Chen M, et al. Investigation of the optimal duration of bed rest in the supine position to reduce complications after lumbar puncture combined with intrathecal chemotherapy: a multicenter prospective randomized controlled trial. Support Care Cancer. 2018;26:2995–3002.
Shapiro WR, Young DF, Mehta BM. Methotrexate: distribution in cerebrospinal fluid after intravenous, ventricular and lumbar injections. N Engl J Med. 1975;293:161–6.
Glantz MJ, Van Horn A, Fisher R, Chamberlain MC. Route of intracerebrospinal fluid chemotherapy administration and efficacy of therapy in neoplastic meningitis. Cancer. 2010;116:1947–52.
De Oca Delgado MM, Díaz BC, Zambrano JS, Juárez VG, Martínez MSL, Martínez EC, et al. The comparative treatment of intraventricular chemotherapy by Ommaya reservoir vs. lumbar puncture in patients with leptomeningeal carcinomatosis. Front Oncol. 2018;8:509.
Zagouri F, Sergentanis TN, Bartsch R, Berghoff AS, Chrysikos D, De Azambuja E, et al. Intrathecal administration of trastuzumab for the treatment of meningeal carcinomatosis in HER2-positive metastatic breast cancer: a systematic review and pooled analysis. Breast Cancer Res Treat. 2013;139:13–22.
Figura NB, Long W, Yu M, Robinson TJ, Mokhtari S, Etame AB, et al. Intrathecal trastuzumab in the management of HER2+ breast leptomeningeal disease: a single institution experience. Breast Cancer Res Treat. 2018;169:391–6.
Glitza IC, Phillips S, Brown C, Haymaker CL, Bassett RL, Lee JJ, et al. Single-center phase I/Ib study of concurrent intrathecal (IT) and intravenous (IV) nivolumab (N) for metastatic melanoma (MM) patients (pts) with leptomeningeal disease (LMD). J Clin Oncol. 2020;38:10008–10008.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neuro-Oncology
Rights and permissions
About this article
Cite this article
Sharma, A., Low, J.T. & Kumthekar, P. Advances in the Diagnosis and Treatment of Leptomeningeal Disease. Curr Neurol Neurosci Rep 22, 413–425 (2022). https://doi.org/10.1007/s11910-022-01198-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-022-01198-3