Abstract
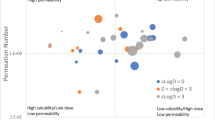
Food can alter drug absorption and impact safety and efficacy. Besides conducting clinical studies, in vitro approaches such as biorelevant solubility and dissolution testing and in vivo dog studies are typical approaches to estimate a drug’s food effect. The use of physiologically based pharmacokinetic models has gained importance and is nowadays a standard tool for food effect predictions at preclinical and clinical stages in the pharmaceutical industry. This manuscript is part of a broader publication from the IQ Consortium’s food effect physiologically based pharmacokinetic model (PBPK) modeling working group and complements previous publications by focusing on cases where the food effect was predicted with low confidence. Pazopanib-HCl, trospium-Cl, and ziprasidone-HCl served as model compounds to provide insights into why several food effect predictions failed in the first instance. Furthermore, the manuscript depicts approaches whereby PBPK-based food effect predictions may be improved. These improvements should focus on the PBPK model functionality, especially better reflecting fasted- and fed-state gastric solubility, gastric re-acidification, and complex mechanisms related to gastric emptying of drugs. For improvement of in vitro methodologies, the focus should be on the development of more predictive solubility, supersaturation, and precipitation assays. With regards to the general PBPK modeling methodology, modelers should account for the full solubility profile when modeling ionizable compounds, including common ion effects, and apply a straightforward strategy to account for drug precipitation.






Similar content being viewed by others
References
Fleisher D, Li C, Zhou Y, Pao LH, Karim A. Drug, meal and formulation interactions influencing drug absorption after oral administration. Clinical implications. Clin Pharmacokinet. 1999;36(3):233–54.
FDA. Assessing the effects of food on drugs in INDs and NDAs — clinical pharmacology considerations guidance for industry. 2019. https://www.fda.gov/media/121313/download
Li M, Zhao P, Pan Y, Wagner C. Predictive performance of physiologically based pharmacokinetic models for the effect of food on oral drug absorption: current status. CPT Pharmacometrics Syst Pharmacol. 2018;7(2):82–9.
Emami Riedmaier A, DeMent K, Huckle J, Bransford P, Stillhart C, Alluri R, et al. Use of PBPK modeling for predicting drug-food interactions: an industry perspective. AAPS J. 2020;22(123):1–15.
Pepin X, Huckle JE, Alluri RV, Basu S, Dodd S, Parrott N, et al. Understanding mechanisms of food effect and developing reliable PBPK models using a middle-out approach. AAPS J. 2021;23:12.
Deng Y, Sychterz C, Suttle AB, Dar MM, Bershas D, Negash K, et al. Bioavailability, metabolism and disposition of oral pazopanib in patients with advanced cancer. Xenobiotica. 2013;43(5):443–53.
Hurwitz HI, Dowlati A, Saini S, Savage S, Suttle AB, Gibson DM, et al. Phase I trial of pazopanib in patients with advanced cancer. Clin Cancer Res. 2009;15(12):4220–7.
FDA. Clinical Pharmacology and Biopharmaceutics review for Votrient (NDA 22-465). 2009. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2009/022465s000_clinpharmr.pdf
Heath EI, Chiorean EG, Sweeney CJ, Hodge JP, Lager JJ, Forman K, et al. A phase I study of the pharmacokinetic and safety profiles of oral pazopanib with a high-fat or low-fat meal in patients with advanced solid tumors. Clin Pharmacol Ther. 2010;88(6):818–23.
Jede C, Wagner C, Kubas H, Weigandt M, Weber C, Lecomte M, et al. Improved prediction of in vivo supersaturation and precipitation of poorly soluble weakly basic drugs using a biorelevant bicarbonate buffer in a gastrointestinal transfer model. Mol Pharm. 2019;16(9):3938–47.
Hogan DL, Ainsworth MA, Isenberg JI. Review article: gastroduodenal bicarbonate secretion. Aliment Pharmacol Ther. 1994;8(5):475–88.
Doroshyenko O, Jetter A, Odenthal K, Fuhr U. Clinical pharmacokinetics of trospium chloride. Clin Pharmacokinet. 2005;44(7):701–20.
Schladitz-Keil G, Spahn H, Mutschler E. Determination of the bioavailability of the quaternary compound trospium chloride in man from urinary excretion data. Arzneimittel-Forschung. 1986;36(6):984–7.
FDA. Clinical Pharmacology and Biopharmaceutics review for Sanctura (NDA 21-595). 2004. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2004/21-595_Sanctura_BioPharmr_P1.pdf
FDA. Clinical Pharmacology and Biopharmaceutics review for Sanctura XR (NDA 22-103). 2007. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2007/022103s000_ClinPharmR.pdf
Heinen CA, Reuss S, Amidon GL, Langguth P. Ion pairing with bile salts modulates intestinal permeability and contributes to food–drug interaction of BCS class III compound trospium chloride. Mol Pharm. 2013;10(11):3989–96.
Tadken T, Weiss M, Modess C, Wegner D, Roustom T, Neumeister C, et al. Trospium chloride is absorbed from two intestinal “absorption windows” with different permeability in healthy subjects. Int J Pharm. 2016;515(1-2):367–73.
Radwan A, Amidon GL, Langguth P. Mechanistic investigation of food effect on disintegration and dissolution of BCS class III compound solid formulations: the importance of viscosity: mechanism of food effect for BCS class III product. Biopharm Drug Dispos. 2012;33(7):403–16.
Miceli JJ, Glue P, Alderman J, Wilner K. The effect of food on the absorption of oral ziprasidone. Psychopharmacol Bull. 2007;40(3):58–68.
FDA. Clinical Pharmacology and Biopharmaceutics review for Geodon (NDA 20-825). 2004. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2001/20-825_Geodan.cfm
FDA. Approved label for Geodon. 2008. p. Revised June 2008. https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/020825s035,020919s023lbl.pdf
Yee S. In vitro permeability across Caco-2 cells (colonic) can predict in vivo (small intestinal) absorption in man—fact or myth. Pharm Res. 1997;14(6):763–6.
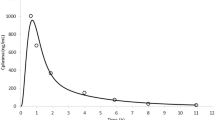
Sutton S, Nause R, Gandelman K. The impact of gastric pH, volume, and emptying on the food effect of ziprasidone oral absorption. AAPS J. 2017;19(4):1084–90.
GSK. An open-label, two-period, randomized, crossover study to evaluate the effect of food on the pharmacokinetics of single doses of pazopanib in cancer subjects (food-effect results only) In: Register G-CS, editor. 2007. https://s3.amazonaws.com/ctr-gsk-7381/VEG10005/3ac4a918-ecb5-4e42-90e9-aaf01a451734/05e47103-37ae-4f2e-a3d1-c3f17953e1f1/gsk-veg10005-clinical-study-report-redact-v1.pdf
Zhang R, Yuan G, Li R, Liu X, Wei C, Wang B, et al. Pharmacokinetic and bioequivalence studies of trospium chloride after a single-dose administration in healthy Chinese volunteers. Arzneimittelforschung. 2012;62(05):247–51.
Gandelman K, Alderman JA, Glue P, Lombardo I, LaBadie RR, Versavel M, et al. The impact of calories and fat content of meals on oral ziprasidone absorption: a randomized, open-label, crossover trial. J Clin Psychiatry. 2009;70(1):58–62.
Hörter D, Dressman JB. Influence of physicochemical properties on dissolution of drugs in the gastrointestinal tract. Adv Drug Deliv Rev. 1997;25:3–14.
Malagelada JR, Longstreth GF, Summerskill WH, Go VL. Measurement of gastric functions during digestion of ordinary solid meals in man. Gastroenterology. 1976;70(2):203–10.
Koziolek M, Schneider F, Grimm M, Modebeta C, Seekamp A, Roustom T, et al. Intragastric pH and pressure profiles after intake of the high-caloric, high-fat meal as used for food effect studies. J Control Release. 2015;220(Pt A):71–8.
Abebe Bayew T, Weiss M, Modess C, Roustom T, Tadken T, Wegner D, et al. Effects of the P-glycoprotein inhibitor clarithromycin on the pharmacokinetics of intravenous and oral trospium chloride: a 4-way crossover drug-drug interaction study in healthy subjects. J Clin Pharmacol. 2019;59(10):1319–30.
Akiyama Y, Ito S, Fujita T, Sugano K. Prediction of negative food effect induced by bile micelle binding on oral absorption of hydrophilic cationic drugs. Eur J Pharm Sci. 2020;155:105543.
Miller JM, Beig A, Krieg BJ, Carr RA, Borchardt TB, Amidon GE, et al. The solubility-permeability interplay: mechanistic modeling and predictive application of the impact of micellar solubilization on intestinal permeation. Mol Pharm. 2011;8(5):1848–56.
Sugano K. Estimation of effective intestinal membrane permeability considering bile micelle solubilisation. Int J Pharm. 2009;368(1-2):116–22.
Kleberg K, Jacobsen J, Mullertz A. Characterising the behaviour of poorly water soluble drugs in the intestine: application of biorelevant media for solubility, dissolution and transport studies. J Pharm Pharmacol. 2010;62(11):1656–68.
O'Reilly JR, Corrigan OI, O'Driscoll CM. The effect of mixed micellar systems, bile salt/fatty acids, on the solubility and intestinal absorption of clofazimine (B663) in the anaesthetised rat. Int J Pharm. 1994;109(2):147–54.
Cone RA. Barrier properties of mucus. Adv Drug Deliv Rev. 2009;61(2):75–85.
Ehehalt R, Braun A, Karner M, Füllekrug J, Stremmel W. Phosphatidylcholine as a constituent in the colonic mucosal barrier-physiological and clinical relevance. Biochim Biophys Acta. 2010;1801(9):983–93.
Shen H, Howles P, Tso P. From interaction of lipidic vehicles with intestinal epithelial cell membranes to the formation and secretion of chylomicrons. Adv Drug Deliv Rev. 2001;50(Suppl 1):S103–25.
Charman WN, Porter CJH, Mithani S, Dressman JB. Physicochemical and physiological mechanisms for the effects of food on drug absorption: the role of lipids and pH. J Pharm Sci. 1997;86(3):269–82.
Lin H, Gebhardt M, Bian S, Kwon KA, Shim CK, Chung SJ, et al. Enhancing effect of surfactants on fexofenadine.HCl transport across the human nasal epithelial cell monolayer. Int J Pharm. 2007;330(1-2):23–31.
Schiff ER, Small NC, Dietschy JM. Characterization of the kinetics of the passive and active transport mechanisms for bile acid absorption in the small intestine and colon of the rat. J Clin Investig. 1972;51(6):1351–62.
Arenson DR, Qi H, inventors; Pfizer Inc., assignee. Ziprasidone suspension. USA patent US 7,175,855 B1 2007 13/02/07.
Miceli JJ, Wilner KD, Swan SK, Tensfeldt TG. Pharmacokinetics, safety, and tolerability of intramuscular ziprasidone in healthy volunteers. J Clin Pharmacol. 2005;45(6):620–30.
Ferrua MJ, Singh RP. Modeling the fluid dynamics in a human stomach to gain insight of food digestion. J Food Sci. 2010;75(7):R151–62.
Koziolek M, Grimm M, Schneider F, Jedamzik P, Sager M, Kühn JP, et al. Navigating the human gastrointestinal tract for oral drug delivery: uncharted waters and new frontiers. Adv Drug Deliv Rev. 2016;101:75–88.
Grimm M, Scholz E, Koziolek M, Kuhn JP, Weitschies W. Gastric water emptying under fed state clinical trial conditions is as fast as under fasted conditions. Mol Pharm. 2017;14(12):4262–71.
Pal A, Brasseur JG, Abrahamsson B. A stomach road or "Magenstrasse" for gastric emptying. J Biomech. 2007;40(6):1202–10.
Jantratid E, Janssen N, Reppas C, Dressman JB. Dissolution media simulating conditions in the proximal human gastrointestinal tract: an update. Pharm Res. 2008;25(7):1663–76.
Biorelevant.com homepage [Available from: https://biorelevant.com/Fed_Gastric_Dissolution_Media/
Collins PJ, Houghton LA, Read NW, Horowitz M, Chatterton BE, Heddle R, et al. Role of the proximal and distal stomach in mixed solid and liquid meal emptying. Gut. 1991;32(6):615–9.
Weitschies W, Friedrich C, Wedemeyer RS, Schmidtmann M, Kosch O, Kinzig M, et al. Bioavailability of amoxicillin and clavulanic acid from extended release tablets depends on intragastric tablet deposition and gastric emptying. Eur J Pharm Biopharm. 2008;70(2):641–8.
Weitschies W, Wedemeyer RS, Kosch O, Fach K, Nagel S, Soderlind E, et al. Impact of the intragastric location of extended release tablets on food interactions. J Control Release. 2005;108(2-3):375–85.
Newton JM. Gastric emptying of multi-particulate dosage forms. Int J Pharm. 2010;395(1-2):2–8.
Goetze O, Steingoetter A, Menne D, van der Voort IR, Kwiatek MA, Boesiger P, et al. The effect of macronutrients on gastric volume responses and gastric emptying in humans: a magnetic resonance imaging study. Am J Physiol Gastrointest Liver Physiol. 2007;292(1):G11–7.
Grimm M, Koziolek M, Saleh M, Schneider F, Garbacz G, Kuhn JP, et al. Gastric emptying and small bowel water content after administration of grapefruit juice compared to water and isocaloric solutions of glucose and fructose: a four-way crossover MRI pilot study in healthy subjects. Mol Pharm. 2018;15(2):548–59.
Houghton LA, Hickson F, Read NW. Effect of food consistency on gastric emptying in man. Gut. 1987;28(12):1584–8.
Koziolek M, Grimm M, Garbacz G, Kuhn JP, Weitschies W. Intragastric volume changes after intake of a high-caloric, high-fat standard breakfast in healthy human subjects investigated by MRI. Mol Pharm. 2014;11(5):1632–9.
Marciani L, Pritchard SE, Hellier-Woods C, Costigan C, Hoad CL, Gowland PA, et al. Delayed gastric emptying and reduced postprandial small bowel water content of equicaloric whole meal bread versus rice meals in healthy subjects: novel MRI insights. Eur J Clin Nutr. 2013;67(7):754–8.
Fuchs A, Leigh M, Kloefer B, Dressman JB. Advances in the design of fasted state simulating intestinal fluids: FaSSIF-V3. Eur J Pharm Biopharm. 2015;94:229–40.
Soderlind E, Karlsson E, Carlsson A, Kong R, Lenz A, Lindborg S, et al. Simulating fasted human intestinal fluids: understanding the roles of lecithin and bile acids. Mol Pharm. 2010;7(5):1498–507.
Al-Gousous J, Salehi N, Amidon GE, Ziff RM, Langguth P, Amidon GL. Mass transport analysis of bicarbonate buffer: effect of the CO 2 – H 2 CO 3 hydration–dehydration kinetics in the fluid boundary layer and the apparent effective p K a controlling dissolution of acids and bases. Mol Pharm. 2019;16(6):2626–35.
Amaral Silva D, Al-Gousous J, Davies NM, Bou Chacra N, Webster GK, Lipka E, et al. Simulated, biorelevant, clinically relevant or physiologically relevant dissolution media: the hidden role of bicarbonate buffer. Eur J Pharm Biopharm. 2019;142:8–19.
Krieg BJ, Taghavi SM, Amidon GL, Amidon GE. In vivo predictive dissolution: comparing the effect of bicarbonate and phosphate buffer on the dissolution of weak acids and weak bases. J Pharm Sci. 2015;104(9):2894–904.
Garbacz G, Kolodziej B, Koziolek M, Weitschies W, Klein S. A dynamic system for the simulation of fasting luminal pH-gradients using hydrogen carbonate buffers for dissolution testing of ionisable compounds. Eur J Pharm Sci. 2014;51:224–31.
Kostewicz ES, Wunderlich M, Brauns U, Becker R, Bock T, Dressman JB. Predicting the precipitation of poorly soluble weak bases upon entry in the small intestine. J Pharm Pharmacol. 2004;56(1):43–51.
O'Dwyer PJ, Litou C, Box KJ, Dressman JB, Kostewicz ES, Kuentz M, et al. In vitro methods to assess drug precipitation in the fasted small intestine - a PEARRL review. J Pharm Pharmacol. 2019;71:536–56.
Carlert S, Palsson A, Hanisch G, von Corswant C, Nilsson C, Lindfors L, et al. Predicting intestinal precipitation-a case example for a basic BCS class II drug. Pharm Res. 2010;27(10):2119–30.
Mann J, Dressman J, Rosenblatt K, Ashworth L, Muenster U, Frank K, et al. Validation of dissolution testing with biorelevant media: an OrBiTo study. Mol Pharm. 2017;14(12):4192–201.
FDA. Chemistry review for Votrient (NDA 22-465). 2009. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2009/022465s000_ChemR.pdf
Drugbank. Pazopanib. 2012. p. https://go.drugbank.com/drugs/DB06589
GSK. An open-label, two-part study to characterize the pharmacokinetics of a single intravenous dose of pazopanib (GW786034) and the absorption, distribution, metabolism and elimination of a single oral [14C] labeled dose of pazopanib in subjects with solid tumor malignancies: final report. In: Register G-CS, editor. 2009. https://s3.amazonaws.com/ctr-gsk-7381/VEG10004/95aab286-8399-4dd6-bd42-48bea4cc216e/c90d2a8d-138f-4c28-8e5f-d37a5219d5f9/veg10004-clinical-study-report-redact-v02-v1.pdf
FDA. Chemistry review for Sanctura XR (NDA 22-103). 2007. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2007/022103s000_ChemR.pdf
Skořepová E, Čejka J, Hušák M, Eigner V, Rohlíček J, Šturc A, et al. Trospium chloride: unusual example of polymorphism based on structure disorder. Cryst Growth Des. 2013;13(12):5193–203.
Mercolini L, Mandrioli R, Protti M, Conca A, Albers L, Raggi M. Dried blood spot testing: a novel approach for the therapeutic drug monitoring of ziprasidone-treated patients. Bioanalysis. 2014;6(11):1487–95.
Hotha KK, Bharathi DV, Kumar SS, Reddy YN, Chatki PK, Ravindranath LK, et al. Determination of the quaternary ammonium compound trospium in human plasma by LC-MS/MS: application to a pharmacokinetic study. J Chromatogr B Anal Technol Biomed Life Sci. 2010;878(13-14):981–6.
Acknowledgements
The authors would like to thank Julian Semeraro, Sabrina Wacker, and Melanie Schneider (Merck KGaA) as well as Amy Dai and Varsha Dhamankar (Vertex) for conducting the in vitro experiments for the model compounds used in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Guest Editor: Filippos Kesisoglou
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 2156 kb)
Rights and permissions
About this article
Cite this article
Wagner, C., Kesisoglou, F., Pepin, X.J.H. et al. Use of Physiologically Based Pharmacokinetic Modeling for Predicting Drug–Food Interactions: Recommendations for Improving Predictive Performance of Low Confidence Food Effect Models. AAPS J 23, 85 (2021). https://doi.org/10.1208/s12248-021-00601-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-021-00601-0