Abstract
Background
Elevated vascular endothelial growth factor (VEGF) was associated with poor prognosis in leptomeningeal carcinomatosis and anti-angiogenic therapy was found to prolong the survival of mice in preclinical studies. This prospective pilot study investigated the efficacy of anti-VEGF therapy plus chemotherapy in patients with leptomeningeal carcinomatosis originating from breast cancer.
Methods
Eligible patients were scheduled to receive bevacizumab combined with etoposide and cisplatin (BEEP) every 3 weeks for a maximum of 6 cycles or until unacceptable toxicity. The primary objective was the central nervous system (CNS)-specific response rate, which was defined as disappearance of cancer cells in the cerebrospinal fluid (CSF) and an improved or stabilized neurologic status. The impact of VEGF inhibition on etoposide penetration into the CSF was analyzed.
Results
Eight patients were enrolled. The CNS-specific response rate was 60% in 5 evaluable patients. According to intent-to-treat analysis, the median overall survival of the eight patients was 4.7 months (95% confidence interval, CI, 0.3–9.0) and the neurologic progression-free survival was 4.7 months (95% CI 0–10.5). The most common grade 3/4 adverse events were neutropenia (23.1%), leukopenia (23.1%), and hyponatremia (23.1%). The etoposide concentrations in the CSF were much lower than those in plasma, and bevacizumab did not increase etoposide delivery to the CSF.
Conclusions
BEEP exhibited promising efficacy in breast cancer patients with leptomeningeal carcinomatosis. Additional studies are warranted to verify its efficacy and clarify the role of anti-angiogenic therapy in this disease.
Trial registration
ClinicalTrials.gov identifying number NCT01281696.
Similar content being viewed by others
Background
Leptomeningeal carcinomatosis results from the spread of cancer cells to the leptomeninges and dissemination within the cerebrospinal fluid (CSF). It has become increasingly common because of the prolonged survival of cancer patients and improvements of diagnostic methods. Approximately 4% − 15% of patients with solid cancers develop leptomeningeal carcinomatosis, and breast cancers, lung cancers, and melanoma are the most common origins. The treatments include intra-CSF and systemic chemotherapy, irradiation, and surgery of bulky metastases. Despite the administration of aggressive treatments, the prognosis is poor, with the median overall survival (OS) ranging from 8 to 16 weeks [1,2].
Recent studies have shown that vascular endothelial growth factor (VEGF) levels in the CSF were significantly higher in patients with leptomeningeal carcinomatosis and correlated with a poor prognosis [3-5]. Reijneveld et al. also found that inhibition of angiogenesis prolonged the survival of mice with leptomeningeal carcinomatosis [6]. These findings suggest that VEGF plays pivotal roles in this disease.
Bevacizumab is a recombinant, humanized monoclonal antibody directed against VEGF. It has exhibited efficacy in metastatic breast cancer, colorectal cancer, non-small-cell lung cancer (NSCLC), and glioblastoma multiforme. Our previous study of bevacizumab combined with etoposide and cisplatin (BEEP) demonstrated significant activity for brain metastasis of breast cancer that progressed after whole brain radiation therapy [7]. This pilot study examined the efficacy of BEEP in breast cancer patients with leptomeningeal carcinomatosis. Translational research was performed to evaluate the effects of anti-VEGF therapy on drug delivery to the CSF.
Methods
Study design
This prospective, multicenter pilot study was conducted to evaluate the efficacy and safety of BEEP in patients with leptomeningeal carcinomatosis originating from breast cancer. The study was performed at 3 centers in Taiwan from November 2010 to March 2013. The protocol was approved by the research ethics committees of all of the participating centers (National Taiwan University Hospital Research Ethics Committee and Institutional Review Board of Taichung Veterans General Hospital). This trial is registered on ClinicalTrials.gov and has the identification number NCT01281696.
Eligibility criteria
Patients who had leptomeningeal carcinomatosis originating from breast cancer, based on positive CSF cytology findings, were eligible to participate in this study. Additional inclusion criteria were an age of 18 to 75 years and adequate organ functions and bone marrow reserve.
The major exclusion criteria were prior VEGF-targeted therapy; a history of thrombotic or hemorrhagic disorders; severe nonhealing wounds, ulcers, or bone fractures; regular use of medication that increases bleeding tendency.
Concurrent intrathecal treatment with methotrexate was permitted during the study period. Patients were required to sign an informed consent form before being enrolled in the study.
Treatment administration
Patients were scheduled to receive BEEP (15 mg/kg of bevacizumab on Day 1; etoposide at 70 mg/m2/d from Day 2 to Day 4; and cisplatin at 70 mg/m2/d on Day 2) every 3 weeks for a maximum of 6 cycles or until a level of unacceptable toxicity was reached. The use of prophylactic G-CSF (granulocyte colony-stimulating factor) was allowed.
In the first cycle, some modifications of the treatment schedule for the translational research were introduced. Etoposide was administered from Day 1 to Day 3, and bevacizumab was administered 6 hours after etoposide infusion was completed on Day 1.
Cerebrospinal fluid concentration of etoposide
Patients who had an Ommaya reservoir were subjected to translational research to assess the effects of anti-VEGF treatment on the delivery of etoposide to the CSF. The temporal changes in the etoposide concentration in the CSF and plasma were determined using ultrahigh-performance liquid chromatography with tandem mass spectrometry, as previously described [8].
Efficacy assessments
Clinical evaluations, including physical, neurological, and CSF cytology examinations, were performed at the baseline and during the study. Tumor-associated neurological signs and symptoms were assessed based on the criteria used by Lin et al. [9]. Cytologic negative conversion was defined as the absence of malignant cells in the CSF 2 times in succession. A CNS-specific response was defined as a negative conversion according to the CSF cytology results and a stable or improved neurological status. Patients whose CSF cytology results were persistently positive or positive after only one negative cytology result was obtained were considered nonresponders. Neurologic progression was defined as the observation of positive cytology results after confirmation of a negative conversion, or evidence of leptomeningeal disease progression upon neurological examination [10,11]. All patients were followed until death.
Safety assessments
Adverse events (AE) were assessed and graded according to NCI CTCAE v3.0 (National Cancer Institute Common Terminology Criteria for Adverse Events). The patients were followed for safety until at least 30 days after discontinuation of the study drug. Severe AEs were defined according to International Conference on Harmonization Good Clinical Practice guidelines. The safety profile was evaluated by recording the incidence and severity of AEs.
Study objectives
The primary end point of the study was the CNS-specific response rate. Secondary end points included neurologic progression-free survival (PFS) and OS. Furthermore, the study evaluated the impact of VEGF inhibition on etoposide penetration into the CSF.
Statistics
OS was defined as the time from the initiation of the study medications until death from any cause or the date of last contact with the patient. Neurologic PFS was defined as the time from the initiation of the study medications until the earliest date of neurologic disease progression or death from any cause. OS and PFS estimates were obtained using Kaplan–Meier survival curves. Continuous variables are reported as means and ranges. Categorical variables are reported as frequencies and percentages. All statistical evaluations were performed using SPSS 15.0. A statistical difference was considered to be significant when P < .05.
Results
Patient characteristics
A total of 8 patients were enrolled in the study, and their baseline clinical characteristics are listed in Table 1. The median age was 55 years (range, 30–65 y) and the median ECOG (Eastern Cooperative Oncology Group) performance status was 2.5 (range, 2–3). Three patients (38%) had received hormone therapy, 2 patients (25%) had received HER2-targeted therapy, and 8 patients (100%) had received chemotherapy for their primary disease; furthermore, 2 patients (25%) had undergone surgery, 4 patients (50%) had undergone radiotherapy, and 6 patients (75%) had received intrathecal chemotherapy for CNS metastases. Five patients (63%) exhibited leptomeningeal metastasis according to MRI examination. Systemic disease outside the central nervous system (CNS) was not under control at the time of leptomeningeal carcinomatosis diagnosis in 5 patients (63%).
Treatment administration
The mean number of cycles administered was 3.3 (median, 3.0). Only 2 of 8 patients (25%) completed the planned 6 cycles of treatments. The reasons that 6 patients did not complete the study are listed as follows: one patient (13%) exhibited both CNS and extra-CNS disease progression; one patient (13%) exhibited only extra-CNS disease progression; one patient (13%) exhibited no CSF cytologic response; and 3 patients (38%) withdrew from the study. Six patients concurrently received intrathecal methotrexate therapy. The treatment course of each patient is shown in the Additional file 1.
Safety
The AEs are listed in Table 2. The most common grade 3/4 AEs were neutropenia (23.1%), leukopenia (23.1%), and hyponatremia (23.1%). Nonhematologic toxicity was generally modest. All AEs resolved to grade 1 or lower.
Efficacy
The patient characteristics and their outcomes are listed in the Table 3. Because 3 patients withdrew from the study before undergoing follow-up CSF studies and neurologic assessments, the CNS-specific response was evaluable in 5 patients. Three patients (60%) were responsive, exhibiting the clearance of malignant cells in successive CSF studies, and 2 of them completed the planned treatment courses. One patient was considered nonresponsive because positive cytology results were observed after a single negative cytology result was obtained, and one patient’s CSF cytology results were persistently positive. Clinically, 3 patients (60%) improved neurologically without evidence of systemic progression; one patient (20%) was neurologically stable but progressed systemically; and one patient (20%) exhibited both neurologic and systemic progression.
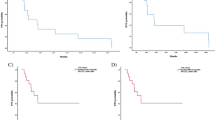
The 8 patients were subjected to a survival analysis according to the intent-to-treat analysis. The median OS was 4.7 months (95% CI 0.3–9.0; Figure 1). The responders of CSF cytology had a trend toward longer median overall survival (9.0 vs 2.9 months, P = 0.076). The OS of the 3 responders was 10.7, 9.0, and 4.7 months respectively. The neurologic PFS was 4.7 months (95% CI 0–10.5; Figure 1).
Cerebrospinal fluid concentration of etoposide
Four patients were subjected to serial measurements of etoposide concentrations in the CSF and plasma before and after bevacizumab administration. A plot of the individual ratio of the etoposide concentration in the CSF to that in the plasma versus time is shown in Figure 2A. We observed that bevacizumab administered 24 hours prior to the administration of cytotoxic drugs exerted no significant effects on etoposide penetration into the CSF (Figure 2B, P = .167, .680, .754, at 1 h, 2 h, and 6 h, respectively).
Discussion
Several retrospective studies and case reports have demonstrated the feasibility of using systemic therapies, including capecitabine, lapatinib, gefitinib, erlotinib, and bevacizumab therapies, in treating leptomeningeal carcinomatosis [12-17]. However, only a few prospective clinical trials have been conducted [18-22] (Table 4). This is partly because of the difficulties in conducting a large trial among patients with extremely poor prognoses, for whom treatment may be discontinued early, precluding a full assessment of the agents that exhibit potential activity in treating this disease.
According to our thorough review of research, this is the first prospective pilot study to report on the efficacy of anti-VEGF therapy plus chemotherapy in leptomeningeal carcinomatosis. Specifically, the CNS-specific response rate was 60% and the median OS was 4.7 months (95% CI 0.3–9.0). Groves et al. [23] reported that administration of bevacizumab alone yielded a 13% CSF response and a median OS of 14 weeks. Because of the heterogeneity of the enrolled patients and differences in response criteria among studies, comparing the efficacy of various systemic treatments is difficult (Table 4). In addition, the ability to make statistically sound conclusions was limited by the small sample size of our study. Because this patient population is seldom included in clinical trials, any treatment with evidence of response warrants further investigation.
Among the 8 patients enrolled in this study, 3 patients dropped out during the early phase of the trial due to patients’ refusal of continued treatments. Only 5 patients underwent follow-up CSF studies and neurologic assessments, and were evaluable for the CNS-specific response. In addition to excluding the 3 dropouts in the final analysis, the response rates could also be estimated by assuming that the 3 dropped patients were non-responders, that is, 3/8 (38%). In this way, it underestimated the true response rate and could be considered as a low bound of the estimated response rate based on the data of this study. Similarly, the PFS could also be analyzed in two ways by including (1) all 8 patients, and (2) only the 5 patients who completed the response evaluation. The former included the 3 dropped patients who did not complete the response evaluation, and thus it also underestimated the effect of the proposed treatment on PFS (4.7 months versus 7.6 months) and could be considered as a low bound of the estimated effect of the proposed treatment on PFS based on the data of this study.
Intrathecal methotrexate has been used for a long time, but its value is questioned, with median survival of about 7–16 weeks in previous reports (7 weeks, Fizazi et al.; 11 weeks, Glantz et al.; 16 weeks, Rudnicka et al. and Grossman et al.) [11,24-26]. The median overall survival in our study was 4.7 months, which seems slightly better than intrathecal methotrexate treatment in previous serials. Although the efficacy of bevacizumab-based therapy might be confounded by the concurrent intrathecal methotrexate therapy administered in this study, the observation that one patient was responsive to BEEP rechallenge while disease progressed under maintenance intrathecal methotrexate therapy provides evidence that BEEP can benefit leptomeningeal carcinomatosis patients (Table 3, Patient 1).
Increasing evidence suggests that abnormal tumor vasculature can hinder effective cancer therapy; furthermore, VEGF inhibition can transiently normalize tumor vasculature and improve tumor perfusion as well as the delivery of subsequent chemotherapy [27-29]. In the study conducted by Dickson et al., the penetration of chemotherapy was improved when it was administered 1 to 3 days after bevacizumab administration in the neuroblastoma xenograft model [29]. Although Van der Veldt et al. observed that bevacizumab reduced perfusion and the uptake of trace amounts of [11C] docetaxel in NSCLC tissues within 5 hours to at least 4 days, the effects of bevacizumab on microdoses of drug delivery in tumors may not hold true for pharmacological drug concentrations [30].
In the present study, cytotoxic drugs were administered 24 hours after the administration of bevacizumab to enhance efficacy based on the normalization theory [29-31]. We observed that anti-VEGF therapy exerted no significant effects on the penetration of etoposide into the CSF. Additional studies are required to clarify whether different schedules for treatments in which bevacizumab is combined with cytotoxic agents increase drug penetration into the CSF and improve the treatment efficacy.
Conclusions
BEEP regimen exhibited promising efficacy in breast cancer patients with leptomeningeal carcinomatosis. Additional studies are warranted to verify the efficacy of the regimen and clarify the role of bevacizumab in this disease.
Abbreviations
- VEGF:
-
Elevated vascular endothelial growth factor
- BEEP:
-
Bevacizumab combined with etoposide and cisplatin
- CNS:
-
Central nervous system
- CSF:
-
Cerebrospinal fluid
- 95% CI:
-
95% confidence interval
- OS:
-
Overall survival
- NSCLC:
-
Non-small cell lung cancer
- G-CSF:
-
Granulocyte colony-stimulating factor
- AE:
-
Adverse events
- PFS:
-
Progression-free survival
References
Beauchesne P. Intrathecal chemotherapy for treatment of leptomeningeal dissemination of metastatic tumours. Lancet Oncol. 2010;11(9):871–9.
Lombardi G, Zustovich F, Farina P, Della Puppa A, Manara R, Cecchin D, et al. Neoplastic meningitis from solid tumors: new diagnostic and therapeutic approaches. Oncologist. 2011;16(8):1175–88.
Herrlinger U, Wiendl H, Renninger M, Forschler H, Dichgans J, Weller M. Vascular endothelial growth factor (VEGF) in leptomeningeal metastasis: diagnostic and prognostic value. Br J Cancer. 2004;91(2):219–24.
Reijneveld JC, Brandsma D, Boogerd W, Bonfrer JG, Kalmijn S, Voest EE, et al. CSF levels of angiogenesis-related proteins in patients with leptomeningeal metastases. Neurology. 2005;65(7):1120–2.
Groves MD, Hess KR, Puduvalli VK, Colman H, Conrad CA, Gilbert MR, et al. Biomarkers of disease: cerebrospinal fluid vascular endothelial growth factor (VEGF) and stromal cell derived factor (SDF)-1 levels in patients with neoplastic meningitis (NM) due to breast cancer, lung cancer and melanoma. J Neurooncol. 2009;94(2):229–34.
Reijneveld JC, Taphoorn MJ, Kerckhaert OA, Drixler TA, Boogerd W, Voest EE. Angiostatin prolongs the survival of mice with leptomeningeal metastases. Eur J Clin Invest. 2003;33(1):76–81.
Lu YS, Chen TW, Lin CH, Yeh DC, Tseng LM, Wu PF, et al. Bevacizumab Preconditioning Followed by Etoposide and Cisplatin Is Highly Effective in Treating Brain Metastases of Breast Cancer Progressing from Whole-Brain Radiotherapy. Clin Cancer Res. 2015; 21(8):1851–8. doi: 10.1158/1078-0432.CCR-14-2075. Epub 2015 Feb 19.
Liao HW LY, Lin CH, Kuo CH. A rapid and sensitive liquid chromatography tandem mass spectrometry method for quantification of etoposide and etoposide chatechol in cerebrospinal fluid (PMo-003). In: International Mass Spectrometry Conference 2012. 2012.
Lin NU, Dieras V, Paul D, Lossignol D, Christodoulou C, Stemmler HJ, et al. Multicenter phase II study of lapatinib in patients with brain metastases from HER2-positive breast cancer. Clin Cancer Res. 2009;15(4):1452–9.
Groves MD, Glantz MJ, Chamberlain MC, Baumgartner KE, Conrad CA, Hsu S, et al. A multicenter phase II trial of intrathecal topotecan in patients with meningeal malignancies. Neuro Oncol. 2008;10(2):208–15.
Glantz MJ, Jaeckle KA, Chamberlain MC, Phuphanich S, Recht L, Swinnen LJ, et al. A randomized controlled trial comparing intrathecal sustained-release cytarabine (DepoCyt) to intrathecal methotrexate in patients with neoplastic meningitis from solid tumors. Clin Cancer Res. 1999;5(11):3394–402.
Shigekawa T, Takeuchi H, Misumi M, Matsuura K, Sano H, Fujiuchi N, et al. Successful treatment of leptomeningeal metastases from breast cancer using the combination of trastuzumab and capecitabine: a case report. Breast Cancer. 2009;16(1):88–92.
Ekenel M, Hormigo AM, Peak S, Deangelis LM, Abrey LE. Capecitabine therapy of central nervous system metastases from breast cancer. J Neurooncol. 2007;85(2):223–7.
Tham YL, Hinckley L, Teh BS, Elledge R. Long-term clinical response in leptomeningeal metastases from breast cancer treated with capecitabine monotherapy: a case report. Clin Breast Cancer. 2006;7(2):164–6.
Paydas S, Bicakci K, Yavuz S. Dramatic response with capecitabine after cranial radiation to the brain parenchymal and leptomeningeal metastases from lung cancer. Eur J Intern Med. 2009;20(1):96–9.
Ku GY, Krol G, Ilson DH. Successful treatment of leptomeningeal disease in colorectal cancer with a regimen of bevacizumab, temozolomide, and irinotecan. J Clin Oncol. 2007;25(13):e14–6.
Onishi H, Morisaki T, Nakafusa Y, Nakashima Y, Yokohata K, Katano M. Objective response with lapatinib in patients with meningitis carcinomatosa derived from HER2/HER1-negative breast cancer. Int J Clin Oncol. 2011;16(6):718–21.
Rivera E, Meyers C, Groves M, Valero V, Francis D, Arun B, et al. Phase I study of capecitabine in combination with temozolomide in the treatment of patients with brain metastases from breast carcinoma. Cancer. 2006;107(6):1348–54.
Tetef ML, Margolin KA, Doroshow JH, Akman S, Leong LA, Morgan Jr RJ, et al. Pharmacokinetics and toxicity of high-dose intravenous methotrexate in the treatment of leptomeningeal carcinomatosis. Cancer Chemother Pharmacol. 2000;46(1):19–26.
Kiewe P, Thiel E, Reinwald M, Korfel A. Topotecan and ifosfamide systemic chemotherapy for CNS involvement of solid tumors. J Neurooncol. 2011;103(3):629–34.
Peereboom DM, Murphy C, Ahluwalia MS, Conlin A, Eichler A, Van Poznak C, et al. Phase II trial of patupilone in patients with brain metastases from breast cancer. Neuro Oncol. 2014;16(4):579–83.
Segura PP, Gil M, Balana C, Chacon I, Langa JM, Martin M, et al. Phase II trial of temozolomide for leptomeningeal metastases in patients with solid tumors. J Neurooncol. 2012;109(1):137–42.
Groves MD, DeGroot J, Tremont I, Forman A, Kang S, Pei BL, et al. A pilot study of systemically administered bevacizumab in patients with neoplastic meningitis: imaging, clinical, CSF, and biomarker outcomes. Neuro Oncol (2011). 2011;13 suppl 3:iii85–91.
Fizazi K, Asselain B, Vincent-Salomon A, Jouve M, Dieras V, Palangie T, et al. Meningeal carcinomatosis in patients with breast carcinoma. Clinical features, prognostic factors, and results of a high-dose intrathecal methotrexate regimen. Cancer. 1996;77(7):1315–23.
Rudnicka H, Niwinska A, Murawska M. Breast cancer leptomeningeal metastasis–the role of multimodality treatment. J Neurooncol. 2007;84(1):57–62.
Grossman SA, Finkelstein DM, Ruckdeschel JC, Trump DL, Moynihan T, Ettinger DS. Randomized prospective comparison of intraventricular methotrexate and thiotepa in patients with previously untreated neoplastic meningitis. Eastern Cooperative Oncology Group. J Clin Oncol. 1993;11(3):561–9.
Batchelor TT, Sorensen AG, di Tomaso E, Zhang WT, Duda DG, Cohen KS, et al. AZD2171, a pan-VEGF receptor tyrosine kinase inhibitor, normalizes tumor vasculature and alleviates edema in glioblastoma patients. Cancer Cell. 2007;11(1):83–95.
Jain RK. Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science. 2005;307(5706):58–62.
Dickson PV, Hamner JB, Sims TL, Fraga CH, Ng CY, Rajasekeran S, et al. Bevacizumab-induced transient remodeling of the vasculature in neuroblastoma xenografts results in improved delivery and efficacy of systemically administered chemotherapy. Clin Cancer Res. 2007;13(13):3942–50.
Van der Veldt AA, Lubberink M, Bahce I, Walraven M, de Boer MP, Greuter HN, et al. Rapid decrease in delivery of chemotherapy to tumors after anti-VEGF therapy: implications for scheduling of anti-angiogenic drugs. Cancer Cell. 2012;21(1):82–91.
Lu YS CB, Lin CH, Chen WW, Wu PF, Cheng AL, Shih Tiffany TF. Normalization of tumor vasculature by anti-angiogenesis therapy in metastatic tumor: A clinical study to determine the timing and effect. Proceedings: AACR Annual Meeting 2014. Cancer Res. 2014;74:abstract 2984.
Acknowledgements
We would like to thank Dr. Ming Gao for administrative support. This work was supported by grants from National Taiwan University (NTU-ICRP-103R7557) and National Science Council, Executive Yuan, Taiwan (NSC 101-2325-B-002–091).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
C-HL, W-WC, Y-SL and A-LC contributed to the design and execution of the study. C-HL, W-WC, Y-SL and D-CY accrued patients, collected clinical data and specimens. C-HK and H-WL carried out the experiments. S-MH provided the administrative support and analyzed the data. C-HL, P-FW, Y-SL and A-LC interpreted the findings. P-FW analyzed the data and drafted the manuscript. Y-SL coordinated and oversaw the execution of the study. All authors read and approved the final manuscript.
Additional file
Additional file 1:
The treatment course of each patient.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Wu, PF., Lin, CH., Kuo, CH. et al. A pilot study of bevacizumab combined with etoposide and cisplatin in breast cancer patients with leptomeningeal carcinomatosis. BMC Cancer 15, 299 (2015). https://doi.org/10.1186/s12885-015-1290-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-015-1290-1