Abstract
Introduction
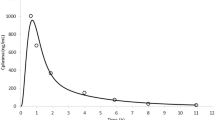
Ketoconazole and posaconazole are two weakly basic broad-spectrum antifungals classified as Biopharmaceutics Classification System class II drugs, indicating that they are highly permeable, but exhibit poor solubility. As a result, oral bioavailability and clinical efficacy can be impacted by the formulation performance in the gastrointestinal system. In this work, we have leveraged in vitro biopharmaceutics and clinical data available in the literature to build physiologically based pharmacokinetic (PBPK) models for ketoconazole and posaconazole, to determine the suitability of forward in vitro-in vivo translation for characterization of in vivo drug precipitation, and to predict food effect.
Methods
A stepwise modeling approach was utilized to derive key parameters related to absorption, such as drug solubility, dissolution, and precipitation kinetics from in vitro data. These parameters were then integrated into PBPK models for the simulation of ketoconazole and posaconazole plasma concentrations in the fasted and fed states.
Results
Forward in vitro-in vivo translation of intestinal precipitation kinetics for both model drugs resulted in poor predictions of PK profiles. Therefore, a reverse translation approach was applied, based on limited fitting of precipitation-related parameters to clinical data. Subsequent simulations for ketoconazole and posaconazole demonstrated that fasted and fed state PK profiles for both drugs were adequately recapitulated.
Conclusion
The two examples presented in this paper show how middle-out modeling approaches can be used to predict the magnitude and direction of food effects provided the model is verified on fasted state PK data.
Graphical Abstract









Similar content being viewed by others
Data Availability
All data used in this research was obtained from public reports and referenced.
References
Chen Y, Jin JY, Mukadam S, Malhi V, Kenny JR. Application of IVIVE and PBPK modeling in prospective prediction of clinical pharmacokinetics: strategy and approach during the drug discovery phase with four case studies. Biopharm Drug Dispos. 2012;33(2):85–98. https://doi.org/10.1002/bdd.1769.
Pathak SM, Schaefer KJ, Jamei M, Turner DB. Biopharmaceutic IVIVE-mechanistic modeling of single- and two-phase in vitro experiments to obtain drug-specific parameters for incorporation into PBPK models. J Pharm Sci. 2019;108(4):1604–18. https://doi.org/10.1016/j.xphs.2018.11.034.
Mudie DM, Shi Y, Ping H, Gao P, Amidon GL, Amidon GE. Mechanistic analysis of solute transport in an in vitro physiological two-phase dissolution apparatus. Biopharm Drug Dispos. 2012;33(7):378–402. https://doi.org/10.1002/bdd.1803.
Cristofoletti R, Hens B, Patel N, Esteban VV, Schmidt S, Dressman J. Integrating drug- and formulation-related properties with gastrointestinal tract variability using a product-specific particle size approach: Case example ibuprofen. J Pharm Sci. 2019;108(12):3842–7. https://doi.org/10.1016/j.xphs.2019.09.012.
Yamazaki S, Evers R, De Zwart L. Physiologically-based pharmacokinetic modeling to evaluate in vitro-to-in vivo extrapolation for intestinal P-glycoprotein inhibition. CPT Pharmacometrics Syst Pharmacol. 2022;11(1):55–67. https://doi.org/10.1002/psp4.12733.
Vinarov Z, Abrahamsson B, Artursson P, Batchelor H, Berben P, Bernkop-Schnürch A, et al. Current challenges and future perspectives in oral absorption research: An opinion of the UNGAP network. Adv Drug Deliv Rev. 2021;171:289–331. https://doi.org/10.1016/j.addr.2021.02.001.
Patel S, Zhu W, Xia B, Sharma N, Hermans A, Ehrick JD, et al. Integration of precipitation kinetics from an in vitro, multicompartment transfer system and mechanistic oral absorption modeling for pharmacokinetic prediction of weakly basic drugs. J Pharm Sci. 2019;108(1):574–83. https://doi.org/10.1016/j.xphs.2018.10.051.
Bouzom F, Ball K, Perdaems N, Walther B. Physiologically based pharmacokinetic (PBPK) modelling tools: how to fit with our needs? Biopharm Drug Dispos. 2012;33(2):55–71. https://doi.org/10.1002/bdd.1767.
Cristofoletti R, Patel N, Dressman JB. Differences in food effects for 2 weak bases with similar BCS drug-related properties: What is happening in the intestinal lumen? J Pharm Sci. 2016;105(9):2712–22. https://doi.org/10.1016/j.xphs.2015.11.033.
Pepin XJH, Huckle JE, Alluri RV, Basu S, Dodd S, Parrott N, et al. Understanding mechanisms of food effect and developing reliable PBPK models using a middle-out approach. AAPS J. 2021;23(1):12. https://doi.org/10.1208/s12248-020-00548-8.
Heeres J, Meerpoel L, Lewi P. Conazoles. Molecules. 2010;15(6):4129-88. doi: https://doi.org/10.3390/molecules15064129.
Pathak SM, Ruff A, Kostewicz ES, Patel N, Turner DB, Jamei M. Model-based analysis of biopharmaceutic experiments to improve mechanistic oral absorption modeling: An integrated in vitro in vivo extrapolation perspective using ketoconazole as a model drug. Mol Pharm. 2017;14(12):4305–20. https://doi.org/10.1021/acs.molpharmaceut.7b00406.
Hens B, Brouwers J, Corsetti M, Augustijns P. Supersaturation and precipitation of posaconazole upon entry in the upper small intestine in humans. J Pharm Sci. 2016;105(9):2677–84. https://doi.org/10.1002/jps.24690.
Hens B, Pathak SM, Mitra A, Patel N, Liu B, Patel S, et al. In silico modeling approach for the evaluation of gastrointestinal dissolution, supersaturation, and precipitation of posaconazole. Mol Pharm. 2017;14(12):4321–33. https://doi.org/10.1021/acs.molpharmaceut.7b00396.
Daneshmend TK, Warnock DW, Turner A, Roberts CJ. Pharmacokinetics of ketoconazole in normal subjects. J Antimicrob Chemother. 1981;8(4):299–304. https://doi.org/10.1093/jac/8.4.299.
Ruff A, Fiolka T, Kostewicz ES. Prediction of ketoconazole absorption using an updated in vitro transfer model coupled to physiologically based pharmacokinetic modelling. European journal of pharmaceutical sciences : official journal of the European Federation for Pharmaceutical Sciences. 2017;100:42–55. https://doi.org/10.1016/j.ejps.2016.12.017.
Mithani SD, Bakatselou V, TenHoor CN, Dressman JB. Estimation of the increase in solubility of drugs as a function of bile salt concentration. Pharm Res. 1996;13(1):163–7. https://doi.org/10.1023/a:1016062224568.
Horter D, Dressman JB. Influence of physicochemical properties on dissolution of drugs in the gastrointestinal tract. Adv Drug Deliv Rev. 2001;46(1–3):75–87. https://doi.org/10.1016/s0169-409x(00)00130-7.
Jambhekar SS, Breen PJ. Drug dissolution: significance of physicochemical properties and physiological conditions. Drug Discovery Today. 2013;18(23–24):1173–84. https://doi.org/10.1016/j.drudis.2013.08.013.
Lu AT, Frisella ME, Johnson KC. Dissolution modeling: factors affecting the dissolution rates of polydisperse powders. Pharm Res. 1993;10(9):1308–14. https://doi.org/10.1023/a:1018917729477.
Kambayashi A, Yasuji T, Dressman JB. Prediction of the precipitation profiles of weak base drugs in the small intestine using a simplified transfer (“dumping”) model coupled with in silico modeling and simulation approach. European journal of pharmaceutics and biopharmaceutics : official journal of Arbeitsgemeinschaft fur Pharmazeutische Verfahrenstechnik eV. 2016;103:95–103. https://doi.org/10.1016/j.ejpb.2016.03.020.
O'Dwyer PJ, Imanidis G, Box KJ, Reppas C. On the usefulness of two small-scale in vitro setups in the evaluation of luminal precipitation of lipophilic weak bases in early formulation development. Pharmaceutics. 2020;12(3). https://doi.org/10.3390/pharmaceutics12030272.
Lindfors L, Forssen S, Westergren J, Olsson U. Nucleation and crystal growth in supersaturated solutions of a model drug. J Colloid Interface Sci. 2008;325(2):404–13. https://doi.org/10.1016/j.jcis.2008.05.034.
Ingels F, Beck B, Oth M, Augustijns P. Effect of simulated intestinal fluid on drug permeability estimation across Caco-2 monolayers. Int J Pharm. 2004;274(1–2):221–32. https://doi.org/10.1016/j.ijpharm.2004.01.014.
Hens B, Bolger MB. Application of a dynamic fluid and pH model to simulate intraluminal and systemic concentrations of a weak base in gastroplus(). J Pharm Sci. 2019;108(1):305–15. https://doi.org/10.1016/j.xphs.2018.10.041.
Huang YC, Colaizzi JL, Bierman RH, Woestenborghs R, Heykants J. Pharmacokinetics and dose proportionality of ketoconazole in normal volunteers. Antimicrob Agents Chemother. 1986;30(2):206–10. https://doi.org/10.1128/AAC.30.2.206.
Nakasato S, Shah GM, Morrissey RL, Winer RL. Ketoconazole treatment of fungal infection in acute renal failure. Clin Exp Dial Apheresis. 1983;7(3):191–6. https://doi.org/10.3109/08860228309076048.
Daneshmend TK, Warnock DW, Ene MD, Johnson EM, Potten MR, Richardson MD, et al. Influence of food on the pharmacokinetics of ketoconazole. Antimicrob Agents Chemother. 1984;25(1):1–3. https://doi.org/10.1128/AAC.25.1.1.
Abduljalil K, Cain T, Humphries H, Rostami-Hodjegan A. Deciding on success criteria for predictability of pharmacokinetic parameters from in vitro studies: an analysis based on in vivo observations. Drug metabolism and disposition: the biological fate of chemicals. 2014;42(9):1478–84. https://doi.org/10.1124/dmd.114.058099.
Margolskee A, Darwich AS, Pepin X, Aarons L, Galetin A, Rostami-Hodjegan A, et al. IMI - oral biopharmaceutics tools project - evaluation of bottom-up PBPK prediction success part 2: An introduction to the simulation exercise and overview of results. European journal of pharmaceutical sciences : official journal of the European Federation for Pharmaceutical Sciences. 2017;96:610–25. https://doi.org/10.1016/j.ejps.2016.10.036.
Poulin P, Jones HM, Jones RD, Yates JW, Gibson CR, Chien JY, et al. PhRMA CPCDC initiative on predictive models of human pharmacokinetics, part 1: goals, properties of the PhRMA dataset, and comparison with literature datasets. J Pharm Sci. 2011;100(10):4050–73. https://doi.org/10.1002/jps.22554.
Kersemaekers WM, van Iersel T, Nassander U, O’Mara E, Waskin H, Caceres M, et al. Pharmacokinetics and safety study of posaconazole intravenous solution administered peripherally to healthy subjects. Antimicrob Agents Chemother. 2015;59(2):1246–51. https://doi.org/10.1128/AAC.04223-14.
Krishna G, Moton A, Ma L, Medlock MM, McLeod J. Pharmacokinetics and absorption of posaconazole oral suspension under various gastric conditions in healthy volunteers. Antimicrob Agents Chemother. 2009;53(3):958–66. https://doi.org/10.1128/AAC.01034-08.
Rodgers T, Leahy D, Rowland M. Physiologically based pharmacokinetic modeling 1: predicting the tissue distribution of moderate-to-strong bases. J Pharm Sci. 2005;94(6):1259–76. https://doi.org/10.1002/jps.20322.
Rodgers T, Rowland M. Physiologically based pharmacokinetic modelling 2: predicting the tissue distribution of acids, very weak bases, neutrals and zwitterions. J Pharm Sci. 2006;95(6):1238–57. https://doi.org/10.1002/jps.20502.
Ghosal A, Hapangama N, Yuan Y, Achanfuo-Yeboah J, Iannucci R, Chowdhury S, et al. Identification of human UDP-glucuronosyltransferase enzyme(s) responsible for the glucuronidation of posaconazole (Noxafil). Drug metabolism and disposition: the biological fate of chemicals. 2004;32(2):267–71. https://doi.org/10.1124/dmd.32.2.267.
Hallifax D, Houston JB. Binding of drugs to hepatic microsomes: comment and assessment of current prediction methodology with recommendation for improvement. Drug metabolism and disposition: the biological fate of chemicals. 2006;34(4):724–6; author reply 7. https://doi.org/10.1124/dmd.105.007658.
Courtney R, Sansone A, Smith W, Marbury T, Statkevich P, Martinho M, et al. Posaconazole pharmacokinetics, safety, and tolerability in subjects with varying degrees of chronic renal disease. J Clin Pharmacol. 2005;45(2):185–92. https://doi.org/10.1177/0091270004271402.
Ezzet F, Wexler D, Courtney R, Krishna G, Lim J, Laughlin M. Oral bioavailability of posaconazole in fasted healthy subjects: comparison between three regimens and basis for clinical dosage recommendations. Clin Pharmacokinet. 2005;44(2):211–20. https://doi.org/10.2165/00003088-200544020-00006.
Krishna G, Ma L, Martinho M, O’Mara E. Single-dose phase I study to evaluate the pharmacokinetics of posaconazole in new tablet and capsule formulations relative to oral suspension. Antimicrob Agents Chemother. 2012;56(8):4196–201. https://doi.org/10.1128/AAC.00222-12.
Dressman JB, Berardi RR, Dermentzoglou LC, Russell TL, Schmaltz SP, Barnett JL, et al. Upper gastrointestinal (GI) pH in young, healthy men and women. Pharm Res. 1990;7(7):756–61. https://doi.org/10.1023/a:1015827908309.
O’Grady J, Murphy CL, Barry L, Shanahan F, Buckley M. Defining gastrointestinal transit time using video capsule endoscopy: a study of healthy subjects. Endoscopy international open. 2020;8(3):E396–400. https://doi.org/10.1055/a-1073-7653.
Fadda HM, McConnell EL, Short MD, Basit AW. Meal-induced acceleration of tablet transit through the human small intestine. Pharm Res. 2009;26(2):356–60. https://doi.org/10.1007/s11095-008-9749-2.
Russell TL, Berardi RR, Barnett JL, Dermentzoglou LC, Jarvenpaa KM, Schmaltz SP, et al. Upper gastrointestinal pH in seventy-nine healthy, elderly, North American men and women. Pharm Res. 1993;10(2):187–96. https://doi.org/10.1023/a:1018970323716.
Psachoulias D, Vertzoni M, Goumas K, Kalioras V, Beato S, Butler J, et al. Precipitation in and supersaturation of contents of the upper small intestine after administration of two weak bases to fasted adults. Pharm Res. 2011;28(12):3145–58. https://doi.org/10.1007/s11095-011-0506-6.
Rostami-Hodjegan A. Reverse translation in PBPK and QSP: going backwards in order to go forward with confidence. Clin Pharmacol Ther. 2018;103(2):224–32. https://doi.org/10.1002/cpt.904.
Adhikari A, Seo PR, Polli JE. Characterization of dissolution-permeation system using hollow fiber membrane module and utility to predict in vivo drug permeation across BCS classes. J Pharmaceutical Sci. 2022. https://doi.org/10.1016/j.xphs.2022.07.002.
Hate SS, Reutzel-Edens SM, Taylor LS. Absorptive dissolution testing: An improved approach to study the impact of residual crystallinity on the performance of amorphous formulations. J Pharm Sci. 2020;109(3):1312–23. https://doi.org/10.1016/j.xphs.2019.11.016.
Augustijns P, Wuyts B, Hens B, Annaert P, Butler J, Brouwers J. A review of drug solubility in human intestinal fluids: implications for the prediction of oral absorption. European journal of pharmaceutical sciences : official journal of the European Federation for Pharmaceutical Sciences. 2014;57:322–32. https://doi.org/10.1016/j.ejps.2013.08.027.
Courtney R, Wexler D, Radwanski E, Lim J, Laughlin M. Effect of food on the relative bioavailability of two oral formulations of posaconazole in healthy adults. Br J Clin Pharmacol. 2004;57(2):218–22. https://doi.org/10.1046/j.1365-2125.2003.01977.x.
Jamil R, Polli JE. Prediction of food effect on in vitro drug dissolution into biorelevant media: Contributions of solubility enhancement and relatively low colloid diffusivity. European journal of pharmaceutical sciences : official journal of the European Federation for Pharmaceutical Sciences. 2022;177:106274. https://doi.org/10.1016/j.ejps.2022.106274.
Riedmaier AE, DeMent K, Huckle J, Bransford P, Stillhart C, Lloyd R, et al. Use of physiologically based pharmacokinetic (PBPK) modeling for predicting drug-food interactions: An industry perspective. AAPS J. 2020;22(6):123. https://doi.org/10.1208/s12248-020-00508-2.
Lake-Bakaar G, Quadros E, Beidas S, Elsakr M, Tom W, Wilson DE, et al. Gastric secretory failure in patients with the acquired immunodeficiency syndrome (AIDS). Ann Intern Med. 1988;109(6):502–4. https://doi.org/10.7326/0003-4819-109-6-502.
Welage LS, Carver PL, Revankar S, Pierson C, Kauffman CA. Alterations in gastric acidity in patients infected with human immunodeficiency virus. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 1995;21(6):1431–8. https://doi.org/10.1093/clinids/21.6.1431.
Ketoconazole. https://pubchem.ncbi.nlm.nih.gov/compound/3823. Accessed 28 Apr 2022.
Posaconazole. https://pubchem.ncbi.nlm.nih.gov/compound/468595. Accessed 28 Apr 2022.
Mannisto PT, Mantyla R, Nykanen S, Lamminsivu U, Ottoila P. Impairing effect of food on ketoconazole absorption. Antimicrob Agents Chemother. 1982;21(5):730–3. https://doi.org/10.1128/AAC.21.5.730.
Noxafil (Posaconazole) Label. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/022003s018s020,0205053s002s004,0205596s001s003lbl.pdf. Accessed 28 Apr 2022.
Acknowledgements
The authors would like to thank Simulations Plus, Lancaster, CA for sponsoring this research and for providing academic licenses of DDDPlus™ and GastroPlus to the Center for Pharmacometrics and Systems Pharmacology at the University of Florida.
Funding
This study was sponsored by Simulations Plus, Lancaster, CA (No. AWD08034).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
RC was an external member of the Simulations Plus scientific advisory board. All the other authors declare that they have no competing financial interests or personal relationships that could have influenced the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Franco, Y.L., Da Silva, L., Charbe, N. et al. Integrating Forward and Reverse Translation in PBPK Modeling to Predict Food Effect on Oral Absorption of Weakly Basic Drugs. Pharm Res 40, 405–418 (2023). https://doi.org/10.1007/s11095-023-03478-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-023-03478-0