Abstract
Purpose
Leishmaniasis is a parasitic disease transmitted by the bite of the phlebotomine female sand fly. Currently, no reported effective vaccines are available for the treatment of leishmaniasis; consequently, restricting this disease completely depends on controlling its transmission. Mitogen-activated protein (MAP) kinases have been reported to be involved in the regulation of the flagellum length and hence play an important role in disease transmission, especially the MAPK3 protein. Therefore, the current work focused on identifying approved drugs that can inhibit the MAPK3 protein.
Methods
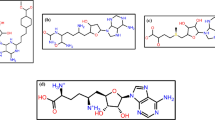
First, the recombinant plasmid (pET28b( +) MAPK3) was cloned into E. coli strain BL21 using the heatshock method. Afterward, E. coli was induced using IPTG, and cells were harvested for protein purification in the next step. After that, the MAPK3 protein was purified using Ni–NTA column. Then, the inhibition kinase activity of the purified MAPK3 protein was performed using an ADP-Glo™ Kinase Assay kit. Furthermore, the cytotoxicity of Leishmania cells were detected by alamarBlue™ Cell Viability Reagent. Finally, the binding affinity within the binding site of MAPK3 protein was performed by computational methods.
Results
Purification of the MAPK3 protein was done using an Ni–NTA column and a protein band was identified at the expected 44 kDa molecular weight. Afterward, the ability of commercial drugs (afatinib and lapatinib) to inhibit the purified MAPK3 kinase activity was performed using an ADP-Glo™ Kinase Assay kit. The half-maximal inhibitory concentrations (IC50) of two drugs inhibited the MAPK3 protein within the same range of IC50 values (3.27 and 2.22 µM for afatinib and lapatinib, respectively). Furthermore, the cytotoxicity assay of compounds toward the extracellular promastigote and intracellular amastigote stages was investigated using alamarBlue™ Cell Viability Reagent. The results showed that both drugs were more efficient against extracellular promastigotes and intracellular amastigotes of both Leishmania donovani and Leishmania martiniquensis. Finally, the molecular dynamics simulation (MD) was performed to study the intermolecular interactions of both drugs with MAPK3 protein. From 100 ns molecular dynamics simulation, the structural stability of both drugs in a complex with MAPK3 was quite stable.
Conclusion
This work was suggesting that afatinib and lapatinib act as MAPK3 inhibitors and might be developed for leishmaniasis treatment.






Similar content being viewed by others
Data Availability
All data and material are included in this article.
References
Torres-Guerrero, E., M.R. Quintanilla-Cedillo, J. Ruiz-Esmenjaud, and R. Arenas (2017) Leishmaniasis: a review. FRes. https://doi.org/10.12688/f1000research.11120.1
Mann S et al (2021) A review of Leishmaniasis: current knowledge and future directions. Curr Trop Med Rep. https://doi.org/10.1007/s40475-021-00232-7
Kedzierski L, Sakthianandeswaren A, Curtis JM, Andrews PC, Junk PC, Kedzierska K (2009) Leishmaniasis: current treatment and prospects for new drugs and vaccines. Curr Med Chem 16(5):599–614. https://doi.org/10.2174/092986709787458489
Lackovic K et al (2010) Inhibitors of Leishmania GDP-mannose pyrophosphorylase identified by high-throughput screening of small-molecule chemical library. Antimicrob Agents Chemother 54(5):1712–1719. https://doi.org/10.1128/AAC.01634-09
Morales MA et al (2008) Phosphoproteomic analysis of Leishmania donovani pro- and amastigote stages. Proteomics 8(2):350–363. https://doi.org/10.1002/pmic.200700697
Tsigankov P, Gherardini PF, Helmer-Citterich M, Spath GF, Myler PJ, Zilberstein D (2014) Regulation dynamics of Leishmania differentiation: deconvoluting signals and identifying phosphorylation trends. Mol Cell Proteomics 13(7):1787–1799. https://doi.org/10.1074/mcp.M114.037705
Tsigankov P, Gherardini PF, Helmer-Citterich M, Späth GF, Zilberstein D (2013) Phosphoproteomic analysis of differentiating leishmania parasites reveals a unique stage-specific phosphorylation motif. J Proteome Res 12(7):3405–3412. https://doi.org/10.1021/pr4002492
Kultz D (1998) Phylogenetic and functional classification of mitogen- and stress-activated protein kinases. J Mol Evol 46(5):571–588. https://doi.org/10.1007/pl00006338
Hindley A, Kolch W (2002) Extracellular signal regulated kinase (ERK)/mitogen activated protein kinase (MAPK)-independent functions of Raf kinases. J Cell Sci 115(Pt 8):1575–1581
Ferrell JE Jr, Bhatt RR (1997) Mechanistic studies of the dual phosphorylation of mitogen-activated protein kinase. J Biol Chem 272(30):19008–19016. https://doi.org/10.1074/jbc.272.30.19008
Efstathiou A, Smirlis D (2021) Leishmania protein kinases: important regulators of the parasite life cycle and molecular targets for treating leishmaniasis. Microorganisms. https://doi.org/10.3390/microorganisms9040691
Aronson N et al (2017) Diagnosis and treatment of Leishmaniasis: clinical practice guidelines by the Infectious Diseases Society of America (idsa) and the American society of tropical medicine and hygiene (ASTMH). Am J Trop Med Hyg 96(1):24–45. https://doi.org/10.4269/ajtmh.16-84256
Cuenda A (2019) Mitogen-Activated Protein Kinases (MAPK) in Cancer. In: Boffetta P, Hainaut P (eds) Encyclopedia of Cancer (Third Edition). Academic Press, Oxford, pp 472–480
Abou-El-Naga IF, Mady RF, N.M. Fawzy Hussien Mogahed, (2020) In vitro effectivity of three approved drugs and their synergistic interaction against Leishmania infantum. Biomedi. https://doi.org/10.7705/biomedica.4891
Raj S, Saha G, Sasidharan S, Dubey VK, Saudagar P (2019) Biochemical characterization and chemical validation of Leishmania MAP Kinase-3 as a potential drug target. Sci Rep 9(1):16209. https://doi.org/10.1038/s41598-019-52774-6
Dichiara M, Marrazzo A, Prezzavento O, Collina S, Rescifina A, Amata E (2017) Repurposing of human kinase inhibitors in neglected protozoan diseases. Chem Med Chem 12(16):1235–1253. https://doi.org/10.1002/cmdc.201700259
Aiebchun T et al (2021) Identification of Vinyl Sulfone Derivatives as EGFR Tyrosine Kinase Inhibitor. Molecules, In Vitro and In Silico Studies. https://doi.org/10.3390/molecules26082211
Sanachai K et al (2021) Discovery of novel JAK2 and EGFR inhibitors from a series of thiazole-based chalcone derivatives. RSC Med Chem. https://doi.org/10.1039/D0MD00436G
Sangpheak K et al (2019) Biological evaluation and molecular dynamics simulation of chalcone derivatives as epidermal growth factor-tyrosine kinase inhibitors. Molecules. https://doi.org/10.3390/molecules24061092
Siripattanapipong S, Boontanom P, Leelayoova S, Mungthin M, Tan-Ariya P (2019) In vitro growth characteristics and morphological differentiation of Leishmania martiniquensis promastigotes in different culture media. Acta Trop 197:105039. https://doi.org/10.1016/j.actatropica.2019.05.030
Intakhan N et al (2020) Antileishmanial activity and synergistic effects of amphotericin B Deoxycholate with Allicin and Andrographolide against Leishmania martiniquensis In Vitro. Pathogens. https://doi.org/10.3390/pathogens9010049
Jones G, Willett P, Glen RC, Leach AR, Taylor R (1997) Development and validation of a genetic algorithm for flexible docking11Edited by F. E. Cohen. J Mol Biol 267(3):727–748. https://doi.org/10.1006/jmbi.1996.0897
Botelho FD et al (2020) Ligand-based virtual screening molecular docking, molecular dynamics, and MM-PBSA calculations towards the identification of potential novel ricin inhibitors. Toxins. https://doi.org/10.3390/toxins12120746
Joshi T et al (2021) Computational investigation of drug bank compounds against 3C-like protease (3CL(pro)) of SARS-CoV-2 using deep learning and molecular dynamics simulation. Mol Divers. https://doi.org/10.1007/s11030-021-10330-3
Kiriwan D, Choowongkomon K (2021) In silico structural elucidation of the rabies RNA-dependent RNA polymerase (RdRp) toward the identification of potential rabies virus inhibitors. J Mol Model 27(6):183. https://doi.org/10.1007/s00894-021-04798-x
Ornnork N, Kiriwan D, Lirdprapamongkol K, Choowongkomon K, Svasti J, Eurtivong C (2020) Molecular dynamics, MM/PBSA and in vitro validation of a novel quinazoline-based EGFR tyrosine kinase inhibitor identified using structure-based in silico screening. J Mole Graph Model 99:107639. https://doi.org/10.1016/j.jmgm.2020.107639
Menezes-Souza D, de Oliveira Mendes TA, de Araujo Leao AC, de Souza Gomes M, Fujiwara RT, Bartholomeu DC (2015) Linear B-cell epitope mapping of MAPK3 and MAPK4 from Leishmania braziliensis: implications for the serodiagnosis of human and canine leishmaniasis. Appl Microbiol Biotechnol 99(3):1323–1336. https://doi.org/10.1007/s00253-014-6168-7
Miller BR III, McGee TD Jr, Swails JM, Homeyer N, Gohlke H, Roitberg AE (2012) MMPBSA.py: an efficient program for end-state free energy calculations. J Chem The Comput 8(9):3314–3321. https://doi.org/10.1021/ct300418h
Zhang Y et al (2019) How does chirality determine the selective inhibition of histone deacetylase 6? A lesson from Trichostatin a enantiomers based on molecular dynamics. ACS Chem Neurosci 10(5):2467–2480. https://doi.org/10.1021/acschemneuro.8b00729
Fu TT et al (2021) Subtype-selective mechanisms of negative allosteric modulators binding to group I metabotropic glutamate receptors. Acta Pharmacol Sin 42(8):1354–1367. https://doi.org/10.1038/s41401-020-00541-z
Xue W et al (2018) What contributes to serotonin-norepinephrine reuptake inhibitors’ Dual-targeting mechanism? The key role of transmembrane domain 6 in human serotonin and norepinephrine transporters revealed by molecular dynamics simulation. ACS Chem Neurosci 9(5):1128–1140. https://doi.org/10.1021/acschemneuro.7b00490
Erdmann M, Scholz A, Melzer IM, Schmetz C, Wiese M (2006) Interacting protein kinases involved in the regulation of flagellar length. Mol Biol Cell 17(4):2035–2045. https://doi.org/10.1091/mbc.e05-10-0976
Sanderson L, Yardley V, Croft SL (2014) Activity of anti-cancer protein kinase inhibitors against Leishmania spp. J Antimicrob Chemother 69(7):1888–1891. https://doi.org/10.1093/jac/dku069
Funding
This work was financially supported by the Kasetsart University Research and Development Institute, (KURDI), Bangkok, Thailand under 404 KURDI (FF(KU)6.64).
Author information
Authors and Affiliations
Contributions
Conceptualization and design: KC and TA; designed and performed the experiments: KC, TA, NR, DK, and SS; data collection and analysis: TA; writing—original draft: TA; writing—review and editing: KC.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
Not required.
Informed consent
Not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aiebchun, T., Rasri, N., Kiriwan, D. et al. In Vitro and In Silico Studies of Kinase Inhibitor of MAPK3 Protein to Determine Leishmania martiniquensis Treatment. Acta Parasit. 68, 240–248 (2023). https://doi.org/10.1007/s11686-023-00659-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11686-023-00659-0