Abstract
Purpose of Review
Fluid retention or congestion is a major cause of symptoms, poor quality of life, and adverse outcome in patients with heart failure (HF). Despite advances in disease-modifying therapy, the mainstay of treatment for congestion—loop diuretics—has remained largely unchanged for 50 years. In these two articles (part I: loop diuretics and part II: combination therapy), we will review the history of diuretic treatment and current trial evidence for different diuretic strategies and explore potential future directions of research.
Recent Findings
We will assess recent trials, including DOSE, TRANSFORM, ADVOR, CLOROTIC, OSPREY-AHF, and PUSH-AHF, and assess how these may influence current practice and future research.
Summary
There are few data on which to base diuretic therapy in clinical practice. The most robust evidence is for high-dose loop diuretic treatment over low-dose treatment for patients admitted to hospital with HF, yet this is not reflected in guidelines. There is an urgent need for more and better research on different diuretic strategies in patients with HF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most patients admitted to the hospital with heart failure (HF) exhibit substantial water and salt retention requiring treatment with intravenous (IV) loop diuretics, [1, 2] a therapeutic strategy that has remained largely unchanged for the last 60 years [3]. Although loop diuretics alone may be sufficient for some patients, there is a ceiling of treatment beyond which increasing the dose does not greatly increase diuresis. Resistance to the actions of escalating doses of loop diuretics is common,[4, 5] which can often be overcome by adding a different class of diuretic agent.
There are many possible adjuncts to loop diuretic therapy, including thiazide diuretics, acetazolamide, sodium-glucose co-transporter 2 inhibitors (SGLT2I), arginine vasopressin (AVP) antagonists, hypertonic saline, and oral salt. Each intervention has evidence to support its use as an adjunct to loop diuretic treatment, [6,7,8,9,10,11,12].
The European Society of Cardiology HF guidelines recommend the use of thiazide diuretics or acetazolamide in patients who fail to respond adequately to loop diuretic treatment [13]. However, most patients admitted with severe congestion spend more than a week in hospital [14]. Early use of combination therapy may lead to rapid decongestion, [15] which may shorten hospital stay, reducing the risk of nosocomial infection, falls, and physical deconditioning. This, in turn, may lead to improved quality of life (QoL) and better outcomes [16]. Combination diuretic therapy may also allow a reduction in the dose of loop diuretic required to control congestion, reducing side effects of loop diuretics including diuretic resistance. [17] .
On the other hand, more aggressive diuresis may lead to hypotension, renal dysfunction, and electrolyte abnormalities, which may contribute to diuretic resistance, longer hospital stays, worse QoL, and, in the case of HeFREF, may impede initiation or titration of disease-modifying therapies. In the present article, we review possible adjunctive therapies to loop diuretic agents, discuss recent evidence on combination therapy, and highlight some of the gaps in evidence that remain to be addressed.
Thiazide or Thiazide-Like Diuretics
Thiazide or thiazide-like diuretics (bendroflumethiazide, metolazone, hydrochlorothiazide) inhibit the Na+-Cl−+ co-transporter in the distal convoluted tubule (DCT) increasing urine sodium excretion which causes a diuresis (Fig. 1). The only evidence to support the use of thiazide and thiazide-like diuretics in patients with HF came from small, randomised trials, often conducted in patients who did not have overt congestion. These generally showed a marked, acute increase in natriuresis and diuresis when given in combination with loop diuretics. [18].
In the CLOROTIC trial, 230 patients admitted to the hospital with HF were randomised to varying doses of oral hydrochlorothiazide or matching placebo based on baseline eGFR in addition to IV furosemide given at usual oral daily dose (mean 80 mg per day) (Table 1)0.7 The co-primary endpoints were changes in body weight and patient-reported symptoms from baseline to 3 days.
Hydrochlorothiazide was associated with greater weight loss (− 2.3 kg vs. − 1.5 kg; P = 0.002) but had no effect on symptoms. Although not a pre-specified endpoint, patients randomised to hydrochlorothiazide had fewer signs of congestion after 3 days of treatment. The median length of stay was 7 days and was unaffected by treatment allocation.
There was no difference in the rate of hyponatraemia between hydrochlorothiazide and placebo, but the rate of hypokalaemia (≤ 3.5 mmol/l) was approximately twice as likely with hydrochlorothiazide. There was a trend towards higher rates of all-cause hospitalisation and all-cause mortality at 3 months in the hydrochlorothiazide arm.
The difference in urine output after 24 h was 375 mL greater in the hydrochlorothiazide group (1775 mL vs. 1400 mL; P = 0.05). The difference was statistically significant but is not clinically relevant unless the daily difference accumulated throughout the hospital stay, which might have led to a ~ 2.5 L extra diuresis across a 7-day treatment period. However, these data were not collected.
Perhaps the biggest flaw with the CLOROTIC trial is the modest dose of furosemide used as standard care (median 80 mg per day in each arm). This is less than what was used in the low-dose arm of the DOSE trial [19] and a fraction of what was encouraged in the diuretic arm of the CARESS trial [20]. Despite the lack of robust evidence, thiazide diuretics are recommended for patients with HF, but only when given in addition to loop diuretics in those who are diuretic resistant. [14].
Acetazolamide
Acetazolamide is a carbonic anhydrase (CA) inhibitor. CA catalyses the interconversion between H+ and HCO3− ions on the one hand to H2O and CO2 on the other. Inhibition of CA in the lumen of the proximal convoluted tubule (PCT) increases luminal H+ concentration, which reduces the activity of the Na+-H+ exchanger on the apical membrane. Inhibition of intracellular CA reduces the concentration of intracellular H+ ions, further reducing the activity of the Na+-H+ exchanger. The net effect is an increase in urine sodium concentration which may increase diuresis (Fig. 1) 0.2 [21] There have been three randomised controlled trials assessing the effect of acetazolamide on diuresis in patients admitted to hospital with HF (Table 1), of which the ADVOR trial was the largest. [8, 22, 23].
In the ADVOR trial, 519 patients admitted to the hospital with HF, all of whom were already taking loop diuretics prior to admission, were randomised to 500 mg IV acetazolamide or placebo for 3 days. IV furosemide was given at twice the usual daily oral dose. The primary endpoint was the proportion of patients with successful decongestion (no or only trace ankle oedema) after 72 h.
Patients randomised to acetazolamide were more likely to be decongested by day 3 (42% vs. 31%; hazard ratio (HR) 1.47 (95% confidence interval (CI) 1.17–1.82); P < 0.001). After 2 days of treatment, acetazolamide was associated with a 0.5 L greater diuresis than placebo (4.6 L (± 1.7 l) vs. 4.1 L (± 1.8 L)). Treatment with acetazolamide also shortened the length of admission by 1 day (9 days (95% CI (9–10 days) vs. 10 days (95% CI 9–11 days) admission duration; P < 0.001).
Acetazolamide was well tolerated, and there was no statistical difference in the safety profile compared to placebo. However, there was a trend towards higher rates of renal dysfunction, hypokalaemia, hypotension, and all-cause mortality at 3 months in those who had received acetazolamide.
The mean dose of IV furosemide in the ADVOR trial was 120 mg per day. The effect of acetazolamide on the primary endpoint was driven entirely by those receiving ≤ 120 mg of IV furosemide per day (N = 263; HR 1.78 (95% CI 1.33–2.36)). In patients receiving > 120 mg IV furosemide per day, acetazolamide had no effect on the primary endpoint (N = 252; HR 1.08 (95% CI 0.76–1.55)).
The use of a clinical composite congestion score as a primary endpoint is problematic because it makes it difficult to be sure what actually improved. Only a third of patients initially had oedema above the knee. Many patients with mild oedema (below the knee) can be managed as an out-patient, particularly if the oral dose of loop diuretic is low, as was the case in ADVOR (median 60 mg per day prior to admission).
The trial was designed prior to the introduction of SGLT2I for the management of HF, but SGLT2i have now become an essential treatment for HF. However, acetazolamide and SGLT2I both increase sodium excretion in the proximal convoluted tubule, and therefore, patients taking SGLT2I were excluded from the ADVOR trial. Whether acetazolamide is effective in the presence of an SGLT2i is uncertain.
Sodium-Glucose Co-Transporter 2 Inhibitors
The prognostic benefits of sodium-glucose co-transporter 2 inhibitors (SGLT2I) in patients with HeFREF are well established, [24] with modest benefits in HF hospitalisation also seen in patients with HF and a normal LVEF [25]. SGLT2i may exert their benefit by several mechanisms, but diuresis leading to plasma volume contraction and decongestion certainly occurs [26, 27] and might be useful as an adjunct to diuretic therapy.
Large RCTs of patients with relatively stable HF show inconsistent evidence of a diuretic-sparing effect. In patients with HF and a preserved ejection fraction (HeFPEF), randomisation to SGLT2i was associated with a lower rate of initiation of loop diuretic in patients not receiving loop diuretic at randomisation and a lower rate of diuretic intensification, compared to placebo. [28, 29] However, in patients with HF and a reduced ejection fraction (HeFREF), neither the use of loop diuretics nor the mean dose of loop diuretic differed between SGLT2I and placebo groups. [30].
Data from trials of hospitalised with HF are more convincing; the EMPAG-HF, EMPA-RESPONSE-AHF, and EMPULSE (empagliflozin) trials all reported a small, but statistically significant, increase in urine output compared to placebo (Table 2)0.9, [31, 32]
The DAPA-RESIST trial (N = 61) compared dapagliflozin to metolazone for overcoming diuretic resistance (defined as < 1 kg weight loss or < 1 L net fluid loss in the preceding 24 h despite high dose loop diuretic (≥ 160 mg per day furosemide equivalents)) in patients admitted with HF [33]. Although patients assigned to metolazone received lower concomitant doses of IV furosemide (presumably reflecting less perceived need) and a trend to greater weight loss, the resolution of congestion was similar for each agent. However, metolazone induced more hyponatraemia and a greater increase in urea and creatinine.
In summary, it appears safe to start an SGLT2I in patients who are congested, and the addition of an SGLT2i may enhance a furosemide-induced diuresis, although the effect may be smaller than for metolazone.
Tolvaptan
Tolvaptan is a selective arginine vasopressin (AVP) V2 receptor antagonist. The AVP V2 receptor is found on the basolateral membrane of cells in the collecting duct of the renal tubule. Activation of AVP V2 increases synthesis of aquaporin-2 channels which increase water reabsorption. Blocking the receptor increases free water excretion [34]. There have been four multi-centre RCTs of arginine vasopressin (AVP) antagonists in patients admitted with HF: EVEREST, [35] TACTICS[36], SECRETs of CHF [10], and the 3T trial. [37].
In the EVEREST trial, patients admitted to hospital with HF were randomised to either tolvaptan 30 mg per day or placebo. There are two aspects to the trial: one focussing on diuretic- and symptom-related endpoints after 7 days of treatment; the other assessing the effect of tolvaptan on long-term outcomes. There was greater weight loss and improvement in breathlessness and peripheral oedema with tolvaptan compared to placebo in the first 7 days but no effect on patient-reported global symptom assessment [38]. Patients assigned to tolvaptan were discharged on lower doses of loop diuretics. However, tolvaptan causes thirst which may have led to a substantial discontinuation rate. In the long term, there was no reduction in cardiovascular hospitalisations or mortality.
In the TACTICS trial, patients admitted with HF were randomised to either tolvaptan 30 mg per day for two days or matching placebo in addition to a fixed dose of IV furosemide (mean dose 71 mg per day). The primary endpoint was the proportion of patients achieving a “moderate” improvement in patient-reported breathlessness at 8 and 24 h after starting treatment. Tolvaptan had no impact on the primary endpoint compared to placebo but was associated with greater weight loss (− 2.8 kg vs. − 1.6 kg; P = 0.004) and water loss (− 1948 mL vs. − 1419 mL; P = 0.01) in the first 48 h. Differences between the two groups were lost after tolvaptan was stopped. [37].
In the SECRETs of the CHF trial, patients admitted to the hospital with HF who either had renal impairment (eGFR < 60 ml/min/1.73 m2), hyponatraemia (≤ 134 mmol/L), or diuretic resistance were randomised to either tolvaptan 30 mg/day vs. matching placebo for 7 days in addition to IV furosemide. The primary endpoint was an improvement in patient-assessed breathlessness after 24 h. As with EVEREST and TACTICS, tolvaptan had no effect on symptoms but was associated with greater weight loss compared to treatment with furosemide alone after 3 days. [10].
The 3T trial was a three-way comparison between tolvaptan, IV chlorothiazide, and oral metolazone in patients admitted with HF who had diuretic resistance defined as urine output < 2.0L in the 12 h before enrolment despite receiving ≥ 240 mg of IV furosemide. Patients were randomised in a 1:1:1 ratio to either tolvaptan 30 mg OD, metolazone 5 mg OD, or chlorothiazide 500 mg twice daily (BD) for 48 h. High doses of IV furosemide were used: 100 mg bolus followed by an infusion of 20 to 30 mg per hour. The primary endpoint was change in weight from baseline to 48 h, and secondary endpoints included urine output and change in patient-reported congestion. [38].
The use of different time periods to measure urine output, and increased doses of loop diuretic, make estimating the diuretic effect of each intervention in the 3T trial difficult. At 48 h, urine output was 7780 mL, 8770 mL, and 9790 mL in the metolazone, chlorothiazide, and tolvaptan arms, respectively, compared to 1170 mL, 1372 mL, and 1022, respectively, in the 12 h prior to randomisation. Cumulative loop diuretic dose was 770 mg, 675 mg, and 770 mg per day, respectively, in the metolazone, chlorothiazide, and tolvaptan compared to 680 mg, 611 mg, and 546 mg per day prior to randomisation.
If urine output was consistent over the 12 h before and 48 h after randomisation, then the greatest increase in daily urine output was in the tolvaptan arm (2044 mL in 24 h prior to randomisation vs. 4895 mL in 24 h after randomisation). However, patients in the tolvaptan arm also had the largest increase in daily loop diuretic dose (546 mg per day before randomisation to 770 mg per day after randomisation. [38].
Tolvaptan may be a useful adjunct to diuretic therapy in patients with diuretic resistance but has no more of a diuretic effect than either IV or oral thiazide diuretics in that circumstance. At present, they are only “suggested” for the treatment of resistant hyponatraemia in the context of congestion. However, the effect of tolvaptan in patients with congestion and hyponatraemia can only be estimated from sub-group analysis of the EVEREST or SECRET of CHF trials—a definitive trial has not been done.
Digoxin
Digoxin is an antagonist of the Na+-K+-ATPase pump which is found on the membrane of all human cells. It removes intracellular Na+ ions in exchange for K+ ions. Na+-K+-ATPase is found on renal tubular cells throughout the nephron [39]. Inhibition of renal Na+-K+-ATPase reduces sodium reabsorption, thus reducing renin secretion via tubuloglomerular feedback, [40, 41] which may have natriuretic and diuretic effects in patients with HF. Other cardiotonic steroids, such as ouabain, increase natriuresis and diuresis in animal models. [42].
RCTs of digoxin withdrawal in patients with stable HF conducted more than 20 years ago, long before beta-blockers, MRA, ARNI, or SGLT2i became established, suggested that digoxin might increase systolic blood pressure (~ 5 mmHg) and LVEF (~ 4%), reduce heart rate (~ 10 bpm) and weight (~ 1 kg), and improve renal function. [43,44,45] Subsequently, a large, long-term RCT found that digoxin reduced heart failure-related hospitalisations and deaths but increased the rate of sudden death, leaving overall mortality unaffected.
However, reductions in HF-related and all-cause hospitalisations appeared substantial for patients with more advanced diseases [46]. Altogether, these data suggest that digoxin could have a role in enhancing diuresis and treating congestion. MRA (by preventing hypokalaemia) and beta-blockers might reduce the risk of sudden death, rendering digoxin safer and more effective in the modern era. Alternatively, digoxin might add little to contemporary treatments for HF. Whether digoxin can enhance a furosemide-induced diuresis for patients receiving contemporary therapy for HF is untested.
Steroid
Prolonged steroid use or high endogenous steroid production is associated with hypertension and an increased risk of cardiovascular disease [47]. Consequently, systemic corticosteroids are considered unsafe in patients with HF [48]. However, several studies suggest that systemic steroids can increase diuresis via activation of glucocorticoid receptors (GR) leading to increases in atrial natriuretic peptide secretion (ANP) and renal blood flow (Fig. 2):
-
In a cross-over trial of patients with Addison’s disease (N = 7), administration of dexamethasone increased circulating ANP concentration and increased diuresis and sodium excretion compared to glucocorticoid withdrawal. [49]
-
In animal studies, activation of GR increases secretion of ANP [50] and expression of natriuretic peptide receptors (NPR-A) in the distal part of the collecting duct (the inner medullary collecting duct (IMCD)), [51] the pulmonary artery [52], and hypothalamus [53]. Activation of NPR-A
-
In animal studies, activation of GR causes renal vasodilation [57] and increases renal blood flow, [58] via increased nitric oxide and prostaglandin synthesis. [59, 60] The mechanism appears independent of the action of angiotensin II [60] and is limited to the renal vasculature (i.e., not in mesenteric, iliac, or coronary arteries)0.6 [61]
-
In animal studies, activation of GR also increases renal dopamine excretion in addition to increased renal blood flow and increased sodium excretion. [62]
In patients with HF, observational data suggest that the addition of steroids to high-dose IV diuretics increases diuresis, [63,64,65] and in RCTs, steroids are associated with increased diuresis, improved renal function, and, possibly, improved outcome in hospitalised patients with HF [66, 67] and in ambulatory out-patients (Table 3)0.6 [68].
Oral steroids are not currently recommended for the treatment of HF, although they may be used for co-morbid conditions such as an exacerbation of COPD. Prednisolone and dexamethasone are widely used, but dexamethasone may be more appropriate for patients with HF as it has little to no effect on mineralocorticoid receptors [69]. More research is required to clarify the safety and efficacy of oral steroids as an adjuvant to diuretic therapy in patients with HF.
Salt Supplements and Hypertonic Saline
The ESC HF guidelines recommend limiting daily salt intake to < 5 g [70]. However, salt restriction is associated with greater neurohormonal activation, [71] and an observational study suggested it may be associated with an increased risk of HF hospitalisation [72]. An RCT comparing salt-restricted diet (< 1.5 g per day) to standard care in ambulatory out-patients with HF found no difference in morbidity or mortality [73]. An RCT of salt and water restriction in patients hospitalised with worsening HF suggested that it did not improve control of congestion but increased thirst. [74].
Meta-analysis of a series of small trials suggests that infusing hypertonic saline (HS) with high-dose IV furosemide increases diuresis, shortens hospital stay, and reduces HF re-admissions [75]. The mechanism of benefit of HS is not well understood: increased renal blood flow, [76] increased cardiac output, [77, 78] and reduced neurohormonal activation [79] are all putative mechanisms. The diuretic effect may simply be due to increased natriuresis in response to an increase in serum sodium concentration. [80].
In the largest RCT of hypertonic saline to date, 1927 patients admitted to the hospital with HF and low urine output (< 0.8 L per day) despite high dose oral loop diuretic were randomised to hypertonic saline (1.4–4.6% depending on serum sodium concentrations) plus 250 mg IV furosemide BD or 250 mg IV furosemide BD alone. At discharge, patients randomised to the HS arm were encouraged to take a liberal salt diet (120 mmol per day), and those in the loop diuretic-only arm were encouraged to take a restricted salt diet (80 mmol per day). The primary endpoint was death or HF hospitalisation, and secondary endpoints included daily diuresis, as well as change in body weight and renal function from randomisation to discharge. HS was associated with shorter length of stay (3.5 vs. 5.5 days), greater diuresis (2150 mL vs. 1675 mL per day), greater reduction in body weight from admission to discharge (9.5 kg vs. 7.9 kg), and an improvement in renal function. Median follow-up was 57 months during which time 12.9% died and 18.5% were re-admitted for those assigned to HS, compared to 23.8% and 34.2% in the control group [11•]. Concerns around data veracity have limited adoption in guidelines. [81, 82].
Regardless of the supporting data, widespread use of HS in patients admitted to hospital with HF is logistically difficult. HS can cause phlebitis, and a rapid increase in serum sodium concentration can cause osmotic demyelination syndrome leading to irreversible neurological damage. As a result, HS infusions are often given via a central vein and under close monitoring in high-dependency or intensive care units [83]. Although some studies suggest that peripheral administration of HS is safe, [84] it is not a routine practice.
Oral sodium chloride (Slow-Sodium®) in doses of up to 12 g per day (20 tablets) may be a pragmatic alternative to IV HS. The OSPREY trial included 65 patients admitted to the hospital with HF (mean age 70; mean LVEF 45%; median NTproBNP 4040 ng/L; mean eGFR 39 ml/min/1.73 m2) all of whom were taking high-dose oral loop diuretic prior to hospitalisation (mean furosemide-equivalent of 770 mg per day). Patients were randomised to 6 g of oral salt per day or placebo for 4 days. Oral salt had no effect on change in body weight or renal function (primary endpoints). The median dose of diuretic was 460 mg per day in the oral salt arm and 405 mg per day in the placebo arm, and total urine output over 4 days was numerically (but not statistically) greater in the oral salt arm (10.0 L vs. 9.4 L; P = 0.61). Oral salt was associated with a smaller reduction in serum sodium concentration (− 0.03 mEq/L vs. − 2.60 mEq/L; P < 0.001) and a smaller increase in serum urea (3.1 mEq/L vs. 11.0 mEq/L; P = 0.025) compared to placebo. Oral salt was well tolerated with no serious adverse events related to treatment reported. [12].
It may be that the dose of oral salt given was too low, or that gastrointestinal absorption of salt was impaired by gut wall oedema. Although the dose and route of administration were sufficient to affect serum sodium concentration, this had no effect on diuresis. While HS or oral salt supplements might be beneficial, the former is logistically challenging, and robust evidence for the latter is lacking.
Directions for Research
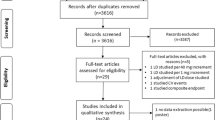
Almost all trials of combination diuretic therapy to date have been head-to-head comparisons. These suggest that any combination might enhance a furosemide-induced diuresis (Fig. 3). Comparisons between the trials are nearly impossible due to the heterogeneity in loop diuretic dosing, administration, and reporting; duration of the intervention(s); and primary and secondary endpoints (Table 4).
Cumulative urine output in RCTs of combination diuretic therapy. Urine output was reported at 24 h in the CLOROTIC and SMAC-HF trials and was used to estimate urine output at 48 and 72 h; urine output was reported at 72 h in the DOSE and TACTICS trials and used to estimate urine output at 24 and 48 h. Urine output from the ADVOR, EMPA-RESPONSE-AHF, EMPAG-HF, OSPREY, and Liu et al. trials was estimated from the figures. Data collection on urine output stopped after 48 h in the ADVOR trial; 72 h urine output is estimated from values at 24 and 48 h. Abbreviations: plbo, placebo; HCTZ, hydrochlorothiazide; ACZ, acetazolamide; Empa, empagliflozin; NaCl, slow sodium; Tolv, tolvaptan; Pred, prednisolone; HSS, hypertonic saline solution
Loop diuretic monotherapy has been the foundation of diuretic therapy for decades. DOSE and PUSH-AHF have demonstrated that high-dose furosemide is safe and more effective than lower doses. While there are several possible adjunctive therapies, most are reserved for patients with diuretic resistance in clinical practice, and none has robust data to support their use. Trials of IV furosemide plus adjunctive therapy compared to high-dose IV furosemide alone, initiated early after admission for patients with evidence of gross water retention and congestion, are needed.
However, such a trial will be difficult to design and perform.
-
There is wide variation in IV furosemide dosing and little agreement on whether continuous or bolus dosing should be standard practice.
-
Duration of treatment is uncertain. Almost all trials of acute diuretic strategies (apart from those using SGLT2I) have treated patients for only 2–5 days. Unsurprisingly, none has shown an effect on medium- to long-term outcomes.
-
There are no data to guide recommendations on the optimal dose of oral loop diuretic to prescribe at the point of discharge, although there is a general consensus that it should be greater than the dose the patient was taking on admission to the hospital [85]. Better in-patient diuresis might lead to under-dosing at discharge.
-
Guidelines recommend that patients should be euvolaemic at discharge, [14] and the rationale for oral diuretic on discharge is to prevent recurrence of congestion. However, many patients leave the hospital with residual signs of congestion, [86] and those who do are at greater risk of adverse outcomes. [87, 88] Sub-clinical venous congestion (detected on ultrasound) is common in patients with HF and is associated with a higher risk of adverse outcome [89]. Inadequate dosing of oral diuretic at discharge may lead to worsening symptoms of HF and, potentially, re-admission.
-
Up to 25% of patients admitted to the hospital with HF who survive to discharge will be readmitted within 30 days, the majority due to HF, renal dysfunction, or respiratory tract infection [90]. Pulmonary congestion can increase the risk of lower respiratory tract infection, and treatment with diuretic can reduce the risk of LRTI in patients with HF. [91, 92] Maintaining adjunctive therapy to diuretic therapy on discharge, at least for a few weeks, might reduce the risk of worsening HF symptoms, readmission, and death.
There is no agreed core outcome set (COS) for patients admitted to the hospital with HF. By contrast, there is a well-defined COS for research and clinical practice in out-patients with chronic HF, which includes symptoms, quality of life, exercise capacity, hospitalisations, and mortality. [93, 94
Achieving decongestion during admission and being “alive and well” at a specific time point after discharge are important outcomes for patients and clinicians. This may be achievable in a large pragmatic trial of adjuncts to diuretic therapy using a combination of established diuresis and decongestion endpoints at the point of discharge and a combination of hospitalisation and mortality endpoints and QoL measured by the KCCQ.
Summary and Conclusion
There are several interventions that might be adjuncts to loop diuretic therapy. However, there is little agreement on how loop diuretic should be used in patients with severe fluid retention, let alone which adjunct to use and when to use it. Until trials are designed that compare different types of combination therapy with high-dose IV loop diuretic in the acute phase followed by effective maintenance therapy post-discharge, the evidence for combination diuretic therapy will remain flimsy.
References
Yeoh SE, Osmanska J, Petrie MC, et al. Dapagliflozin vs. metolazone in heart failure resistant to loop diuretics. Eur Heart J. 2023;44(31):2966–77. https://doi.org/10.1093/eurheartj/ehad341. DAPA-RESIST trial comparing dapagliflozin to metolazone in patients treated with high dose IV loop diuretics with diuretic resistance
Doggrell SA. Tolvaptan (Otsuka). Curr Opin Investig Drugs. 2004;5(9):977–83.
Gheorghiade M, Konstam MA, Burnett JC Jr, Grinfeld L, Maggioni AP, Swedberg K, Udelson JE, Zannad F, Cook T, Ouyang J, Zimmer C, Orlandi C. Efficacy of vasopressin antagonism in heart failure outcome study with tolvaptan (EVEREST) investigators. Short-term clinical effects of tolvaptan, an oral vasopressin antagonist, in patients hospitalized for heart failure: the EVEREST Clinical Status Trials. JAMA. 2007;297(12):1332–43.
Felker GM, Mentz RJ, Cole RT, Adams KF, Egnaczyk GF, Fiuzat M, Patel CB, Echols M, Khouri MG, Tauras JM, Gupta D, Monds P, Roberts R, O’Connor CM. Efficacy and safety of tolvaptan in patients hospitalized with acute heart failure. J Am Coll Cardiol. 2017;69(11):1399–406.
Cox ZL, Hung R, Lenihan DJ, Testani JM. Diuretic strategies for loop diuretic resistance in acute heart failure: the 3T trial. JACC Heart Fail. 2020;8(3):157–68. https://doi.org/10.1016/j.jchf.2019.09.012.
Gheorghiade M, Konstam MA, Burnett JC Jr, et al. Short-term clinical effects of tolvaptan, an oral vasopressin antagonist, in patients hospitalized for heart failure: the EVEREST clinical status trials. JAMA. 2007;297(12):1332–43. https://doi.org/10.1001/jama.297.12.1332.
Katz AI. Renal Na-K-ATPase: its role in tubular sodium and potassium transport. Am J Physiol. 1982;242(3):F207–19.
Torretti J, Hendler E, Weinstein E, Longnecker RE, Epstein FH. Functional significance of Na- K-ATPase in the kidney: effects of ouabain inhibition. Am J Physiol. 1972;222(6):1398–405. https://doi.org/10.1152/ajplegacy.1972.222.6.1398.
Covit AB, Schaer GL, Sealey JE, Laragh JH, Cody RJ. Suppression of the renin-angiotensin system by intravenous digoxin in chronic congestive heart failure. Am J Med. 1983;75(3):445–7. https://doi.org/10.1016/0002-9343(83)90346-7.
Pamnani MB, Chen S, Bryant HJ, et al. Effects of three sodium-potassium adenosine triphosphatase inhibitors. Hypertension. 1991;18(3):316–24.
Uretsky BF, Young JB, Shahidi FE, Yellen LG, Harrison MC, Jolly MK. Randomized study assessing the effect of digoxin withdrawal in patients with mild to moderate chronic congestive heart failure: results of the PROVED trial. PROVED Investigative Group. J Am Coll Cardiol. 1993;22(4):955–62. https://doi.org/10.1016/0735-1097(93)90403-n.
Packer M, Gheorghiade M, Young JB, et al. Withdrawal of digoxin from patients with chronic heart failure treated with angiotensin-converting-enzyme inhibitors. Radiance Study N Engl J Med. 1993;329(1):1–7. https://doi.org/10.1056/NEJM199307013290101.
Adams KF Jr, Gheorghiade M, Uretsky BF, et al. Patients with mild heart failure worsen during withdrawal from digoxin therapy. J Am Coll Cardiol. 1997;30(1):42–8. https://doi.org/10.1016/s0735-1097(97)00133-2.
Gheorghiade M, Patel K, Filippatos G, et al. Effect of oral digoxin in high-risk heart failure patients: a pre-specified subgroup analysis of the DIG trial. Eur J Heart Fail. 2013;15(5):551–9. https://doi.org/10.1093/eurjhf/hft010.
Walker BR. Glucocorticoids and cardiovascular disease. Eur J Endocrinol. 2007;157:545–59.
National Institute for Health and Care Excellence. British National Formulary. Prednisolone. Available from: https://bnf.nice.org.uk/drugs/prednisolone
Damjancic P, Vierhapper H. Permissive action of glucocorticoid substitution therapy on the effects of atrial natriuretic peptide (hANP) in patients with adrenocortical insufficiency. Exp Clin Endocrinol. 1990;95(3):315–21.
Garcia R, Debinski W, Gutkowska J, et al. Gluco- and mineralocorticoids may regulate the natriuretic effect and the synthesis and release of atrial natriuretic factor by the rat atria in vivo. Biochem Biophys Res Commun. 1985;131(2):806–14.
Liu C, Chen Y, Kang Y, et al. Glucocorticoids improve renal responsiveness to atrial natriuretic peptide by up-regulating natriuretic peptide receptor-A expression in the renal inner medullary collecting duct in decompensated heart failure. J Pharmacol Exp Ther. 2011;339(1):203–9.
Lanier-Smith KL, Currie MG. Effect of glucocorticoids on the binding of atrial natriuretic peptide to endothelial cells. Eur J Pharmacol. 1990;178(1):105–9.
Liu C, Guan J, Kang Y, et al. Inhibition of dehydration-induced water intake by glucocorticoids is associated with activation of hypothalamic natriuretic peptide receptor-A in rat. PLoS ONE. 2010;5(12):e15607.
Genest J, Cantin M. Atrial natriuretic factor. Circulation. 1987;75(1 Pt 2):I118–24.
Gutkowska J, Antunes-Rodrigues J, McCann SM. Atrial natriuretic peptide in brain and pituitary gland. Physiol Rev. 1997;77(2):465–515.
Brown RD, Strott CA, Liddle GW. Site of stimulation of aldosterone biosynthesis by angiotensin and potassium. J Clin Invest. 1972;51(6):1413–8. https://doi.org/10.1172/JCI106937.
Baylis C, Brenner BM. Mechanism of the glucocorticoid-induced increase in glomerular filtration rate. Am J Physiol. 1978;234(2):F166–70.
Baylis C, Handa RK, Sorkin M. Glucocorticoids and control of glomerular filtration rate. Semin Nephrol. 1990;10(4):320–9.
de Matteo R, May CN. Inhibition of prostaglandin and nitric oxide synthesis prevents cortisol-induced renal vasodilatation in sheep. Am J Physiol. 1999;276(4):R1125–31.
De Matteo R, May CN. Glucocorticoid-induced renal vasodilatation is mediated by a direct renal action involving nitric oxide. Am J Physiol. 1997;273(6):R1972–9.
Bednarik JA, May CN. Differential regional hemodynamic effects of corticotropin in conscious sheep. Hypertension. 1994;24(1):49–55.
Aguirre JA, Ibarra FR, Barontini M, Arrizurieta EE, Armando I. Effect of glucocorticoids on renal dopamine production. Eur J Pharmacol. 1999;370(3):271–8.
Massari F, Mastropasqua F, Iacoviello M, Nuzzolese V, Torres D, Parrinello G. The glucocorticoid in acute decompensated heart failure: Dr Jekyll or Mr Hyde?. Am J Emerg Med. 2012;30(3). https://doi.org/10.1016/j.ajem.2011.01.023
Liu C, Liu G, Zhou C, Ji Z, Zhen Y, Liu K. Potent diuretic effects of prednisone in heart failure patients with refractory diuretic resistance. Can J Cardiol. 2007;23(11):865–8.
Zhang H, Liu C, Ji Z, et al. Prednisone adding to usual care treatment for refractory decompensated congestive heart failure. Int Heart J. 2008;49(5):587–95.
Liu C, Chen H, Zhou C, et al. Potent potentiating diuretic effects of prednisone in congestive heart failure. J Cardiovasc Pharmacol. 2006;48(4):173–6.
Liu C, Liu K; COPE-ADHF Study Group. Cardiac outcome prevention effectiveness of glucocorticoids in acute decompensated heart failure: COPE-ADHF study. J Cardiovasc Pharmacol. 2014;63(4):333–8.
Liu C, Zhao Q, Zhen Y, et al. Prednisone in uric acid lowering in symptomatic heart failure patients with hyperuricemia (PUSH-PATH) study. Can J Cardiol. 2013;29(9):1048–54. https://doi.org/10.1016/j.cjca.2012.11.008.
Hadoke PW, Iqbal J, Walker BR. Therapeutic manipulation of glucocorticoid metabolism in cardiovascular disease. Br J Pharmacol. 2009;156(5):689–712.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Skibelund AK; ESC Scientific Document Group. focused update of the 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2023;25:195. https://doi.org/10.1093/eurheartj/ehad195.
Miller WL, Borgeson DD, Grantham JA, Luchner A, Redfield MM, Burnett JC Jr. Dietary sodium modulation of aldosterone activation and renal function during the progression of experimental heart failure. Eur J Heart Fail. 2015;17(2):144–50.
Doukky R, Avery E, Mangla A, et al. Impact of dietary sodium restriction on heart failure outcomes. JACC Heart Fail. 2016;4(1):24–35.
Ezekowitz JA, Colin-Ramirez E, Ross H, et al. Reduction of dietary sodium to less than 100 mmol in heart failure (SODIUM-HF): an international, open-label, randomised, controlled trial [published correction appears in Lancet. Lancet. 2022;399(10333):1391–400.
Aliti GB, Rabelo ER, Clausell N, Rohde LE, Biolo A, Beck-da-Silva L. Aggressive fluid and sodium restriction in acute decompensated heart failure: a randomized clinical trial. JAMA Intern Med. 2013;173(12):1058–64.
Gandhi S, Mosleh W, Myers RB. Hypertonic saline with furosemide for the treatment of acute congestive heart failure: a systematic review and meta-analysis. Int J Cardiol. 2014;173(2):139–45.
Maleki M, Nematbakhsh M. Renal blood flow response to angiotensin 1–7 versus hypertonic sodium chloride 7.5% administration after acute hemorrhagic shock in rats. Int J Vasc Med. 2016;2016:6562017.
Kien ND, Reitan JA, White DA, Wu CH, Eisele JH. Cardiac contractility and blood flow distribution following resuscitation with 7.5% hypertonic saline in anesthetized dogs. Circ Shock. 1991;35(2):109–16.
Sirieix D, Hongnat JM, Delayance S, et al. Comparison of the acute hemodynamic effects of hypertonic or colloid infusions immediately after mitral valve repair. Crit Care Med. 1999;27(10):2159–65. https://doi.org/10.1097/00003246-199910000-00014.
Vaklotton MB, Davison JM, Riondel AM, Lindheimer MD. Response of the renin-aldosterone system and antidiuretic hormone to oral water loading and hypertonic saline infusion during and after pregnancy. Clin Exp Hypertens B. 1982;1(2–3):385–400.
Paterna S, Di Pasquale P, Parrinello G, et al. Changes in brain natriuretic peptide levels and bioelectrical impedance measurements after treatment with high-dose furosemide and hypertonic saline solution versus high-dose furosemide alone in refractory congestive heart failure: a double-blind study. J Am Coll Cardiol. 2005;45(12):1997–2003. https://doi.org/10.1016/j.jacc.2005.01.059.
DiNicolantonio JJ, Di Pasquale P, Taylor RS, Hackam DG. Heart. Retraction. Low sodium versus normal sodium diets in systolic heart failure: systematic review and meta-analysis. Heart. Published Online First: 21 August 2012. 2023; https://doi.org/10.1136/heartjnl-2012-302337
Francis GS. Notice of concern. J Card Fail. 2013;19(7):523. https://doi.org/10.1016/j.cardfail.2013.05.015.
Griffin M, Soufer A, Goljo E, et al. Real world use of hypertonic saline in refractory acute decompensated heart failure: A U.S. Center’s Experience. JACC Heart Fail. 2020;8(3):199–208. https://doi.org/10.1016/j.jchf.2019.10.012.
Madieh J, Hasan B, Khamayseh I, et al. The safety of intravenous peripheral administration of 3% hypertonic saline: a systematic review and meta-analysis. Am J Med Sci. 2023;366(2):135–42.
National Institute for Health and Care Excellence. Acute heart hailure: diagnosis and management. Clinical guideline [CG187]. November 2021. Available from: https://www.nice.org.uk/guidance/cg187 [accessed 1/7/2022]
Chioncel O, Mebazaa A, Harjola VP, Coats AJ, Piepoli MF, Crespo-Leiro MG, et al. ESC heart failure long-term registry investigators. Clinical phenotypes and outcome of patients hospitalized for acute heart failure: the ESC heart failure long-term registry. Eur J Heart Fail. 2017;19:1242–54.
Chioncel O, Mebazaa A, Maggioni AP, Harjola VP, Rosano G, Laroche C, et al. ESC-EORP-HFA heart failure long-term registry investigators. Acute heart failure congestion and perfusion status – impact of the clinical classification on in-hospital and long-term outcomes; insights from the ESC-EORP-HFA Heart Failure Long-Term Registry. Eur J Heart Fail. 2019;21:1338–52.
Rubio-Gracia J, Demissei BG, Ter Maaten JM, et al. Prevalence, predictors and clinical outcome of residual congestion in acute decompensated heart failure. Int J Cardiol. 2018;258:185–91.
Pellicori P, Shah P, Cuthbert J, et al. Prevalence, pattern and clinical relevance of ultrasound indices of congestion in outpatients with heart failure. Eur J Heart Fail. 2019;21(7):904–16.
Bottle A, Aylin P, Bell D. Effect of the readmission primary diagnosis and time interval in heart failure patients: analysis of English administrative data. Eur J Heart Fail. 2014;16(8):846–53. https://doi.org/10.1002/ejhf.129.
Krahnke JS, Abraham WT, Adamson PB, et al. Heart failure and respiratory hospitalizations are reduced in patients with heart failure and chronic obstructive pulmonary disease with the use of an implantable pulmonary artery pressure monitoring device. J Card Fail. 2015;21(3):240–9. https://doi.org/10.1016/j.cardfail.2014.12.008.
Mor A, Thomsen RW, Ulrichsen SP, Sørensen HT. Chronic heart failure and risk of hospitalization with pneumonia: a population-based study. Eur J Intern Med. 2013;24(4):349–53.
Zannad F, Garcia AA, Anker SD, Armstrong PW, Calvo G, Cleland JG, et al. Clinical outcome endpoints in heart failure trials: a European Society of Cardiology Heart Failure Association consensus document. Eur J Heart Fail. 2013;15:1082–94.
Burns DJP, Arora J, Okunade O, Beltrame JF, Bernardez-Pereira S, Crespo-Leiro MG, et al. International consortium for health outcomes measurement (ICHOM): standardized patient-centered outcomes measurement set for heart failure patients. JACC Heart Fail. 2020;8:212–22. https://doi.org/10.1016/j.jchf.2019.09.007. Important consensus document on patient related outcome measures in clinical trials of acute heart failure
Papers of particular interest, published recently, have been highlighted as: • Of importance
Shoaib A, Mamas MA, Ahmad QS, et al. Characteristics and outcome of acute heart failure patients according to the severity of peripheral oedema. Int J Cardiol. 2019;285:40–6. https://doi.org/10.1016/j.ijcard.2019.03.020.
Shoaib A, Waleed M, Khan S, et al. Breathlessness at rest is not the dominant presentation of patients admitted with heart failure. Eur J Heart Fail. 2014;16(12):1283–91. https://doi.org/10.1002/ejhf.153.
Stokes W. A new effective diuretic - Lasix. Br Med J. 1964;2(5414):910–4.
Trullàs JC, Casado J, Morales-Rull JL, Formiga F, Conde-Martel A, Quirós R, Epelde F, González-Franco Á, Manzano L, Montero-Pérez-Barquero M. Prevalence and outcome of diuretic resistance in heart failure. Intern Emerg Med. 2019;14(4):529–37. https://doi.org/10.1007/s11739-018-02019-7.
Neuberg GW, Miller AB, O’Connor CM, Belkin RN, Carson PE, Cropp AB, Frid DJ, Nye RG, Pressler ML, Wertheimer JH, Packer M. PRAISE Investigators. Prospective randomized amlodipine survival evaluation. Diuretic resistance predicts mortality in patients with advanced heart failure. Am Heart J. 2002;144(1):31–8. https://doi.org/10.1067/mhj.2002.123144.
Trulls JC, Morales-Rull JL, Casado J, et al. Combining loop with thiazide diuretics for decompensated heart failure: the CLOROTIC trial. Eur Heart J. 2023;44(5):411–21. RCT of hydrochlorothiazide in patients hospitalised with heart failure
Mullens W, Dauw J, Martens P, et al. Acetazolamide in acute decompensated heart failure with volume overload. N Engl J Med. 2022. https://doi.org/10.1056/NEJMoa2203094. RCT of acetazolamide in patients hospitalised with heart failure
Damman K, Beusekamp JC, Boorsma EM, et al. Randomized, double-blind, placebo-controlled, multicentre pilot study on the effects of empagliflozin on clinical outcomes in patients with acute decompensated heart failure (EMPA-RESPONSE-AHF). Eur J Heart Fail. 2020;22(4):713–22.
Konstam MA, Kiernan M, Chandler A, Dhingra R, Mody FV, Eisen H, Haught WH, Wagoner L, Gupta D, Patten R, Gordon P, Korr K, Fileccia R, Pressler SJ, Gregory D, Wedge P, Dowling D, Romeling M, Konstam JM, Massaro JM, Udelson JE. SECRET of CHF Investigators, Coordinators, and Committee Members. Short-term effects of tolvaptan in patients with acute heart failure and volume overload. J Am Coll Cardiol. 2017;69(11):1409–19.
Paterna S, Fasullo S, Parrinello G, et al. Short-term effects of hypertonic saline solution in acute heart failure and long-term effects of a moderate sodium restriction in patients with compensated heart failure with New York Heart Association class III (Class C) (SMAC-HF Study). Am J Med Sci. 2011;342(1):27–37.
Montgomery RA, Mauch J, Sankar P, et al. Oral sodium to preserve renal efficiency in acute heart failure: a randomized, placebo-controlled, double-blind study [published online ahead of print. J Card Fail. 2023;S1071–9164(23)00111–2 (RCT of oral salt supplements in patients admitted to hospital with heart failure)
Butler J, Anstrom KJ, Felker GM, et al. Efficacy and safety of spironolactone in acute heart failure: the ATHENA-HF randomized clinical trial. JAMA Cardiol. 2017;2(9):950–8. https://doi.org/10.1001/jamacardio.2017.2198.
McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure [published correction appears in Eur Heart. J Eur Heart J. 2021;42(36):3599–726.
National Institute for Cardiovascular Outcomes Research. National Heart Failure Audit. 2022 summary report. Available from: https://www.nicor.org.uk/wp-content/uploads/2023/10/10633-NICOR-Annual-Summary_Reports_NHFA_v5.AC_.pdf. Accessed 22 Sep 2023.
Bromage DI, Cannata A, McDonagh TA. Combination diuretic therapy for acute heart failure: ‘alone we can do so little; together we can do so much.’ Eur J Heart Fail. 2022;24(9):1611–3. https://doi.org/10.1002/ejhf.2634.
McCallum W, Tighiouart H, Testani JM, et al. Rates of reversal of volume overload in hospitalized acute heart failure: association with long-term kidney function. Am J Kidney Dis. 2022;80(1):65–78.
Martens P, Testani J, Damman K. Prevention and treatment of diuretic resistance in acute heart failure: when to use which combination of diuretics? Eur Heart J. 2023;44(31):2978–81. https://doi.org/10.1093/eurheartj/ehad463.
Jentzer JC, DeWald TA, Hernandez AF. Combination of loop diuretics with thiazide-type diuretics in heart failure. J Am Coll Cardiol. 2010;56(19):1527–34.
Felker GM, Lee KL, Bull DA, et al. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med. 2011;364(9):797–805. https://doi.org/10.1056/NEJMoa1005419.
Bart BA, Goldsmith SR, Lee KL, et al. Ultrafiltration in decompensated heart failure with cardiorenal syndrome. N Engl J Med. 2012;367(24):2296–304. https://doi.org/10.1056/NEJMoa1210357.
Cuthbert JJ, Bhandari S, Clark AL. Hypochloraemia in patients with heart failure: causes and consequences. Cardiol Ther. 2020;9(2):333–47.
Imiela T, Budaj A. Acetazolamide as add-on diuretic therapy in exacerbations of chronic heart failure: a pilot study. Clin Drug Investig. 2017;37(12):1175–81. https://doi.org/10.1007/s40261-017-0577-1.
Verbrugge FH, Martens P, Ameloot K, et al. Acetazolamide to increase natriuresis in congestive heart failure at high risk for diuretic resistance. Eur J Heart Fail. 2019;21(11):1415–22. https://doi.org/10.1002/ejhf.1478.
McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381(21):1995–2008. https://doi.org/10.1056/NEJMoa1911303.
Solomon SD, McMurray JJV, Claggett B, et al. Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N Engl J Med. 2022;387(12):1089–98. https://doi.org/10.1056/NEJMoa2206286.
Mordi NA, Mordi IR, Singh JS, McCrimmon RJ, Struthers AD, Lang CC. Renal and cardiovascular effects of SGLT2 inhibition in combination with loop diuretics in patients with type 2 diabetes and chronic heart failure: the RECEDE-CHF trial [published correction appears in Circulation. Circulation. 2020;142(18):1713–24. https://doi.org/10.1161/CIRCULATIONAHA.120.048739.
McMurray J. EMPA-REG - the “diuretic hypothesis.” J Diabetes Complications. 2016;30(1):3–4. https://doi.org/10.1016/j.jdiacomp.2015.10.012.
Packer M, Butler J, Zannad F, et al. Effect of empagliflozin on worsening heart failure events in patients with heart failure and preserved ejection fraction: EMPEROR-preserved trial. Circulation. 2021;144(16):1284–94. https://doi.org/10.1161/CIRCULATIONAHA.121.056824.
Chatur S, Vaduganathan M, Claggett B, et al. Dapagliflozin and diuretic utilization in heart failure with mildly reduced or preserved ejection fraction: the DELIVER trial. Eur Heart J. 2023;44(31):2930–43. https://doi.org/10.1093/eurheartj/ehad283.
Jackson AM, Dewan P, Anand IS, et al. Dapagliflozin and diuretic use in patients with heart failure and reduced ejection fraction in DAPA-HF [published correction appears in Circulation. Circulation. 2020;142(11):1040–54. https://doi.org/10.1161/CIRCULATIONAHA.120.047077.
Schulze PC, Bogoviku J, Westphal J, et al. Effects of early empagliflozin initiation on diuresis and kidney function in patients with acute decompensated heart failure (EMPAG-HF). Circulation. 2022;146(4):289–98. https://doi.org/10.1161/CIRCULATIONAHA.122.059038.
Biegus J, Voors AA, Collins SP, et al. Impact of empagliflozin on decongestion in acute heart failure: the EMPULSE trial. Eur Heart J. 2023;44(1):41–50. https://doi.org/10.1093/eurheartj/ehac530. Empagliflozin in patients admitted to hospital with heart failure
Author information
Authors and Affiliations
Contributions
JJC, JGFC, and ALC wrote the manuscript and prepared the tables and figures.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
J.J, C., J.G.F, C. & A.L, C. Diuretic Treatment in Patients with Heart Failure: Current Evidence and Future Directions—Part II: Combination Therapy. Curr Heart Fail Rep 21, 115–130 (2024). https://doi.org/10.1007/s11897-024-00644-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-024-00644-2