Abstract
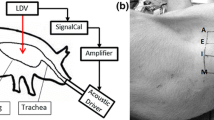
Pulmonary diseases and injury lead to structural and functional changes in the lung parenchyma and airways, often resulting in measurable sound transmission changes on the chest wall surface. Additionally, noninvasive imaging of externally driven mechanical wave motion in the chest (e.g., using magnetic resonance elastography) can provide information about lung stiffness and other structural property changes which may be of diagnostic value. In the present study, a comprehensive computational simulation (in silico) model was developed to simulate sound wave propagation in the airways, parenchyma, and chest wall under normal and pathological conditions that create distributed structural (e.g., pneumothoraces) and diffuse material (e.g., fibrosis) changes, as well as a localized structural and material changes as may be seen with a neoplasm. Experiments were carried out in normal subjects to validate the baseline model. Sound waves with frequency content from 50 to 600 Hz were introduced into the airways of three healthy human subjects through the mouth, and transthoracic transmitted waves were measured by scanning laser Doppler vibrometry at the chest wall surface. The computational model predictions of a frequency-dependent decreased sound transmission due to pneumothorax were consistent with experimental measurements reported in previous work. Predictions for the case of fibrosis show that while shear wave motion is altered, changes to compression wave propagation are negligible, and thus, insonification, which primarily drives compression waves, is not ideal to detect the presence of fibrosis. Results from the numerical simulation of a tumor show an increase in the wavelength of propagating waves in the immediate vicinity of the tumor region.

Graphical abstract












Similar content being viewed by others
References
Rice D a (1983) Sound speed in pulmonary parenchyma. J Appl Physiol Respir Environ Exerc Physiol 54(1):304–308. https://doi.org/10.1152/jappl.1983.54.1.304
Smith NB, Webb A (2010) Introduction to medical imaging: physics, engineering and clinical applications. Retrieved from https://ebookcentral.proquest.com/lib/uic/detail.action?docID=585341
McGee KP, Hubmayr RD, Ehman RL (2008) MR elastography of the lung with hyperpolarized 3He. Magn Reson Med 59(1):14–18. https://doi.org/10.1002/mrm.21465
Goss BC, McGee KP, Ehman EC, Manduca A, Ehman RL (2006) Magnetic resonance elastography of the lung: technical feasibility. Magn Reson Med 56(5):1060–1066. https://doi.org/10.1002/mrm.21053
Mariappan YK, Kolipaka A, Manduca A, Hubmayr RD, Ehman RL, Araoz P, McGee KP (2012) Magnetic resonance elastography of the lung parenchyma in an in situ porcine model with a noninvasive mechanical driver: correlation of shear stiffness with trans-respiratory system pressures. Magn Reson Med 67(1):210–217. https://doi.org/10.1002/mrm.22976
Liu Y, Royston TJ, Klatt D, Lewandowski ED (2016) Cardiac MR elastography of the mouse: initial results. Magn Reson Med 76(6):1879–1886. https://doi.org/10.1002/mrm.26030
Romano A, Scheel M, Hirsch S, Braun J, Sack I (2012) In vivo waveguide elastography of white matter tracts in the human brain. Magn Reson Med 68(5):1410–1422. https://doi.org/10.1002/mrm.24141
Palnitkar H, Reiter R, Majumdar S, Lewis PL, Hammersley M, Shah RN et al (2019) An investigation into the relationship between inhomogeneity and wave shapes in phantoms and ex-vivo skeletal muscle using magnetic resonance elastography and finite element analysis. J Mech Behav Biomed Mater 98:108–120. https://doi.org/10.1016/j.jmbbm.2019.06.007
Lutchen KR, Suki B (1996) Understanding pulmonary mechanics using the forced oscillations technique. In Bioengineering approaches to pulmonary physiology and medicine (pp. 227–253). Springer, Boston. doi:https://doi.org/10.1007/978-0-585-34964-0_15
Peng Y, Dai Z, Mansy HA, Henry B, Balk RA, Sandler RH, Roys (2016) Sound transmission in porcine thorax through airway insonification. Med Biol Eng Comput 54(4):675–689. https://doi.org/10.1007/s11517-015-1358-8
Peng Y, Dai Z, Mansy HA, Sandler RH, Balk RA, Royston TJ (2014) Sound transmission in the chest under surface excitation: an experimental and computational study with diagnostic applications. Med Biol Eng Comput 52(8):695–706. https://doi.org/10.1007/s11517-014-1172-8
Polytec PSV-500 scanning vibrometer: full field optical vibration measurement. (n.d.). Retrieved from https://www.polytec.com/us/vibrometry/products/full-field-vibrometers/psv-500-scanning-vibrometer/
Dai Z, Peng Y, Mansy HA, Sandler RH, Royston TJ (2014) Comparison of poroviscoelastic models for sound and vibration in the lungs. J Vib Acoust 136(5):051012. https://doi.org/10.1115/1.4026436
Dai Z, Peng Y, Mansy HA, Sandler RH, Royston TJ (2015) Experimental and computational studies of sound transmission in a branching airway network embedded in a compliant viscoelastic medium. J Sound Vib 339:215–229. https://doi.org/10.1016/j.jsv.2014.11.026
Henry B, Royston TJ (2017) A multiscale analytical model of bronchial airway acoustics. J Acoust Soc Am 142(4):1774–1783. https://doi.org/10.1121/1.5005497
Dai Z, Peng Y, Henry B, Mansy H, Royston T (2014) A comprehensive computational model of sound transmission through the porcine lung. J Acoust Soc Am 136:1419–1429
Tawhai MH (2004) CT-based geometry analysis and finite element models of the human and ovine bronchial tree. J Appl Physiol 97(6):2310–2321. https://doi.org/10.1152/japplphysiol.00520.2004
Horsfield K, Cumming G (1968) Morphology of the bronchial tree in man. Respir Physiol 26(2):173–182. https://doi.org/10.1016/0034-5687(76)90095-5
Kitaoka H (2012) Construction of the human lung and air flow analysis. Forma 27:21–27 Retrieved from https://pdfs.semanticscholar.org/75b5/645f58a808d6559c5000bf99ad70942cbc9a.pdf
Henry B, Royston TJ (2017) A multiscale analytical model of bronchial airway acoustics. J Acoust Soc Am 142(4):1774–1780. Retrieved from. https://doi.org/10.1121/1.5005497
Royston TJ, Zhang X, Mansy HA, Sandler RH (2002) Modeling sound transmission through the pulmonary system and chest with application to diagnosis of a collapsed lung. J Acoust Soc Am 111(4):1931–1946
Wodicka GR, Stevens KN, Golup HL, Carvalho EG, Shannon DC (1989) A model of acoustic transmission in the respiratory system. IEEE Trans Biomed Eng 36(9):925–934. https://doi.org/10.1121/1.398217
NIH US National Library of Medicine (2018) Primary spontaneous pneumothorax. NIH. Retrieved from https://ghr.nlm.nih.gov/condition/primary-spontaneous-pneumothorax
NIH US National Library of Medicine (2018) Idiopathic pulmonary fibrosis. NIH. Retrieved from https://ghr.nlm.nih.gov/condition/idiopathic-pulmonary-fibrosis#statistics
American Lung Association (2018) Lung cancer fact sheet. American Lung Assoc. Retrieved from https://www.lung.org/lung-health-and-diseases/lung-disease-lookup/lung-cancer/resource-library/lung-cancer-fact-sheet.html
Choi S, Yoon S, Jichan J, Zou C, Choi J, Tawhai MH et al (2019) 1D network simulations for evaluating regional flow and pressure distributions in healthy and asthmatic human lungs. J Appl Physiol 127:122–133. https://doi.org/10.1152/japplphysiol.00016.2019
Habib RH, Chalker RB, Suki B, Jackson AC (1994) Airway geometry and wall mechanical properties estimated from subglottal input impedance in humans. J Appl Physiol (1985) 77:441–451. https://doi.org/10.1152/jappl.1994.77.1.441
Jackson AC, Habib RH, Suki B, Wood SA, Mitzner W (1995) Serial distribution of airway diameters from input impedance and computed tomography. Ann Biomed Eng 23(6):740–749. https://doi.org/10.1007/BF02584473
Kitaoka H, Koc S, Tetsumoto S, Koumo S, Hirata H, Kijima T (2013) 4D model generator of the human lung, “Lung4Cer” Conference proceedings:.. Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual Conference, 2013, 453–456. doi:https://doi.org/10.1109/EMBC.2013.6609534
Royston TJ, Ozer MB, Acikgoz S, Mansy HA, Sandler RH (2008) Advances in computational modeling of sound propagation in the lungs and torso with diagnostic applications. In: Vibration and acoustics in biomedical applications: imaging, characterization and diagnostics. ASME, New York, pp 215–246. https://doi.org/10.1115/1.802755.ch9
Dubois AB, Brody AW, Lewis DH, Burgess BF Jr (1956) Oscillation mechanics of lungs and chest in man. J Appl Physiol 8:587–594
Schanz M (2001) Wave propagation in viscoelastic and poroelastic continua: a boundary element approach (Vol. 4). Springer, Berlin
The Visible Human Project (n.d.) The US National Library of Medicine. Retrieved from https://www.nlm.nih.gov/research/visible/animations.html
Hughes T (2000) The finite element method: linear static and dynamic finite element analysis (First.). Upper Saddle River: Prentice-Hall Inc
von Gierke HE, Oestreicher HL, Franke EK, Parrack HO, von Wittern WW (1952) Physics of vibrations in living tissues. J Appl Physiol 4(12):886–900
Royston TJ, Dai Z, Chaunsali R, Liu Y, Peng Y, Magin RL (2011) Estimating material viscoelastic properties based on surface wave measurements: a comparison of techniques and modeling assumptions. J Acoust Soc Am 130(6):4126–4138. https://doi.org/10.1121/1.3655883
Garner E, Lakes R, Lee T, Swan C, Brand R (2000) Viscoelastic dissipation in compact bone: implications for stress-induced fluid flow in bone. J Biomech Eng 122(2):166–172. https://doi.org/10.1115/1.429638
Lakes RS, Katz JL, Sternstein SS (1979) Viscoelastic properties of wet cortical bone—I. torsional and biaxial studies. J Biomech 12(9):657–678. https://doi.org/10.1016/0021-9290(79)90016-2
American Cancer Society (2018) Lung carcinoid tumor stages: early detection, diagnosis and staging. Retrieved from https://www.cancer.org/cancer/lung-carcinoid-tumor/detection-diagnosis-staging/staging.html
Sinkus R, Tanter M, Xydeasc T, Cathelineb S, Bercoff J, Fink M (2005) Viscoelastic shear properties of in vivo breast lesions measured by MR elastography. J Magn Reson Imaging 23:159–165. https://doi.org/10.1016/j.mri.2004.11.060
Mansy HA, Royston TJ, Balk RA, Sandler RH (2002) Pneumothorax detection using computerised analysis of breath sounds. Med Biol Eng Comput 40(5):526–532. https://doi.org/10.1007/BF02345450
Mansy HA, Royston TJ, Balk RA, Sandler RH (2002) Pneumothorax detection using pulmonary acoustic transmission measurements. Med Biol Eng Comput 40(5):520–525. https://doi.org/10.1007/BF02345449
Mansy HA, Balk RA, Warren WH, Royston TJ, Dai Z, Peng Y, Sandler RH (2015) Pneumothorax effects on pulmonary acoustic transmission. J Appl Physiol 119(3):250–257. https://doi.org/10.1152/japplphysiol.00148.2015
Loomba R, Wolfson T, Ang B, Hooker J, Behling C, Peterson M, Valasek M, Lin G, Brenner D, Gamst A, Ehman R, Sirlin C (2014) Magnetic resonance elastography predicts advanced fibrosis in patients with nonalcoholic fatty liver disease: a prospective study. Hepatology 60(6):1920–1928. https://doi.org/10.1002/hep.27362
Funding
This study received financial support from the National Institutes of Health (Grant Nos. EB012142 and UL1 TR002003 pilot grant 2018-04).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix. Comparison of sound propagation in healthy human lung parenchyma (experiment versus computation)
Appendix. Comparison of sound propagation in healthy human lung parenchyma (experiment versus computation)
Rights and permissions
About this article
Cite this article
Palnitkar, H., Henry, B.M., Dai, Z. et al. Sound transmission in human thorax through airway insonification: an experimental and computational study with diagnostic applications. Med Biol Eng Comput 58, 2239–2258 (2020). https://doi.org/10.1007/s11517-020-02211-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-020-02211-y