Abstract
Purpose of Review
Understanding barriers to self-management behaviors and glycemic stability may inform specific needs for behavior change in adolescents and young adults with type 1 diabetes (T1D). The current review aims to systematically synthesize the literature on the relationships between executive functioning, self-management, and A1C in adolescents and young adults with T1D. Fifteen studies were retained in the current review. Study quality assessment for the majority of the studies were “Fair” or “Good.”
Recent Findings
This review highlights several advances in research design, including use of longitudinal designs, data from multiple informants, and use of objective measures. Adolescents and young adults reported that more executive functioning weaknesses were related to decreased self-management behaviors and higher A1C.
Summary
The current review demonstrated that self-perceived executive functioning weaknesses negatively impact self-management behaviors and A1C. Future research is needed to determine the utility of objective measures in assessing the relationships between executive functioning, T1D self-management, and A1C.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Pettitt DJ, Talton J, Dabelea D, Divers J, Imperatore G, Lawrence JM, et al. Prevalence of diabetes in US youth in 2009: the SEARCH for diabetes in youth study. Diabetes Care. 2014;37(2):402–8. https://doi.org/10.2337/dc13-1838.
Dabelea D, Rewers A, Stafford JM, Standiford DA, Lawrence JM, Saydah S, et al. Trends in the prevalence of ketoacidosis at diabetes diagnosis: the SEARCH for diabetes in youth study. Pediatrics. 2014;133(4):e938–45. https://doi.org/10.1542/peds.2013-2795.
Mayer-Davis EJ, Lawrence JM, Dabelea D, Divers J, Isom S, Dolan L, et al. Incidence trends of type 1 and type 2 diabetes among youths, 2002–2012. N Engl J Med. 2017;376:1419–29. https://doi.org/10.1056/NEJMoa1610187.
Schilling LS, Grey M, Knafl KA. The concept of self-management of type 1 diabetes in children and adolescents: an evolutionary concept analysis. J Adv Nurs. 2002;37(1):87–99. https://doi.org/10.1046/j.1365-2648.2002.02061.x.
Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–86. https://doi.org/10.1056/NEJM199309303291401.
Clements MA, Foster NC, Maahs DM, Schatz DA, Olson BA, Tsalikian E, et al. Hemoglobin A1c (HbA1c) changes over time among adolescent and young adult participants in the T1D exchange clinic registry. Pediatr Diabetes. 2016;17(5):327–36. https://doi.org/10.1111/pedi.12295.
Foster NC, Beck RW, Miller KM, Clements MA, Rickels MR, DiMeglio LA, et al. State of type 1 diabetes management and outcomes from the T1D Exchange in 2016–2018. Diabetes Technol Ther. 2019;21(2):66–72. https://doi.org/10.1089/dia.2018.0384.
Goran MI, Gower BA. Longitudinal study on pubertal insulin resistance. Diabetes. 2001;50(11):2444–50. https://doi.org/10.2337/diabetes.50.11.2444.
Helgeson VS, Reynolds KA, Siminerio L, Escobar O, Becker D. Parent and adolescent distribution of responsibility for diabetes self-care: links to health outcomes. J Pediatr Psychol. 2008;33(5):497–508. https://doi.org/10.1093/jpepsy/jsm081.
Markowitz JT, Garvey KC, Laffel LMB. Developmental changes in the roles of patients and families in type 1 diabetes management. Curr Diabetes Rev. 2015;11(4):231–8. https://doi.org/10.2174/1573399811666150421114146.
Garvey KC, Wolpert HA. Identifying the unique needs of transition care for young adults with type 1 diabetes. Diabetes Spectrum. 2011;24(1):22–5. https://doi.org/10.2337/diaspect.24.1.22.
Monaghan M, Helgeson V, Wiebe D. Type 1 diabetes in young adulthood. Curr Diabetes Rev. 2015;11(4):239–50. https://doi.org/10.2174/1573399811666150421114957.
Suchy Y. Executive functioning: Overview, assessment, and research issues for non-neuropsychologists. Ann Behav Med. 2009;37(2):106–16. https://doi.org/10.1007/s12160-009-9097-4.
Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A, Wager TD. The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: a latent variable analysis. Cogn Psychol. 2000;41(1):49–100. https://doi.org/10.1006/cogp.1999.0734.
Wiebe DJ, Chow CM, Palmer DL, Butner J, Butler JM, Osborn P, et al. Developmental processes associated with longitudinal declines in parental responsibility and adherence to type 1 diabetes management across adolescence. J Pediatr Psychol. 2014;39(5):532–41. https://doi.org/10.1093/jpepsy/jsu006.
Vloemans AF, Eilander MM, Rotteveel J, Bakker-van Waarde WM, Houdijk EC, Nuboer R, et al. Youth with type 1 diabetes taking responsibility for self-management: the importance of executive functioning in achieving glycemic control: results from the longitudinal DINO study. Diabetes Care. 2019;42(2):225–31. https://doi.org/10.2337/dc18-1143.
Goethals ER, de Wit M, Van Broeck N, Lemiere J, Van Liefferinge D, Böhler S, et al. Child and parental executive functioning in type 1 diabetes: their unique and interactive role toward treatment adherence and glycemic control. Pediatr Diabetes. 2018;19(3):520–6. https://doi.org/10.1111/pedi.12552.
Wasserman RM, Anderson BJ, Schwartz DD. Screening of neurocognitive and executive functioning in children, adolescents, and young adults with type 1 diabetes. Diabetes Spectrum. 2016;29(4):202–10. https://doi.org/10.2337/ds16-0037.
Northam EA, Anderson PJ, Werther GA, Warne GL, Adler RG, Andrewes D. Neuropsychological complications of IDDM in children 2 years after disease onset. Diabetes Care. 1998;21(3):379–84. https://doi.org/10.2337/diacare.21.3.379.
Northam EA, Anderson PJ, Jacobs R, Hughes M, Warne GL, Werther GA. Neuropsychological profiles of children with type 1 diabetes 6 years after disease onset. Diabetes Care. 2001;24(9):1541–6. https://doi.org/10.2337/diacare.24.9.1541.
Mauras N, Mazaika P, Buckingham B, Weinzimer S, White NH, Tsalikian E, et al. Longitudinal assessment of neuroanatomical and cognitive differences in young children with type 1 diabetes: association with hyperglycemia. Diabetes. 2015;64(5):1770–9. https://doi.org/10.2337/db14-1445.
Duke DC, Harris MA. Executive function, adherence, and glycemic control in adolescents with type 1 diabetes: a literature review. Curr Diabetes Rep. 2014;14(10):532. https://doi.org/10.1007/s11892-014-0532-y.
Bagner DM, Williams LB, Geffken GR, Silverstein JH, Storch EA. Type 1 diabetes in youth: the relationship between adherence and executive functioning. Children’s Healthcare. 2007;36(2):169–79. https://doi.org/10.1080/02739610701335001.
McNally K, Rohan J, Pendley JS, Delamater A, Drotar D. Executive functioning, treatment adherence, and glycemic control in children with type 1 diabetes. Diabetes Care. 2010;33(6):1159–62. https://doi.org/10.2337/dc09-2116.
Miller MM, Rohan JM, Delamater A, Shroff-Pendley J, Dolan LM, Reeves G, et al. Changes in executive functioning and self-management in adolescents with type 1 diabetes: a growth curve analysis. J Pediatr Psychol. 2013;38(1):18–29. https://doi.org/10.1093/jpepsy/jss100.
Moher D, Liberati A, Tetzlaff J, Altman DG. Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097.
National Heart, Lung, and Blood Institute. Quality assessment tool for observational cohort and cross-sectional studies. Bethesda: National Institutes of Health, Department of Health and Human Services. 2014
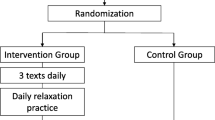
Crochiere RJ, Lansing AH, Carracher A, Stanger C. Executive function and somatic problems in adolescents with above target glycemic control. Pediatr Diabetes. 2019;20(1):119–26. https://doi.org/10.1111/pedi.12789. This recent secondary data analysis demontrates a significant relationship between caregiver report in adolescents' executive functioning and their self-management behaviors. Research results also indicate a significant relationship between caregiver report in self-management and A1C.
Berg CA, Wiebe DJ, Suchy Y, Turner SL, Butner J, Munion A, et al. Executive function predicting longitudinal change in type 1 diabetes management during the transition to emerging adulthood. Diabetes Care. 2018;41(11):2281–8. https://doi.org/10.2337/dc18-0351This study utilizes longitudinal design to assess changes in self-management over time and incorporation of performance-based assessment in executive functioning to evaluate the utility and predictability of this measurement modality in research.
Hamburger ER, Lyttle M, Compas BE, Jaser SS. Performance-based and questionnaire measures of executive function in adolescents with type 1 diabetes. J Behav Med. 2019;42(6):1041–9. https://doi.org/10.1007/s10865-019-00027-2Comparison between the relationships between performance-based assessment and questionnaire measures of executive functioning contributes to preliminary research understanding of the utility of objective measures of executive functioning.
Nylander C, Tindberg Y, Haas J, Swenne I, Torbjörnsdotter T, Åkesson K, et al. Self-and parent-reported executive problems in adolescents with type 1 diabetes are associated with poor metabolic control and low physical activity. Pediatr Diabetes. 2018;19(1):98–105. https://doi.org/10.1111/pedi.12520. Including both adoelscents and young adults, this study demonstrates that individuals with self reported executive functioning weaknesses are three times more likely to experience higher A1C.
Wiebe DJ, Baker AC, Suchy Y, Stump TK, Berg CA. Individual differences and day-to-day fluctuations in goal planning and type 1 diabetes management. Health Psychol. 2018;37(7):638. https://doi.org/10.1037/hea0000624This study incorporates performance-based assessment of executive functioning that contributes to research understanding of the preliminary contribution from this measurement modality.
Perez KM, Patel NJ, Lord JH, Savin KL, Monzon AD, Whittemore R, et al. Executive function in adolescents with type 1 diabetes: relationship to adherence, glycemic control, and psychosocial outcomes. J Pediatr Psychol. 2017;42(6):636–46. https://doi.org/10.1093/jpepsy/jsw093. This recent study incorporates multiple informants in self-management, including self-report, caregiver report, and blood glucose checks.
Suchy Y, Turner SL, Queen TL, Durracio K, Wiebe DJ, Butner J, et al. The relation of questionnaire and performance-based measures of executive functioning with Type 1 diabetes outcomes among late adolescents. Health Psychol. 2016;35(7):661–9. https://doi.org/10.1037/hea0000326.
Berg CA, Wiebe DJ, Suchy Y, Hughes AE, Anderson JH, Godbey EI, et al. Individual differences and day-to-day fluctuations in perceived self-regulation associated with daily adherence in late adolescents with type 1 diabetes. J Pediatr Psychol. 2014;39(9):1038–48. https://doi.org/10.1093/jpepsy/jsu051The study incorporated objective measures of daily glucose checks via meter downloads, which contributes to research understanding of engagement in self-management behaviors beyond self-report in questionnaires.
Duke DC, Raymond JK, Harris MA. The diabetes related executive functioning scale (DREFS): pilot results. Children’s Health Care. 2014;43(4):327–44. https://doi.org/10.1080/02739615.2013.870040.
Smith LB, Kugler BB, Lewin AB, Duke DC, Storch EA, Geffken GR. Executive functioning, parenting stress, and family factors as predictors of diabetes management in pediatric patients with type 1 diabetes using intensive regimens. Children’s Health Care. 2014;43(3):234–52. https://doi.org/10.1080/02739615.2013.839383.
Stupiansky NW, Hanna KM, Slaven JE, Weaver MT, Fortenberry JD. Impulse control, diabetes-specific self-efficacy, and diabetes management among emerging adults with type 1 diabetes. J Pediatr Psychol. 2013;38(3):247–54. https://doi.org/10.1093/jpepsy/jss110.
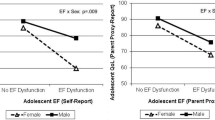
Graziano PA, Geffken GR, Williams LB, Lewin AB, Duke DC, Storch EA, et al. Gender differences in the relationship between parental report of self-regulation skills and adolescents’ management of type 1 diabetes. Pediatr Diabetes. 2011;12(4 pt2):410–8. https://doi.org/10.1111/j.1399-5448.2010.00692.x.
Lin A, Northam EA, Rankins D, Werther GA, Cameron FJ. Neuropsychological profiles of young people with type 1 diabetes 12 yr after disease onset. Pediatr Diabetes. 2010;11(4):235–43. https://doi.org/10.1111/j.1399-5448.2009.00588.x.
Ohmann S, Popow C, Rami B, König M, Blaas S, Fliri C, et al. Cognitive functions and glycemic control in children and adolescents with type 1 diabetes. Psychol Med. 2010;40(1):95–103. https://doi.org/10.1017/S0033291709005777.
Rovet J, Alvarez M. Attentional functioning in children and adolescents with IDDM. Diabetes Care. 1997;20(5):803–10. https://doi.org/10.2337/diacare.20.5.803.
Iannotti RJ, Nansel TR, Schneider S, Haynie DL, Simons-Morton B, Sobel DO, et al. Assessing regimen adherence of adolescents with type 1 diabetes. Diabetes Care. 2006;29(10):2263–7. https://doi.org/10.2337/dc06-0685.
Lewin AB, LaGreca AM, Geffken GR, Williams LB, Duke DC, Storch EA, et al. Validity and reliability of an adolescent and parent rating scale of type 1 diabetes adherence behaviors: the Self-Care Inventory (SCI). J Pediatr Psychol. 2009;34(9):999–1007. https://doi.org/10.1093/jpepsy/jsp032.
Harris MA, Wysocki T, Sadler MI, Wilkinson KA, Harvey LM, Buckloh LM, et al. Validation of a structured interview for the assessment of diabetes self-management. Diabetes Care. 2000;23(9):1301–4. https://doi.org/10.2337/diacare.23.9.1301.
Wysocki T, Buckloh LM, Antal H, Lochrie A, Taylor A. Validation of a self-report version of the diabetes self-management profile. Pediatr Diabetes. 2012;13(5):438–43. https://doi.org/10.1111/j.1399-5448.2011.00823.x.
Gioia GA, Isquith PK, Guy SC, Kenworthy L. BRIEF-2: Behavior rating inventory of executive function. Lutz: Psychological Assessment Resources; 2015.
Delis DC, Kaplan E, Kramer JH. Delis-Kaplan executive function system.
Zelazo PD, Anderson JE, Richler J, Wallner-Allen K, Beaumont JL, Weintraub S II. NIH Toolbox Cognition Battery (CB): Measuring executive function and attention. Monogr Soc Res Child Dev. 2013;78(4):16–33. https://doi.org/10.1111/mono.12032.
Grant DA, Berg EA. Wisconsin Card Sorting Test (WCST).
Rovet J. A parametric measure of reflection-impulsivity. J Appl Dev Psychol. 1980;1(3):221–5. https://doi.org/10.1016/0193-3973(80)90011-8.
Garfinkel BD, Klee SH. A computerized assessment battery for attention deficits. Psychiatr Hosp. 1983;14(3):163–6.
Friedman NP, Miyake A, Corley RP, Young SE, DeFries JC, Hewitt JK. Not all executive functions are related to intelligence. Psychol Sci. 2006;17(2):172–9. https://doi.org/10.1111/j.1467-9280.2006.01681.x.
Ross LA, Frier BM, Kelnar CJ, Deary IJ. Child and parental mental ability and glycaemic control in children with Type 1 diabetes. Diabet Med. 2001;18(5):364–9. https://doi.org/10.1046/j.1464-5491.2001.00468.x.
Murphy KR, Myors B, Wolach A. Statistical power analysis: a simple and general model for traditional and modern hypothesis tests. Routledge; 2014.
Toplak ME, West RF, Stanovich KE. Practitioner review: do performance-based measures and ratings of executive function assess the same construct? J Child Psychol Psychiatry. 2013;54(2):131–43. https://doi.org/10.1111/jcpp.12001.
Miller VA, Jawad AF. Decision-making involvement and prediction of adherence in youth with type 1 diabetes: A cohort sequential study. J Pediatr Psychol. 2019;44(1):61–71. https://doi.org/10.1093/jpepsy/jsy032.
Wiley J, Westbrook M, Greenfield JR, Day RO, Braithwaite J. Shared decision-making: the perspectives of young adults with type 1 diabetes mellitus. Patient Prefer Adherence. 2014;8:423. https://doi.org/10.2147/PPA.S57707.
Reynolds CR, Kamphaus RW. RIAS-2 (Reynolds Intellectual Assessment Scales) and the RIST-2 (Reynolds Intellectual Screening Test). Psychol Assess Resources; 2015.
McCrimmon AW, Smith AD. Review of the Wechsler abbreviated scale of intelligence, (WASI-II). https://doi.org/10.1177/0734282912467756.
American Diabetes Association. 13. Children and adolescents: standards of medical care in diabetes 2020. Diabetes Care. 2020;43(Supplement 1):S163–82. https://doi.org/10.2337/dc20-S013.
Messer LH, Cook PF, Tanenbaum ML, Hanes S, Driscoll KA, Hood KK. CGM benefits and burdens: two brief measures of continuous glucose monitoring. J Diabetes Sci Technol. 2019;13(6):1135–41. https://doi.org/10.1177/1932296819832909.
Farfel A, Liberman A, Yackobovitch-Gavan M, Phillip M, Nimri R. Executive functions and adherence to continuous glucose monitoring in children and adolescents with type 1 diabetes. Diabetes Technol Ther. 2020;22(4):265–70. https://doi.org/10.1089/dia.2019.0341.
Patton SR. Adherence to glycemic monitoring in diabetes. J Diabetes Sci Technol. 2015;9(3):668–75. https://doi.org/10.1177/1932296814567709.
Wasserman RM, Hilliard ME, Schwartz DD, Anderson BJ. Practical strategies to enhance executive functioning and strengthen diabetes management across the lifespan. Curr Diabetes Rep. 2015;15(8):52. https://doi.org/10.1007/s11892-015-0622-5.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Psychosocial Aspects
Rights and permissions
About this article
Cite this article
Ding, K., Reynolds, C.M., Driscoll, K.A. et al. The Relationship Between Executive Functioning, Type 1 Diabetes Self-Management Behaviors, and Glycemic Control in Adolescents and Young Adults. Curr Diab Rep 21, 10 (2021). https://doi.org/10.1007/s11892-021-01379-3
Accepted:
Published:
DOI: https://doi.org/10.1007/s11892-021-01379-3