Abstract
Introduction
There is lack of data on the pharmacodynamics of low-molecular-weight heparins in obese patients.
Background
The aims of this study are to investigate the correlation between anti-factor Xa (anti-Xa) levels and body weight with fixed-dose enoxaparin after bariatric surgery and to investigate the percentage of patients that reach the desired prophylactic range for anti-Xa levels.
Methods
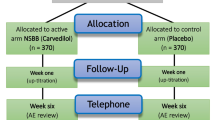
Blood for anti-Xa peak levels measurement was drawn 3–5 h after administration of enoxaparin at the planned visit 8–16 days after surgery. Patients were included in three categories: <110 kg (group 1), 110–150 kg (group 2), and >150 kg (group 3).
Results
Fifty-one patients were included (43.9 ± 9.9 years, 75 % women). Mean anti-Xa level was 0.37 ± 0.14 IU/ml. This level was the highest in group 1 (0.47 ± 0.13 IU/ml) and lowest in group 3 (0.23 ± 0.07). No subprophylactic (<0.2 IU/ml) anti-Xa levels were detected in group 1, whereas this was observed in 38 % in patients in group 3. Supraprophylactic levels (>0.5 IU/ml) were most often present in group 1 (36 %). With multivariable regression analysis, body weight (β −0.720 (95 % confidence interval −.717; −.993), p < 0.001) was an independent predictor of anti-Xa levels, whereas lean body was not independently associated. This was confirmed in a non-linear mixed effects analysis of the data.
Conclusions
Patients with excessive body weight may not be adequately treated with fixed-dose enoxaparin thromboprophylaxis while patients with lower body weight may have an increased bleeding risk. Body weight is a better predictor of anti-Xa levels compared to lean body weight.


Similar content being viewed by others
References
Holst AG, Jensen G, Prescott E. Risk factors for venous thromboembolism: results from the Copenhagen city heart study. Circulation. 2010;121(17):1896–903.
Severinsen MT, Kristensen SR, Johnsen SP, et al. Anthropometry, body fat, and venous thromboembolism: a Danish follow-up study. Circulation. 2009;120(19):1850–7.
Ageno W, Becattini C, Brighton T, et al. Cardiovascular risk factors and venous thromboembolism: a meta-analysis. Circulation. 2008;117(1):93–102.
Sobieraj DM, Coleman CI, Tongbram V, et al. Comparative effectiveness of low-molecular-weight heparins versus other anticoagulants in major orthopedic surgery: a systematic review and meta-analysis. Pharmacotherapy. 2012;32(9):799–808.
Lepic K, Crowther MA. A logical approach to surgical thromboprophylaxis. Curr Opin Hematol. 2009;16(5):397–401.
Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition). Chest. 2008;133(6 Suppl):381S–453S.
Freeman A, Horner T, Pendleton RC, et al. Prospective comparison of three enoxaparin dosing regimens to achieve target anti-factor Xa levels in hospitalized, medically ill patients with extreme obesity. Am J Hematol. 2012;87(7):740–3.
Simone EP, Madan AK, Tichansky DS, et al. Comparison of two low-molecular-weight heparin dosing regimens for patients undergoing laparoscopic bariatric surgery. Surg Endosc. 2008;22(11):2392–5.
Rowan BO, Kuhl DA, Lee MD, et al. Anti-Xa levels in bariatric surgery patients receiving prophylactic enoxaparin. Obes Surg. 2008;18(2):162–6.
Sanderink GJ, Le Liboux A, Jariwala N, et al. The pharmacokinetics and pharmacodynamics of enoxaparin in obese volunteers. Clin Pharmacol Ther. 2002;72(3):308–18.
Gotto Jr AM, Bierman EL, Connor WE, et al. Recommendations for treatment of hyperlipidemia in adults. A joint statement of the Nutrition Committee and the Council on Arteriosclerosis. Circulation. 1984;69(5):1065A–90A.
Schulman S, Angeras U, Bergqvist D, et al. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in surgical patients. J Thromb Haemost. 2010;8(1):202–4.
Janmahasatian S, Duffull SB, Ash S, et al. Quantification of lean bodyweight. Clin Pharmacokinet. 2005;44(10):1051–65.
Salazar DE, Corcoran GB. Predicting creatinine clearance and renal drug clearance in obese patients from estimated fat-free body mass. Am J Med. 1988;84(6):1053–60.
Diepstraten J, Hackeng CM, van Kralingen S, et al. Anti-Xa levels 4 h after subcutaneous administration of 5,700 IU nadroparin strongly correlate with lean body weight in morbidly obese patients. Obes Surg. 2012 Feb 1.
Nutescu EA, Spinler SA, Wittkowsky A, et al. Low-molecular-weight heparins in renal impairment and obesity: available evidence and clinical practice recommendations across medical and surgical settings. Ann Pharmacother. 2009;43(6):1064–83.
Frederiksen SG, Hedenbro JL, Norgren L. Enoxaparin effect depends on body-weight and current doses may be inadequate in obese patients. Br J Surg. 2003;90(5):547–8.
Patel JP, Green B, Patel RK, et al. Population pharmacokinetics of enoxaparin during the antenatal period. Circulation. 2013;128(13):1462–9.
Janmahasatian S, Duffull SB, Chagnac A, et al. Lean body mass normalizes the effect of obesity on renal function. Br J Clin Pharmacol. 2008;65(6):964–5.
Khoursheed M, Al Bader I, Al Asfar F, et al. Therapeutic effect of low-molecular weight heparin and incidence of lower limb deep venous thrombosis and pulmonary embolism after laparoscopic bariatric surgery. Surg Laparosc Endosc Percutan Tech. 2013;23(6):491–3.
Imberti D, Legnani C, Baldini E, et al. Pharmacodynamics of low molecular weight heparin in patients undergoing bariatric surgery: a prospective, randomised study comparing two doses of parnaparin (BAFLUX study). Thromb Res. 2009;124(6):667–71.
Borkgren-Okonek MJ, Hart RW, Pantano JE, et al. Enoxaparin thromboprophylaxis in gastric bypass patients: extended duration, dose stratification, and antifactor Xa activity. Surg Obes Relat Dis. 2008;4(5):625–31.
Heizmann M, Baerlocher GM, Steinmann F, et al. Anti-Xa activity in obese patients after double standard dose of nadroparin for prophylaxis. Thromb Res. 2002;106(4-5):179–81.
Simoneau MD, Vachon A, Picard F. Effect of prophylactic dalteparin on anti-factor Xa levels in morbidly obese patients after bariatric surgery. Obes Surg. 2010;20(4):487–91.
Green B, Duffull SB. Development of a dosing strategy for enoxaparin in obese patients. Br J Clin Pharmacol. 2003;56(1):96–103.
Mayr AJ, Dunser M, Jochberger S, et al. Antifactor Xa activity in intensive care patients receiving thromboembolic prophylaxis with standard doses of enoxaparin. Thromb Res. 2002;105(3):201–4.
Hainer JW, Barrett JS, Assaid CA, et al. Dosing in heavy-weight/obese patients with the LMWH, tinzaparin: a pharmacodynamic study. Thromb Haemost. 2002;87(5):817–23.
Bickford A, Majercik S, Bledsoe J, et al. Weight-based enoxaparin dosing for venous thromboembolism prophylaxis in the obese trauma patient. Am J Surg. 2013;206(6):847–51. discussion.
Ludwig KP, Simons HJ, Mone M, et al. Implementation of an enoxaparin protocol for venous thromboembolism prophylaxis in obese surgical intensive care unit patients. Ann Pharmacother. 2011;45(11):1356–62.
Rondina MT, Wheeler M, Rodgers GM, et al. Weight-based dosing of enoxaparin for VTE prophylaxis in morbidly obese, medically-Ill patients. Thromb Res. 2010;125(3):220–3.
Becattini C, Agnelli G, Manina G, et al. Venous thromboembolism after laparoscopic bariatric surgery for morbid obesity: clinical burden and prevention. Surg Obes Relat Dis. 2012;8(1):108–15.
Brotman DJ, Shihab HM, Prakasa KR, et al. Pharmacologic and mechanical strategies for preventing venous thromboembolism after bariatric surgery: a systematic review and meta-analysis. JAMA Surg. 2013;148(7):675–86.
Bucaloiu ID, Wood GC, Norfolk ER, et al. Fat-free weight prediction in morbidly obese females. Int J Nephrol Renov Dis. 2011;4:149–55.
Yee JY, Duffull SB. The effect of body weight on dalteparin pharmacokinetics. A preliminary study. Eur J Clin Pharmacol. 2000;56(4):293–7.
Chagnac A, Weinstein T, Korzets A, et al. Glomerular hemodynamics in severe obesity. Am J Physiol Ren Physiol. 2000;278(5):F817–22.
Celik F, Bounif F, Fliers JM, et al. The impact of surgical complications as a main risk factor for venous thromboembolism: a multicenter study. Obes Surg. 2014 Apr 5.
Conflict of Interest
The authors (Funda Celik, Alwin D. R. Huitema, Jan H. Hooijberg, Arnold W. J. M. van de Laar, Dees P. M. Brandjes, Victor E. A. Gerdes) certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Statement of Human Rights
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Celik, F., Huitema, A.D.R., Hooijberg, J.H. et al. Fixed-Dose Enoxaparin After Bariatric Surgery: The Influence of Body Weight on Peak Anti-Xa Levels. OBES SURG 25, 628–634 (2015). https://doi.org/10.1007/s11695-014-1435-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1435-3