Abstract
To improve interventions for people with cancer who experience clinically relevant distress, it is important to understand how distress evolves over time and why. This review synthesizes the literature on trajectories of distress in adult patients with cancer. Databases were searched for longitudinal studies using a validated clinical tool to group patients into distress trajectories. Twelve studies were identified reporting trajectories of depression, anxiety, adjustment disorder or post-traumatic stress disorder. Heterogeneity between studies was high, including the timing of baseline assessments and follow-up intervals. Up to 1 in 5 people experienced persistent depression or anxiety. Eight studies examined predictors of trajectories; the most consistent predictor was physical symptoms or functioning. Due to study methodology and heterogeneity, limited conclusions could be drawn about why distress is maintained or emerges for some patients. Future research should use valid clinical measures and assess theoretically driven predictors amendable to interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unsurprisingly, a diagnosis of cancer is often associated with psychological distress, such as symptoms of depression, anxiety, traumatic stress, fear of cancer progression or recurrence (FCR), or death anxiety. While longitudinal studies suggest that rates of distress generally improve over time, a substantial proportion of patients continue to experience clinically relevant distress (Calman et al., 2021; Henry et al., 2019; Krebber et al., 2014; Savard & Ivers, 2013). For mental health clinicians, understanding patients’ likely distress trajectory, specifically the timepoints at which distress is likely to emerge and whether the distress is likely to remain clinically relevant, is critical for the design and implementation of mental health and systemic interventions.
There are several gaps in the existing literature about how and why distress evolves amongst cancer patients. Firstly, longitudinal research has mainly reported prevalence data (Niedzwiedz et al., 2019), which conflates distress trajectories across different cancer cohorts and is not informative about how distress trajectories evolve for individual patients. For instance, there is evidence that distress increases longitudinally amongst younger patients and those with cancers that are more likely to recur, such as ovarian or oesophageal cancers (Liu et al., 2022; Starreveld et al., 2018; Watts et al., 2015). Additionally, there is scant longitudinal research regarding how distress evolves for individuals with advanced disease receiving novel therapies, who are likely at greater risk for psychological distress (Thewes et al., 2017). For example, amongst patients with advanced melanoma who achieved remission on immunotherapy, 64% had clinical levels of anxiety or depression at one point during the following year despite having no active disease (Rogiers et al., 2020). However, the distress trajectories and factors associated with recovered or persistent distress could not be ascertained by the data.
Secondly, longitudinal studies that group patients into distress trajectories vary in method. Some have used clinical cut-off scores and assessed individuals longitudinally at two time points (e.g. Linden et al., 2015), resulting in four clinically meaningful trajectories of distress: (1) non-cases (not meeting clinical criteria at either time point), (2) recovered (clinically significant distress at the first timepoint only), (3) persistent (meeting clinical criteria at both time points), and 4) emerging (clinically significant distress at the second timepoint only). In longitudinal studies conducted over more than two timepoints a fluctuating trajectory of distress may also be evident where a person meets clinical criteria at some, but not all, assessments (e.g., Mols et al., 2018). However, the majority of longitudinal studies of distress trajectories have used statistical methods, such as latent class growth analysis, to group participants into trajectories rather than utilising pre-determined clinical cut-off scores. Consequently, the number of trajectories identified, and the participants assigned to each trajectory, will differ according to the method used (e.g., Custers et al., 2020). Also, statistical analyses identify patterns in samples, so if the average outcome score is low, a statistically derived “persistently high” trajectory may include patients below a clinically meaningful threshold (e.g., Stanton et al., 2015). Since distress trajectories identified by statistical methods are difficult to interpret clinically, they have limited utility in informing clinical questions of how and why distress trajectories differ for individual patients.
Thirdly, it is unclear why some people are more likely to experience persistent or emerging distress over time. Theorists have suggested that intrapersonal and interpersonal constructs, such as metacognitions, cognitive appraisals, coping styles, physical symptom severity, social support, and the relationship with health care providers, may be important in understanding the evolution of distress and adjustment (Curran et al., 2017; Edmondson, 2014; Fardell et al., 2016; Kangas & Gross, 2020). However, the role of these constructs across the illness trajectory and within subgroups of patients is not clearly understood. For instance, a recent systematic review concluded that the only consistent psychological predictors of clinically relevant distress longitudinally are initial distress and neuroticism (Cook et al., 2018). However, this finding does not elucidate why some people had high distress scores at study entry or personality traits associated with experiencing more negative emotions. The reviewers called for better designed, theoretically informed longitudinal research to determine the psychological factors underpinning the aetiology and maintenance of cancer-related distress, which could then inform improvements in interventions. Separately, Kangas and Gross (2020) have called for further research to understand the trajectories of distress in a way that recognises cancer as a dynamic experience.
To address the above gaps, this study aims to summarize the literature regarding (1) the course of clinically relevant, individual trajectories of distress after a cancer diagnosis and (2) the psychological, sociodemographic and medical factors associated with different distress trajectories; and comment on how these findings relate to existing theories of cancer-related distress.
Method
A systematic literature search was conducted following the PRISMA 2020 statement (Page et al., 2021). PsycINFO and Medline ALL were searched in December 2021 and updated in January 2023. Search terms related to clinical distress (depression, anxiety, trauma or stress related disorders), cancer AND longitudinal studies, were mapped to Medical Subject Headings (MeSH) and exploded where possible (see Supplementary Material for the full list of search items). The search was limited to peer-reviewed journals and articles in English, due to the unavailability of resources or funds to translate non-English articles. Reference lists of relevant articles were examined to identify further publications. Ethical approval was not required for this review of previously published data.
The first author (LC) inspected article titles and abstracts for the inclusion criteria: (1) written in English; (2) peer-reviewed; (3) adult patients with cancer; (4) mental health outcomes were assessed longitudinally with a validated clinically relevant measure and (5) results could be clustered according to clinical cut-off scores to identify distress trajectories. Articles were excluded if the sample (1) related to adult survivors of childhood cancer, (2) lacked statistical power to accurately determine the proportion of participants in each trajectory (power calculation in Supplementary Material), (3) only grouped patients into trajectories using statistical methods or (4) participants were enrolled in an intervention trial. A second reviewer (AM) independently examined 10% of article titles and abstracts, with disagreement resolved by consensus. The full text of retained articles were examined independently by both reviewers for further inclusion/exclusion with agreement reached by consensus.
The following data was obtained from the included studies by LC and fact-checked by AM: sample characteristics (sample size, age, gender, cancer type and stage, place of recruitment), time of study entry (T1), time since diagnosis, follow-up timepoints and the interval from T1, the proportion of patients in active treatment at follow-up, outcome measure used, trajectories identified, proportion of sample in each trajectory, and predictors of between group differences (if examined). When trajectories were not reported in the article, but data was available to calculate them, the proportion of patients in each trajectory was calculated from the completer sample. Results were tabulated according to the clinical outcome measured, and the number of assessments conducted longitudinally. Due to the heterogeneity of studies, a meta-analysis was not possible, and a narrative review was conducted.
The methodological quality of included studies was evaluated independently by LC and AM using four domains from the Quality in Prognosis Studies (QUIPS) tool (Hayden et al., 2013): study participation, attrition, outcome measurement and study confounding. A fifth domain, statistical analyses, was rated only if analyses of between group factors were conducted (some studies only reported descriptive statistics to calculate the proportion of the sample in each distress trajectory).
Results
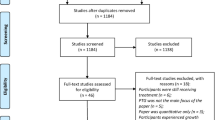
Figure 1 outlines the process of article selection and reasons for exclusion. After removing duplicates, 5509 articles were identified. Inter-rater reliability (Cohen’s Kappa) of 10% of the articles was 0.73. Title and abstract review yielded 82 articles for full-text review and two articles were identified via the ancestry method. Independent review of the articles resulted in full consensus to retain 14 articles, describing 12 samples. Studies were excluded where the proportion of patients in each distress trajectory could not be calculated from the published data (e.g., Lopes et al., 2022; Sutton et al., 2022).
Table 1 provides the characteristics of the 12 study samples included in this review (N = 8566). Results are discussed according to the outcome measured. Also, the results are discussed according to the number of timepoints measured, as this impacts on the potential number of trajectories identified, and the proportion of patients assigned to each trajectory.
Depression Studies with Two Assessment Timepoints
Six studies assessed depression over two timepoints to identify four trajectories: non-cases, recovered, emerging and persistent (Alfonsson et al., 2016; Boyes et al., 2013; Hasegawa et al., 2019; Kim et al., 2012; Linden et al., 2015; Sullivan et al., 2016). Studies involved breast (Alfonsson et al., 2016; Kim et al., 2012), lung (Sullivan et al., 2016), or mixed cancer diagnoses (Boyes et al., 2013; Linden et al., 2015) or malignant Lymphoma or Multiple Myeloma (Hasegawa et al., 2019). In the non-breast cancer studies, male and female patients were equally represented. One study excluded patients with “secondary” disease (Kim et al., 2012) and three studies excluded terminally ill patients or those deemed unsuitable or too unwell by their physician to participate (Boyes et al., 2013; Hasegawa et al., 2019; Sullivan et al., 2016). Only three studies reported patients’ mean age, and participants were typically in their 50 s and 60 s (Alfonsson et al., 2016; Kim et al., 2012; Linden et al., 2015). Further analysis of one study sample (Kim et al., 2012) produced two additional publications (Kim et al., 2013, 2018).
Caseness was usually determined by cut-off scores on self-report measures such as the depression subscale of the Hospital Anxiety and Depression Scale (HADS-D; Zigmond & Snaith, 1983), the depression subscale of the Psychosocial Screen for Cancer (PSSCAN; Linden et al., 2005), the Patient Health Questionnaire (Kroenke et al., 2001), and the Centre for Epidemiological Studies Depression Scale– short-form (Turvey et al., 1999). A structured diagnostic interview was only used in one sample and participants were classified as cases if they met criteria for minor or major depression (Kim et al., 2012). Assessment points varied considerably. Two studies assessed depression prior to treatment but the samples were followed up one month or 12 months later (Hasegawa et al.; Linden et al., 2015). One study assessed depression post-surgery and 12 months later (Kim et al., 2012). Three studies assessed depression 4–6 months post-diagnosis (on average) and followed up six (Boyes et al., 2013), seven (Sullivan et al., 2016), or 38 months later (Alfonsson et al., 2016). Most studies did not report whether patients were in active treatment throughout the course of the assessment period or had completed treatment.
In terms of depression trajectories, about half of patients with lung cancer were classified as non-cases (Sullivan et al., 2016), compared to two thirds of participants in other newly diagnosed cancer groups (Hasegawa et al., 2019; Kim et al., 2012; Linden et al., 2015). The highest rates of non-cases were reported in two studies that recruited patients 4–6 months post-diagnosis (80–82%; Alfonsson et al., 2016; Boyes et al., 2013). The proportion of recovered cases varied from 6 to 16% and was lowest in the sample that had low rates of depression at baseline (Alfonsson et al., 2016). The sample of patients with lung cancer had the highest rate of persistent depression (22%) measured over a seven-month period (Sullivan et al., 2016). The remaining studies reporting rates of persistent depression at 4–10%, measured over intervals ranging from 1–36 months. Emerging depression was most common in a mixed sample of newly diagnosed patients assessed before treatment and 12 months later (19%; Linden et al., 2015). The remaining studies reported emerging depression rates of 6–10%.
Group comparisons were conducted on three study samples to identify predictors associated with depression trajectories (Table 2). Amongst patients with newly diagnosed haematological malignancies, non-cases were more likely to be physically active compared to those with persistent depression (Hasegawa et al., 2019). No other demographic or medical variables were differentially associated with trajectories. Similarly, amongst newly diagnosed patients with breast cancer, recovery from depression was associated with greater improvements in general health, emotional, social and role functioning, fatigue, and insomnia over the 12-month follow-up period, compared to persistent cases (Kim et al., 2013). Conversely, persistent or emerging depression was associated with larger decrements in general health, and emotional and role functioning, and worsening physical symptoms compared to non-cases. Persistent depression was also associated with financial difficulties, personal or family history of depression, more metastatic axillary lymph nodes, larger tumour size, and specific genotypes compared to non-cases (Kim et al., 2012, 2013). However, age, education, time since diagnosis or tumour stage were not associated with depression trajectories.
In contrast, younger age was associated with persistent depression in a study of people with various cancer diagnoses (Linden et al., 2015). Higher illness intrusiveness (i.e., the perceived impact of illness on functioning) was associated with persistent depression, although illness intrusiveness did not differentiate between persistent, recovered, or emerging groups. Persistent depression was also associated with higher baseline anxiety and depression scores. However, post-hoc analysis showed that baseline anxiety and depression scores were equally high for persistent and recovered cases and equally low for non-cases and emerging cases, suggesting that baseline anxiety and depression scores had limited utility in predicting depression trajectories.
Depression Studies with More Than Two Assessment Timepoints
Two studies assessed depression trajectories over three or more time points using a HADS-D score of > 8 to define caseness. Newly diagnosed patients with head and neck cancer, treated with curative intent, were assessed for depression before commencing treatment and 4 and 12 months later (Jansen et al., 2018). The number of patients still in active treatment was not reported. Five trajectories were identified: non-cases (63%), recovered (16%), persistent (7%), late emerging (12%), and recurrent (1%). Compared to non-cases and those who recovered, persistent, emerging or recurrent depression was associated with being single, widowed or divorced, lower education, lower income, later tumour stage at diagnosis, having chemotherapy, more co-morbidities, smoking and being a non-drinker or a hazardous drinker of alcohol. Age was associated with depression trajectories but was assessed as a categorical variable, making the results difficult to interpret.
Patients from a colorectal cancer registry who were one to ten years post-diagnosis were assessed yearly for depression over four years (Mols et al., 2018). Three depression trajectories were identified: non-cases (71%), persistent (8%) and fluctuating (21%). Those with persistent or fluctuating depression were more likely to have two or more comorbidities compared to non-cases. Fluctuating depression was also associated with older age, lower education, and stage IV disease (compared to stage III as assessed at study entry). Changes in disease status or treatment course were not assessed over time.
Anxiety Studies with Two Assessment Timepoints
Four studies assessed clinically relevant anxiety over two timepoints. Caseness was defined by a cut-score of ≥ 8 on the anxiety subscale of the HADS (HADS-A) or PSSCAN (Alfonsson et al., 2016; Boyes et al., 2013; Kim et al., 2020; Linden et al., 2015). Two studies involved women with breast cancer: women with stage 0-III cancer were assessed pre-surgery and 12 months later (Kim et al., 2020), and women with all cancer stages were assessed within 9 months of diagnosis and 3 years later (Alfonsson et al., 2016). The other two anxiety studies involved people with mixed cancer diagnoses assessed 6 months post-diagnosis and 6 months later (Boyes et al., 2013), and assessed before treatment commenced and 12 months later (Linden et al., 2015). Boyes et al. (2013) reported that 8% of their sample were receiving chemotherapy or radiotherapy at follow-up, but the proportion of patients in active treatment was not reported in the other studies.
Despite differences in samples and assessment timepoints across studies, some patterns emerged. Studies that recruited patients before commencing treatment had lower proportions of “non-cases” (48%-55%) and higher proportions of recovered cases (17–23%; Kim et al., 2020; Linden et al., 2015) compared to the studies that recruited on average 4–6 months after diagnosis (61–70% non-cases and 8–13% recovered cases; Alfonsson et al., 2016; Boyes et al., 2013). The rate of emerging anxiety was about 10% and was lowest in the study that recruited patients 6 months after diagnosis (7%; Boyes et al., 2013). The rate of persistent anxiety ranged from 14 to 21%, and was highest in a sample of newly diagnosed women with breast cancer (Boyes et al., 2013; Kim et al., 2020).
Two of these studies examined predictors of anxiety trajectories (Table 2). Persistent anxiety was associated with younger age and higher baseline anxiety or depression severity compared to non-cases; and recovered anxiety was associated with lower baseline anxiety compared to persistent cases (Linden et al., 2015). Persistent and emerging anxiety was also associated with more pain, breast and arm symptoms at follow-up compared to non-cases (Kim et al., 2020).
Anxiety Studies with More Than Two Assessment Timepoints
One study assessed patients with colorectal cancer for clinically relevant anxiety at diagnosis and yearly for three years (Mols et al., 2018). Using the HADS-A, patients were grouped into three trajectories: non-cases (68%), persistent (10%) and fluctuating (22%). As with depression, those with fluctuating or persistent anxiety were more likely to have two or more comorbidities compared to non-cases (Table 2). Fluctuating anxiety was also associated with being female, younger age, lower education, and stage IV disease (compared to stage I).
Mixed Anxiety and Depression
One study assessed patients who scored above the clinical cut-off on both the depression and anxiety HADS subscales (Boyes et al., 2013). Not surprisingly, the proportion of patients in the clinical range was much smaller than for anxiety or depression alone (5% emerging, 4% persistent).
Adjustment Disorder (AD)
One study examined AD (defined as marked distress not meeting criteria for another mental disorder) amongst patients with breast cancer who had completed treatment within the previous 5 years (Wijnhoven et al., 2022). Patients were assessed four times over 12 months using the HADS total score (HADS-T). Scores of 11–14 were defined as AD, and scores ≥ 15 were defined as “other mental disorder.” Participants were classified into 4 trajectories: non-cases (54%), fluctuating (38%), persistent “other mental disorder” (7%), and persistent AD (1%). Persistent or fluctuating trajectories (combined and compared to non-cases) were associated with younger age, more difficulties with daily activities, less social support than desired, lower optimism, and higher neuroticism.
Post-Traumatic Stress Disorder (PTSD)
Two studies examined PTSD trajectories. Patients with Non-Hodgkin’s Lymphoma (NHL) were assessed for PTSD two years post-diagnosis and five years later (Smith et al., 2011). 10% of the sample were receiving active treatment at study entry but the proportion receiving active treatment at follow-up is not reported. Male and female participants were equally represented, and sample mean age was 62 years. Using the PTSD Checklist-Civilian Version (PCL-C; Weathers et al., 1993), those at least moderately bothered by one re-experiencing, three avoidance and two arousal symptoms were classified as PTSD cases. Most patients in this cohort were non-cases for PTSD (90%), with small proportions of recovered (3%), emerging (4%) and persistent (3%) cases reported. The authors examined predictors of PCL-C scores not PTSD trajectories.
In the second study, patients with stage I-III breast cancer were assessed for PTSD on three occasions: 2–3, 4 and 6 months after diagnosis (Vin-Raviv et al., 2013). Whether participants were actively receiving cancer treatment was not assessed. Caseness was determined by Impact of Events Scale score ≥ 24 (Horowitz et al., 1979). At 4 months post-diagnosis, four trajectories were identifiable from the published data: non-cases (72%), recovered (12%), persistent (11%), and emerging (5%). At 6 months post-diagnosis, eight trajectories were identifiable. Four trajectories described those who did not meet criteria for PTSD at 6 months: non-cases (71%), sustained recovery (9%), PTSD emerged then resolved (4%), and late recovery (4%). Four trajectories described patients who met criteria for PTSD at 6 months: persistent (7%), late onset (2%), resolved but re-emerged (2%), and emerged and sustained (1%). Non-cases were compared to those who met PTSD criteria at two or more consecutive assessments. No clinical variables distinguished these groups, but non-cases were more likely to be aged over 50 and be White or Hispanic rather than Black or Asian.
FCR and Death Anxiety
No studies meeting our inclusion criteria examined trajectories of FCR or death anxiety.
Risk of Bias Assessment
Risk of bias assessment results are presented in Table 3 (see Supplementary Material for more detail). Inter-rater agreement was 84%. No studies were rated as having a low risk of bias across all domains. Of clinical importance, four studies were rated high on risk of bias for study participation due to low recruitment rates (38–51%; Boyes et al., 2013; Kim et al., 2020; Sullivan et al., 2016; Wijnhoven et al., 2022), while six studies were rated high on risk of bias for attrition, due to low completer rates (53–64%; Alfonsson et al., 2016; Jansen et al., 2018; Kim et al., 2020; Wijnhoven et al., 2022), non-completers were more likely to be anxious or depressed,31 or key characteristics of non-completers were not described (Linden et al., 2015; Wijnhoven et al., 2022). In terms of outcome measurement, the window for baseline data collection post-diagnosis was wide in five studies (Alfonsson et al., 2016; Boyes et al., 2013; Mols et al., 2018; Smith et al., 2011; Wijnhoven et al., 2022). None of the studies examining why the trajectory groups differed (Hasegawa et al., 2019; Jansen et al., 2018; Kim et al., 2012, 2020; Linden et al., 2015; Mols et al., 2018; Vin-Raviv et al., 2013; Wijnhoven et al., 2022) were informed by a theoretical model.
Discussion
This is the first review to synthesise the current knowledge about longitudinal distress trajectories in patients with cancer. We identified 12 study samples assessing trajectories of depression (8), anxiety (5), PTSD (2) and AD (1). Unfortunately, due to heterogeneity between studies, we were unable to conduct a meta-analysis on the prevalence of trajectories or the predictors. Nevertheless, patterns did emerge in the findings which are discussed below.
Depression
Findings suggest that depression trajectories may be related to cancer cohorts, with higher levels of persistent depression evident in the study of patients with lung cancer (Sullivan et al., 2016). These findings contrast with a meta-analysis reporting that the average point-prevalence of depression amongst patients with lung cancer was similar to other cancer groups (Krebber et al., 2014). A key limitation of the cross-sectional prevalence studies included in the meta-analysis is that they do not inform who continued to have depression over time. For lung cancer, high rates of persistent depression have been associated with stigma (Cataldo & Brodsky, 2013), poor sleep quality (He et al., 2022), impacts on physical functioning (Hopwood & Stephens, 2000), and diagnosis commonly occurring at a later stage (Schabath & Cote, 2019). Within this context, early screening for depression may be a more robust indicator of persistent distress amongst lung cancer patients and flag the need for psychological intervention, compared to other cancer groups.
Findings also indicate that future studies should take greater account of survivor bias. Rates of non-cases of depression were highest amongst the two studies that recruited from large cancer registries (Alfonsson et al., 2016; Boyes et al., 2013) and were therefore more likely to include patients who had completed their initial treatment. Conversely, rates of recovery from depression were lower when initial assessments were conducted some months after diagnosis (Alfonsson et al., 2016; Boyes et al., 2013) compared to those studies that recruited close to diagnosis (Jansen et al., 2018; Kim et al., 2012). These data suggest that future research should commence longitudinal studies closer to diagnosis to allow comparisons across studies and identify patients who recover, and the protective factors associated with their recovery.
No conclusions could be drawn from the data about when depression is likely to emerge after a cancer diagnosis. Rates of emerging depression were highest amongst newly diagnosed patients with mixed cancer types assessed before treatment and 12 months later (19%; Linden et al., 2015). The 12-month assessment point was chosen to coincide with patients completing their initial treatment regime and adjusting to survivorship. However, some patients were in the palliative phase and about 5% of patients died during the follow-up period. Given the heterogeneity in the sample and the long interval between assessment timepoints, future studies should assess more frequently to determine when clinically relevant depression emerged, and for which patients, so that screening efforts can be directed accordingly.
Regarding predictors of depression trajectories, findings indicate that greater emphasis is needed on understanding physical symptom severity and psychological factors as predictors of depression. Physical symptom severity as measured by performance status (Hasegawa et al., 2019), the impact of physical symptoms on functioning (Kim et al., 2012, 2013), or the presence of comorbidities (Jansen et al., 2018; Mols et al., 2018), was consistently associated with persistent depression. Demographic variables were not significant predictors (Jansen et al., 2018; Kim et al., 2013; Linden et al., 2015; Mols et al., 2018), and age inconsistently predicted depression trajectories (Hasegawa et al., 2019; Jansen et al., 2018; Linden et al., 2015). Clinical variables, such as time since diagnosis, treatment type, or tumour stage were also not significant predictors of persistent depression in most studies. Importantly, one study assessed changes in physical symptoms over time (Kim et al., 2013). Surprisingly, no studies examined whether being in active treatment or completing treatment explained distress trajectories. As adaptation to cancer evolves within a changing context of symptoms and functioning, contextual physical and treatment variables should also be assessed longitudinally and considered in future predictive models.
The two studies exploring psychological predictors of depression reported that a baseline or previous history of depression was associated with a persistent depression trajectory (Kim et al., 2012; Linden et al., 2015), suggesting that previous history should be included in early psychological screening processes. This also suggests that exploring the vulnerability factors that predisposed these individuals to depression is important in identifying psychological predictors amenable to treatment. For instance, theories suggest that habitual coping strategies and the quality of social support may impede or facilitate adjustment to cancer (Kangas & Gross, 2020) Separately, illness intrusiveness, or the subjective meaning and salience of symptoms, was argued to be a psychological predictor associated with persistent depression (Linden et al., 2015). The illness intrusiveness rating scale used in this study assesses the extent to which illness disrupts functioning in various quality-of-life domains (Devins et al., 2001), and may be a proxy for symptom severity. Consequently, more refined measures of illness meaning and salience are needed. Interestingly, there is evidence that related psychological constructs, such as illness representations and the impact of illness on self-schemas, are associated with depression amongst people with cancer (Carpenter et al., 2009; Richardson et al., 2017). These constructs are important to investigate in future research to identify psychological predictors of depression trajectories that may be amenable to interventions.
Anxiety
As with depression, anxiety trajectories were related to assessment timepoints. Studies that recruited at least 6 months after diagnosis from cancer registries had the highest proportion of non-cases (Boyes et al., 2013; Mols et al., 2018) while studies that recruited before treatment commenced had the lowest rate of non-cases and higher rates of persistent and recovered anxiety (Kim et al., 2020; Linden et al., 2015). The early phase of adjustment to diagnosis and treatment is an especially anxious period for patients who are experiencing uncertainty about treatment efficacy and the possible impacts on their roles and relationships (Thewes et al., 2017). However, a substantial proportion of patients did adjust without any specific intervention.
Findings regarding the emerging anxiety trajectory highlight the importance of assessing patients at multiple timepoints to identify patients in need of clinical intervention. While emerging anxiety was the least common trajectory, around 1 in 10 people did develop anxiety over time, even amongst those recruited up to nine months after diagnosis (Alfonsson et al., 2016). The rate of emerging anxiety occurred similarly across studies, suggesting this phenomenon was related to aspects of the cancer experience that are common across cancer cohorts, such as ongoing uncertainty and fears about the cancer progressing or recurring (Curran et al., 2017).
In terms of predictors of anxiety trajectories, demographic variables, such as education, income and age, were not consistent predictors (Kim et al., 2020; Linden et al., 2015; Mols et al., 2018). As with depression, cancer symptoms, comorbidities and/or general health functioning were associated with persistent anxiety (Kim et al., 2020; Mols et al., 2018). Higher illness intrusiveness and physical symptoms were also associated with emerging anxiety (Kim et al., 2020; Linden et al., 2015). This accords with the Enduring Somatic Threat Model, based on Terror Management Theory, that posits that physical symptoms remind a person of their mortality and inflate anxiety (Edmondson, 2014). Consequently, it is important that future studies assess contextual physical factors longitudinally to understand the course of anxiety and ensure effective physical symptom management to improve mental health outcomes.
Only one study examined predictors of recovered anxiety, and reported that, compared to persistent anxiety, baseline anxiety was lower (Linden et al., 2015). However, this does not inform us about why these patients had lower anxiety at baseline. Given the paucity of research on the predictors of anxiety trajectories, theoretically informed research is needed to understand the vulnerability and protective factors that underpin anxiety trajectories.
PTSD
The two studies assessing PTSD trajectories also highlight a need for future studies to carefully consider assessment time-points (Smith et al., 2011; Vin-Raviv et al., 2013). Not surprisingly rates of persistent PTSD were lowest in the sample that included people on average 7 years post diagnosis (Smith et al., 2011). Neither of these studies examined predictors of trajectories specifically, although higher PTSD scores were associated with greater impacts of the cancer on appearance, life interference and worrying (Smith et al., 2011), and younger patients were more likely to meet criteria for PTSD on two consecutive longitudinal assessments (Vin-Raviv et al., 2013). Other possible predictors of persistent PTSD that are amenable to interventions warrant further investigation, such as a history of trauma or major life stressors prior to the cancer diagnosis (Silver-Aylaian & Cohen, 2001; Swartzman et al., 2017), avoidant coping (Jacobsen et al., 2002), greater illness uncertainty (Kuba et al., 2017), higher disease burden (Kuba et al., 2017; Shand et al., 2015), and lower social support (Jacobsen et al., 2002; Shand et al., 2015).
Since these studies, diagnostic criteria have changed so that PTSD is diagnosed only when there has been a sudden, catastrophic event in addition to the cancer diagnosis (such as a life-threatening haemorrhage), and the person experiences intrusive, hyperarousal and avoidance symptoms related to memories of that event (APA, 2013). Consequently, in the cancer context, where intrusions are generally related to future-orientated fears, PTSD should be rarely diagnosed; instead, patients with cancer who experience traumatic stress symptoms would likely meet criteria for AD (Kangas, 2013). Indeed, some researchers have argued that the classification of AD as a distinct stress disorder more appropriately describes the distress experienced in cancer settings and therefore may lead to improvements in research and interventions (Esser et al., 2019).
AD
Only one study examined trajectories of AD (Wijnhoven et al., 2022), so no meaningful conclusions can be drawn from our review of the literature to date. The study was limited to patients with breast cancer who had completed treatment given with curative intent. Only 1.4% met the study criteria for persistent AD, that is, marked but not high levels of distress on the HADS-T. The low case-rate for persistent AD may relate to assessment validity or that the study included patients that would be expected to be past the initial post-diagnosis adjustment phase. More studies are needed to understand the trajectory of AD from diagnosis.
FCR or Death Anxiety
No studies examining trajectories of FCR met our inclusion criteria, principally because many studies of FCR have used statistical methods to group participants into trajectories rather than clinical cut-off scores. Investigating FCR is important because FCR is a pattern of worry, preoccupation and hypervigilance to body symptoms centred on fears about the cancer progressing or recurring, that can be distinguished from other anxiety disorders (Mutsaers et al., 2020). FCR is also likely to have a unique course and predictors with evidence that FCR persists over time, and may even increase in severity, especially for younger patients (Starreveld et al., 2018). Also, no studies of trajectories of death anxiety were reported. Death anxiety is important to consider as it is associated with, but distinct from other manifestations of anxiety, such as general anxiety, health anxiety or FCR (Curran et al., 2020; Menzies et al., 2021), and occurs across cancer cohorts, affecting people with metastatic or late-stage cancer (Lo et al., 2011; Neel et al., 2015) as well as people who have completed their cancer treatment and seem to be disease free (Cella & Tross, 1987; Lagerdahl et al., 2014). The lack of research on death anxiety may be due to there being no agreed definition of clinically relevant death anxiety, and the commonly used measures of death anxiety were developed for patients with incurable disease and their validity has not been tested in other cancer populations (Sharpe et al., 2018).
Study Limitations
While our review of the literature on distress trajectories was comprehensive, there were some limitations. The review was not pre-registered. Also, the findings were limited to articles published in English. While it is possible that some important non-English publications may have been missed, this approach is a standard methodology for reviews of cancer-related themes (e.g. Arring et al., 2023; Hasson-Ohayon et al., 2022). Further, given that our review aimed to identify the clinical utility of research to date, we decided to use clinical terms in our search strategy, such as anxiety, depression and adjustment disorder, rather than a generic search term, such as distress. We expected that the course, predictors, and potential intervention targets of various clinically meaningful psychological states, such as anxiety or depression, would differ and would not be captured if these constructs were conflated into a broader category of distress. This may have meant that we failed to capture the diversity of people’s experiences of distress after a cancer diagnosis.
Furthermore, the generalisability of our findings to the broader cancer population may be limited due to several considerations. Arguably, study quality criteria relating to rates of study participation and attrition are particularly important for indicating the clinical importance or meaningfulness of results because these criteria demonstrate how representative the study samples are of the general cancer population, and therefore how well results reflect clinical cohorts in naturalistic settings. Across studies, rates of participation and attrition were not robust, and studies typically excluded individuals with advanced cancers, those who were very unwell, and those with a previous cancer diagnosis. Bias due to attrition was only low in two studies, and individuals who did not complete follow-up assessments were generally more psychologically distressed and physical unwell at baseline compared to those who completed all study measures (Alfonsson et al., 2016; Boyes et al., 2013; Mols et al., 2018). Given that poorer physical health status was associated with persistent depression or anxiety, it is likely that our findings underestimate the prevalence of clinically meaningful distress amongst individuals with cancer. Future longitudinal research should maximise recruitment inclusivity across all stages of cancer and systematically account for study attrition.
Additionally, consistent findings regarding distress trajectories were difficult to determine due to methodological heterogeneity. Studies varied by the number of follow-up assessments conducted and the number of trajectories identified, with possible implications for the proportion of patients assigned to each trajectory. Also, initial assessments ranged from close to diagnosis (Jansen et al., 2018), when distress may be expected to be higher, to years after diagnosis (Mols et al., 2018). Follow-up assessments were generally conducted at pre-determined study time points rather than at times that are clinically meaningful or personally relevant to cancer patients such as prior to surveillance scans, or around diagnosis anniversary dates. Also, whether patients were receiving active treatment was generally not assessed. Incomplete clinical data about the context in which assessments occurred limits the clinical utility and ecological validity of findings and precludes conclusions regarding the optimal time to assess psychological distress in routine care. Future longitudinal research should consider taking measurements from the point of diagnosis, followed by meaningful points along the cancer care pathway.
Furthermore, it is unclear whether the psychological assessments conducted in the reviewed studies were optimal. Only one sample completed a structured diagnostic interview (Kim et al., 2012, 2013, 2018), but minor and major depression were merged to categorise caseness, potentially confounding the findings. While the most frequently used self-report measure was the HADS, there has been debate regarding optimal cut-off values (Annunziata et al., 2020; Vodermaier et al., 2009), and concern over its use as a case-finding instrument (Mitchell, 2010). This highlights the need for foundational research to establish valid case-finding measures so that clinically meaningful research can be conducted.
Lastly, there was limited assessment of psychological variables predicting distress trajectories. Studies generally investigated demographic and medical variables with little evaluation of psychological constructs that may explain the aetiology or maintenance of distress and are responsive to psychotherapy. For instance, one interesting area of research is coping strategies and how they may impact on emotion regulation differently at various phases of diagnosis, treatment, survivorship, recurrence and end of life (cf. Kangas & Gross, 2020). Future longitudinal studies need to assess therapeutically relevant constructs informed by theoretical models of cancer-related distress.
Conclusions
This study aimed to examine the course of clinically relevant, individual trajectories of distress after a cancer diagnosis and the psychological, sociodemographic and medical factors associated with different distress trajectories. The limited findings from this review suggest that depression screening efforts should be particularly directed at patients with lung cancer. Also, longitudinal approaches to screening are needed to detect emerging depression and anxiety, since up to 1 in 5 patients developed depression in the first year after diagnosis and about 1 in 10 developed clinically relevant anxiety (Kim et al., 2020; Linden et al., 2015). The review also highlighted that consistent assessment timepoints across studies are needed to establish a wider evidence base to inform screening efforts. Furthermore, since assessments conducted at diagnosis or during clinic visits capture distress that is understandable and often subsides, more finely grained assessments, such as utilising smart phone applications, would be useful in future studies to understand when high distress is likely to be sustained. This would ensure that interventions are utilised efficiently, do not pathologize understandable distress and allow natural adaptation to occur, while ensuring that unremitting distress is treated as early as possible.
Understanding why distress develops, resolves or continues is important clinically to elucidate the protective and maintaining factors underpinning distress trajectories, thereby providing intervention targets that can be tailored to individual trajectories. The review suggests that symptom burden was the most consistent predictor of persistent distress, highlighting that mental health interventions should be multi-disciplinary in their approach. Furthermore, prior history should be screened as a potential predictor of depression. Disappointingly, there was limited information about other psychosocial predictors that could guide interventions. Future research should be guided by theoretical models of cancer-related distress, such as cognitive processing and metacognitive approaches (Cook et al., 2015; Curran et al., 2017; Edmondson, 2014; Fardell et al., 2016; Kangas & Gross, 2020), that may identify targets for treatments.
Data Availability
More detail about QUIPs assessment is available in Supplementary Materials.
Code Availability
Not applicable.
References
Alfonsson, S., Olsson, E., Hursti, T., Lundh, M. H., & Johansson, B. (2016). Socio-demographic and clinical variables associated with psychological distress 1 and 3 years after breast cancer diagnosis. Supportive Care in Cancer, 24, 4017–4023. https://doi.org/10.1007//s00520-016-3242y
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425596
Annunziata, M. A., Muzzatti, B., Bidoli, E., Flaiban, C., Bomben, F., Piccinin, M., Gipponi, K. M., Mariutti, G., Busato, S., & Mella, S. (2020). Hospital Anxiety and Depression Scale (HADS) accuracy in cancer patients. Supportive Care in Cancer, 28, 3921–3926. https://doi.org/10.1007/s00520-019-05244-8
Arring, N., Barton, D. L., & Reese, J. B. (2023). Clinical practice strategies to address sesxual health in female cancer survivors. Journal of Clinical Oncology, 41, 4927–4936. https://doi.org/10.1200/JCO.23.00523
Boyes, A. W., Girgis, A., D’Este, C. A., Zucca, A. C., Lecathelinais, C., & Carey, M. L. (2013). Prevalence and predictors of the short-term trajectory of anxiety and depression in the first year after a cancer diagnosis: A population-based longitudinal study. Journal of Clinical Oncology, 31, 2724–2729. https://doi.org/10.1200/JCO.2012.44.7540
Calman, L., Turner, J., Fenlon, D., Permyakova, N. V., Wheelwright, S., Patel, M., . . . members of the, C. S. A. C. (2021). Prevalence and determinants of depression up to 5 years after colorectal cancer surgery: results from the ColoREctal Wellbeing (CREW) study. Colorectal Disease, 23, 3234–3250. https://doi.org/10.1111/codi.15949.
Carpenter, K., Andersen, B., Fowler, J., & Maxwell, G. (2009). Sexual self schema as a moderator of sexual and psychological outcomes for gynecologic cancer survivors. Archives of Sexual Behavior, 38, 828–841. https://doi.org/10.1007/s10508-008-9349-6
Cataldo, J. K., & Brodsky, J. L. (2013). Lung cancer stigma, anxiety, depression and symptom severity. Oncology, 85, 33–40. https://doi.org/10.1159/000350834
Cella, D. F., & Tross, S. (1987). Death anxiety in cancer survival: A preliminary cross-validation study. Journal of Personality Assessment, 51, 451–461. https://doi.org/10.1207/s15327752jpa5103_12
Cook, S. A., Salmon, P., Dunn, G., Holcombe, C., Cornford, P., & Fisher, P. (2015). A prospective study of the association of metacognitive beliefs and processes with persistent emotional distress after diagnosis of cancer. Cognitive Therapy and Research, 39, 51–60. https://doi.org/10.1007/s10608014-9640-x
Cook, S. A., Salmon, P., Hayes, G., Byrne, A., & Fisher, P. L. (2018). Predictors of emotional distress a year or more after diagnosis of cancer: A systematic review of the literature. Psycho-Oncology, 27, 791–801. https://doi.org/10.1002/pon.4601
Curran, L., Sharpe, L., & Butow, P. (2017). Anxiety in the context of cancer: A systematic review and development of an integrated model. Clinical Psychology Review, 56, 40–54. https://doi.org/10.1016/j.cpr.2017.06.003
Curran, L., Sharpe, L., MacCann, C., & Butow, P. (2020). Testing a model of fear of cancer recurrence or progression: The central role of intrusions, death anxiety and threat appraisal. Journal of Behavioral Medicine, 43, 225–236. https://doi.org/10.1007/s10865-019-00129-x
Custers, J. A., Kwakkenbos, L., van der Graaf, W. T., Prins, J. B., Gielissen, M. F., & Thewes, B. (2020). Not as stable as we think: A descriptive study of 12 monthly assessments of fear of cancer recurrence among curatively-treated breast cancer survivors 0–5 years after surgery. Frontiers in Psychology, 11, 580979. https://doi.org/10.3389/fpsyg.2020.580979
Devins, G. M., Dion, R., Pelletier, L. G., Shapiro, C. M., Abbey, S., Raiz, L. R., Binik, Y. M., McGowan, P., Kutner, N. G., Beanlands, H., & Edworthy, S. M. (2001). Structure of lifestyle disruptions in chronic disease: A confirmatory factor analysis of the Illness Intrusiveness Ratings Scale. Medical Care, 39, 1097–1104. https://doi.org/10.1097/00005650-200110000-00007
Edmondson, D. (2014). An enduring somatic threat model of posttraumatic stress disorder due to acute life-threatening medical events. Social and Personality Psychology Compass, 8, 118–134. https://doi.org/10.1111/spc3.12089
Esser, P., Glaesmer, H., Faller, H., Koch, U., Härter, M., Schulz, H., Wegscheider, K., Weis, J., & Mehnert, A. (2019). Posttraumatic stress disorder among cancer patients—Findings from a large and representative interview-based study in Germany. Psycho-Oncology, 28, 1278–1285. https://doi.org/10.1002/pon.5079
Fardell, J. E., Thewes, B., Turner, J., Gilchrist, J., Sharpe, L., Smith, A., Girgis, A., & Butow, P. (2016). Fear of cancer recurrence: A theoretical review and novel cognitive processing formulation. Journal of Cancer Survivorship, 10, 663–673. https://doi.org/10.1007/s11764-015-0512-5
Hasegawa, T., Okuyama, T., Uchida, M., Aiki, S., Imai, F., Nishioka, M., Suzuki, N., Iida, S., Komatsu, H., Kusumoto, S., Ri, M., Osaga, S., & Akechi, T. (2019). Depressive symptoms during the first month of chemotherapy and survival in patients with hematological malignancies: A prospective cohort study. Psycho-Oncology, 28, 1687–1694. https://doi.org/10.1002/pon.5143
Hasson-Ohayon, I., Goldzweig, G., Braun, M., & Hagedoorn, M. (2022). Beyond “being open about it”: A systematic review on cancer related communication within couples. Clinical Psychology Review, 96, 102176. https://doi.org/10.1016/j.cpr.2022.102176
Hayden, J. A., van der Windt, D. A., Cartwright, J. L., Côté, P., & Bombardier, C. (2013). Assessing bias in studies of prognostic factors. Annals of Internal Medicine, 158, 280–286. https://doi.org/10.7326/0003-4819-158-4-201302190-00009
He, Y., Sun, L. Y., Peng, K. W., Luo, M. J., Deng, L., Tang, T., & You, C. X. (2022). Sleep quality, anxiety and depression in advanced lung cancer: Patients and caregivers. BMJ Supportive & Palliative Care, 12, e194–e200. https://doi.org/10.1136/bmjspcare-2018-001684
Henry, M., Fuehrmann, F., Hier, M., Zeitouni, A., Kost, K., Richardson, K., … Frenkiel, S. (2019). Contextual and historical factors for increased levels of anxiety and depression in patients with head and neck cancer: A prospective longitudinal study. Head & Neck, 41, 2538–2548. https://doi.org/10.1002/hed.25725.
Hopwood, P., & Stephens, R. J. (2000). Depression in patients with lung cancer: prevalence and risk factors derived from quality-of-life data. Journal of Clinical Oncology, 18, 893–903. https://doi.org/10.1200/jco.2000.18.4.893
Horowitz, M. M. D., Wilner, N. B. A., & Alvarez, W. M. A. (1979). Impact of event scale: A measure of subjective stress. Psychosomatic Medicine, 41, 209–218. https://doi.org/10.1097/00006842-197905000-00004
Jacobsen, P. B., Sadler, I. J., Booth-Jones, M., Soety, E., Weitzner, M. A., & Fields, K. K. (2002). Predictors of posttraumatic stress disorder symptomatology following bone marrow transplantation for cancer. Journal of Consulting and Clinical Psychology, 70, 235–240. https://doi.org/10.1037/0022-006X.70.1.235
Jansen, F., Verdonck-de Leeuw, I. M., Cuijpers, P., Leemans, C. R., Waterboer, T., Pawlita, M., Penfold, C., Thomas, A. W., & Ness, A. R. (2018). Depressive symptoms in relation to overall survival in people with head and neck cancer: A longitudinal cohort study. Psycho-Oncology, 27, 2245–2256. https://doi.org/10.1002/pon.4816
Kangas, M. (2013). DSM-5 trauma and stress-related disorders: Implications for screening for cancer-related stress. Frontiers in Psychiatry, 4, 122. https://doi.org/10.3389/fpsyt.2013.00122
Kangas, M., & Gross, J. (2020). The affect regulation in cancer framework: Understanding affective responding across the cancer trajectory. Journal of Health Psychology, 25, 7–25. https://doi.org/10.1177/1359105317748468
Kim, J., Cho, J., Lee, S. K., Choi, E. K., Kim, I. R., Lee, J. E., Seok, W. K., & Nam, S. J. (2020). Surgical impact on anxiety of patients with breast cancer: 12-month follow-up prospective longitudinal study. Annals of Surgical Treatment and Research, 98, 215–223. https://doi.org/10.4174/astr.2020.98.5.215
Kim, J. M., Kim, S. W., Stewart, R., Kim, S. Y., Shin, I. S., Park, M. H., Yoon, J. H., Lee, J. S., Park, S. W., Kim, Y. H., & Yoon, J. S. (2012). Serotonergic and BDNF genes associated with depression 1 week and 1 year after mastectomy for breast cancer. Psychosomatic Medicine, 74, 8–15. https://doi.org/10.1097/PSY.0b013e318241530c
Kim, J. M., Stewart, R., Kim, S. Y., Kang, H. J., Jang, J. E., Kim, S. W., Shin, I. S., Park, M. H., Yoon, J. H., Park, S. W., Kim, Y. H., & Yoon, J. S. (2013). A one year longitudinal study of cytokine genes and depression in breast cancer. Journal of Affective Disorders, 148, 57–65. https://doi.org/10.1016/j.jad.2012.11.048
Kim, S. Y., Kim, S. W., Shin, I. S., Park, M. H., Yoon, J. H., Yoon, J. S., & Kim, J. M. (2018). Changes in depression status during the year after breast cancer surgery and impact on quality of life and functioning. General Hospital Psychiatry, 50, 33–37. https://doi.org/10.1016/j.genhosppsych.2017.09.009
Krebber, A. M. H., Buffart, L. M., Kleijn, G., Riepma, I. C., de Bree, R., Leemans, C. R., Becker, A., Burg, J., van Straten, A., Cuijpers, P., & Verdonck-de Leeuw, I. M. (2014). Prevalence of depression in cancer patients: A meta-analysis of diagnostic interviews and self-report instruments. Psycho-Oncology, 23, 121–130. https://doi.org/10.1002/pon.3409
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9. Journal of General Internal Medicine, 16, 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Kuba, K., Esser, P., Scherwath, A., Schirmer, L., Schulz-Kindermann, F., Dinkel, A., Balck, F., Koch, U., Kroger, N., Gotze, H., & Mehnert, A. (2017). Cancer-and-treatment-specific distress and its impact on posttraumatic stress in patients undergoing allogeneic hematopoietic stem cell transplantation (HSCT). Psycho-Oncology, 26, 1164–1171. https://doi.org/10.1002/pon.4295
Lagerdahl, A. S., Moynihan, M., & Stollery, B. (2014). An exploration of the existential experiences of patients following curative treatment for cancer: Reflections from a U.K. sample. Journal of Psychosocial Oncology, 32, 555–575. https://doi.org/10.1080/07347332.2014.936647
Linden, W., MacKenzie, R., Rnic, K., Marshall, C., & Vodermaier, A. (2015). Emotional adjustment over 1 year post-diagnosis in patients with cancer: Understanding and predicting adjustment trajectories. Supportive Care in Cancer, 23, 1391–1399. https://doi.org/10.1007/s00520-014-2492-9
Linden, W., Yi, D., Barroetavena, M. C., MacKenzie, R., & Doll, R. (2005). Development and validation of a psychosocial screening instrument for cancer. Health and Quality of Life Outcomes, 3, 54. https://doi.org/10.1186/1477-7525-3-54
Liu, Y., Pettersson, E., Schandl, A., Markar, S., Johar, A., & Lagergren, P. (2022). Psychological distress after esophageal cancer surgery and the predictive effect of dispositional optimism: A nationwide population-based longitudinal study. Supportive Care in Cancer, 30, 1315–1322. https://doi.org/10.1007/s00520-021-06517-x
Lo, C., Hales, S., Zimmermann, C., Gagliese, L., Rydall, A., & Rodin, G. (2011). Measuring death-related anxiety in advanced cancer: Preliminary psychometrics of the death and dying distress scale. Journal of Pediatric Hematology/oncology, 33, S140–S145. https://doi.org/10.1097/MPH.0b013e318230e1fd
Lopes, C., Lopes-Conceicao, L., Fontes, F., Ferreira, A., Pereira, S., Lunet, N., & Araujo, N. (2022). Prevalence and persistence of anxiety and depression over five years since breast cancer diagnosis—the NEON-BC prospective study. Current Oncology, 29, 2141–2153. https://doi.org/10.3390/curroncol29030173
Menzies, R. E., Sharpe, L., Helgadóttir, F. D., & Dar-Nimrod, I. (2021). Overcome death anxiety: The development of an online cognitive behaviour therapy programme for fears of death. Behaviour Change, 38, 235–249. https://doi.org/10.1017/bec.2021.14
Mitchell, A. J. (2010). Short screening tools for cancer-related distress: A review and diagnostic validity meta-analysis. Journal of the National Comprehensive Cancer Network, 8, 487–494. https://doi.org/10.6004/jnccn.2010.0035
Mols, F., Schoormans, D., de Hingh, I., Oerlemans, S., & Husson, O. (2018). Symptoms of anxiety and depression among colorectal cancer survivors from the population-based, longitudinal PROFILES Registry: Prevalence, predictors, and impact on quality of life. Cancer, 124, 2621–2628. https://doi.org/10.1002/cncr.31369
Mutsaers, B., Butow, P., Dinkel, A., Humphris, G., Maheu, C., Ozakinci, G., . . . Lebel, S. (2020). Identifying the key characteristics of clinical fear of cancer recurrence: An international Delphi study. Psycho-Oncology, 29, 430–436. https://doi.org/10.1002/pon.5283.
Neel, C., Lo, C., Rydall, A., Hales, S., & Rodin, G. (2015). Determinants of death anxiety in patients with advanced cancer. BMJ Supportive and Palliative Care, 5, 373–380. https://doi.org/10.1136/bmjspcare-2012-000420
Niedzwiedz, C. L., Knifton, L., Robb, K. A., Katikireddi, S. V., & Smith, D. J. (2019). Depression and anxiety among people living with and beyond cancer: A growing clinical and research priority. BMC Cancer, 19, 943. https://doi.org/10.1186/s12885-019-6181-4
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., . . . Moher, D. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Systematic Reviews, 10, 89. https://doi.org/10.1186/s13643-021-01626-4.
Richardson, E. M., Schüz, N., Sanderson, K., Scott, J. L., & Schüz, B. (2017). Illness representations, coping, and illness outcomes in people with cancer: A systematic review and meta-analysis. Psycho-Oncology, 26, 724–737. https://doi.org/10.1002/pon.4213
Rogiers, A., Leys, C., De Cremer, J., Awada, G., Schembri, A., Theuns, P., De Ridder, M., & Neyns, B. (2020). Health-related quality of life, emotional burden, and neurocognitive function in the first generation of metastatic melanoma survivors treated with pembrolizumab: A longitudinal pilot study. Supportive Care in Cancer, 28, 3267–3278. https://doi.org/10.1007/s00520-019-05168-3
Savard, J., & Ivers, H. (2013). The evolution of fear of cancer recurrence during the cancer care trajectory and its relationship with cancer characteristics. Journal of Psychosomatic Research, 74, 354–360. https://doi.org/10.1016/j.jpsychores.2012.12.013
Schabath, M. B., & Cote, M. L. (2019). Cancer progress and priorities: lung cancer. Cancer Epidemiology, Biomarkers & Prevention, 28, 1563–1579. https://doi.org/10.1158/1055-9965.Epi-19-0221
Shand, L. K., Cowlishaw, S., Brooker, J. E., Burney, S., & Ricciardelli, L. A. (2015). Correlates of post-traumatic stress symptoms and growth in cancer patients: A systematic review and meta-analysis. Psycho-Oncology, 24, 624–634. https://doi.org/10.1002/pon.3719
Sharpe, L., Curran, L., Butow, P., & Thewes, B. (2018). Fear of cancer recurrence and death anxiety. Psycho-Oncology, 27, 2559–2565. https://doi.org/10.1002/pon.4783
Silver-Aylaian, M., & Cohen, L. H. (2001). Role of major lifetime stressors in patients’ and spouses’ reactions to cancer. Journal of Traumatic Stress, 14, 405–412. https://doi.org/10.1023/A:1011129321431
Smith, S. K., Zimmerman, S., Williams, C. S., Benecha, H., Abernethy, A. P., Mayer, D. K., Edwards, L. J., & Ganz, P. A. (2011). Post-traumatic stress symptoms in long-term non-Hodgkin’s lymphoma survivors: Does time heal? Journal of Clinical Oncology, 29, 4526–4533. https://doi.org/10.1200/JCO.2011.37.2631
Stanton, A. L., Wiley, J. F., Krull, J. L., Crespi, C. M., Hammen, C., Allen, J. J., Barron, M., Jorge, A., & Weihs, K. L. (2015). Depressive episodes, symptoms, and trajectories in women recently diagnosed with breast cancer. Breast Cancer Research and Treatment, 154, 105–115. https://doi.org/10.1007/s10549-015-3563-4
Starreveld, D. E. J., Markovitz, S. E., van Breukelen, G., & Peters, M. L. (2018). The course of fear of cancer recurrence: Different patterns by age in breast cancer survivors. Psycho-Oncology, 27, 295–301. https://doi.org/10.1002/pon.4505
Sullivan, D. R., Forsberg, C. W., Ganzini, L., Au, D. H., Gould, M. K., Provenzale, D., & Slatore, C. G. (2016). Longitudinal changes in depression symptoms and survival among patients with lung cancer: A national cohort assessment. Journal of Clinical Oncology, 34, 3984–3991. https://doi.org/10.1200/JCO.2016.66.8459
Sutton, T. L., Koprowski, M. A., Grossblatt-Wait, A., Brown, S., McCarthy, G., Liu, B., . . . Sheppard, B. C. (2022). Psychosocial distress is dynamic across the spectrum of cancer care and requires longitudinal screening for patient-centered care. Supportive Care in Cancer, 30, 4255–4264. https://doi.org/10.1007/s00520-022-06814-z
Swartzman, S., Booth, J. N., Munro, A., & Sani, F. (2017). Posttraumatic stress disorder after cancer diagnosis in adults: A meta-analysis. Depression and Anxiety, 34, 327–339. https://doi.org/10.1002/da.22542
Thewes, B., Husson, O., Poort, H., Custers, J. A. E., Butow, P. N., McLachlan, S. A., & Prins, J. B. (2017). Fear of cancer recurrence in an era of personalized medicine. Journal of Clinical Oncology, 35, 3275–3278. https://doi.org/10.1200/JCO.2017.72.8212
Turvey, C. L., Wallace, R. B., & Herzog, R. (1999). A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. International Psychogeriatrics, 11, 139–148. https://doi.org/10.1017/S1041610299005694
Vin-Raviv, N., Hillyer, G. C., Hershman, D. L., Galea, S., Leoce, N., Bovbjerg, D. H., … Neugut, A. I. (2013). Racial disparities in posttraumatic stress after diagnosis of localized breast cancer: the BQUAL study. Journal of the National Cancer Institute, 105, 563–572. https://doi.org/10.1093/jnci/djt024.
Vodermaier, A., Linden, W., & Siu, C. (2009). Screening for emotional distress in cancer patients: A systematic review of assessment instruments. Journal of the National Cancer Institute, 101, 1464–1488. https://doi.org/10.1093/jnci/djp336
Watts, S., Prescott, P., Mason, J., McLeod, N., & Lewith, G. (2015). Depression and anxiety in ovarian cancer: A systematic review and meta-analysis of prevalence rates. British Medical Journal Open, 5, e007618. https://doi.org/10.1136/bmjopen-2015-007618
Weathers, F. W., Litz, B. T., Herman, D. S., Huska, J. A., & Keane, T. M. (1993). The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the annual convention of the international society for traumatic stress studies, San Antonio, TX.
Wijnhoven, L., Custers, J., Kwakkenbos, L., & Prins, J. (2022). Trajectories of adjustment disorder symptoms in post-treatment breast cancer survivors. Supportive Care in Cancer, 30, 3521–3530. https://doi.org/10.1007/s00520-022-06806-z
Zigmond, A., & Snaith, R. (1983). The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica, 67, 361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. Partial financial support was provided by Health@Business Research Network, School of Management and Governance, University of New South Wales, Australia.
Author information
Authors and Affiliations
Contributions
LC designed the study, conducted the systematic literature review and independently rated included articles for bias. AM reviewed the selection of articles and independently conducted a full-text review of selected articles and a bias assessment. LC and AM wrote the first draft of the manuscript with detailed revisions provided by BH. All authors contributed to and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors Leah Jane Curran, Alison Mahoney, and Bradley Hastings declare that they have no conflict of interest.
Human and Animal Rights
No new data was collected from human subjects for this review. All studies included in the review received ethics approval prior to initiation of study procedures.
Informed Consent
All studies included in the review ensured that informed consent was obtained from study participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Curran, L., Mahoney, A. & Hastings, B. A Systematic Review of Trajectories of Clinically Relevant Distress Amongst Adults with Cancer: Course and Predictors. J Clin Psychol Med Settings (2024). https://doi.org/10.1007/s10880-024-10011-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s10880-024-10011-x