Abstract
Background
MRI treatment response assessment maps (TRAMs) were introduced to distinguish recurrent malignant glioma from therapy related changes. TRAMs are calculated with two contrast-enhanced T1-weighted sequences and reflect the “late” wash-out (or contrast clearance) and wash-in of gadolinium. Vital tumor cells are assumed to produce a wash-out because of their high turnover rate and the associated hypervascularization, whereas contrast medium slowly accumulates in scar tissue. To examine the real value of this method, we compared TRAMs with the pathology findings obtained after a second biopsy or surgery when recurrence was suspected.
Methods
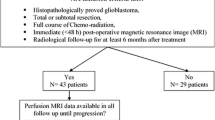
We retrospectively evaluated TRAMs in adult patients with histologically demonstrated glioblastoma, contrast-enhancing tissue and a pre-operative MRI between January 1, 2017, and December 31, 2022. Only patients with a second biopsy or surgery were evaluated. Volumes of the residual tumor, contrast clearance and contrast accumulation before the second surgery were analyzed.
Results
Among 339 patients with mGBM who underwent MRI, we identified 29 repeated surgeries/biopsies in 27 patients 59 ± 12 (mean ± standard deviation) years of age. Twenty-eight biopsies were from patients with recurrent glioblastoma histology, and only one was from a patient with radiation necrosis. We volumetrically evaluated the 29 pre-surgery TRAMs. In recurrent glioblastoma, the ratio of wash-out volume to tumor volume was 36 ± 17% (range 1–73%), and the ratio of the wash-out volume to the sum of wash-out and wash-in volumes was 48 ± 21% (range 22–92%). For the one biopsy with radiation necrosis, the ratios were 42% and 54%, respectively.
Conclusions
Typical recurrent glioblastoma shows a > 20%ratio of the wash-out volume to the sum of wash-out and wash-in volumes. The one biopsy with radiation necrosis indicated that such necrosis can also produce high wash-out in individual cases. Nevertheless, the additional information provided by TRAMs increases the reliability of diagnosis.




Similar content being viewed by others
Data availability
The datasets used and analyzed in the current study are partially available on request. Because individual patient data were not published, individual patients cannot be identified.
Code availability
Not applicable.
Abbreviations
- MRI :
-
Magnetic resonance imaging
- MP-RAGE :
-
Magnetization prepared–rapid gradient echo
- MR :
-
Magnetic resonance
- SD :
-
Standard deviation
- TRAMs :
-
Treatment assessment maps
- WOR :
-
(Normalized) wash-out ratio
References
Giglio P, Gilbert MR (2003) Cerebral radiation necrosis. Neurologist 9:180–188.https://doi.org/10.1097/01.nrl.0000080951.78533.c4
Kumar AJ, Leeds NE, Fuller GN et al (2000) Malignant gliomas: MR imaging Spectrum of radiation therapy- and chemotherapy-induced necrosis of the brain after treatment. Radiology 217:377–384. https://doi.org/10.1148/radiology.217.2.r00nv36377
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996. https://doi.org/10.1056/NEJMoa043330
Peca C, Pacelli R, Elefante A et al (2009) Early clinical and neuroradiological worsening after radiotherapy and concomitant temozolomide in patients with glioblastoma: Tumour progression or radionecrosis? Clin Neurol Neurosurg 111:331–334. https://doi.org/10.1016/j.clineuro.2008.11.003
Smith EJ, Naik A, Shaffer A et al (2023) Differentiating radiation necrosis from tumor recurrence: A systematic review and diagnostic meta-analysis comparing imaging modalities. J Neurooncol 162:15–23. https://doi.org/10.1007/s11060-023-04262-1
Mayo ZS, Halima A, Broughman JR et al (2023) Radiation necrosis or tumor progression? A review of the radiographic modalities used in the diagnosis of cerebral radiation necrosis. J Neurooncol 161:23–31. https://doi.org/10.1007/s11060-022-04225-y
Zach L, Guez D, Last D et al (2012) Delayed contrast extravasation MRI for depicting tumor and non-tumoral tissues in primary and metastatic brain tumors. PLoS One 7:e52008. https://doi.org/10.1371/journal.pone.0052008
Zach L, Guez D, Last D et al (2015) Delayed contrast extravasation MRI: A new paradigm in neuro-oncology. Neuro-Oncol 17:457–465. https://doi.org/10.1093/neuonc/nou230
Wen PY, Macdonald DR, Reardon DA et al (2010) Updated response assessment criteria for high-grade gliomas: Response assessment in neuro-oncology working group. J Clin Oncol 28:1963–1972. https://doi.org/10.1200/JCO.2009.26.3541
Perry JR, Laperriere N, O’Callaghan CJ et al (2017) Short-course radiation plus temozolomide in elderly patients with glioblastoma. N Engl J Med 376:1027–1037. https://doi.org/10.1056/NEJMoa1611977
Kuhl CK, Mielcareck P, Klaschik S et al (1999) Dynamic breast MR imaging: are signal intensity time course data useful for differential diagnosis of enhancing lesions? Radiology 211:101–110. https://doi.org/10.1148/radiology.211.1.r99ap38101
Ayuso C, Rimola J, Vilana R et al (2018) Diagnosis and staging of hepatocellular carcinoma (HCC): Current guidelines. Eur J Radiol 101:72–81. https://doi.org/10.1016/j.ejrad.2018.01.025
Thust SC, Heiland S, Falini A et al (2018) Glioma imaging in Europe: A survey of 220 centres and recommendations for best clinical practice. Eur Radiol 28:3306–3317. https://doi.org/10.1007/s00330-018-5314-5
Lai P-H, Chung H-W, Chang H-C et al (2019) Susceptibility-weighted imaging provides complementary value to diffusion-weighted imaging in the differentiation between pyogenic brain abscesses, necrotic glioblastomas, and necrotic metastatic brain tumors. Eur J Radiol 117:56–61. https://doi.org/10.1016/j.ejrad.2019.05.021
Nair SM, Sahu A, Dasgupta A et al (2023) Post-ictal changes presenting as late pseudoprogression on MRI and PET in a patient with diffuse glioma: Case report and brief literature review. Neuroradiol J 197140092311661. https://doi.org/10.1177/19714009231166105
Zikou A, Sioka C, Alexiou GA et al (2018) Radiation necrosis, pseudoprogression, pseudoresponse, and tumor recurrence: Imaging challenges for the evaluation of treated gliomas. Contrast Media Mol Imaging 2018:1–6. https://doi.org/10.1155/2018/6828396
Ellingson BM, Chung C, Pope WB et al (2017) Pseudoprogression, radionecrosis, inflammation or true tumor progression? Challenges associated with glioblastoma response assessment in an evolving therapeutic landscape. J Neurooncol 134:495–504. https://doi.org/10.1007/s11060-017-2375-2
Sanghera P, Perry J, Sahgal A et al (2010) Pseudoprogression following chemoradiotherapy for glioblastoma multiforme. Can J Neurol Sci J Can Sci Neurol 37:36–42. https://doi.org/10.1017/S0317167100009628
Brandsma D, Stalpers L, Taal W et al (2008) Clinical features, mechanisms, and management of pseudoprogression in malignant gliomas. Lancet Oncol 9:453–461. https://doi.org/10.1016/S1470-2045(08)70125-6
Brandes AA, Franceschi E, Tosoni A et al (2008) MGMT promoter methylation status can predict the incidence and outcome of pseudoprogression after concomitant radiochemotherapy in newly diagnosed glioblastoma patients. J Clin Oncol 26:2192–2197. https://doi.org/10.1200/JCO.2007.14.8163
Nguyen TB, Zakhari N, Velasco Sandoval S et al (2023) Diagnostic accuracy of arterial spin-labeling, dynamic contrast-enhanced, and DSC perfusion imaging in the diagnosis of recurrent high-grade gliomas: A prospective study. Am J Neuroradiol 44:134–142. https://doi.org/10.3174/ajnr.A7771
Zakhari N, Taccone MS, Torres CH et al (2019) Prospective comparative diagnostic accuracy evaluation of dynamic contrast-enhanced (DCE) vs. dynamic susceptibility contrast (DSC) MR perfusion in differentiating tumor recurrence from radiation necrosis in treated high-grade gliomas: Dynamic MR perfusion comparison. J Magn Reson Imaging 50:573–582. https://doi.org/10.1002/jmri.26621
Patel P, Baradaran H, Delgado D et al (2017) MR perfusion-weighted imaging in the evaluation of high-grade gliomas after treatment: A systematic review and meta-analysis. Neuro-Oncol 19:118–127. https://doi.org/10.1093/neuonc/now148
Weinberg BD, Kuruva M, Shim H, Mullins ME (2021) Clinical applications of magnetic resonance spectroscopy in brain tumors. Radiol Clin North Am 59:349–362. https://doi.org/10.1016/j.rcl.2021.01.004
Sacli-Bilmez B, Danyeli AE, Yakicier MC et al (2023) Magnetic resonance spectroscopic correlates of progression free and overall survival in “glioblastoma, IDH-wildtype, WHO grade-4.” Front Neurosci 17:1149292. https://doi.org/10.3389/fnins.2023.1149292
Sidibe I, Tensaouti F, Gilhodes J et al (2023) Pseudoprogression in GBM versus true progression in patients with glioblastoma: A multiapproach analysis. Radiother Oncol 181:109486. https://doi.org/10.1016/j.radonc.2023.109486
Zhang J, Wu Y, Wang Y et al (2022) Diffusion-weighted imaging and arterial spin labeling radiomics features may improve differentiation between radiation-induced brain injury and glioma recurrence. Eur Radiol 33:3332–3342. https://doi.org/10.1007/s00330-022-09365-3
Müller SJ, Khadhraoui E, Voit D et al (2023) Comparison of EPI DWI and STEAM DWI in early postoperative MRI controls after resection of tumors of the central nervous system. Clin Neuroradiol. https://doi.org/10.1007/s00062-023-01261-7
Kamali A, Gandhi A, Nunez LC et al (2022) The role of apparent diffusion coefficient values in glioblastoma: Differentiating tumor progression versus treatment-related changes. J Comput Assist Tomogr 46:923–928. https://doi.org/10.1097/RCT.0000000000001373
Chung H, Seo H, Choi SH, et al (2022) Cluster analysis of DSC MRI, dynamic contrast-enhanced MRI, and DWI parameters associated with prognosis in patients with glioblastoma after removal of the contrast-enhancing component: A preliminary study. Am J Neuroradiol ajnr;ajnr.A7655v1. https://doi.org/10.3174/ajnr.A7655
Qiao Z, Zhao X, Wang K et al (2019) Utility of dynamic susceptibility contrast perfusion-weighted MR imaging and 11 C-methionine PET/CT for differentiation of tumor recurrence from radiation injury in patients with high-grade gliomas. Am J Neuroradiol 40:253–259. https://doi.org/10.3174/ajnr.A5952
Soni N, Ora M, Mohindra N et al (2020) Diagnostic performance of PET and perfusion-weighted imaging in differentiating tumor recurrence or progression from radiation necrosis in posttreatment gliomas: A review of literature. Am J Neuroradiol ajnr;ajnr.A6685v1. https://doi.org/10.3174/ajnr.A6685
Satvat N, Korczynski O, Müller-Eschner M et al (2022) A rapid late enhancement MRI protocol improves differentiation between brain tumor recurrence and treatment-related contrast enhancement of brain parenchyma. Cancers 14:5523. https://doi.org/10.3390/cancers14225523
Guez D, Last D, Daniels D et al (2019) Radiation-induced vascular malformations in the brain, mimicking tumor in MRI-based treatment response assessment maps (TRAMs). Clin Transl Radiat Oncol 15:1–6. https://doi.org/10.1016/j.ctro.2018.11.004
Lakehayli Z, Phlips P, Margoum A et al (2023) What effective technique to differentiate radiation brain necrosis from a tumor progression in patients treated with radiation: A monocentric retrospective study combining the MRI TRAMs technique and the (18F)-dopa PET/CT. Cancer/Radiothérapie 27:273–280. https://doi.org/10.1016/j.canrad.2022.12.002
Admojo L, Korte J, Anderson N et al (2023) Investigating the role of delayed contrast magnetic resonance imaging (MRI) to differentiate radiation necrosis from tumour recurrence in brain metastases after stereotactic radiosurgery. J Med Imaging Radiat Oncol 67:292–298. https://doi.org/10.1111/1754-9485.13504
Peker S, Samanci Y, Aygun MS et al (2021) The use of treatment response assessment maps in discriminating between radiation effect and persistent tumoral lesion in metastatic brain tumors treated with gamma knife radiosurgery. World Neurosurg 146:e1134–e1146. https://doi.org/10.1016/j.wneu.2020.11.114
Millard T, Chau I, Iyengar S et al (2022) Treatment Response Assessment Maps (TRAMs), a new tool for CNS lymphoma. eJHaem 3:247–248. https://doi.org/10.1002/jha2.346
Jajodia A, Goel V, Goyal J et al (2022) Combined diagnostic accuracy of diffusion and perfusion MR imaging to differentiate radiation-induced necrosis from recurrence in glioblastoma. Diagnostics 12:718. https://doi.org/10.3390/diagnostics12030718
Nael K, Bauer AH, Hormigo A et al (2018) Multiparametric MRI for differentiation of radiation necrosis from recurrent tumor in patients with treated glioblastoma. Am J Roentgenol 210:18–23. https://doi.org/10.2214/AJR.17.18003
Li AY, Iv M (2022) Conventional and advanced imaging techniques in post-treatment glioma imaging. Front Radiol 2:883293. https://doi.org/10.3389/fradi.2022.883293
Alexiou GA, Tsiouris S, Kyritsis AP et al (2009) Glioma recurrence versus radiation necrosis: accuracy of current imaging modalities. J Neurooncol 95:1–11. https://doi.org/10.1007/s11060-009-9897-1
Phillips KA, Kamson DO, Schiff D (2023) Disease assessments in patients with glioblastoma. Curr Oncol Rep. https://doi.org/10.1007/s11912-023-01440-2
Funding
No funding was received for the conduct of this study.
Author information
Authors and Affiliations
Contributions
All authors have reviewed and approved the submitted manuscript for publication. The authors agree to be accountable for all aspects of the work, and to ensure its integrity and accuracy. SM was the project administrator and organized the data curation, measurements, design, literature review, and writing of the manuscript. EK contributed to data collection, measurements and analysis. GG contributed to the conceptualization, literature review, and design of the study. OG and HH contributed to the formal analysis and literature review of the study, draft, review, and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
This study was ethically approved by the institutional review board Ethik-Kommission der Landesärztekammer Baden-Württemberg (Liebknechtstr. 33, D-70565 Stuttgart, Germany, No. F-2023–037) and adhered to the 2013 Declaration of Helsinki.
Consent to participate
Because of the retrospective, observational nature of the study, the ethics committee (“Ethik-Kommission der Landesärztekammer Baden-Württemberg”) waived the requirement for informed consent.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Müller, S.J., Khadhraoui, E., Ganslandt, O. et al. MRI Treatment Response Assessment Maps (TRAMs) for differentiating recurrent glioblastoma from radiation necrosis. J Neurooncol 166, 513–521 (2024). https://doi.org/10.1007/s11060-024-04573-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-024-04573-x