Abstract
Background
The impact of cirrhosis on perioperative outcomes for elderly patients undergoing hepatectomy remains not well defined. We sought to determine the influence of underlying cirrhosis and minimally invasive surgery (MIS) on postoperative outcomes among elderly patients who underwent a hepatectomy.
Methods
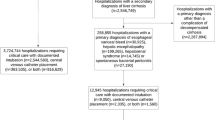
Patients who underwent hepatectomy between 2013 and 2015 were identified using the Center for Medicare Services (CMS) 100% Limited Data Set (LDS) Standard Analytic Files (SAFs). Short-term outcomes after hepatectomy, stratified by the presence of cirrhosis and MIS, were examined.
Results
Among 7452 patients who underwent a hepatectomy, a minority had cirrhosis (n = 481, 6.5%) whereas the vast majority did not (n = 6971, 93.5%). Overall, median patient age was 72 years (IQR 68–76) and preoperative Charlson comorbidity score was 6 (IQR 2–8). Patients with cirrhosis were more likely to be younger (median age 71 [67–76] vs 72 [IQR 68–76] years), male (64.4% vs 50%), African American (8.1% vs 6.4%) and have a malignant diagnosis (87.1% vs 78.7%) compared to non-cirrhotic patients (all p < 0.001). There was no difference among patients with and without cirrhosis regarding type of hepatectomy or surgical approach (open vs MIS) (both p > 0.05). Patients with versus without cirrhosis had similar complication rates (24.1% vs 22.3%, p = 0.36), as well as 30-day (6.2% vs 5%, p = 0.25) and 90-day (10.4% vs 8.5%, p = 0.15) mortality. MIS reduced the length-of-stay in non-cirrhotic patients (OR 0.79, 95% CI 0.62–0.99, p < 0.05), yet was not associated with morbidity or mortality (both p > 0.05).
Conclusion
The presence of cirrhosis did not generally impact outcomes in elderly patients undergoing hepatectomy for benign and malignant diseases. MIS hepatectomy in the elderly Medicare beneficiary population reduced LOS among patients without cirrhosis, yet was not associated with differences in morbidity or mortality.

Similar content being viewed by others
References
Ali N, O’Rourke C, El-Hayek K, Chalikonda S, Jeyarajah DR, Walsh RM. Estimating the need for hepato-pancreatico-biliary surgeons in the USA. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2015;17(4):352–6. doi:https://doi.org/10.1111/hpb.12370.
Setiawan VW, Stram DO, Porcel J, Lu SC, Le Marchand L, Noureddin M. Prevalence of chronic liver disease and cirrhosis by underlying cause in understudied ethnic groups: The multiethnic cohort. Hepatology. 2016;64(6):1969–77. doi:https://doi.org/10.1002/hep.28677.
Zerillo J, Agarwal P, Poeran J, Zubizarreta N, Poultsides G, Schwartz M et al. Perioperative Management in Hepatic Resections: Comparative Effectiveness of Neuraxial Anesthesia and Disparity of Care Patterns. Anesthesia and analgesia. 2018;127(4):855–63. doi:https://doi.org/10.1213/ane.0000000000003579.
Bell BP, Manos MM, Zaman A, Terrault N, Thomas A, Navarro VJ et al. The epidemiology of newly diagnosed chronic liver disease in gastroenterology practices in the United States: results from population-based surveillance. The American journal of gastroenterology. 2008;103(11):2727–36; quiz 37. doi:https://doi.org/10.1111/j.1572-0241.2008.02071.x.
Fan ST, Lai EC, Lo CM, Ng IO, Wong J. Hospital mortality of major hepatectomy for hepatocellular carcinoma associated with cirrhosis. Archives of surgery (Chicago, Ill : 1960). 1995;130(2):198–203.
Gozzetti G, Mazziotti A, Cavallari A, Bellusci R, Bolondi L, Grigioni W et al. Clinical experience with hepatic resections for hepatocellular carcinoma in patients with cirrhosis. Surgery, gynecology & obstetrics. 1988;166(6):503–10.
Nagasue N, Kohno H, Chang YC, Taniura H, Yamanoi A, Uchida M et al. Liver resection for hepatocellular carcinoma. Results of 229 consecutive patients during 11 years. Annals of surgery. 1993;217(4):375–84.
Xu HW, Liu F, Li HY, Wei YG, Li B. Outcomes following laparoscopic versus open major hepatectomy for hepatocellular carcinoma in patients with cirrhosis: a propensity score-matched analysis. Surgical endoscopy. 2018;32(2):712–9. doi:https://doi.org/10.1007/s00464-017-5727-2.
Cauchy F, Fuks D, Nomi T, Dokmak S, Scatton O, Schwarz L et al. Benefits of Laparoscopy in Elderly Patients Requiring Major Liver Resection. Journal of the American College of Surgeons. 2016;222(2):174–84.e10. doi:https://doi.org/10.1016/j.jamcollsurg.2015.11.006.
Schmucker DL. Age-related changes in liver structure and function: Implications for disease ? Exp Gerontol. 2005;40(8-9):650-9. doi:https://doi.org/10.1016/j.exger.2005.06.009.
Poon RT, Fan ST, Lo CM, Liu CL, Lam CM, Yuen WK et al. Extended hepatic resection for hepatocellular carcinoma in patients with cirrhosis: is it justified? Annals of surgery. 2002;236(5):602-11. doi:https://doi.org/10.1097/01.sla.0000033038.38956.5e.
Wu CC, Cheng SB, Ho WM, Chen JT, Liu TJ, P’Eng F K. Liver resection for hepatocellular carcinoma in patients with cirrhosis. The British journal of surgery. 2005;92(3):348–55. doi:https://doi.org/10.1002/bjs.4838.
Menon KV, Al-Mukhtar A, Aldouri A, Prasad RK, Lodge PA, Toogood GJ. Outcomes after major hepatectomy in elderly patients. Journal of the American College of Surgeons. 2006;203(5):677–83. doi:https://doi.org/10.1016/j.jamcollsurg.2006.07.025.
Paredes AZ, Beal EW, Bagante F, Dillhoff ME, Cloyd JM, Pawlik TM. Patterns of readmission among the elderly after hepatopancreatobiliary surgery. American journal of surgery. 2018. doi:https://doi.org/10.1016/j.amjsurg.2018.09.011.
Gani F, Cerullo M, Amini N, Buettner S, Margonis GA, Sasaki K et al. Frailty as a Risk Predictor of Morbidity and Mortality Following Liver Surgery. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2017;21(5):822–30. doi:https://doi.org/10.1007/s11605-017-3373-6.
Li J, Shen Y, Tan L, Feng M, Wang H, Xi Y et al. Is minimally invasive esophagectomy beneficial to elderly patients with esophageal cancer? Surgical endoscopy. 2015;29(4):925–30. doi:https://doi.org/10.1007/s00464-014-3753-x.
Fan CJ, Chien HL, Weiss MJ, He J, Wolfgang CL, Cameron JL et al. Minimally invasive versus open surgery in the Medicare population: a comparison of post-operative and economic outcomes. Surgical endoscopy. 2018;32(9):3874–80. doi:https://doi.org/10.1007/s00464-018-6126-z.
Clark JR, Wills VL, Hunt DR. Cirrhosis and laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2001;11(3):165–9.
Yoon YI, Kim KH, Kang SH, Kim WJ, Shin MH, Lee SK et al. Pure Laparoscopic Versus Open Right Hepatectomy for Hepatocellular Carcinoma in Patients With Cirrhosis: A Propensity Score Matched Analysis. Annals of surgery. 2017;265(5):856–63. doi:https://doi.org/10.1097/sla.0000000000002072.
Chen J, Bai T, Zhang Y, Xie ZB, Wang XB, Wu FX et al. The safety and efficacy of laparoscopic and open hepatectomy in hepatocellular carcinoma patients with liver cirrhosis: a systematic review. International journal of clinical and experimental medicine. 2015;8(11):20679–89.
Tsilimigras DI, Moris D, Vagios S, Merath K, Pawlik TM. Safety and oncologic outcomes of robotic liver resections: A systematic review. J Surg Oncol. 2018;117(7):1517–30. doi:https://doi.org/10.1002/jso.25018.
Ciria R, Cherqui D, Geller DA, Briceno J, Wakabayashi G. Comparative Short-term Benefits of Laparoscopic Liver Resection: 9000 Cases and Climbing. Annals of surgery. 2016;263(4):761–77. doi:https://doi.org/10.1097/sla.0000000000001413.
Cheung TT, Dai WC, Tsang SH, Chan AC, Chok KS, Chan SC et al. Pure Laparoscopic Hepatectomy Versus Open Hepatectomy for Hepatocellular Carcinoma in 110 Patients With Liver Cirrhosis: A Propensity Analysis at a Single Center. Annals of surgery. 2016;264(4):612–20. doi:https://doi.org/10.1097/sla.0000000000001848.
Wang WL, Zhu Y, Cheng JW, Li MX, Xia JM, Hao J et al. Major hepatectomy is safe for hepatocellular carcinoma in elderly patients with cirrhosis. European journal of gastroenterology & hepatology. 2014;26(4):444–51. doi:https://doi.org/10.1097/meg.0000000000000046.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical care. 2005;43(11):1130–9.
Iezzoni LI, Daley J, Heeren T, Foley SM, Fisher ES, Duncan C et al. Identifying complications of care using administrative data. Medical care. 1994;32(7):700–15.
Osborne NH, Nicholas LH, Ryan AM, Thumma JR, Dimick JB. Association of hospital participation in a quality reporting program with surgical outcomes and expenditures for Medicare beneficiaries. Jama. 2015;313(5):496–504. doi:https://doi.org/10.1001/jama.2015.25.
Iezzoni LI, Daley J, Heeren T, Foley SM, Hughes JS, Fisher ES et al. Using administrative data to screen hospitals for high complication rates. Inquiry : a journal of medical care organization, provision and financing. 1994;31(1):40–55.
Mokdad AA, Lopez AD, Shahraz S, Lozano R, Mokdad AH, Stanaway J et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med. 2014;12:145. doi:https://doi.org/10.1186/s12916-014-0145-y.
Petrowsky H, Clavien PA. Should we deny surgery for malignant hepato-pancreatico-biliary tumors to elderly patients? World journal of surgery. 2005;29(9):1093–100. doi:https://doi.org/10.1007/s00268-005-1130-6.
Poon RT, Fan ST, Lo CM, Liu CL, Lam CM, Yuen WK et al. Improving perioperative outcome expands the role of hepatectomy in management of benign and malignant hepatobiliary diseases: analysis of 1222 consecutive patients from a prospective database. Annals of surgery. 2004;240(4):698–708; discussion -10.
Müller-Höcker J, Aust D, Rohrbach H, Napiwotzky J, Reith A, Link TA et al. Defects of the respiratory chain in the normal human liver and in cirrhosis during aging. Hepatology. 1997;26(3):709–19. doi:https://doi.org/10.1002/hep.510260324.
Brouwer A, Barelds RJ, Knook DL. Age-related changes in the endocytic capacity of rat liver Kupffer and endothelial cells. Hepatology. 1985;5(3):362–6.
Sastre J, Pallardó FV, Plá R, Pellín A, Juan G, O’Connor JE et al. Aging of the liver: age-associated mitochondrial damage in intact hepatocytes. Hepatology. 1996;24(5):1199–205. doi:https://doi.org/10.1002/hep.510240536.
Vitale A, Spolverato G, Bagante F, Gani F, Popescu I, Marques HP et al. A multi-institutional analysis of elderly patients undergoing a liver resection for intrahepatic cholangiocarcinoma. J Surg Oncol. 2016;113(4):420–6. doi:https://doi.org/10.1002/jso.24148.
Zhang X-F, Bagante F, Chakedis J, Moris D, Beal EW, Weiss M et al. Perioperative and Long-Term Outcome for Intrahepatic Cholangiocarcinoma: Impact of Major Versus Minor Hepatectomy. Journal of Gastrointestinal Surgery. 2017;21(11):1841–50. doi:https://doi.org/10.1007/s11605-017-3499-6.
Cheung TT, Poon RT, Yuen WK, Chok KS, Jenkins CR, Chan SC et al. Long-term survival analysis of pure laparoscopic versus open hepatectomy for hepatocellular carcinoma in patients with cirrhosis: a single-center experience. Annals of surgery. 2013;257(3):506-11. doi:https://doi.org/10.1097/SLA.0b013e31827b947a.
Belli G, Fantini C, D’Agostino A, Cioffi L, Langella S, Russolillo N et al. Laparoscopic versus open liver resection for hepatocellular carcinoma in patients with histologically proven cirrhosis: short- and middle-term results. Surgical endoscopy. 2007;21(11):2004–11. doi:https://doi.org/10.1007/s00464-007-9503-6.
Belli G, Limongelli P, Fantini C, D’Agostino A, Cioffi L, Belli A et al. Laparoscopic and open treatment of hepatocellular carcinoma in patients with cirrhosis. The British journal of surgery. 2009;96(9):1041–8. doi:https://doi.org/10.1002/bjs.6680.
Kaneko H, Tsuchiya M, Otsuka Y, Yajima S, Minagawa T, Watanabe M et al. Laparoscopic hepatectomy for hepatocellular carcinoma in cirrhotic patients. Journal of hepato-biliary-pancreatic surgery. 2009;16(4):433–8. doi:https://doi.org/10.1007/s00534-009-0123-5.
Sucandy I, Cheek S, Tsung A, Marsh JW, Geller DA. Minimally invasive liver resection for primary and metastatic liver tumors: influence of age on perioperative complications and mortality. Surgical endoscopy. 2018;32(4):1885–91. doi:https://doi.org/10.1007/s00464-017-5880-7.
Nomi T, Fuks D, Kawaguchi Y, Mal F, Nakajima Y, Gayet B. Laparoscopic major hepatectomy for colorectal liver metastases in elderly patients: a single-center, case-matched study. Surgical endoscopy. 2015;29(6):1368–75. doi:https://doi.org/10.1007/s00464-014-3806-1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 16 kb)
Rights and permissions
About this article
Cite this article
Sahara, K., Paredes, A.Z., Tsilimigras, D.I. et al. Impact of Liver Cirrhosis on Perioperative Outcomes Among Elderly Patients Undergoing Hepatectomy: the Effect of Minimally Invasive Surgery. J Gastrointest Surg 23, 2346–2353 (2019). https://doi.org/10.1007/s11605-019-04117-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04117-z