Abstract
Motivation
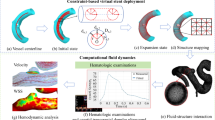
Intra-saccular devices (ID), developed for the treatment of bifurcation aneurysms, offer new alternatives for treating complex terminal and bifurcation aneurysms. In this work, a complete workflow going from medical images to post-treatment CFD analysis is described and used in the assessment of a concrete clinical problem.
Materials and methods
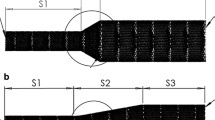
Two different intra-saccular device sizes were virtually implanted in 3D models of the patient vasculature using the ID-Fit method. After deployment, the local porosity at the closed end of the device in contact with the blood flow was computed. This porosity was then used to produce a CFD porous medium model of the device. Velocities and wall shear stress were assessed for each model.
Results
Six patients treated with intra-saccular devices were included in this work. For each case, 2 different device sizes were virtually implanted and 3 CFD simulations were performed: after deployment simulation with each size and before deployment simulation (untreated). A visible reduction in velocities was observed after device implantation. Velocity and WSS reduction was statistically significant (K–S statistics, \(p<0.001\)).
Conclusions
Placement of different device size can lead to a partial filling of the aneurysm, either at the dome or at the neck, depending on the particular positioning by the interventionist. The methodology used in this work can have a strong clinical impact, since it provides additional information in the process of device selection using preoperative data.





Similar content being viewed by others
References
Grasso G, Alafaci C, Macdonald RL (2017) Management of aneurysmal subarachnoid hemorrhage: State of the art and future perspectives. Surg Neurol Int 8:11
Molyneux A, Kerr R, International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group (2002) International subarachnoid aneurysm trial (isat) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized trial. J Stroke Cerebrovasc Dis 11(6):304–314
Pierot L, Wakhloo AK (2013) Endovascular treatment of intracranial aneurysms: current status. Stroke 44(7):2046–2054
Cebral JR, Castro MA, Appanaboyina S, Putman CM, Millan D, Frangi AF (2005) Efficient pipeline for image-based patient-specific analysis of cerebral aneurysm hemodynamics: technique and sensitivity. IEEE Trans Med Imag 24(4):457–467
Ford MD, Nikolov HN, Milner JS, Lownie SP, DeMont EM, Kalata W, Loth F, Holdsworth DW, Steinman DA (2008) Piv-measured versus cfd-predicted flow dynamics in anatomically realistic cerebral aneurysm models. J Biomech Eng 130(2):021015
Ma D, Dargush GF, Natarajan SK, Levy EI, Siddiqui AH, Meng H (2012) Computer modeling of deployment and mechanical expansion of neurovascular flow diverter in patient-specific intracranial aneurysms. J Biomech 45(13):2256–2263
Larrabide I, Kim M, Augsburger L, Villa-Uriol MC, Rüfenacht D, Frangi AF (2012) Fast virtual deployment of self-expandable stents: method and in vitro evaluation for intracranial aneurysmal stenting. Med Image Anal 16(3):721–730
Mut F, Chung BJ, Chudyk J, Lylyk P, Kadirvel R, Kallmes DF, Cebral JR (2019) Image-based modeling of blood flow in cerebral aneurysms treated with intrasaccular flow diverting devices. Int J Numer Methods Biomed Eng 35(6):e3202
Muñoz R, Narata AP, Larrabide I (2020) Id-fit: Intra-saccular device adjustment for personalized cerebral aneurysm treatment. International conference on medical image computing and computer-assisted intervention. Springer, New York, pp 97–105
Moyano RK, Fernandez H, Macho JM, Blasco J, Roman LS, Narata AP, Larrabide I (2017) A robustness test of the braided device foreshortening algorithm. In: Proceedings of the 13th international conference on medical information processing and analysis, vol 10572. International Society for Optics and Photonics, p 105721H
Larrabide I, Villa-Uriol M-C, Cárdenes R, Barbarito V, Carotenuto L, Geers AJ, Morales HG, Pozo JM, Mazzeo MD, Hrvoje Bogunović P, Olmedas CR, Macho JM, Frangi AF (2012) Angiolab: a software tool for morphological analysis and endovascular treatment planning of intracranial aneurysms. Comput Methods Programs Biomed 108(2):806–819
Narata AP, Blasco J, Roman LS, Macho JM, Fernandez H, Moyano RK, Winzenrieth R, Larrabide I (2018) Early results in flow diverter sizing by computational simulation: quantification of size change and simulation error assessment. Operat Neurosurg 15(5):557–566
Arthur A, Hoit D, Coon A, Almandoz JED, Elijovich L, Cekirge S, Fiorella D (2018) Physician training protocol within the web intrasaccular therapy (web-it) study. J Neuroint Surg 10(5):500–504
Dazeo N, Dottori J, Boroni G, Larrabide I (2018) A comparative study of porous medium cfd models for flow diverter stents: advantages and shortcomings. Int J Numer Methods Biomed Eng 34(12):e3145
Jasak H, Jemcov A, Tukovic Z (2007) Openfoam: A c++ library for complex physics simulations. In: International workshop on coupled methods in numerical dynamics, vol 1000. IUC Dubrovnik, Croatia, pp 1–20
Dazeo NI, Dottori JA, Boroni GA, Larrabide I (2018) Heterogeneous porous media simulation. Mecánica Comput 36:1173–1181
Morales HG, Larrabide I, Geers AJ, Aguilar ML, Frangi AF (2013) Newtonian and non-newtonian blood flow in coiled cerebral aneurysms. J Biomech 46(13):2158–2164
Valencia A (2005) Simulation of unsteady laminar flow in models of terminal aneurysm of the basilar artery. Int J Comput Fluid Dyn 19(4):337–345
Castro MA, Putman CM, Sheridan MJ, Cebral JR (2009) Hemodynamic patterns of anterior communicating artery aneurysms: a possible association with rupture. Am J Neuroradiol 30(2):297–302
Cebral JR, Castro MA, Soto O, Löhner R, Alperin N (2003) Blood-flow models of the circle of willis from magnetic resonance data. J Eng Math 47(3–4):369–386
Steinman DA, Milner JS, Norley CJ, Lownie SP, Holdsworth DW (2003) Image-based computational simulation of flow dynamics in a giant intracranial aneurysm. Am J Neuroradiol 24(4):559–566
Hassan T, Timofeev EV, Saito T, Shimizu H, Ezura M, Tominaga T, Takahashi A, Takayama K (2004) Computational replicas: anatomic reconstructions of cerebral vessels as volume numerical grids at three-dimensional angiography. Am J Neuroradiol 25(8):1356–1365
Stuhne GR, Steinman DA (2004) Finite-element modeling of the hemodynamics of stented aneurysms. J Biomech Eng 126(3):382–387
Ohta M, Wetzel SG, Dantan P, Bachelet C, Lovblad KO, Yilmaz H, Flaud P, Rüfenacht DA (2005) Rheological changes after stenting of a cerebral aneurysm: a finite element modeling approach. Cardiovasc Intervent Radiol 28(6):768–772
Castro MA, Putman CM, Cebral JR (2006) Computational fluid dynamics modeling of intracranial aneurysms: effects of parent artery segmentation on intra-aneurysmal hemodynamics. Am J Neuroradiol 27(8):1703–1709
CFD Direct Ltd. snappyHexMesh user guide, 2021. https://cfd.direct/openfoam/user-guide/v8-snappyHexMesh/
Dazeo N, Dottori J, Boroni G, Narata AP, Larrabide I (2020) Stenting as porous media in anatomically accurate geometries. a comparison of models and spatial heterogeneity. J Biomech 110:109945
Utkarsh A (2015) The paraview guide: a parallel visualization application. Kitware. Inc., New York
Ding YH, Lewis DA, Kadirvel R, Dai D, Kallmes DF (2011) The woven endobridge: a new aneurysm occlusion device. Am J Neuroradiol 32(3):607–611
Valencia A, Morales H, Rivera R, Bravo E, Galvez M (2008) Blood flow dynamics in patient-specific cerebral aneurysm models: the relationship between wall shear stress and aneurysm area index. Med Eng Phys 30(3):329–340
Cagnazzo F, Marnat G, Ferreira I, Daube P, Derraz I, Dargazanli C, Lefevre PH, Gascou G, Riquelme C, Morganti R, Berge J, Gariel F, Barreau X, Costalat V (2020) Comparison of woven endobridge device sizing with conventional measurements and virtual simulation using the sim&size software: a multicenter experience. J NeuroIntervent Surg. https://doi.org/10.1136/neurintsurg-2020-017060
Kayembe KN, Sasahara M, Hazama F (1984) Cerebral aneurysms and variations in the circle of willis. Stroke 15(5):846–850
Larrabide I, Aguilar ML, Morales HG, Geers AJ, Kulcsár Z, Rüfenacht D, Frangi AF (2013) Intra-aneurysmal pressure and flow changes induced by flow diverters: relation to aneurysm size and shape. Am J Neuroradiol 34(4):816–822
Cebral JR, Chung BJ, Mut F, Chudyk J, Bleise C, Scrivano E, Lylyk P, Kadirvel R, Kallmes D (2019) Analysis of flow dynamics and outcomes of cerebral aneurysms treated with intrasaccular flow-diverting devices. Am J Neuroradiol 40(9):1511–1516
Mut F, Raschi M, Scrivano E, Bleise C, Chudyk J, Ceratto R, Lylyk P, Cebral JR (2015) Association between hemodynamic conditions and occlusion times after flow diversion in cerebral aneurysms. J Neuroint Surg 7(4):286–290
Cebral JR, Hernandez M, Frangi A, Putman C, Pergolizzi R, Burgess J (2004) Subject-specific modeling of intracranial aneurysms. In: Medical imaging 2004: physiology, function, and structure from medical images, vol 5369. International society for optics and photonics, pp 319–327
Funding
This project was partly funded by PICT 2016-0116 - FONCYT - ANPCYT of Argentina. N.D. and R. M. are supported by CONICET PhD grant. The Titan V used for this research was donated by the NVIDIA Corporation. The financial support of these institutions is greatly appreciated.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
HF and IL are Co-Founders of Galgo Medical S.L.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dazeo, N., Muñoz, R., Narata, A.P. et al. Intra-saccular device modeling for treatment planning of intracranial aneurysms: from morphology to hemodynamics. Int J CARS 16, 1663–1673 (2021). https://doi.org/10.1007/s11548-021-02427-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-021-02427-9