Abstract
Psoriasis is an inflammatory disease that changes plasma composition, and it is detectable by differential scanning calorimetry (DSC). Besides the general change in plasma, the aim of the study was to demonstrate which components are changing and how the anti-psoriatic drug treatment affects back all this. Retrospectively, blood plasma DSC data were analyzed from patients, who have different severities of symptoms and who received steroids (n = 10), or retinoids (n = 10), or biological drug treatment (n = 10). Complex curves were deconvoluted in several individual transitions (Tm1–Tm5), modeling each individual transition. In the examined psoriasis stages, the thermodynamic parameters excess heat capacity and enthalpy of the transitions in proportion corresponded to the targeted treatment and the degree of disease severity, as well as the numbers of transitions were determined from the calorimetric profiles. In conclusion, deconvoluted plasma DSC profiles showed similarities but exhibited marked differences in the thermal denaturation on different treated psoriasis stages. This examination has shown that drug therapy affects the composition of plasma proteins, which should be always considered for the evaluation of DSC results in similar studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Psoriasis is a lifelong skin disorder, which has different appearances and shapes (plaque, nail, scalp, guttate, inverse, pustular, and erythrodermic psoriasis), and in rare cases it can affect the joints (psoriatic arthritis). Symptoms are frequently categorized into two groups: mild or moderate to severe psoriasis. The classification is depending on the clinical severity of the lesions, the percentage of affected body surface area, and patient quality of life. Clinical diagnosis is usually based on full skin physical examination by a dermatologist, and rarely skin biopsy is useful to determine the exact type of psoriasis. In the case of joint involvement, radiological examinations (X-ray, ultrasound, and MRI) should be necessary to confirm the diagnosis. At present, specific blood tests and/or radiographic findings often not available that reliably confirmed the diagnosis [1,2,3,4].
More and more things are known about the pathogenesis of the process, and parallel to this new and better treatment options are already available today. According to our knowledge, proinflammatory cyto- and chemokines (C3, C4, IL-23, TNFα, IFNα, IL2,6,8,12,15,17,22,23), adhesion and growth factors (TGFβ, EGF, HSP27 and 60, Cx26 and 30), different T cells (CD4+, DCs, CD8+), and their receptors act in that inflammatory and proliferative processes which finally appear as psoriatic skin signs and symptoms [2, 5]. Despite all this, psoriasis is a chronic relapsing disease, which often necessitates a long-term therapy. The choice of treatment for it is determined by disease severity, comorbidities, and access to health care [3]. Mild to moderate psoriasis can be treated locally (topical therapy with corticosteroids, vitamin D analogues, retinoids, and phototherapies). In some moderate cases and in every severe case, systemic treatment (drug administration in monotherapy or in combination) should be required [6].
The task is not easy, because to the intervention of the pathogenesis today only few molecular attack points are known, meaning that key pathogenic mechanisms are still not understood, and the known mechanisms may not always apply to every individual. At least 15–20% of patients do not respond to the newest, targeted anti-psoriatic agents; thus, in such cases or during exacerbation we must return to the conventional and also conservative steroid drug therapy. Biologic therapies in psoriasis are highly effective and can be classified according to their mechanism of action. The two main classes of biological agents are targeted at T cells or at cytokines. Moreover, the second-generation retinoids have been well useful drugs, and they have relatively few, local side effects [1, 2, 6]. Currently used drugs for psoriasis treatment are summarized in Table 1.
Differential scanning calorimetry (DSC) is a thermoanalytical method which was firstly described in the 1960s by Watson and O’Neill in the USA, and it was used initially during the examination of physical properties of inorganic materials [7]. Afterward, the technique was validated and was efficiently usable for the demonstration of structural changes not only in the physical sciences, but also in numerous biological macromolecules [8, 9], in different experimental animal studies [10,11,12,13], and in many clinical researches [14, 15].
Knowing these antecedents, our research group was looking for an answer to the question that how the different medications and the variable symptoms affect the human blood plasma composition on patients with psoriasis.
Materials and methods
Patient selection
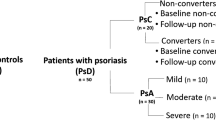
Thirty patients with psoriasis (15 women and 15 men, aged 21 to 75 years) with a mean age of 51.25 ± 5.2 were included in the study. Ten age- and sex-matched healthy volunteers with a mean age of 48.6 ± 3.2 were selected as the controls. Some of the patients who received drug medication did not have any symptoms, while others had moderate or severe symptoms. To define the severity of symptoms, three groups were established based on PASI (Psoriasis Area Severity Index) scoring system as previously described [16]. As brief, PASI 0 meant symptomless, while PASI 1–15 showed moderate symptoms, and serious symptoms were observed if PASI was over 15. According to the administration of anti-psoriatic monotherapy, the patients were divided into three groups: cytostatic-therapy-receiving (n = 10), retinoid-treatment-receiving (n = 10), and biological-agents-receiving persons (n = 10). The type, the dosage, and the timing of drug treatment were identified in accordance with the current dermatological protocols. The study protocol was approved by the regional ethical committee of Pécs University (4077/2011).
Blood sample collection and preparation
Peripheral blood samples were collected from patients (n = 30) and from healthy individuals (n = 10). Blood samples were collected into the Vacutainer tubes containing EDTA (1.5 mg mL−1 of blood) centrifuged at 1.600 g for 15 min at 4 °C to separate plasma fraction from cell components. Native plasmas were stored at − 80 °C until DSC measurement.
Calorimetric measurement
The thermal unfolding of the human plasma components was monitored by SETARAM Micro DSC-II calorimeter as previously described [17]. As brief, all experiments were conducted between 0 and 100 °C. The heating rate was 0.3 K min−1 in all cases. Conventional Hastelloy batch vessels were used during the denaturation experiments with 850 μL sample volume in average. The reference sample was normal saline (0.9% NaCl). The sample and reference samples were equilibrated with a precision of ± 0.1 mg. The repeated scan of the denatured sample was used as a baseline reference, which was subtracted from the original DSC curve. We have plotted the heat flow (DSC-II is a heat flux instrument with hermetically closed vessels) in the function of temperature. Calorimetric enthalpy was calculated from the area under the heat flow curve by using two-point setting SETARAM peak integration.
Deconvolution of DSC thermal curve
The plasma is a complex protein mixture. Therefore, it contains from a thermal point of view different “thermal domains” which can be assigned to the different compounds [18,19,20]. It means that a DSC scan can be decomposed into a sum of Gaussian curves; that way, their total area is nearly the same as of the experimental curve one, within a reasonable error (< 1%). To have the best fitting, we applied more than five curves, but some contribution was less than the error of enthalpy determination, so they cannot influence our final interpretation of data.
Statistical Analysis
All results are given in mean values ± standard error of the mean (SEM). Data were analyzed with one-way ANOVA. The level of significance was set at p < 0.05.
Results
This study investigated the thermal changes and deconvoluted DSC profile of human blood plasma following different systemic drug treatments on patients suffering from severe psoriasis. In Figs. 1–3 are shown the convoluted curves of the average DSC scans of persons with psoriasis after steroid, retinoid, and biological treatment in symptomless, in moderate, and in severe stages. To find them, we have chosen the critical plasma protein melting points to perform the deconvolution of the curves on the basis of papers published by Garbett et al. [18, 21], Michnik et al. [22], Todinova et al. [19, 23], Monaselidze et al. [24], Kikalishvili et al. [25] as well as Tenchov et al. [26, 27]. According to these studies, today the next melting points are well accepted for the identification of plasma protein compounds: at ~ 50 °C fibrinogen, ~ 62 °C albumin, ~ 70 °C Ig and the transition of the tail of albumin, ~ 76 °C C3 protein, IgA, IgG, and albumin, and ~ 82 °C IgG and transferrin. Characteristic thermal parameters (Tm and ΔHcal) have been collected on the one hand from healthy volunteers and on the other hand from patients who were differently treated for their various symptoms (Table 2).
Our aim with the deconvolution of average experimental curves was to get very good fitting (R was better than 0.99) between the deconvoluted and the experimental curves, using the above-accepted melting points. The control samples exhibited only four separable plasma compounds (see Figs. 1–3, and Table 2): fibrinogen at 56 °C which is higher than the widely accepted 50 °C. This deviation could be explained by our different DSC equipment (heat flow SETARAM Micro DSC-II with a sample holder of 1 mL), and we used—because of the big volume—the original plasma concentration without any dilution. (In most papers, the samples are 20-fold diluted, to avoid the unpleasant consequential of irreversible denaturation of proteins during the cleaning of the sample holders.) The very characteristic albumin contribution appeared at 62.5 °C (in the literature for healthy plasma is 62 °C), while the denaturation of C3, IgA and IgG as well as albumin parts was at 74.8 °C (in the literature 76 °C). The transition at 65.3 °C was identified as the contribution of Ig and the tail of albumin (in the literature 70 °C).
The thermal data of DSC scans measured in the case of psoriatic patients treated with different interventions showed practically partly identical results in Tms and ΔHcal for the symptomless cases. (We have throughout those decomposition values where the enthalpy contribution was in the range of ~ 3% of total enthalpy.) In terms of detail, the following observations can be made in the symptomless samples: (1) Tm1 decreased slightly during steroid therapy (56.0 °C vs. 54.5 °C), while the decrease was the same following the retinoid and biological drug treatment and less than next to steroids therapy (56.0 °C vs. 55.5 °C). (2) At Tm2, Tm3, and Tm4, the melting temperatures generally increased in every symptomless patient, and after steroid drug administration this elevation was notable. (3) Only retinoid administration caused a well-measurable fifth thermal transition (Tm5 at 85.5 °C) in plasma samples.
Comparing the melting temperatures on deconvoluted curves of patients with moderate or severe symptoms, different drug treatments show changes as follows: (1) A significant decrease in plasma in moderate-symptom patients treated with steroids compared to symptomless cases (51.0 °C vs. 54.5 °C). (2) But in terms of temperature, retinoid and biological drugs did not cause any difference in Tm1.
The second transitions (Tm2) have been identified between 61 and 64.8 °C to the albumin contribution being the dominant constituent of plasma. Most values were higher than in control and compared with the symptomless state in all treatment, and its value decreased in moderate and severe stadium. As it can be assumed from the results that the denaturation in 68–72 °C range is coming from Ig and the transition of the albumin tail, the control and the moderate stages in biological and steroid treatments exhibited smaller Tms, but based on calorimetric enthalpy we put them into this contribution. The enthalpy of Tm2 transitions increases significantly in almost all treated cases, while Tm3 transition enthalpies decreased in the function of the severity of disease in each case of biological, retinoid, or steroid treatments (Table 3).
In the case of healthy plasma, the denaturation around 76 °C is assigned to C3 protein, IgA and IgG fragments, and albumin. In the treated cases, the same compounds in the 72–80 °C temperature range (the biologic moderate state was put here because of its high enthalpy contribution) could be identified. Following retinoid and biological therapy, the calorimetric enthalpy slightly fluctuates, but in steroid-treated moderate stage an extra enthalpy jump has been observed. The widely accepted fifth denaturation temperature is around ~ 82 °C, which involves the contributions of IgG and transferrin. According to our data, we can set them into the 70.6–90 °C range. These changes could not be found in cases of healthy controls, neither after steroid nor after biological treatment in symptomless patients, as well as following retinoid therapy in a moderate stage. Surprisingly, the enthalpy of this transition was high in biologically treated moderate state, while in other cases it varied between 0.04 and 0.06 J g−1 ranges.
Discussion
These results can be considered as novel because no other results describing such blood plasma changes with a deconvoluted thermoanalytical method on patients with psoriasis have ever been reported. But the present observations are in accordance with our previous results also, in which we have demonstrated similar results on patients with chronic pancreatitis, as in other systematic inflammatory diseases [17]. An indisputable fact that these results are in line with other previous findings is observed during inflammatory processes [23, 28,29,30].
Several research groups have investigated blood plasma changes in patients who were treated for cancer, inflammatory disease, or other causes. But this is the first research that shows the changes in plasma protein components through the “glasses” of DSC. No doubt, the importance and role of DSC analysis is incontestable for understanding the stability of biological systems in the human body in the future.
References
Ferencz A, Moezzi M, Lőrinczy D. Differential Scanning Calorimetry (DSC) as a new diagnostic and screening method on patients with psoriasis. In: Lambert W, editor. Psoriasis: epidemiology, diagnosis and management strategies. New York: Nova Science Publishers Press; 2016. p. 45–64.
Raychaudhuri SP. A cutting-edge overview: psoriatic disease. Clinic Rev Allerg Immunol. 2013;44:109–13.
Rendon A, Schäkel K. Psoriasis pathogenesis and treatment. Int J Mol Sci. 2019;20:1475–503.
Bhosle MJ, Kulkarni A, Feldman SR, Balkrishnan R. Quality of life in patients with psoriasis. Health Qual Life Outcomes. 2006;4:35–41.
Di Meglio P, Perera GK, Nestle FO. The multitasking organ: recent insights into skin immune function. Immunity. 2011;35:857–69.
Nestle FO, Kaplan DH, Barker J. Psoriasis. N Engl J Med. 2009;361:496–509.
Watson ES, O’Neill MJ, Justin J, Brenner N. A differential scanning calorimeter for quantitative differential thermal analysis. Anal Chem. 1964;36:1233–8.
Lőrinczy D, Belágyi J. Effects of nucleotide on skeletal muscle myosin unfolding in myofibrils by DSC. Biochem Biophys Res Commun. 1995;217:592–8.
Dergez T, Lőrinczy D, Könczöl F, Farkas N, Belágyi J. Differential scanning calorimetry study of glycerinated rabbit psoas muscle fibres in intermediate state of ATP hydrolysis. BMC Struct Biol. 2007;7:41–50.
Nedvig K, Ferencz A, Rőth E, Lőrinczy D. DSC examination of intestinal tissue following warm ischemia and reperfusion injury. J Therm Anal Calorim. 2009;95:775–9.
Ferencz A, Nedvig K, Lőrinczy D. DSC examination of intestinal tissue following cold preservation. Thermochim Acta. 2010;497:41–5.
Szántó Z, Kovács G, Nagy V, Rőth E, Molnár FT, Horváth ŐP. Differential scanning calorimetric examination of the tracheal cartilage after primary reconstruction with differential suturing techniques. Thermochim Acta. 2006;445:190–4.
Ferencz A, Nedvig K, László E, Magyarlaki T, Lőrinczy D. DSC examination of kidney tissue following warm ischemia and reperfusion injury. Thermochim Acta. 2011;525:161–6.
Farkas P, Könczöl F, Lőrinczy D. New possibilities of application of DSC as a new clinical diagnostic method. J Therm Anal Calorim. 2018;133:579–89.
Szalai ZS, Molnár FT, Lőrinczy D. Role of differential scanning calorimetry (DSC) in the staging of COPD. A new approach to an old definition problem. J Therm Anal Calorim. 2017;127:1231–8.
Moezzi M, Ferencz A, Lőrinczy D. Evaluation of blood plasma changes by differential scanning calorimetry in psoriatic patients treated with drugs. J Therm Anal Calorim. 2014;116:557–62.
Ferencz A, Lőrinczy D. DSC measurements of blood plasma on patients with chronic pancreatitis and operable and inoperable pancreatic adenocarcinoma. J Therm Anal Calorim. 2017;127:1187–92.
Garbett NC, Mekmaysy C, Helm CV, Jenson AB, Chaires JB. Differential scanning calorimetry of blood plasma for clinical diagnosis and monitoring. Exp Mol Pathol. 2009;86:186–91.
Todinova S, Krumova S, Kurtev P, Dimitrov V, Djongov L, Dudunkov Z, Taneva SG. Calorimetry-based profiling of blood plasma from colorectal cancer patients. Biochim Biophys Acta. 2012;1820:1879–85.
Michnik A, Drzazga Z. Thermal denaturation of mixtures of human serum proteins. DSC study. J Therm Anal Calorim. 2010;101:513–8.
Garbett NC, Miller JJ, Jenson AB, Chaires JB. Calorimetry outside the box: a new window into the plasma proteome. Biophys J. 2008;94:1377–83.
Michnik A, Drzazga Z, Michalik K, Barczyk A, Santura I, Sozanska E, Pierzchała W. Differential scanning calorimetry study of blood serum in chronic obstructive pulmonary disease. J Therm Anal Calorim. 2010;102:57–60.
Todinova S, Krumova S, Gartcheva L, Robeerts C, Taneva SG. Microcalorimetry of blood serum proteome: a modified interaction network in the multiple myeloma case. Anal Chem. 2011;83:7992–8.
Monaselidze J, Tevdoradze T, Zibzibadze M, Alibegashvili M, Ramishvili L, Gordeziani M, Kotrikadze N. The study of blood serum proteins in patients with mammary gland tumours. J Biol Phys Chem. 2012;1:19–22.
Kikalishvili L, Ramishvili M, Nemsadze G, Lezhava T, Khorava P, Gorgoshidze M, Kiladze M, Monaselidze J. Thermal stability of blood plasma proteins of breast cancer patients, DSC study. J Therm Anal Calorim. 2015;120:501–5.
Tenchov B, Abarova S, Koynova R, Traikov L, Tancheva L. Low-temperature exothermic transitions in brain proteome of mice, effect of scopolamine. Thermochim Acta. 2017;650:26–32.
Tenchov B, Abarova S, Koynova R, Traikov L, Dragomanova S, Tancheva LA. New approach for investigating neurodegenerative disorders in mice based on DSC. J Therm Anal Calorim. 2017;127:483–6.
Garbett NC, Merchant ML, Helm CW, Jenson AB, Klein JB, Chaires JB. Detection of cervical cancer biomarker patterns in blood plasma and urine by differential scanning calorimetry and mass spectrometry. PLoS ONE. 2014;9:e84710.
Johnson CM. Differential scanning calorimetry as a tool for protein folding and stability. Arch Biochem Biophys. 2013;531:100–9.
Fish DJ, Brewood GP, Kim JS, Garbett NC, Chaires JB, Benight AS. Statistical analysis of plasma thermograms measured by differential scanning calorimetry. Biophys Chem. 2010;152:184–90.
Acknowledgements
Open access funding provided by Semmelweis University (SE). This research was funded by Grant OTKA (C272 for D.L. and PD77474 for A.F.) and PTE ÁOK Research Grant (114-603/2009 for A.F.).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lőrinczy, D., Moezzi, M. & Ferencz, A. Deconvoluted plasma DSC curves on patients with psoriasis. J Therm Anal Calorim 142, 789–796 (2020). https://doi.org/10.1007/s10973-020-09443-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10973-020-09443-y