Abstract
Fibroblast growth factor 23 (FGF23) discovery has provided new insights into the regulation of Pi and Ca homeostasis. It is secreted by osteoblasts and osteocytes, and acts mainly in the kidney, parathyroid, heart, and bone. The aim of this review is to highlight the current knowledge on the factors modulating the synthesis of FGF23, the canonical and non-canonical signaling pathways of the hormone, the role of FGF23 in different pathophysiological conditions, and the anti-FGF23 therapy. This is a narrative review based on the search of PubMed database in the range of years 2000–2023 using the keywords local and systemic regulators of FGF23 synthesis, FGF23 receptors, canonical and non-canonical pathways, pathophysiological conditions and FGF23, and anti-FGF23 therapy, focusing the data on the molecular mechanisms. The regulation of FGF23 synthesis is complex and multifactorial. It is regulated by local factors and systemic regulators mainly involved in bone mineralization. The excessive FGF23 production is associated with different congenital diseases and with diseases occurring with a secondary high FGF23 production such as in chronic disease kidney and tumor-induced osteomalacia (TIO). The anti-FGF23 therapy appears to be useful to treat chromosome X-linked hypophosphatemia and TIO, but there are doubts about the handle of excessive FGF23 production in CKD. FGF23 biochemistry and pathophysiology are generating a plethora of knowledge to reduce FGF23 bioactivity at many levels that might be useful for future therapeutics of diseases associated with high-serum FGF23 levels.
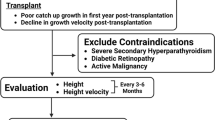
Graphical abstract



Similar content being viewed by others
Data Availability
No datasets were generated or analysed during the current study.
Abbreviations
- 1,25(OH)2D3:
-
1,25-Dihydroxyvitamin D
- ADHR:
-
Autosomal-dominant hereditary rickets
- BMD:
-
Bone mineral density
- Ca:
-
Calcium
- cFGF23:
-
C-terminal FGF23
- CKD:
-
Chronic kidney disease
- DMP1:
-
Dentin matrix protein 1
- EPO:
-
Erythropoietin
- ERK1/2:
-
Extracellular signal-regulated kinases 1/2
- ESRD:
-
End-stage renal disease
- FGFR:
-
FGF receptor
- FGFR1:
-
FGF receptor 1
- GalNT3:
-
N-acetylgalactosaminyltransferase 3
- HIF:
-
Hypoxia-inducible factor
- iFGF23:
-
Intact FGF23
- LVH:
-
Left ventricular hypertrophy
- NFAT:
-
Nuclear factor of activated T-cells
- OB:
-
Osteoblasts
- oc:
-
Osteocytes
- PHEX:
-
Pi-regulating gene homologous to endopeptidase on X chromosome
- Pi:
-
Phosphate
- SGK1:
-
Serum/glucocorticoid-regulated kinase-1
- TIO:
-
Tumor-induced osteomalacia
- TNAP:
-
Non-tissue-specific alkaline phosphatase
- TRPV5:
-
Transient receptor potential vanilloid 5
- VC:
-
Vascular calcifications
- VDR:
-
Vitamin D receptor
- XLH:
-
Chromosome X-linked hypophosphatemia
- Αkl:
-
αKlotho
References
Vervloet M (2019) Renal and extrarenal effects of fibroblast growth factor 23. Nat Rev Nephrol 15(2):109–120. https://doi.org/10.1038/s41581-018-0087-2
Murali SK, Roschger P, Zeitz U, Andrukhova KK, Erben ORG (2016) FGF23 regulates bone mineralization in a 1,25(OH)2D3 and klotho-independent manner. J Bone Miner Res 31(1):129–142. https://doi.org/10.1002/jbmr.2606
Rausch S, Foller M (2022) The regulation of FGF23 under physiological and pathophysiological conditions. Pfügers Archiv Eur J Physiol 474:281–292. https://doi.org/10.1007/s00424-022-02668-w
Yamashita T, Yoshioka M, Itoh N (2000) Identification of a novel fibroblast growth factor, FGF-23, preferentially expressed in the ventrolateral thalamic nucleus of the brain. Biochem Biophys Res Commun 277:494–498. https://doi.org/10.1006/bbrc.2000.3696
ADHR-CONSORTIUM (2000) Autosomal dominant hypophosphataemic rickets is associated with mutations in FGF23. Nat Genet 26:345–348. https://doi.org/10.1038/81664
Shimada T, Mizutani S, Muto T, Yoneya T, Hino R, Takeda S, Takeuchi Y, Fujita T, Fukumoto S, Yamashita T (2001) Cloning and characterization of FGF23 as a causative factor of tumor-induced osteomalacia. Proc Natl Acad Sci USA 98:6500–6505. https://doi.org/10.1073/pnas.101545198
Aono Y, Yamazaki Y, Yasutake J, Kawata T, Hasegawa H, Urakawa I, Fujita T, Wada M, Yamashita T, Fukumoto S, Shimada T (2009) Therapeutic effects of anti-FGF23 antibodies in hypophosphatemic rickets/osteomalacia. J Bone Miner Res 24(11):1879–1888. https://doi.org/10.1359/jbmr.090509
Kritmetapak K, Kumar R (2023) Phosphatonins: from discovery to therapeutics. Endocr Pract 29(1):69–79. https://doi.org/10.1016/j.eprac.2022.09.007
Isakova T, Cai X, Lee J, Mehta R, Zhang X, Yang W, Nessel L, Anderson AH, Lo J, Porter A, Nunes JW, Negrea L, Hamm L, Horwitz E, Chen J, Scialla JJ, de Boer IH, Leonard MB, Feldman HI, Wolf M (2020) Longitudinal evolution of markers of mineral metabolism in patients with CKD: the chronic renal insufficiency cohort (CRIC) study. Am J Kidney Dis 75:235–244. https://doi.org/10.1053/j.ajkd.2019.07.022
Bergwitz C, Jüppner H (2010) Regulation of phosphate homeostasis by PTH, vitamin D, and FGF23. Annu Rev Med 61:91–104. https://doi.org/10.1146/annurev.med.051308.111339
Ritter CS, Zhang S, Delmez J, Finch JL, Slatopolsky E (2015) Differential expression and regulation of Klotho by paricalcitol in the kidney, parathyroid, and aorta of uremic rats. Kidney Int 87:1141–1152. https://doi.org/10.1038/ki.2015.22
Quarles LD (2019) Fibroblast growth factor 23 and α-Klotho co-dependent and independent functions. Curr Opin Nephrol Hypertens 28(1):16–25. https://doi.org/10.1097/MNH.0000000000000467
Michigami T (2022) Roles of osteocytes in phosphate metabolism. Front Endocrinol 13:967774. https://doi.org/10.3389/fendo.2022.967774
Noonan ML, White KE (2019) FGF23 synthesis and activity. Curr Mol Biol Rep 5(1):18–25. https://doi.org/10.1007/s40610-019-0111-8
Leifheit-Nestler M, Grabner A, Hermann L, Richter B, Schmitz K, Fischer DC, Yanucil C, Faul C, Haffner D (2017) Vitamin D treatment attenuates cardiac FGF23/FGFR4 signaling and hypertrophy in uremic rats. Nephrol Dial Transplant 32:1493–1503. https://doi.org/10.1093/ndt/gfw454
Matsui I, Oka T, Kusunoki Y, Mori D, Hashimoto N, Matsumoto A, Shimada K, Yamaguchi S, Kubota K, Yonemoto S, Higo T, Sakaguchi Y, Takabatake Y, Hamano T, Isaka Y (2018) Cardiac hypertrophy elevates serum levels of fibroblast growth factor 23. Kidney Int 94:60–71. https://doi.org/10.1016/j.kint.2018.02.018
Yamazaki Y, Tamada T, Kasai N, Urakawa I, Aono Y, Hasegawa H, Fujita T, Kuroki R, Yamashita T, Fukumoto S, Shimada T (2008) Anti-FGF23 neutralizing antibodies show the physiological role and structural features of FGF23. J Bone Miner Res 23(9):1509–1518. https://doi.org/10.1359/jbmr.080417
Richter B, Faul C (2018) FGF23 actions on target tissues-with and without Klotho. Front Endocrinol 9:189. https://doi.org/10.3389/fendo.2018.00189
White KE, Carn G, Lorenz-Depiereux B, Benet-Pages A, Strom TM, Econs MJ (2001) Autosomal-dominant hypophosphatemic rickets (ADHR) mutations stabilize FGF-23. Kidney Int 60(6):2079–2086. https://doi.org/10.1046/j.1523-1755.2001.00064.x
Faul C, Amaral AP, Oskouei B, Hu MC, Sloan A, Isakova T, Gutierrez OM, Aguillon-Prada R, Lincoln J, Hare JM, Mundel P, Morales A, Scialla J, Fischer M, Soliman EZ, Chen J, Go AS, Rosas SE, Nessel L, Townsend RR, Feldman HI, John Sutton M, Ojo A, Gadegbeku C, Di Marco GS, Reuter S, Kentrup D, Tiemann K, Brand M, Hill JA, Moe OW, Kuro-O M, Kusek JW, Keane MG, Wolf M (2011) FGF23 induces left ventricular hypertrophy. J Clin Invest 121(11):4393–4408. https://doi.org/10.1172/JCI46122
Tagliabracci V, Engel JL, Wiley SE, Xiao J, Gonzalez DJ, Nidumanda Appaiah H, Koller A, Nizet V, White KE, Dixon JE (2014) Dynamic regulation of FGF23 by Fam20C phosphorylation, GalNAc-T3 glycosylation, and furin proteolysis. Proc Natl Acad Sci USA 111(15):5520–5525. https://doi.org/10.1073/pnas.1402218111
Ho BB, Bergwitz C (2021) FGF23 Signalling and physiology. J Mol Endocrinol 66(2):R23–R32. https://doi.org/10.1530/JME-20-0178
Chande S, Bergwitz C (2018) Role of phosphate sensing in bone and mineral metabolism. Nat Rev Endocrinol 14:637–655. https://doi.org/10.1038/s41574-018-0076-3
Goetz R, Beenken A, Ibrahimi OA, Kalinina J, Olsen SK, Eliseenkova AV, Xu C, Neubert TA, Zhang F, Linhardt RJ, Yu X, White KE, Inagaki T, Kliewer SA, Yamamoto M, Kurosu H, Ogawa Y, Kuo-o M, Lanske B, Razzaque MS, Mohammadi M (2007) Molecular insights into the klotho-dependent, endocrine mode of action of fibroblast growth factor 19 subfamily members. Moll Cell Biol 27:3417–3428. https://doi.org/10.1128/MCB.02249-06
Kato K, Jeanneau C, Tarp MA, Benet-Pagès A, Lorenz-Depiereux B, Bennett EP, Mandel U, Strom TM, Clausen H (2006) Polypeptide GalNAc-transferase T3 and familial tumoral calcinosis. Secretion of fibroblast growth factor 23 requires O-glycosylation. J Biol Chem 281:18370–18377. https://doi.org/10.1074/jbc.M602469200
Ichikawa S, Imel EA, Sorenson AH, Severe R, Knudson P, Harris GJ, Shaker JL, Econs MJ (2006) Tumoral calcinosis presenting with eyelid calcifications due to novel missense mutations in the glycosyl transferase domain of the GALNT3 gene. J Clin Endocrinol Metab 91(11):4472–4475. https://doi.org/10.1210/jc.2006-1247
Kuro-o M, Matsumura Y, Aizawa H, Kawaguchi H, Suga T, Utsugi T, Ohyama Y, Kurabayashi M, Kaname T, Kume E, Iwasaki H, Iida A, Shiraki-Iida T, Nishikawa S, Nagai R, Nabeshima YI (1997) Mutation of the mouse klotho gene leads to a syndrome resembling ageing. Nature 390(6655):45–51. https://doi.org/10.1038/36285
Komaba H, Kaludjerovic J, Hu DZ, Nagano K, Amano K, Ide N, Sato T, Densmore MJ, Hanai JI, Olauson H, Bellido T, Larsson TE, Baron R, Lanske B (2017) Klotho expression in osteocytes regulates bone metabolism and controls bone formation. Kidney Int 92(3):599–611. https://doi.org/10.1016/j.kint.2017.02.014
Shiraki-Iida T, Aizawa H, Matsumura Y, Sekine S, Iida A, Anazawa H, Nagai R, Kuro-o M, Nabeshima Y (1998) Structure of the mouse klotho gene and its two transcripts encoding membrane and secreted protein. FEBS Lett 424(1–2):6–10. https://doi.org/10.1016/s0014-5793(98)00127-6
Navarro-García JA, Fernández-Velasco M, Delgado C, Delgado JF, Kuro-o M, Ruilope LM, Ruiz-Hurtado G (2018) PTH, vitamin D, and the FGF-23-klotho axis and heart: going beyond the confines of nephrology. Eur J Clin Invest. https://doi.org/10.1111/eci.12902
Ornitz DM, Itoh N (2001) Fibroblast growth factors. Genome Biol 2(3):3005. https://doi.org/10.1186/gb-2001-2-3-reviews3005
Turner N, Grose R (2010) Fibroblast growth factor signalling: from development to cancer. Nat Rev Cancer 10(2):116–129. https://doi.org/10.1038/nrc2780
Goetz R, Ohnishi M, Kir S, Kurosu H, Wang L, Pastor J, Ma J, Gai W, Kuro-o M, Razzaque MS, Mohammadi M (2012) Conversion of a paracrine fibroblast growth factor into an endocrine fibroblast growth factor. J Biol Chem 287(34):29134–29146. https://doi.org/10.1074/jbc.M112.342980
Suzuki Y, Kuzina E, An SJ, Tome F, Mohanty F, Li W, Lee S, Liu Y, Lax I, Schlessinger J (2020) FGF23 contains two distinct high-affinity binding sites enabling bivalent interactions with α-Klotho. Proc Natl Acad Sci USA 117(50):31800–31807. https://doi.org/10.1073/pnas.2018554117
Yanucil C, Kentrup D, Campos I, Czaya B, Heitman K, Westbrook D, Osis G, Grabner A, Wende AR, Vallejo J, Wacker MJ, Navarro-Garcia JA, Ruiz-Hurtado G, Zhang F, Song Y, Linhardt RJ, White K, Kapiloff MS, Faul C (2022) Soluble α-klotho and heparin modulate the pathologic cardiac actions of fibroblast growth factor 23 in chronic kidney disease. Kidney Int 102(2):261–279. https://doi.org/10.1016/j.kint.2022.03.028
Miyagawa K, Yamazaki M, Kawai M, Nishino J, Koshimizu T, Ohata Y, Tachikawa K, Mikuni-Takagaki Y, Kogo M, Ozono K, Michigami T (2014) Dysregulated gene expression in the primary osteoblasts and osteocytes isolated from hypophosphatemic hyp mice. PLoS ONE 9(4):e93840. https://doi.org/10.1371/journal.pone.0093840
Dussold C, Gerber C, White S, Wang X, Qi L, Francis C, Capella M, Courbon G, Wang J, Li C, Feng JQ, Isakova T, Wolf M, David V, Martin A (2019) DMP1 prevents osteocyte alterations, FGF23 elevation and left ventricular hypertrophy in mice with chronic kidney disease. Bone Res 7:12. https://doi.org/10.1038/s41413-019-0051-1
Martin A, Liu S, David V, Li H, Karydis A, Feng JQ, Quarles LD (2011) Bone proteins PHEX and DMP1 regulate fibroblastic growth factor Fgf23 expression in osteocytes through a common pathway involving FGF receptor (FGFR) signaling. FASEB J 25(8):2551–2562. https://doi.org/10.1096/fj.10-177816
Liu C, Zhang H, Jani P, Wang X, Lu Y, Li N, Xiao J, Qin C (2018) FAM20C regulates osteoblast behaviors and intracellular signaling pathways in a cell-autonomous manner. J Cell Physiol 233(4):3476–3486. https://doi.org/10.1002/jcp.26200
Ito N, Prideaux M, Wijenayaka AR, Yang D, Ormsby RT, Bonewald LF, Atkins GJ (2021) Sclerostin directly stimulates osteocyte synthesis of fibroblast growth factor-23. Calcif Tissue Int 109(1):66–76. https://doi.org/10.1007/s00223-021-00823-6
Razzaque MS (2022) Interactions between FGF23 and vitamin D. Endocr Connect 11(10):e220239. https://doi.org/10.1530/EC-22-0239
Zittermann A, Berthold HK, Pilz S (2021) The effect of vitamin D on fibroblast growth factor 23: a systematic review and meta-analysis of randomized controlled trials. Eur J Clin Nutr 75:980–987. https://doi.org/10.1038/s41430-020-00725-0
Meshkini F, Soltani S, Clark CCT, Tam V, Meyre D, Toupchian O, Saraf-Bank S, Abdollahi S (2022) The effect of vitamin D supplementation on serum levels of fibroblast growth factor-23: a systematic review and meta-analysis of randomized controlled trials. J Steroid Biochem Mol Biol 215:106012. https://doi.org/10.1016/j.jsbmb.2021.106012
Kolek OI, Hines ER, Jones MD, LeSueur LK, Lipko MA, Kiela PR, Collins JF, Haussler MR, Ghishan FK (2005) 1alpha,25-Dihydroxyvitamin D3 upregulates FGF23 gene expression in bone: the final link in a renal-gastrointestinal-skeletal axis that controls phosphate transport. Am J Physiol Gastrointest Liver Physiol 289(6):G1036–G1042. https://doi.org/10.1152/ajpgi.00243.2005
Masuyama R, Stockmans I, Torrekens S, Van Looveren R, Maes C, Carmeliet P, Bouillon R, Carmeliet G (2006) Vitamin D receptor in chondrocytes promotes osteoclastogenesis and regulates FGF23 production in osteoblasts. J Clin Invest 116(12):3150–3159. https://doi.org/10.1172/JCI29463
Nguyen-Yamamoto L, Karaplis AC, St-Arnaud R, Goltzman D (2017) Fibroblast growth factor 23 regulation by systemic and local osteoblast-synthesized 1,25-dihydroxyvitamin D. J Am Soc Nephrol 28(2):586–597. https://doi.org/10.1681/ASN.2016010066
Saji F, Shigematsu T, Sakaguchi T, Ohya M, Orita H, Maeda Y, Ooura M, Mima T, Negi S (2010) Fibroblast growth factor 23 production in bone is directly regulated by 1{alpha},25-dihydroxyvitamin D, but not PTH. Am J Physiol Renal Physiol 299(5):F1212–F1217. https://doi.org/10.1152/ajprenal.00169.2010
Lanske B, Razzaque MS (2014) Molecular interactions of FGF23 and PTH in phosphate regulation. Kidney Int 86(6):1072–1074. https://doi.org/10.1038/ki.2014.316
Kobayashi K, Imanishi Y, Miyauchi A, Onoda N, Kawata T, Tahara H, Goto H, Miki T, Ishimura E, Sugimoto T, Ishikawa T, Inaba M, Nishizawa Y (2006) Regulation of plasma fibroblast growth factor 23 by calcium in primary hyperparathyroidism. Eur J Endocrinol 154(1):93–99. https://doi.org/10.1530/eje.1.02053
Yamashita H, Yamashita T, Miyamoto M, Shigematsu T, Kazama JJ, Shimada T, Yamazaki Y, Fukumoto S, Fukagaw M, Noguchi S (2004) Fibroblast growth factor (FGF)-23 in patients with primary hyperparathyroidism. Eur J Endocrinol 151(1):55–60. https://doi.org/10.1530/eje.0.1510055
Knab VM, Corbin B, Andrukhova O, Hum JM, Ni P, Rabadi S, Maeda A, White KE, Erben RG, Jüppner H, Christov M (2017) Acute parathyroid hormone injection increases C-terminal but not intact fibroblast growth factor 23 levels. Endocrinology 158(5):1130–1139. https://doi.org/10.1210/en.2016-1451
Onal M, Carlson AH, Thostenson JD, Benkusky NA, Meyer MB, Lee SM, Pike JW (2018) A novel distal enhancer mediates inflammation-, PTH-, and early onset murine kidney disease-induced expression of the mouse Fgf23 gene. JBMR Plus 2(1):32–47. https://doi.org/10.1002/jbm4.10023
Wolf M (2010) Forging forward with 10 burning questions on FGF23 in kidney disease. J Am Soc Nephrol 21(9):1427–1435. https://doi.org/10.1681/asn.2009121293
Mace ML, Olgaard K, Lewin E (2020) New aspects of the kidney in the regulation of fibroblast growth factor 23 (FGF23) and mineral homeostasis. Int J Mol Sci 21(22):8810
Shimada T, Yamazaki Y, Takahashi M, Hasegawa H, Urakawa I, Oshima T, Ono K, Kakitani M, Tomizuka K, Fujita T, Fukumoto S, Yamashita T (2005) Vitamin D receptor-independent FGF23 actions in regulating phosphate and vitamin D metabolism. Am J Physiol Renal Physiol 289(5):F1088-1095. https://doi.org/10.1152/ajprenal.00474.2004
Rodriguez-Ortiz ME, Lopez I, Muñoz-Castañeda JR, Martinez-Moreno JM, Peralta Ramírez A, Pineda C, Canalejo A, Jaeger P, Aguilera-Tejero E, Rodriguez M, Felsenfeld A, Almaden Y (2012) Calcium deficiency reduces circulating levels of FGF23. J Am Soc Nephrol 23(7):1190–1197. https://doi.org/10.1681/ASN.2011101006
David V, Dai B, Martin A, Huang J, Han X, Quarles LD (2013) Calcium regulates FGF-23 expression in bone. Endocrinology 154(12):4469–4482. https://doi.org/10.1210/en.2013-1627
Quinn SJ, Thomsen AR, Pang JL, Kantham L, Bräuner-Osborne H, Pollak M, Goltzman D, Brown EM (2013) Interactions between calcium and phosphorus in the regulation of the production of fibroblast growth factor 23 in vivo. Am J Physiol Endocrinol Metab 304(3):E310-320. https://doi.org/10.1152/ajpendo.00460.2012
Akiyama KI, Miura Y, Hayashi H, Sakata A, Matsumura Y, Kojima M, Tsuchiya K, Nitta K, Shiizaki K, Kurosu H, Kuro-o M (2020) Calciprotein particles regulate fibroblast growth factor-23 expression in osteoblasts. Kidney Int 97(4):702–712. https://doi.org/10.1016/j.kint.2019.10.019
Thein OS, Ali NA, Mahida RY, Dancer RCA, Ostermann M, Amrein K, Martucci G, Scott A, Thickett DR, Parekh D (2023) Raised FGF23 correlates to increased mortality in critical illness, independent of Vitamin D. Biology (Basel) 12(2):309. https://doi.org/10.3390/biology12020309
Perwad F, Azam N, Zhang MY, Yamashita T, Tenenhouse HS, Portale AA (2005) Dietary and serum phosphorus regulate fibroblast growth factor 23 expression and 1,25-dihydroxyvitamin D metabolism in mice. Endocrinology 146(12):5358–5864. https://doi.org/10.1210/en.2005-0777
Nishida Y, Taketani Y, Yamanaka-Okumura H, Imamura F, Taniguchi A, Sato T, Shuto E, Nashiki K, Arai H, Yamamoto H, Takeda E (2006) Acute effect of oral phosphate loading on serum fibroblast growth factor 23 levels in healthy men. Kidney Int 70(12):2141–2147. https://doi.org/10.1038/sj.ki.5002000
Antoniucci DM, Yamashita T, Portale AA (2006) Dietary phosphorus regulates serum fibroblast growth factor-23 concentrations in healthy men. J Clin Endocrinol Metab 91(8):3144–3149. https://doi.org/10.1210/jc.2006-0021
Larsson T, Nisbeth U, Ljunggren O, Jüppner H, Jonsson KB (2003) Circulating concentration of FGF-23 increases as renal function declines in patients with chronic kidney disease, but does not change in response to variation in phosphate intake in healthy volunteers. Kidney Int 64(6):2272–2279. https://doi.org/10.1046/j.1523-1755.2003.00328.x
Tsai WC, Wu HY, Peng YS, Hsu SP, Chiu YL, Yang JY, Chen HY, Pai MF, Lin WY, Hung KY, Chu FY, Tsai SM, Chien KL (2019) Short-term effects of very-low-phosphate and low-phosphate diets on fibroblast growth factor 23 in hemodialysis patients: a randomized crossover trial. Clin J Am Soc Nephrol 14(10):1475–1483. https://doi.org/10.2215/CJN.04250419
Isakova T, Gutiérrez OM, Smith K, Epstein M, Keating LK, Jüppner H, Wolf M (2011) Pilot study of dietary phosphorus restriction and phosphorus binders to target fibroblast growth factor 23 in patients with chronic kidney disease. Nephrol Dial Transplant 26(2):584–591. https://doi.org/10.1093/ndt/gfq419
Oliveira RB, Cancela AL, Graciolli FG, Dos Reis LM, Draibe SA, Cuppari L, Carvalho AB, Jorgetti V, Canziani ME, Moysés RM (2010) Early control of PTH and FGF23 in normophosphatemic CKD patients: a new target in CKD-MBD therapy? Clin J Am Soc Nephrol 5(2):286–291
Memmos E, Papagianni A (2021) New insights into the role of FGF-23 and Klotho in cardiovascular disease in chronic kidney disease patients. Curr Vasc Pharmacol 19(1):55–62. https://doi.org/10.2174/1570161118666200420102100
Hori M, Kinoshita Y, Taguchi M, Fukumoto S (2016) Phosphate enhances Fgf23 expression through reactive oxygen species in UMR-106 cells. J Bone Miner Metab 34(2):132–139. https://doi.org/10.1007/s00774-015-0651-9
Heijboer AC, Cavalier E (2023) The measurement and interpretation of fibroblast growth factor 23 (FGF23) concentrations. Calcif Tissue Int 112(2):258–270. https://doi.org/10.1007/s00223-022-00987-9
Kato H, Miyazaki H, Kimura T, Hoshino Y, Hidaka N, Koga M, Nangaku M, Makita N, Ito N (2023) Clinical performance of a new intact FGF23 immunoassay in healthy individuals and patients with chronic hypophosphatemia. Bone Rep 18:101659. https://doi.org/10.1016/j.bonr.2023.101659
Bouma-de Krijger A, Vervloet MG (2020) Fibroblast growth factor 23: are we ready to use it in clinical practice? J Nephrol 33(3):509–527. https://doi.org/10.1007/s40620-020-00715-2
Pons-Belda OD, Alonso-Álvarez MA, González-Rodríguez JD, Mantecón-Fernández L, Santos-Rodríguez F (2023) Mineral metabolism in children: interrelation between vitamin D and FGF23. Int J Mol Sci 24(7):6661. https://doi.org/10.3390/ijms24076661
Lerch C, Shroff R, Wan M, Rees L, Aitkenhead H, Kaplan Bulut I, Thurn D, Karabay Bayazit A, Niemirska A, Canpolat N, Duzova A, Azukaitis K, Yilmaz E, Yalcinkaya F, Harambat J, Kiyak A, Alpay H, Habbig S, Zaloszyc A, Soylemezoglu O, Candan C, Rosales A, Melk A, Querfeld U, Leifheit-Nestler M, Sander A, Schaefer F, Haffner D, 4C Study Consortium; ESPN CKD-MBD Working Group (2018) Effects of nutritional vitamin D supplementation on markers of bone and mineral metabolism in children with chronic kidney disease. Nephrol Dial Transplant 33(12):2208–2217. https://doi.org/10.1093/ndt/gfy012
Aurelle M, Basmaison O, Ranchin B, Kassai-Koupai B, Sellier-Leclerc AL, Bertholet-Thomas A, Bacchetta J (2020) Intermittent cholecalciferol supplementation in children and teenagers followed in pediatric nephrology: data from a prospective single-center single-arm open trial. Eur J Pediatr 179(4):661–669. https://doi.org/10.1007/s00431-019-03553-y
Sheriff A, Mathew G, Sinha A, Hari S, Gupta N, Ramakrishnan L, Hari P, Bagga A (2022) Short-term effects of cholecalciferol supplementation on cFGF23 levels in children with chronic kidney disease and vitamin D insufficiency. Indian J Pediatr 89(10):1037–1039. https://doi.org/10.1007/s12098-022-04247-4
Ali FN, Josefson J, Mendez AJ, Mestan K, Wolf M (2016) Cord blood ferritin and fibroblast growth factor-23 levels in neonates. J Clin Endocrinol Metab 101(4):1673–1679. https://doi.org/10.1210/jc.2015-3709
Fischer DC, Mischek A, Wolf S, Rahn A, Salweski B, Kundt G, Haffner D (2012) Paediatric reference values for the C-terminal fragment of fibroblast-growth factor-23, sclerostin, bone-specific alkaline phosphatase and isoform 5b of tartrate-resistant acid phosphatase. Ann Clin Biochem 49(Pt 6):546–553. https://doi.org/10.1258/acb.2012.011274
Stanczyk M, Chrul S, Wyka K, Tkaczyk M (2021) Serum intact fibroblast growth factor 23 in healthy paediatric population. Open Med (Wars) 16(1):1022–1027
Andrukhova O, Zeitz U, Goetz R, Mohammadi M, Lanske B, Erben RG (2012) FGF23 acts directly on renal proximal tubules to induce phosphaturia through activation of the ERK1/2-SGK1 signaling pathway. Bone 51(3):621–628. https://doi.org/10.1016/j.bone.2012.05.015
Kawai M (2016) The FGF23/Klotho axis in the regulation of mineral and metabolic homeostasis. Horm Mol Biol Clin Investig 28(1):55–67. https://doi.org/10.1515/hmbci-2015-0068
Ide N, Olauson H, Sato T, Densmore MJ, Wang H, Hanai J, Larsson T, Lanske B (2016) In vivo evidence for a limited role of proximal tubular Klotho in renal phosphate handling. Kidney Int 90(2):348–362. https://doi.org/10.1016/j.kint.2016.04.009
Blau JE, Collins MT (2015) The PTH-vitamin D-FGF23 axis. Rev Endocr Metab Disord 16:165–174. https://doi.org/10.1007/s11154-015-9318-z
Latic N, Erben RG (2022) Interaction of vitamin D with peptide hormones with emphasis on parathyroid hormone, FGF23, and the renin-angiotensin-aldosterone system. Nutrients 14(23):5186. https://doi.org/10.3390/nu14235186
Ben-Dov IZ, Galitzer H, Lavi-Moshayoff V, Goetz R, Kuro-o M, Mohammadi M, Sirkis R, Naveh-Many T, Silver J (2007) The parathyroid is a target organ for FGF23 in rats. J Clin Invest 117:4003–4008. https://doi.org/10.1172/JCI32409
Han X, Cai C, Xiao Z, Quarles LD (2020) FGF23 induced left ventricular hypertrophy mediated by FGFR4 signaling in the myocardium is attenuated by soluble Klotho in mice. J Mol Cell Cardiol 138:66–74. https://doi.org/10.1016/j.yjmcc.2019.11.149
Singh S, Grabner A, Yanucil C, Schramm K, Czaya B, Krick S, Czaja MJ, Bartz R, Abraham R, Di Marco GS, Brand M, Wolf M, Faul C (2016) Fibroblast growth factor 23 directly targets hepatocytes to promote inflammation in chronic kidney disease. Kidney Int 90(5):985–996. https://doi.org/10.1016/j.kint.2016.05.019
Vogt I, Haffner D, Leifheit-Nestler M (2019) FGF23 and phosphate-cardiovascular toxins in CKD. Toxins (Basel) 11(11):647. https://doi.org/10.3390/toxins11110647
Leifheit-Nestler M, Haffner D (2021) How FGF23 shapes multiple organs in chronic kidney disease. Mol Cell Pediatr 8(1):12. https://doi.org/10.1186/s40348-021-00123-x
Yamada S, Giachelli CM (2017) Vascular calcification in CKD-MBD: roles for phosphate, FGF23, and Klotho. Bone 100:87–93. https://doi.org/10.1016/j.bone.2016.11.012
Figurek A, Rroji M, Spasovski G (2023) FGF23 in chronic kidney disease: bridging the heart and anemia. Cells 12(4):609. https://doi.org/10.3390/cells12040609
Muras-Szwedziak K, Pawłowicz-Szlarska E, Nowicki M (2023) Effect of intravenous iron on endogenous erythropoietin and FGF-23 secretion in patients with chronic kidney disease. Ren Fail 45(1):2164305. https://doi.org/10.1080/0886022X.2022.2164305
Lindberg K, Amin R, Moe OW, Hu M, Erben RG, Östman Wernerson A, Lanske B, Olauson H, Larsoon TE (2014) The kidney is the principal organ mediating klotho effects. J Am Soc Nephrol 25(10):2169–2175. https://doi.org/10.1681/ASN.2013111209
Sakan H, Nakatani K, Asai O, Imura A, Tanaka T, Yoshimoto S, Iwamoto N, Kurumatami N, Iwano M, Nabeshima I, Konishi N, Saito Y (2014) Reduced renal alpha-Klotho expression in CKD patients and its effect on renal phosphate handling and vitamin D metabolism. PLoS ONE 9(1):e86301. https://doi.org/10.1371/journal.pone.0086301
Eisenga MF, De Jong MA, Van der Meer P, Leaf DE, Huls G, Nolte IM, Gaillard CA, Bakker SJL, De Borst MH (2019) Iron deficiency, elevated erythropoietin, fibroblast growth factor 23, and mortality in the general population of the Netherlands: a cohort study. PLoS Med 16(6):e1002818. https://doi.org/10.1371/journal.pmed.1002818
Hain D, Bednarski D, Cahill M, Dix A, Foote B, Haras MS, Pace R, Gutierrez OM (2023) Iron-deficiency anemia in CKD: a narrative review for the kidney care team. Kidney Med 5(8):100677. https://doi.org/10.1016/j.xkme.2023.100677
Imel EA, Liu Z, Coffman M, Acton D, Mehta R, Econs MJ (2020) Oral iron replacement normalizes fibroblast growth factor 23 in iron-deficient patients with autosomal dominant hypophosphatemic rickets. J Bone Miner Res 35(2):231–238. https://doi.org/10.1002/jbmr.3878
Artunc F, Risler T (2007) Serum erythropoietin concentrations and responses to anaemia in patients with or without chronic kidney disease. Nephrol Dial Transplant 22(10):2900–2908. https://doi.org/10.1093/ndt/gfm316
Afsar B, Kanbay M, Afsar RE (2022) Interconnections of fibroblast growth factor 23 and klotho with erythropoietin and hypoxia-inducible factor. Mol Cell Biochem 477(7):1973–1985. https://doi.org/10.1007/s11010-022-04422-3
Eitner F, Richter B, Schwänen S, Szaroszyk M, Vogt I, Grund A, Thum T, Heineke J, Haffner D, Leifheit-Nestler M (2022) Comprehensive expression analysis of cardiac fibroblast growth factor 23 in health and pressure-induced cardiac hypertrophy. Front Cell Dev Biol 9:791479. https://doi.org/10.3389/fcell.2021.791479
Akhabue E, Montag S, Reis JP, Pool LR, Mehta R, Yancy CW, Zhao L, Wolf M, Gutierrez OM, Carnethon MR, Isakova T (2018) FGF23 (fibroblast growth factor-23) and incident hypertension in young and middle-aged adults: the CARDIA study. Hypertension 72(1):70–76. https://doi.org/10.1161/HYPERTENSIONAHA.118.11060
Andrukhova O, Slavic S, Smorodchenko A, Zeitz U, Shalhoub V, Lanske B, Pohl EE, Erben RG (2014) FGF23 regulates renal sodium handling and blood pressure. EMBO Mol Med 6(6):744–59. https://doi.org/10.1002/emmm.201303716
Kanbay M, Demiray A, Afsar B, Covic A, Tapoi L, Ureche C, Ortiz A (2021) Role of klotho in the development of essential hypertension. Hypertension 77(3):740–750. https://doi.org/10.1161/HYPERTENSIONAHA.120.16635
Yamazaki Y, Imura A, Urakawa I, Shimada T, Murakami J, Aono Y, Hasegawa H, Yamashita T, Nakatani K, Saito Y, Okamoto N, Kurumatani N, Namba N, Kitaoka T, Ozono K, Sakai T, Hataya H, Ichikawa S, Imel EA, Econs MJ, Nabeshima Y (2010) Establishment of sandwich ELISA for soluble alpha-Klotho measurement: age-dependent change of soluble alpha-Klotho levels in healthy subjects. Biochem Biophys Res Commun 398(3):513–8. https://doi.org/10.1016/j.bbrc.2010.06.110
Citterio L, Delli Carpini S, Lupoli S, Brioni E, Simonini M, Fontana S, Zagato L, Messaggio E, Barlassina C, Cusi D, Manunta P, Lanzani C (2020) Klotho gene in human salt-sensitive hypertension. Clin J Am Soc Nephrol 15(3):375–383. https://doi.org/10.2215/CJN.08620719
Nanba K, Vaidya A, Williams GH, Zheng I, Else T, Rainey WE (2017) Age-related autonomous aldosteronism. Circulation 136(4):347–355. https://doi.org/10.1161/CIRCULATIONAHA.117.028201
Gao P, Xu TT, Lu J, Li L, Xu J, Hao DL, Chen HZ, Liu DP (2014) Overexpression of SIRT1 in vascular smooth muscle cells attenuates angiotensin II-induced vascular remodeling and hypertension in mice. J Mol Med (Berl) 92(4):347–357. https://doi.org/10.1007/s00109-013-1111-4
Kitagawa M, Sugiyama H, Morinaga H, Inoue T, Takiue K, Ogawa A, Yamanari T, Kikumoto Y, Uchida HA, Kitamura S, Maeshima Y, Nakamura K, Ito H, Makino H (2013) A decreased level of serum soluble Klotho is an independent biomarker associated with arterial stiffness in patients with chronic kidney disease. PLoS ONE 8(2):e56695. https://doi.org/10.1371/journal.pone.0056695
Richter B, Haller J, Haffner D, Leifheit-Nestler M (2016) Klotho modulates FGF23-mediated NO synthesis and oxidative stress in human coronary artery endothelial cells. Pflugers Arch 468(9):1621–1635. https://doi.org/10.1007/s00424-016-1858-x
Courbebaisse M, Lanske B (2018) Biology of fibroblast growth factor 23: from physiology to pathology. Cold Spring Harb Perspect Med 8(5):a031260. https://doi.org/10.1101/cshperspect.a031260
Zuo Q, Yang W, Liu B, Yan D, Wang Z, Wang H, Deng W, Cao X, Yang J (2022) A novel FGF23 mutation in hyperphosphatemic familial tumoral calcinosis and its deleterious effect on protein O-glycosylation. Front Endocrinol (Lausanne) 13:1008800. https://doi.org/10.3389/fendo.2022.1008800
Huang T, He Y, Li Y, Zang H, Wang Q, Gao Y (2024) The relationship between serum fibroblast growth factor 23 and klotho protein and low bone mineral density in middle-aged and elderly patients with end-stage renal disease. Horm Metab Res 56(2):142–149. https://doi.org/10.1055/a-2168-5089
Lima F, Monier-Faugere MC, Mawad H, David V, Malluche HH (2023) FGF-23 and sclerostin in serum and bone of CKD patients. Clin Nephrol 99(5):209–218. https://doi.org/10.5414/CN111111
Zhang H, Xiang G, Li J, He S, Wang Y, Deng A, Wang Y, Guo C (2023) Promotion effect of FGF23 on osteopenia in congenital scoliosis through FGFr3/TNAP/OPN pathway. Chin Med J (Engl) 136(12):1468–1477. https://doi.org/10.1097/CM9.0000000000002690
Liu Y, Cheng Y, Sun M, Hao X, Li M (2023) Analysis of serum insulin-like growth factor-1, fibroblast growth factor 23, and Klotho levels in girls with rapidly progressive central precocious puberty. Eur J Pediatr 182(11):5007–5013. https://doi.org/10.1007/s00431-023-05174-y
Ewendt F, Feger M, Föller M (2021) Role of fibroblast growth factor 23 (FGF23) and αKlotho in cancer. Front Cell Dev Biol 8:601006. https://doi.org/10.3389/fcell.2020.601006
Boland JM, Tebben PJ, Folpe AL (2018) Phosphaturic mesenchymal tumors: what an endocrinologist should know. J Endocrinol Invest 41(10):1173–1184. https://doi.org/10.1007/s40618-018-0849-5
Minisola S, Peacock M, Fukumoto S, Cipriani C, Pepe J, Tella SH, Collins MT (2017) Tumour-induced osteomalacia. Nat Rev Dis Primers 3:17044. https://doi.org/10.1038/nrdp.2017.44
Mansinho A, Ferreira AR, Casimiro S, Alho I, Vendrell I, Costa AL, Sousa R, Abreu C, Pulido C, Macedo D, Pacheco TR, Correia L, Costa L (2019) Levels of circulating fibroblast growth factor 23 (FGF23) and prognosis in cancer patients with bone metastases. Int J Mol Sci 20(3):695. https://doi.org/10.3390/ijms20030695
Feng S, Wang J, Zhang Y, Creighton CJ, Ittmann M (2015) FGF23 promotes prostate cancer progression. Oncotarget 6(19):17291–17301. https://doi.org/10.18632/oncotarget.4174
Choudhary S, Ramasundaram P, Dziopa E, Mannion C, Kissin Y, Tricoli L, Albanese C, Lee W, Zilberberg J (2018) Human ex vivo 3D bone model recapitulates osteocyte response to metastatic prostate cancer. Sci Rep 8(1):17975. https://doi.org/10.1038/s41598-018-36424-x
Cymbaluk-Płoska A, Gargulińska P, Chudecka-Głaz A, Kwiatkowski S, Pius-Sadowska E, Machaliński B (2020) The suitability of FGF21 and FGF23 as new biomarkers in endometrial cancer patients. Diagnostics (Basel) 10(6):414. https://doi.org/10.3390/diagnostics10060414
Lamb YN (2018) Burosumab: first global approval. Drugs 78(6):707–714. https://doi.org/10.1007/s40265-018-0905-7
Kubota T, Namba N, Tanaka H, Muroya K, Imanishi Y, Takeuchi Y, Kanematsu M, Sun W, SeinoY OK (2023) Self-administration of burosumab in children and adults with X-linked hypophosphataemia in two open-label. Single-Arm Clinical Studies Adv Ther 40(4):1530–1545. https://doi.org/10.1007/s12325-022-02412-x
Ewert A, Rehberg M, Schlingmann KP, Hiort O, John-Kroegel U, Metzing O, Wühl E, Schaefer F, Kemper MJ, Derichs U, Richter-Unruh A, Patzer L, Albers N, Dunstheimer D, Haberland H, Heger S, Schröder C, Jorch N, Schmid E, Staude H, Weitz M, Freiberg C, Leifheit-Nestler M, Zivicnjak M, Schnabel D, Haffner D (2023) Effects of burosumab treatment on mineral metabolism in children and adolescents with X-linked hypophosphatemia. J Clin Endocrinol Metab 108(10):e998–e1006. https://doi.org/10.1210/clinem/dgad223
Levy-Shraga Y, Levi S, Regev R, Gal S, Brener A, Lebenthal Y, Gillis D, Strich D, Zung A, Cleper R, Borovitz Y, Bello R, Tenenbaum A, Zadik Z, Davidovits M, Zeitlin L, Tiosano D (2023) Linear growth of children with X-linked hypophosphatemia treated with burosumab: a real-life observational study. Eur J Pediatr 182(11):5191–5202. https://doi.org/10.1007/s00431-023-05190-y
Crotti C, Zucchi F, Alfieri C, Caporali R, Varenna M (2023) Long-term use of burosumab for the treatment of tumor-induced osteomalacia. Osteoporos Int 34(1):201–206. https://doi.org/10.1007/s00198-022-06516-6
Jan de Beur SM, Miller PD, Weber TJ, Peacock M, Insogna K, Kumar R, Rauch F, Luca D, Cimms T, Roberts MS, San Martin J, Carpenter TO (2021) Burosumab for the treatment of tumor-induced osteomalacia. J Bone Miner Res 36(4):627–635. https://doi.org/10.1002/jbmr.4233
Carpenter TO, Whyte MP, Imel EA, Boot AM, Högler W, Linglart A, Padidela R, Van’t Hoff W, Mao M, Chen CY, Skrinar A, Kakkis E, San Martin J, Portale AA (2018) Burosumab therapy in children with X-linked hypophosphatemia. N Engl J Med 378(21):1987–1998. https://doi.org/10.1056/NEJMoa1714641
Seefried L, Bravenboer N, Imel EA (2023) Editorial: rare musculoskeletal disorders: disease mechanisms and therapies. Front Endocrinol (Lausanne) 14:1215941. https://doi.org/10.3389/fendo.2023.1215941
Perwad F, Portale AA (2019) Burosumab therapy for X-linked hypophosphatemia and therapeutic implications for CKD. Clin J Am Soc Nephrol CJASN 14(7):1097. https://doi.org/10.2215/CJN.15201218
Verbueken D, Moe OW (2022) Strategies to lower fibroblast growth factor 23 bioactivity. Nephrol Dial Transplant 37(10):1800–1807. https://doi.org/10.1093/ndt/gfab012
Acknowledgements
This work was supported by grants from FONCYT (PICT-2018-1809), SECYT (UNC), Argentina. Prof. Dr. Nori Tolosa de Talamoni and Dr. Vanessa Areco are Members of Investigator Career from the Consejo Nacional de Investigaciones Científicas y Tecnológicas (CONICET), Argentina. The authors thank Darío Talamoni for his corrections in the English language.
Funding
This study was funded by Fondo para la Investigación Científica y Tecnológica (FONCYT), PICT 2018-1809, PICT 2018-1809, PICT 2018-1809, Secretaría de Ciencia y Tecnología (SECYT).
Author information
Authors and Affiliations
Contributions
MAR: Searched literature, Discussed topics, Checked the references, Prepared Figs 1 and 2, and Graphical Abstract MEPL: Searched literature, Discussed topics, VA: Searched literature, Discussed topics, Checked the references GDdeB: Searched literature, Discussed topics, Checked the references MPD: Searched literature, Discussed topics NTdeT: Had the original idea, Searched literature, Discussed topics, Wrote the main manuscript text All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rivoira, M.A., Peralta López, M.E., Areco, V. et al. Emerging concepts on the FGF23 regulation and activity. Mol Cell Biochem (2024). https://doi.org/10.1007/s11010-024-04982-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11010-024-04982-6