Abstract
There is a growing demand for three-dimensional scaffolds for expanding applications in regenerative medicine, tissue engineering, and cell culture techniques. The material requirements for such three-dimensional structures are as diverse as the applications themselves. A wide range of materials have been investigated in the recent decades in order to tackle these requirements and to stimulate the anticipated biological response. Among the most promising class of materials are inorganic/organic hydrogel composites for regenerative medicine. The generation of synergetic effects by hydrogel composite systems enables the design of materials with superior properties including biological performance, stiffness, and degradation behavior in vitro and in vivo. Here, we review the most important organic and inorganic materials used to fabricate hydrogel composites. We highlight the advantages of combining different materials with respect to their use for biofabrication and cell encapsulation as well as their application as injectable materials for tissue enhancement and regeneration.
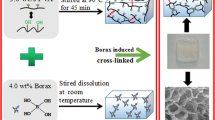
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nearly all cells in the body are situated in a three-dimensional architecture [1]. Geometry and arrangement of these three-dimensional structures have strong influences on cell morphology, function, and fate. In order to understand the governing complex mechanical and biochemical interactions, three-dimensional (3D) model systems are required [2, 3]. By designing cell culture systems which are able to mimic or simulate the behavior of native tissue, profound insights into the fundamental biological processes are accessible [4]. There are various other motivations for the development of 3D scaffolds and cell culture units. From the design of more physiologically relevant culture systems in biological analysis and drug development to the regeneration of malign or destroyed tissue, almost all areas of modern biology, medicine, biotechnology, and life science are affected by these new developments. Tissue engineering (TE), for example, aims to create artificial tissues that are able to exhibit native processes and functions [5, 6]. Cells are incorporated into a three-dimensional scaffold which can then be delivered into the injured or diseased site. Subsequently, the material can either be integrated into the native tissue or it can stimulate the formation of new tissue accompanied by its own degradation. Therefore, the availability of TE materials with precisely controlled physical and chemical properties and well-defined biological responses is essential, and the biomaterial used must be adapted to the environmental conditions of the biological site [5]. These conditions are rather complex considering the requirement of highly flexible and soft materials for skin, cartilage, and soft tissue regeneration to hard, load-bearing materials in bone TE.
The dissimilarity and complexity of the potential applications render the design of scaffold materials extremely versatile and challenging. However, there are some fundamental requirements that all scaffold materials need to fulfill, which are as follows: 1. All included materials and applied processing techniques need to be biocompatible. 2. The scaffold needs to be able to withstand the mechanical stresses applied to the system and maintain its mechanical integrity over its lifetime. 3. The microstructure of the material should enable cellular attachment, and in the ideal case, the integration into the surrounding biological microenvironment. 4. Highly porous systems are mandatory to enable cellular migration and proliferation as well as the potential ingrowth of surrounding tissue and blood vessels (angiogenesis). Less prominent but nevertheless important considerations are the controlled stimulation of the anticipated cellular response, namely proliferation, migration, organization, and differentiation. These complex requirements are further complicated by the need for easy and convenient sterilization, handling, and processing procedures of all included materials.
Many materials have been applied to develop scaffolds including numerous synthetic and natural polymers as well as inorganic materials, ceramics, and glasses, and their combinations. By combining different materials, one can benefit from the advantages of both materials while limiting, or in the ideal case eliminating, their individual disadvantages. When the materials are chosen wisely, composite scaffolds emerge which exhibit properties that are more than the sum of its parts [5–7]. Hydrogels, for example, provide excellent environments for cell encapsulation and culture due to their structural resemblance to the extracellular matrix found in vivo [8]. Cells can be incorporated into a hydrogel’s three-dimensional network which offers structural support while enabling the transport of nutrients, oxygen, and metabolites to and from the encapsulated cells [9–11]. Hydrogels are not only useful for in vitro studies (cellular behavior) in three dimensions, but they are also capable of delivering cells in a controlled manner using appropriate carrier morphologies. In addition, via the incorporation of magnetic moieties into the carrier system, the delivery can be magnetically triggered and actuated [12, 13]. Besides the generation of micrometer-sized cell-containing hydrogel capsules via emulsification methods, new approaches, grouped in the field of biofabrication techniques, are currently uprising [14–16]. The high viscosity of polymeric precursor solutions and their rapid gelation in the presence of appropriate cues render hydrogels as promising candidates for 3D printing and bioplotting processes [17]. These new manufacturing techniques enable the generation of arbitrary structures with precise control of shape and dimensions, which can be used for the creation of 3D tissue models or for the replacement of damaged tissue in TE applications. However, in some cases, a precise knowledge of a given defect or the injured tissue site’s dimensions is not accessible or too complex to be replicated. In this case, injectable materials are an obvious choice. The injection of a hydrogel precursor solution and the subsequent triggered network formation are attractive considering the highly flexible nature of hydrogels which will adapt to the given environmental conditions. Damaged tissue sites can thus be filled in a rapid, convenient, and minimal invasive fashion.
Although the discussed practices make hydrogels an outstanding basis for biomedical and TE applications, their low mechanical strength and unsuitable degradation behavior often limit their applicability. By the addition of inorganic fillers, the hydrogel’s properties can often be enhanced and further adapted to a variety of applications. Mechanical properties, degradation behavior, and cell–material interactions are among the most dominantly affected characteristics resulting from the addition of inorganic materials to polymeric hydrogel networks. In this review paper, we aim to discuss the current state-of-the-art technology in the field of composite materials based on hydrogel networks incorporating rigid inorganic fillers for biomedical applications. An overview with regard to the general characteristics of hydrogels and relevant properties of available inorganic rigid fillers, which captures the overall goal of this paper, is illustrated in Fig. 1. Several reviews about hydrogel nanocomposites for biomedical applications are available [5, 7, 18, 19]. Here, we focus on studies which have actually demonstrated the ability of these materials to be processed in (i) bioprinting or bioplotting, as techniques as (ii) injectable materials or as (iii) matrix materials for cell encapsulation. We thus explicitly concentrate in this review article on the addition of pre-formed inorganic moieties to the hydrogel structure. The in-situ mineralization of polymeric materials is not within the scope of this review since these methods have already been summarized in a comprehensive review by Kretlow et al. [20]. Other review papers [21–23] have covered polymer matrix composites for TE scaffolds.
In the following sections, we discuss different kinds of hydrogels and inorganic materials used for the generation of composite scaffolds. We briefly highlight their general characteristics before outlining the difficulties and problems arising from the use of pure organic or inorganic materials. Afterward, we review promising composites and discuss the effects and origins of the arising material’s properties. Overall, this review intends to present a comprehensive summary of the field of hydrogel–inorganic filler composites, given the increasing interest in their use for the fabrication of scaffolds and matrices via 3D biofabrication, cell encapsulation, and injectable systems.
Hydrogels
Hydrogels are hydrophilic, physically or chemically crosslinked polymeric materials, which are specifically well known for their enormous water-uptake capacity [24, 25]. In biomedical and biotechnological applications, hydrogels are a commonly applied class of materials. Their structural resemblance to the extracellular matrix found in vivo makes them an excellent substrate for cell culture applications. In addition, their high water content and biocompatibility allow the cultivation of living cells inside the polymeric network structure which can conveniently be shaped and structured into various geometries [5]. The highly elastic nature of most hydrogels allows for easy manufacturing and adaption to environmental influences [26]. By controlling the chemical composition and crosslinking density, network structure and pore size can be tuned and customized for a given application [26]. Chemical modification of the polymeric chains allows for the incorporation of functional motives like integrin-binding sites promoting cellular attachment, for example. Not only the chemical properties of the hydrogel can be modified but also the physical characteristics of the hydrogel are adjustable. The mechanical properties of most hydrogels can be influenced by altering the degree of crosslinking or the incorporation of additional binding sites via physical crosslinking. Another beneficial effect is the stimulus-responsive behavior of some polymers like poly(N-isopropylacrylamide) (pNIPAAm) [27, 28]. These stimulus-responsive properties can be used to load the polymers with drugs or growth factors which will be subsequently released upon stimulation of the appropriate physical or chemical clues [12, 13, 29–31].
The decision regarding the use of hydrogels derived from natural sources or synthetic polymers depends on the aspired properties and applications, and it is vigorously discussed in the literature [24, 32, 33]. While natural polymers are typically characterized by a high degree of biocompatibility, they lack reliability and consistency due to their natural origin leading to troublesome batch-to-batch variations. By contrast, synthetic polymers are highly reproducible materials with precisely controlled chemical and physical characteristics. Unfortunately, they are classically less biocompatible than natural biopolymers either due to the material properties themselves or due to harmful residues arising from the manufacturing process which often involves cytotoxic or non-biocompatible organic solvents, starting monomers, or by-products [34].
In the following section, we review the most important hydrogels used in biofabrication techniques, as injectable materials and as 3D matrices for cell culture applications.
Natural polymers
Collagen
As the main structural protein in connective tissue, collagen, especially collagen type I, is among the most prominent biopolymers for TE and biofabrication applications. Each collagen molecule consists of three left-handed polypeptide helices. The three helices are staggered together to form a right-handed triple helix [35]. These so-called tropocollagen subunits spontaneously self-assemble into fibrils which themselves assemble into larger fibers and bundles. This highly organized structure is the origin of collagens extraordinary tensile strength [36, 37]. In addition, collagen offers integrin-binding sites allowing for an excellent attachment of adherent cells [36, 38, 39]. In vivo, collagen is degraded by enzymatic reactions [36].
Collagen can either be used in the form of soluble collagen which is subsequently transformed into reconstituted collagen or in the form of tissue-derived collagen. In the latter case, a mild enzyme treatment is used to remove non-collagenous proteins from natural tissue. The remaining insoluble collagenous material is comminuted to obtain collagen powder. Collagen-based materials are available in various forms and architectures including sheets, membranes, sponges, gels, and fibers. However, pristine collagen materials are typically characterized by poor mechanical properties making them inherently unstable. This drawback can be overcome by densification or composite formation with other structural proteins like elastin [40–43].
Hyaluronic acid (HA)
Hyaluronic acid (HA) is a linear polysaccharide or more specifically a glycosaminoglycan (GAG) consisting of alternating units of glucuronic acid and N-acetylglucosamine (see Table 1 for chemical structure) [44, 45]. HA is accessible with molecular weights ranging from 100000 to 8000000 g/mol. The extremely high water-uptake ability (up to 6 L/1 g) results from the highly negative charge of the polymeric chains. The high affinity to positively charged ions results in an osmotic pressure which drives water into the polymer [44]. Since water is noncompressible, HA is able to resist high compressive forces in its hydrated state. It is found throughout the human body, most prominently as a structural component in the extracellular matrix (ECM) where it contributes to embryonic development, morphogenesis, tissue organization, wound healing, cell signaling, proliferation, and migration [44, 45]. Several cell receptors for HA have been identified including CD44 which is expressed in a large number of mammalian cell types [44]. Its natural appearance in the extracellular matrix as well as chemical structure, which offers convenient chemical modification, makes HA an excellent starting material for biotechnological techniques. In vivo, HA is degraded by hyaluronidase within hours to days. By chemical crosslinking of the HA chains via carbodiimide, click, and photochemistry, or the incorporation of thiols, methacrylates, dihydrazides, etc., the degradation times can be significantly improved, and long-term stability can be achieved [44, 46, 47]. Furthermore, the introduction of crosslinking points allows for the generation of network structures with controlled pore sizes [44].
Alginate
Alginate is a linear polysaccharide isolated from brown algae consisting of alternating units of α-l-guluronic acid (G) and β-d-mannuronic acid (M) (Table 1) [48, 49]. Molecular weight and its distribution as well as M-to-G block ratio and sequence depend on the origin of alginate and vary over a wide range. Alginates with molecular weights between 50000 and 100000000 g/mol are available [48]. Alginate can be ionically crosslinked in the presence of bivalent cations, most commonly Ca2+, where two G units chelate one bivalent ion in the so-called egg-box configuration [49]. Properties like stiffness and pore size of the resulting hydrogel depend on the molecular weight and molecular weight distribution, the M/G ratio, and the concentration of polymer and crosslinking ions [48]. Under neutral conditions, ionically crosslinked alginate hydrogels degrade slowly and become uncontrolled upon losing chelated ions [48]. The degradation behavior can be controlled by manipulating the polymer’s molecular weight using gamma-irradiation resulting in lower molecular weights and accelerated degradation behavior [50]. Degradation can also be enhanced by chemical partial oxidation by hydrolysis with sodium periodate [51, 52]. The resulting ring-opening cleavage of the carbon–carbon bond generates an uronate residue which is susceptible to hydrolytic degradation. Alginate can be easily chemically modified either by carbodiimide coupling via the carboxylic groups or by Schiff’s base formation via the aldehyde groups resulting from oxidation [52]. The Schiff’s base reaction can also be used to introduce additional, in this case, covalent crosslinking points. This also allows for the incorporation of different polymeric chains, which significantly alters the hydrogel’s mechanical properties, degradation profile, and cell–matrix interactions [53]. Alginate itself does not offer cellular-binding sites which can be introduced by the covalent coupling with biomolecules like gelatin or the EDC-mediated coupling with integrin-binding sites like the tripeptide arginylglycylaspartic acid (Arg-Gly-Asp, RGD) [52, 54–58].
Agarose
Agarose is a linear polysaccharide extracted from seaweed. It is formed by the a bisaccharide of β-d-galactose and 3,6-anhydro-α-l-galactopyranose and most commonly known as component of agar [59]. Agarose can be dissolved in hot water and forms a gel upon cooling due to the formation of double helices and their subsequent aggregation [60]. The gelation process is thermoreversible with gelation temperatures depending on the type of agarose or more specifically on the methoxy content [61]. Agarose forms physically and chemically strong gels even at concentrations below 1 % [61]. Due to its large pores (100–500 nm) and adjustable pore sizes which depend on the agarose concentration, agarose gels offer high diffusion rates and are commonly used as filters, sieves, or purification systems [62, 63].
Gelatin
Gelatin is a biodegradable protein which is produced by acidic or basic hydrolysis of collagen from porcine or bovine skin, respectively. There are two types of gelatin available depending on the origin and extraction reaction: cationic gelatin with an isoelectric point (IEP) of 9 (Gelatin A) and anionic gelatin with an IEP of 5 (Gelatin B) [64]. The hydrolysis of animal skin results in the breaking-up of collagen’s triple helix structure producing random polymeric gelatin chains [52, 65]. Upon cooling, the random coils partially reassemble into a triple helix structure resulting in the formation of a three-dimensional hydrogel network [66–68]. In vivo, gelatin is enzymatically degraded without the production of harmful side products. In addition, gelatin contains the RGD sequence of collagen which offers integrin-binding sites and promotes cell adhesion [52].
Gellan gum (GG)
Gellan gum (GG) is a linear polysaccharide consisting of a tetrasaccharide repeat unit composed of two molecules of d-glucose, one of d-glucuronic acid and one of l-rhamnose [69]. GG is produced by bacteria and has an average molecular weight of approximately 500 kDa [69]. At low temperatures, it forms ordered double-stranded helices which are transformed into single-stranded chains at higher temperature making the viscosity of GG solutions highly temperature dependent [70]. The transition occurs at about 35 °C. In vivo, GG degradation occurs via enzymatic cleavage in the d-glucose, d-glucuronic acid site, by gellan lyases [70]. In analogy to alginate, GG forms hydrogels in the presence of bivalent ions and does not offer integrin-binding sites.
Chitosan
Chitosan is a linear polysaccharide consisting of β-(1-4)-linked d-glucosamine and N-acetyl-d-glucosamine (Table 1). It is derived by partial deacetylation of chitin. Its molecular weight ranges from 300 to 1000 kDa depending on origin and preparation method [71]. Under basic conditions, chitosan is insoluble in water but it can be dissolved in diluted acids with pH values below 6. Its ability to form hydrogels is based on the formation of hydrogen bonds, thus being highly pH dependent. Chitosan can also be complexed with polyanions due to its high charge density resulting in three-dimensionally crosslinked composites [71, 72]. Furthermore, chitosan can be easily functionalized via its hydroxyl or amino groups. In vivo, chitosan is mainly degraded through lysozyme-mediated hydrolysis [71, 73].
Matrigel
Matrigel is a commercially available hydrogel based on a protein mixture isolated from the Engelbreth–Holm–Swarm (EHS) mouse sarcoma, a tumor rich in extracellular matrix protein [74]. Matrigel is composed of several structural proteins found in the extracellular matrix like laminin and collagen making it an excellent substrate for adherent cells. Additional additives like growth factors and proteins are also included. Unfortunately, the composition of Matrigel is not too well described, which can cause variability in experimental results thus leading to problems in data analysis and reproducibility [75]. At temperatures between 22 and 35 °C, Matrigel polymerizes rapidly into a three-dimensional hydrogel network. At 4 °C, Matrigel starts to liquefy. Consequently, sample preparation and processing need to be performed under cold conditions.
Others
There is a large variety of available biopolymers suitable for TE applications. Besides the discussed materials various animal-derived proteins like elastin and silk as well as plant proteins, e.g., cellulose, soy protein, zein, and their composites have already been explored [42, 76–80]. Although all these proteins are able to form hydrogels, few of them have been used in combination with inorganic fillers so far.
Synthetic hydrogels
Poly(ethylene glycol) (PEG) and derivatives
Poly(ethylene glycol) (PEG), also known as poly(ethylene oxide) (PEO) or poly(oxyethylene) (POE), is one of the most prominent examples of synthetic polymers used for biomedical and biotechnological applications. The chemical structure of PEG is giving in Table 1. It is available over a broad range of molecular weights covering values between 300 and 10000000 g/mol [81]. There are also various geometries like linear, branched or combed chains available. The nature of the polymer’s end groups depends on the synthetic procedure and allows the introduction of specific functional groups or the linkage to other polymers. Like all polyethers, PEG is highly biocompatible [82]. Nevertheless, it is resistant to hydrolytic or enzymatic degradation causing concern about accumulation effects of PEG-based biomaterials [82]. Integrin or other cell-binding sites need to be specifically incorporated into the polymeric matrix to enable cellular attachment. PEG-based hydrogels can be formed by various mechanisms including physical, ionic, or covalent crosslinking. However, the highest mechanical stability can be achieved by covalent crosslinking, for example, by the incorporation of diacrylate units into the PEG chains (PEGDA) which can be used to form double bonds upon UV-irradiation [83, 84]. One drawback of PEG and its derivatives is the generation of acidic by-products by poly(acrylic acid) generation during degradation [82].
Cyclic acetals are a class of PEG derivatives synthesized from poly(ethylene glycol) diacrylate (PEGDA) and 5-ethyl-5-(hydroxymethyl)-β, β-dimethyl-1,3-dioxane-2-ethanol diacrylate (EHD). In contrast to classic polyesters, these materials do not produce acidic by-products during degradation [85]. In addition, they have been reported to support cell adhesion [86].
Poly(acrylic acid) (PAA) and its derivatives
Poly(acrylic acid) (PAA) and its derivatives are among the most intensively studies synthetic polymers for biomedical application (see Table 1 for chemical structure) [87]. Hydrophilicity, swelling behavior, and permeability of these ionic hydrogels depend on the crosslinking agent, pH value, and ion composition of the surrounding solution [24, 87].
The PAAc derivative poly(2-hydroxyethyl methacrylate) (pHEMA) exhibits an excellent optical transparency and stability in water making pHEMA-based hydrogels excellent candidates for ophthalmic applications like intraocular lenses [87]. pHEMA hydrogels have also been used in drug delivery applications [88]. The chemical structure of pHEMA is displayed in Table 1. Pure pHEMA hydrogels are not biodegradable. However, chemical modification like the introduction of dextran can be used to induce the degradation behavior of these polymers [87, 89].
Poly(N-isopropylacrylamide (pNIPAAm, also pNIPAm) is a temperature-responsive PAA derivative (Table 1). This classic example for stimuli-responsive or smart polymers displays a reversible lower critical solution temperature (LCST) phase transition at approximately 33 °C [90]. The phase-transition temperature can be manipulated by chemical modification [91]. Having a LCST in the range of body temperature makes pNIPAAm an excellent drug delivery material. It can be loaded with biomolecules in vitro which will subsequently be released in vivo due to the collapse of the gel [27, 28, 92, 93]. pNIPAAm is nonbiodegradable, and RGD or other cell-binding motifs need to be incorporated for cellular attachment.
Semi-synthetic polymers
Semi-synthetic polymers are chemically modified or functionalized polymers from natural origin. This approach combines the advantages of biopolymers with the benefits of the chemical control of the material properties known from synthetic polymers. Thus, the materials’ chemical and physical properties can be tailored specifically for the particular application, while the common characteristics of naturally derived polymers like biocompatibility, biodegradability, and the presence of cell-binding sites are maintained.
Gelatin methacrylate (GelMA)
The gelation of gelatin is a temperature-dependent, reversible process [66]. In addition, gelatin is rapidly degraded in vivo. Consequently, the use of gelatin hydrogels as scaffold materials for TE is limited to temporary applications. The introduction of vinyl methacrylate groups into the polymeric backbone allows the generation of permanent, covalent crosslinking points [94]. The vinyl methacrylate groups can thereby react between themselves or with vinyl groups of other small molecules, oligomers, or polymers via photo- or temperature-initiated radical polymerization.
Hydroxypropylmethylcellulose (HPMC)
Hydroxypropylmethylcellulose (HPMC) is prepared by high-temperature reaction between cellulose, propylene oxide, and methylchloride (see, Table 1 for chemical structure). It shows a lower critical solution temperature resulting in the gelation of aqueous HPMC solution upon heating to 75–90 °C. This reversible gelation is mainly induced by interactions between the methoxy side groups which makes HPMC-based systems attractive candidates for drug delivery applications [95, 96]. The gelation temperature is antiproportional to the degree of hydroxypropyl functionalization and can thus be easily adjusted. Silane-grafted HPMC (Si-HPMC) has been reported as self-setting injectable material. Under certain pH conditions, the silane groups are transformed into silanol groups which react with each other in a condensation reaction resulting in the formation of a three-dimensional network structure [97].
Challenges of hydrogels
Hydrogels offer many advantages for TE and cell encapsulation applications. However, their mechanical strength is typically too low to persist in load-bearing applications [26, 32]. In addition, the biodegradation behaviors of many polymers are not suitable for TE applications. Many of the hydrogels discussed above degenerate too fast, and the degradation is accompanied by the generation of acidic byproducts [82, 98, 99]. Another issue is the lack of cell-binding sites especially regarding synthetic polymers [32]. In the absence of cell-binding sites, the stimulation of cellular adhesion and cell–matrix interactions are difficult to achieve. Consequently, cellular behaviors like phenotypic modification and differentiation cannot easily be controlled [26]. Thus, the missing materials’ properties need to be introduced by either chemical modification or the incorporation of a second material exhibiting the required characteristics [25, 26, 32]. Table 2 summarizes the discussed hydrogel-forming systems and highlights their most prominent advantages and disadvantages.
Inorganic materials
Inorganic nanoparticles, namely glasses, salts, and polycrystalline ceramics, offer high specific surface areas, in some cases, being enhanced by a highly porous structure and high protein adsorption. The adsorption of extracellular matrix glycoproteins like fibronectin and vitronectin is likely to provide cell-binding sites causing cells to adhere to the surface of inorganic (nano)materials [100]. Besides these adhesive effects, several inorganic materials, especially silicate glasses and calcium phosphates, termed bioactive ceramics, are known for their release of ionic species during their dissociation. Many of these ions have significant biological effects on cell proliferation, gene expression, differentiation, and extracellular matrix mineralization [101]. By doping these materials with additional ions like Zn, Sr, Mg, and Cu, the biological effects of tracer elements can also be investigated and exploited [101]. Additional effects of inorganic nanomaterials like anisotropy or electrical stimulation using metallic or carbonaceous particles of different shapes can be used for the controlled direction and organization of cellular growth and to apply electrical stimuli to affect cell growth and proliferation [102–104]. In addition, the use of rigid nanoparticles provides nano-topographic features to the otherwise soft and flat hydrogel’s surface and imparts stiffening and strengthening effects to the hydrogel matrix.
In the following paragraphs, we highlight a variety of inorganic rigid materials which are commonly applied in TE and cell culture applications focusing on these inorganic systems that have been considered as fillers in hydrogels.
Calcium phosphates (CaP)
Bone itself is an organic/inorganic composite material consisting of mainly collagen and calcium phosphate crystals [105]. Ca10(PO4)6(OH)2, hydroxyapatite (HAp), is the major component of the bone inorganic phase [106]. Thus, it is not surprising that hydroxyapatite and related calcium phosphates like tricalcium phosphate (α-TCP and β-TCP) and biphasic calcium phosphates (BCPs) are permanently being investigated in bone TE [107]. Calcium phosphates are characterized by a high degree of biocompatibility, they are osteoconductive, and are able to bind directly to bone [108]. Depending on their composition and crystallinity, CaPs can be degradable or nondegradable in the body. Degradability, mineralization, and biological properties can be tuned by doping with trace elements (K, Na, Mg, Zn, Sr, Se) which results in calcium phosphates with a composition closer to natural bone apatites [109–111].
Bioactive glasses/ceramics (BG)
Bioactive glass, first discovered by Hench et al. in the late 1970, displays an extraordinary bonding capacity to living tissue [112]. The release of ionic dissolution products from BGs results in a highly active interface leading to the formation of a carbonated hydroxyapatite (HCA) surface layer when immersed in biological fluids [6]. Bioactive glasses and ceramics can be divided into three categories depending on their interaction with biological environment: Class A biomaterials are osteoproductive and osteoconductive [6]. They show a rapid surface reaction and ion dissolution causing intra- and extracellular response. Class B bioactive materials show solely osteoconductivity due to their slow surface reaction and minimal ion release. Thus, only extracellular responses result. Class C bioactive materials are resorbed with 10–30 days due to their high reactivity [112, 113]. The reactivity is highly dependent on the material’s composition. A detailed description of the compositions and properties of bioactive glasses can be found elsewhere [112–114]. Although the exact reasons and mechanisms are still being investigated, it has been proven that the ionic dissolution products of bioactive glasses stimulate cellular behavior inducing in some cases also an angiogenic effect [101, 115–117]. It has to be noted that these effects are not always positive but can also result in harmful pH changes or the release of cytotoxic ions or intolerable ion concentrations [101, 118]. More recently, nanosized bioactive glasses have become available and are now being intensively investigated [119–122]. Due to their high surface area, surface effects and ion dissolution are more pronounced compared to bulk systems. In addition, they can be dispersed in polymeric materials at the nanoscale, an essential advantage for the fabrication of composite materials, which has opened also applications in soft TE [123]. To this group not only silicate but also phosphate and borate glasses belong, which are of relevance for applications in TE [118, 124, 125]. Also mesoporous glasses, e.g., BG (nano)particles containing ordered, nanoscale porosity are becoming highly prominent and the focus of extensive research [126–129]. Furthermore, ion-doped bioactive glasses are continuously gaining attention, especially with regard to bactericidal materials [101, 130, 131].
Clays
Although clay is mostly known for its application as building material, its medical use goes back to prehistoric and ancient times when it was used as wound dressing or as a treatment for stomach ache [132]. Today, it is mainly used as antacids and antidiarrhoeics or in cosmetic formulations [133]. The medical effectiveness of clay minerals results from its structure. Clay minerals are typically micro- or nanosized particles consisting of layered 2D silicate sheets [133]. Due to their large surface area, clay particles show a distinct adsorptive behavior. Protons, peptides, and polymeric materials like proteins or other biomolecules can be adsorbed onto the minerals surface. Thus, toxins can effectively be eliminated by clay administration. The adsorption capacity of clay minerals can also be used as delivery systems or as physical crosslinking points of polymeric materials resulting in hydrogels with extraordinary gelation behavior and mechanical strength [133–135]. The toxicological effects of clay minerals have been investigated by several groups. The results indicate that high clay concentrations reduce cell proliferation in vitro [136, 137]. However, most in vivo studies do confirm these findings. Indeed, the extent and origins of the potential toxicological effects of clays need to be further and more systematically investigated.
Carbonaceous materials
Carbon nanotubes (CNTs) are rolled sheets of graphene which can either be single-walled (SWCNTs) or multiwalled CNTs (MWCNTs) and are generally characterized by their high aspect ratio (>0.7). Their special physical and electrical properties as well as their ability to pack and align into highly ordered structures have motivated numerous groups to investigate their applicability as biomaterials in TE applications [138, 139]. Especially interesting with respect to TE is the induction of cellular organization based on either electrical stimulation or solely directed cellular growth on highly ordered CNT substrates. Furthermore, CNTs can be used as vehicles for the delivery of drugs, growth factors, bioactive agents, or genetic material [138]. Their nondegradable nature and low solubility are the major drawbacks, but the latter can be overcome by chemical functionalization [139].
Graphene oxide (GO) is obtained by oxidation of graphite and can be dispersed in aqueous media in the form of thin platelets [140]. The presence of oxygen-containing groups reduces the irreversible aggregation behavior known from graphite sheets allowing for the preparation of homogenous aqueous dispersions [141]. Nevertheless, the dispersion of GO sheets in biological media often requires stabilization with surfactants or ultrasound treatment to prevent agglomeration [141]. The presence of reactive oxygen groups allows for the chemical modification of GO as well as noncovalent interactions with polymers and proteins through van-der-Waals interactions or hydrogen bonding offering an excellent basis for the preparation of polymeric composite materials [142].
Superparamagnetic iron oxide nanoparticles (SPIONs)
Superparamagnetic iron oxide nanoparticles (SPIONs) are well known for their excellent magnetic properties enabling their convenient use in targeted drug delivery [143]. Their small size facilitates their incorporation into almost all matrices including uptake into cells and bacteria [144]. Depending on the preparation method, SPIONs carry a certain surface modification which can typically be used to introduce further functionalities [145, 146]. SPIONs can be dissipated through the natural human metabolic iron pathway [147]. Particle aggregation and oxidation, which result in the diminishment or loss of the magnetic properties, are common complications [144].
Cerium oxide nanoparticles (CONPs)
CONPs are known for a high capability to switch reversibly between oxidative states [148]. This redox property enables CONPs to efficiently scavenge free radicals making it an excellent antioxidant agent. Since medical implants are particularly susceptible to oxidative damage caused by inflammation-related oxidative stress, CONPs are being investigated concerning their pharmaceutical potential [149, 150]. Unfortunately, cytotoxic effects have been reported, being caused by cellular internalization and accumulation of free particles which disturb intracellular free radical signaling pathways [151, 152].
Others
Indeed, other kinds of inorganic materials have also been investigated and used in combination with polymers in composite scaffolds including Au, Ag, Al, Si, Mg, TiO2, ZrO2, CS, graphite, and carbonated fluorapatite [5, 43, 153–163]. Salts such as CaCO3 and polyphosphates have been also considered in combination with polymers as well as NaCl crystals which have been used to improve the pore interconnectivity of polymeric scaffolds [164–166]. In this review, only those that have been considered in combination with hydrogel-based composites for cell encapsulation, biofabrication, and injectable systems are further discussed.
Challenges of inorganic fillers
Due to their chemical resemblance to the inorganic components of bone, calcium phosphates are able to directly bind to bone making them excellent candidates for bone TE [101, 167]. Similar high bioreactivity and affinity to bone tissue are provided by bioactive glasses [112, 113]. However, these materials are usually brittle making them hard to handle and unsuitable for many load-bearing applications. Further difficulties in the use of purely inorganic materials, in particular highly biodegradable systems, are caused by the ionic dissolution. Although under given conditions, dissolution products are able to stimulate cell metabolism and differentiation, in some cases, dissolution of inorganic ceramics and glasses may be accompanied by the release of basic components which show harmful effects on neighboring cells [114, 168]. Higher mechanical resistance and flexibility as well as the stabilization of the pH value during the dissolution processes can often be achieved by the combination of inorganic fillers with polymeric carriers as will be discussed in the following sections [6, 169].
Focusing on the inorganic materials that have been used in combination with hydrogels, Table 3 summarizes their relevant properties.
Hydrogel–inorganic phase composites
Interactions between hydrogel networks and inorganic additives
The idea behind the formation of inorganic/organic composites is the design of materials with superior mechanical and biological properties. As in all composite systems, in the ideal case, the disadvantages of both materials are counterbalanced and thus eliminated by synergetic effects. The preparation of inorganic/organic composite materials can be performed by various methods from simple mixing of the two components to the in situ mineralization of polymeric scaffolds [170]. The in situ mineralization of polymers has been recently comprehensively reviewed by Kretlow et al. [20] and will thus not be included in this review. Another possibility is the initiation of the polymerization/gelation of the hydrogel from the surface of micro- or nanoparticles, which typically results in extremely tough and resistant hydrogel networks [171–174]. Furthermore, many of these systems have been reported to show stimulus-responsive and self-healing properties [173, 174]. So far, this technique has mainly be used to generate organic/organic composites based on polymeric networks crosslinked via polymeric microgels, micelles, clusters, or macromolecular microspheres but is generally also applicable to inorganic/organic composite materials [171–174]. Here, we focus on the approach of mixing the two phases to form the composite, namely, a hydrogel matrix and the inorganic filler. In order to understand the effects arising from the addition of inorganic fillers to a hydrogel, the structural properties of hydrogel networks need to be considered as well as the interactions at the interphase [18, 19, 175]. As described above, hydrogels are three-dimensional networks of crosslinked polymeric chains. These networks can be separated into chemically and physically crosslinked materials. While chemical crosslinking is based on covalent bonds between the polymeric chains and/or their side groups, physical crosslinking results from noncovalent interactions. These interactions can be found between the polymeric chains, polymer chains and ions (which is commonly described as ionic crosslinking) or between a polymer and the surface of the inorganic filler.
The addition of inorganic materials to a polymer solution can result in different interactions between the two materials, as schematically illustrated in Fig. 2, which generates different conditions at the interfaces leading to new structural properties. In the easiest case, a simple mixture of the two components is obtained. The inorganic particles are dispersed in the polymeric matrix, but there are no specific interactions between the two materials. Another possibility is the formation of specific physical interactions chemical bonding between the polymeric chains and the inorganic material, as described above. This effect results in an enhancement of the crosslinking density and thus, in the increased strength and mechanical stability of the polymeric network. However, the adsorption of the polymer on the surface of the inorganic additive can also result in the disturbance of the polymeric network structure (especially in absence of chemical bonds) and thus in weakening of the mechanical strength of the hydrogel. The discussed classes of interactions occurring between hydrogels and inorganic additives are schematically illustrated in Fig. 2.
Properties
By combining the advantages of hydrogels and inorganic fillers, synergetic effects are generated which, in the ideal case, are able to counteract individual materials’ disadvantages. More specifically, the combination of hydrogels with inorganic fillers should result in highly biocompatible materials which can meet the mechanical requirements of the implanted site, stimulate the desired cellular behavior, and exhibit well-defined degradation profiles.
Clearly, two families of composites can be developed; those incorporating degradable fillers such as BGs and those including persistent fillers such as carbon nanotubes. In fully biodegradable hydrogel/inorganic filler composites, there is an important synergetic effect between the degradation of hydrogel matrix and the dissolution of inorganic compounds, like bioactive glasses and calcium phosphate. While the degradation of synthetic polymers like polyethers and polyester is typically accompanied by acidic byproducts which often cause a significant inflammatory response [98, 99], bioactive glasses release noteworthy basic dissolution products [176–178]. By combining polymeric scaffolds with inorganic moieties, neutral and consequently less harmful conditions can be achieved during the decomposition of the composite [19]. In addition, the incorporation of inorganic fillers alters the hydrophilicity and thus the water adsorption of the polymeric matrix. The generation of new interfaces and interfacial regions can allow water to penetrate more easily, altering the degradation behavior of the polymeric matrix and leading to a more homogenous degradation of the polymer [179]. In general, it is important that the degradations of the inorganic and organic materials are matched. A simultaneous degradation of both materials is required to maintain the structural and mechanical integrities of the system during degradation and to gain the greatest benefits from synergetic effects: As is well known, in TE approaches, cells should be able to populate, grow, and proliferate within the system, to synthesize their own extracellular matrix, while the scaffold is gradually disintegrating giving space for the newly formed tissue [6].
When a material is implanted into the body, it is rapidly coated with blood components. Many of these components are proteins, like fibronectin and vitronectin, which are typically found in the extracellular matrix [100]. One common characteristic of several of these proteins is the RGD-motif which is known to contribute to cellular adhesion via integrin receptors present on the surface of most cells [180]. Hydroxyapatite, bioactive glasses, and other ceramic materials, especially the nanosized particles, are known to be specifically prone to protein adsorption [100, 181]. This characteristic of inorganic particles is particularly useful in the design of organic–inorganic composite materials. The adsorption of proteins on the inorganic particles inside the composite material provides the vital basis for cellular attachment to many composites in which the organic material often lacks the mandatory cell-binding sites [182]. Therefore, the careful choice of the composite’s components can circumvent the need for chemical modification of the polymeric matrix. Although the complex process of protein adsorption is not yet fully understood, it is commonly agreed that this process is one of the most decisive factors for the cellular and immunologic response to medical implants and drug delivery vehicles [183–185]. Thus, while designing proper combinations of hydrogels and inorganic fillers, one should consider predominantly the protein adsorption at the interface.
Another important reason for the need of composite materials lies in the enhancement of the mechanical properties of hydrogel matrices [23]. TE requires specific mechanical properties, e.g., stiffness and mechanical strength, especially in load-bearing applications. The incorporation of inorganic nanoparticles into hydrogels should lead to superior mechanical strength and stiffness by keeping the high flexibility of the polymeric matrix [186]. Consequently, in well-designed hydrogel composites, mechanical properties, and the previously discussed advantages of inorganic particles like protein adsorption, bioactivity, and tailored degradation can synergetically be combined.
The alteration of the mechanical properties is not only beneficial for in vivo applications but also for the processability of the particular scaffold material. 3D printing and bioplotting as well as many cell encapsulation techniques require specific physical material’s properties like viscosity, flow characteristics and stiffness [187–189]. Thus, incorporating inorganic particles into hydrogels can also be beneficial for facilitating processibility into 3D structures using techniques as varied as bioprinting, electrospinning, and freeze-drying by inducing changes in the hydrogel’s viscosity or flow characteristics.
Applications of hydrogel composites
Conventional cell culture procedures are based on the adherence of cells to the surface of a substrate [14]. The substrate itself can exhibit a three-dimensional architecture. Nevertheless, cells are typically seeded on top of the structure. However, it is well known that in the real in vivo situation cell–cell and cell–matrix interactions occur in three dimensions [2, 190]. In order to construct functional biological units to form tissues and organs, it is therefore of predominant importance to focus on the embedding of cells into 3D (porous) substrates [190, 191]. The natural cellular environment in vivo, the extracellular matrix (ECM), is a three-dimensional fibrous network embedded in a highly hydrated gel-like matrix [192]. The matrix does not only offer a 3D scaffold for the cells to grow in but also mechanical stability, sufficient space to enable the transport of metabolites and nutrients, cell transport, and vascularization as well as biophysical and biochemical clues [192]. The ECM is a dynamic network which can adapt to environmental conditions like compression and shear stress and guide cellular organization and behavior [193, 194]. Given the complexity of the functions of the ECM, it is easy to understand that the material requirements for man-made scaffolds cannot be met by one single material but by the smart choice and combination of various materials. Of particular challenge is the development of hydrogels and their composites for biofabrication strategies [17].
Here, we summarize three main approaches focusing on the generation of 3D scaffolds based on hydrogel–inorganic filler composites, namely: scaffold structures obtained by novel additive manufacturing methods, more general techniques for the encapsulation of living cells and the well-investigated area of injectable materials. These three areas, although exhibiting some different characteristics and material requirements, can be unified by their purpose of generating 3D scaffolds supporting cellular growth and organization and represent important fields for applications of hydrogel–inorganic phase composites.
Cell encapsulation
The encapsulation of cells into 3D structures for TE is a relatively new research area. In this approach, the 3D hydrogel type matrices act as microenvironments for the encapsulated cells. Physical and chemical clues can be specifically altered to stimulate the anticipated cellular reaction, and these extracellular matrix analogues are usually applied for the investigation of fundamental cellular behavior in a 3D environment. In addition, the encapsulation of cells into small, micro-sized hydrogel compartments allows the independent manipulation or delivery of individual cells [195, 196]. Using high-throughput techniques like microfluidics, these independent units can be used in drug testing and development or as building blocks for the bottom-up generation of larger cellular superstructures [197]. There is also increasing effort in considering cell encapsulating 3D hydrogels as tissue models to investigate tumor development in advanced cancer research [198–206].
In the following sections, we discuss different composite materials used for cell encapsulation with applications in bone ("Examples of cell-containing hydrogel composites for bone tissue engineering" section) and cartilage ("Examples of cell-containing hydrogel composites for cartilage tissue engineering" section) TE, dentistry ("Examples of cell-containing hydrogel composites for applications in dentistry" section) as well as materials used for the generation of cardiac patches ("Examples of cell-containing hydrogel composites for the design of cardiac patches" section) and cell delivery/protection systems ("Examples of cell-containing hydrogel composites for cell/drug delivery" section).
Composites for cell encapsulation
Examples of cell-containing hydrogel composites for bone tissue engineering
PEG is a commonly used material in various biomedical, TE, and drug delivery applications. Despite being available over a broad range of molecular weights and thus mechanical stabilities, a further enhancement of the network is often necessary. In addition, PEG lacks the binding sites mandatory for cellular adhesion. Clay minerals are receiving increasing attention as mechanical reinforcement additive for hydrogel matrices. The high surface area of clay minerals enables physical interactions between the particles surface and polymeric materials. Thus, chemically crosslinked gels can be reinforced by the introduction of additional physical crosslinking points. Improved mechanical performance including enhanced compressive and elastic properties was reported for PEG diacrylate (PEGDA)/clay (more specifically Laponite particles) composites [207]. Cell-containing PEGDA/clay composites have been synthesized by simple mixing of all components and subsequent photo-crosslinking of the PEG chains via reaction between the diacrylate units of neighboring chains. Physical crosslink formation between PEG and the clay particles as well as energy dissipation effects were shown to lead to the described mechanical reinforcement. The swelling behavior of the resulting composite strongly depended on the amount of clay mineral added. Low clay concentrations caused an increased swelling behavior due to an osmotic pressure induced water influx. High concentrations showed a contrary swelling behavior. The water uptake of composites containing high amounts of clay can probably be attributed to the higher density of physical crosslinking points. The composite exhibited adhesive behavior of encapsulated human bone marrow derived mesenchymal stem cells (hMSCs) which was also dependent on the content of clay particles. Since PEG does not offer any binding sites for cellular attachment, the adherence and spreading of encapsulated cells must depend on the protein adsorption ability of clay mineral particles. This assumption was supported by an increase in cellular attachment with increasing clay content.
Enhanced gel mechanics and osteogenic differentiation have also been reported for calcium phosphate reinforced oligo(poly(ethylene glycol) fumarate (OPF) [208]. In this case, cell-binding sites (RGD-units) were incorporated into the polymeric network and compared to unfunctionalized OPF, OPF/calcium phosphate and OPF-RGD/calcium phosphate composites. The incorporation of RGD into the polymeric matrix enhanced the spreading and viability of the encapsulated cells. However, the cells were unable to proliferate in both, RGD-modified and RGD-free OPF hydrogels. Calcium phosphate addition enhanced the cell-mediated mineralization of the scaffold which is an indication of osteogenic differentiation. However, in contrast to the study of Chang et al. [207] the adhesion of the encapsulated cells to the scaffold could not be enhanced by addition of an inorganic filler. It was hypothesized that the embedding of the particles into the hydrogel matrix hinders cell migration, adhesion, and spreading. Only the combined effects of RGD and calcium phosphate resulted in the increases of cell viability and mineralized matrix production.
The stimulation of osteogenic differentiation was also found by Patel et al. [209] in cyclic acetal hydrogels based on poly(ethylene glycol) diacrylate (PEGDA) and 5-ethyl-5-(hydroxymethyl)-b, b-dimethyl-1,3-dioxane-2-ethanol diacrylate (EHD) reinforced by hydroxyapatite (HAp) nanoparticles. Upregulation of morphogenetic protein-2 (BMP-2), alkaline phosphatase (ALP) and osteocalcin (OC) expression of encapsulated bone marrow stromal cells (BMSCs) was found. The effect was attributed to either osteogenic effects of HAp particles or the enhanced adsorption of proteins and osteoblast growth factors on the HAp particles.
Another example for the stimulation of osteogenic differentiation using hydrogel/inorganic phase composites was presented by investigating 45S5 bioactive glass reinforced alginate [210]. The enhanced proliferation, and differentiation of MC3T3-E1 and rBMSCs encapsulated into millimeter-sized composite beads was explained by stimulating effects of ions, especially silicon ions, released during bioactive glass dissolution. Consequently, the incorporation of bioactive glass into cell-containing alginate beads can improve the efficiency of bone formation in a relatively cost effective and easy way without the need for expensive proteins or growth factors, thus, increasing the performance of this cell delivery system in bone regeneration applications.
Using a photocrosslinkable gelatin methacrylate (GelMA) hydrogel, Sadat-Shojai et al. [211] demonstrated that the compressive modulus of the polymeric matrix can be significantly enhanced by the addition of hydroxyapatite (HAp) nanoparticles. The particles could be homogenously dispersed within the hydrogel network and no influence of the inorganic filler on the hydrogels swelling ratio was observed. With increasing HAp concentration, an increase of the compressive modulus was detected. However, particle concentrations above 2.5 mg/mL did not result in any further mechanical reinforcement. It has to be noted that HAp particles are opaque and thus, their presence might interfere with the photo-induced crosslinking process of gelatin methacrylate at high particle concentrations. The encapsulation of preosteoblastic MC3T3-E1 cells resulted in good cell viabilities, growth, cell adhesion, and spreading for all investigated system with a slight decrease in cell spreading and metabolic activity with increasing filler concentrations. This effect can be explained as a result of the higher mechanical strength of the composite materials compared to pure gelatin hydrogels.
An example of CNT-reinforced hydrogels was presented by Wheeler et al. [212]. They used an elastin-like polypeptide (ELP)–collagen composite as polymeric matrix and investigated the effect of carbon nanosphere chains (average diameter 20–40 nm) and bioactive glass (45S5, average particle diameter: 200–350 µm) incorporation. In both cases, they observed an increase in Young’s modulus and tensile strength. Simultaneous encapsulation of MC3T3-E1 mouse pre-osteoblastic cells revealed high cell viabilities, cell attachment and proliferation for the investigated systems as well as the control of pure ELP–collagen hydrogels. A slight increase in the osteoblastic differentiation was observed in case of bioactive glass addition which was explained by the stimulating effect of the higher mechanical strength of the cellular environment.
Examples of cell-containing hydrogel composites for cartilage tissue engineering
An agarose-based composite material was investigated by Khanarian et al. [213] who studied the influence of hydroxyapatite (HAp) particles on calcified cartilage formation. In the first objective of the study, the behavior of chondrocytes from the native osteochondral interface (hypertrophic chondrocytes) and deep zone chondrocytes in HAp-free and HAp-containing scaffolds was compared. It was found that the presence of HAp particles had little effect on the matrix deposition and hypertrophy of deep zone chondrocytes while hypertrophic chondrocytes showed a significant increase in matrix deposition and mineralization. The enhanced mineralization behavior of hypertrophic chondrocytes is probably a result of the release of calcium and phosphate ions by the inorganic filler which are known to up-regulate chondrocyte mineralization [214, 215]. The authors note that in contrast to agarose/HAp composites where no stimulation of deep zone chondrocytes was observed, enhanced hypertrophy and matrix deposition of deep zone chondrocytes could be induced in alginate/HAp composites [216]. It is hypothesized that higher calcium concentrations in the ionically crosslinked alginate systems stimulates chondrocyte maturation resulting in hypertrophy and elevated matrix synthesis of deep zone chondrocytes. Consequently, it becomes obvious that besides the identification of suitable hydrogel and inorganic filler combinations, an adequate choice of the cellular component is of great importance in order to control and stimulate the anticipated cellular behavior. In the second objective, the authors optimized the dose and size (micro- vs. nanoparticles) of the inorganic fillers to promote hypertrophy and calcified matrix deposition of both cell types. No influence of the particle size on the hypertrophy was observed, while cell-laden agarose gels containing micron-sized HAp particles showed an enhanced matrix deposition compared to cells encapsulated in the presence of HAp nanoparticles. This effect can probably be explained by the improved cell–ceramic interactions in case of micron-sized particles compared to nano-scale systems. Matrix deposition increased with increasing ceramics content up to 3 %. Higher HAp concentrations of 6 % led to a decrease in matrix deposition which might be a result of the limited space available for extensive matrix elaboration. Matrix deposition, alkaline phosphatase activity (ALP), compressive strength and shear moduli were highest for systems containing 3 % of micron-sized HAp particles which most closely approximates the mineral nature (content and size) of native tissue [217, 218]. Furthermore, the authors suggest that synergetic effects among mechanical reinforcement, ion release, matrix deposition, and hypertrophy result in significant structure–function correlation of the cell-laden hydrogel/HAp scaffold [215].
Examples of cell-containing hydrogel composites for applications in dentistry
In a recent publication, Chatzistavrou et al. [219] presented the use of collagen/fibrin microbeads as a delivery system for Ag-doped bioactive glasses and dental pulp stem cells (DPSCs) in dental applications. They compared pure collagen/fibrin microbeads with DPSC-containing collagen/fibrin beads and beads containing DPSCs in addition to silver-doped bioactive glass (Ag-BG). They found that both, cells and bioactive glass, enhance the degradation process of the microbeads. Microbeads containing cells and bioactive glass showed the strongest effect on the degradation behavior. In in vitro experiments, no odontoblastic differentiation was observed inside DPSC- and Ag-BG-containing beads during culture. However, the same system showed odontoblast-like cells in in vivo experiments in nude mice. However, the control group of nonencapsulated DPSCs showed no differentiation when implanted into the tooth slides. Thus, the differentiation of DPSCs seems to be induced by collagen/fibrin beads and/or Ag-BG. The authors suggest that the ionic degradation product of Ag-BG improves the differentiation of DPSCs inside the Ag-BG-containing beads. However, the differentiation behavior of cells encapsulated into pure collagen/fibrin microbeads was not investigated, and therefore the effect of Ag-BG particles on the differentiation behavior of the encapsulated cells can only be hypothesized. Nevertheless, the authors could show that Ag-BG increases the antibacterial activity of the system. A slight decrease in the bactericidal activity of Ag-BG was observed in case of the co-encapsulation of DPSCs which might be a result of cell-material interactions or lower amounts of Ag-BG particles being encapsulated in this case. This study clearly indicates the ability to encapsulate antibacterial ion-releasing bioactive glass particles in biodegradable hydrogels, which offer an innovative alternative to couple osteogenic materials with antibacterial agents.
Examples of cell-containing hydrogel composites for the design of cardiac patches
Shin et al. published several studies focusing on gelatin-based composites for cell encapsulation [220, 221]. In analogy to the results obtained by Sadat-Shojai et al. [211], the compressive modulus of UV-crosslinkable gelatin methacrylate (GelMA) hydrogels could be enhanced by the addition of an inorganic rigid filler, in this case GO [220]. The strong noncovalent interactions between the gelatin chains and the GO particles also influenced the degradation behavior of the polymer. Pure GelMA hydrogels maintained its ordered structure after collagenase-mediated degradation. Degradation mainly resulted in an increased pore size. In contrast, GelMA/GO composites showed a collapsed, disordered morphology after degradation. In addition, an increase in metabolic activity of encapsulated NIH-3T3 cells was observed. This effect could be explained by an enhancement of cell adhesion in GO-containing hydrogels compared to pristine hydrogels.
The same group also reported the mechanical reinforcement of GelMA gels with carbon nanotubes (CNTs) [221]. Enhanced tensile strength and elastic modulus were observed. Encapsulated NIH-3T3 cells and human mesenchymal stem cells (hMSCs) showed increased spreading and proliferation inside the composite material compared to pure GelMA hydrogels with similar stiffness. The deterred cellular growth and spreading in pristine highly concentrated hydrogels was attributed to the high density and low porosity of the material. CNT-reinforced hydrogels with the same stiffness exhibited a less dense (more porous) structure allowing for cellular growth and spreading. The incorporated CNTs also enhanced the polymers’ resistance to degradation by hindering the influx of water and thus the permeation of collagenase into the hydrogel. Furthermore, the cell viability was found to be inversely proportional to longer exposure times in CNT-containing hydrogels. This effect was explained by the ability of CNTs to scavenge harmful radical oxygenated species released during carbon–carbon double-bond formation in the crosslinking reaction of methacrylate groups.
In a related study by the same authors, it was reported that the mechanical properties are highly dependent on the amount of CNTs being incorporated into the hydrogel system [222]. An increase in the compressive modulus was observed for CNT concentrations up to 3 mg/mL. Higher CNTs contents weakened the polymeric network. This phenomenon is probably a result of the high UV-absorption of CNTs which impedes the UV-induced gelation of GelMA as has been discussed above for the addition of HAp particles to GelMA hydrogels. Furthermore, an increase in cell adhesion, viability, and alignment with the increasing CNTs content was observed (Fig. 3). Cell proliferation was not influenced by the CNTs incorporation as shown by the unaltered DNA content in Fig. 3d. The authors argue that enhanced cell adhesion and stretching forces resulting from interactions between the cells and the CNT network cause the increased cellular alignment, as schematically illustrated in Fig. 3g.
Effects of CNT incorporation into GelMA hydrogels on cardiac cells. a Cell retention and distribution are significantly improved on CNT–GelMA composites compared to pristine GelMA hydrogels. Cell retention (b), viability (c), DNA content (d) and alignment (e, f) are highly dependent on the amount of CNTs incorporated. Highly aligned cells are observed on CNT–GelMA composites. No significant effects were found on the DNA content after 3 and 6 days. g Schematic illustration of stretching forces resulting from cell–CNT interactions. Reprinted from Ref. [222] with permission. Copyright 2013 ACS Publications
This series of studies thus report the convenient combination of hydrogels with carbonaceous nano-materials, and further investigations are expected in this field.
Examples of cell-containing hydrogel composites for cell/drug delivery
A recent publication by Weaver et al. [223] discusses the use of cerium oxide nanoparticles as antioxidant fillers in alginate hydrogels. Cerium oxide nanoparticles (CONPs) effectively scavenge ambient-free radicals making it a promising candidate as antioxidant protection material. However, phagocytosis of CONPs by beta cells showed significant cytotoxic effects even at low concentrations, thus limiting the applicability of CONPs as antioxidant in cell culture and biomedical applications. As the authors could show, this cytotoxic effect can be eliminated by embedding cells and CONPs into a hydrogel matrix. The mesh size of the investigated alginate hydrogel impedes the diffusion of CONP particles and, thus, their phagocytosis by the co-encapsulated cells. In addition, it was shown that the CONP particles can effectively protect the encapsulated cells from free radical damage when exposed to superoxide radicals. Consequently, cytotoxic effects can be eliminated up to high concentrations, while the catalytic activity of the CONPs particles is maintained. Furthermore, stable encapsulation and reactivity of the particles could be demonstrated up to 1 year after encapsulation. The authors compared the alginate/CONP system to CONP-containing agarose gels which, by contrast, did not show the anticipated long-term stability. It was postulated that specific interactions between the COO− terminals of the alginate chains bind the particles, leading to a stable physical entrapment and long-term stability. Since agarose does not contain any carboxyl groups, the interactions between polymer and CONPs are less significant.
Another alginate-based system for cell and drug delivery applications was investigated by Ciriza et al. [224]. In this case, alginate composite microcapsules containing different concentrations of GO were produced via extrusion through a disposable nebulizer and subsequent gelation in the presence of bivalent calcium ions. Murine C2C12 myoblasts which were genetically engineered to secrete murine erythropoietin (EPO) could simultaneously be encapsulated with high cell viability. GO concentrations between 25 and 50 µg/mL resulted in enhanced viability, metabolic activity, and membrane integrity of the encapsulated cells while concentration of 100 µg/mL seemed to decrease cell viability and metabolic activity. Most interestingly, it was shown that the presence of GO particles significantly decreased the amount of EPO released from the microcapsules thus diminishing the efficiency of the presented drug delivery system. A control experiment in which the adsorption of EPO on pristine GO particles was evaluated indicated that approximately 10 % of the present protein was adsorbed by the particles which explains the observed decrease in the amount of EPO released from GO-containing alginate microcapsules. The adsorption of EPO could be significantly reduced by preconditioning GO with fetal bovine serum (FBS) which introduced a protective protein coating to the GO nanosheets thus making the surface unavailable for the adsorption of EPO to the particles surface.
Given the high number of hydrogel composite systems for cell encapsulation, which have been discussed in detail in this section, a comprehensive summary is given in Table 4, in which, in addition to the materials employed, the key results and applications are collected.
Bioprinting
Three-dimensional constructs can be manufactured via layer-by-layer deposition of a polymeric precursor which is subsequently crosslinked for permanent preservation of the structural integrity of the generated geometry [197]. This technique enables the highly controlled production of scaffold materials for TE. Pore size, overall porosity, and scaffold dimensions can be precisely controlled [225]. Regarding TE applications this is a crucial step toward personalized implants. Additive manufacturing techniques also allow the fabrication of very accurate architectures consisting of different materials. Furthermore, the respective placement of different cell types within a scaffold can be readily controlled with excellent precision [14, 226, 227]. Thus, complex geometries like the ones found in tissues and organs can be replicated and incorporated with cells or growth factors with high level of accuracy.
Naturally derived materials like alginate-based hydrogels are popular ink materials for bioprinting applications. Alginate offers excellent biocompatibility, with its high viscosity allowing the printing of stable 3D structures and mild and rapid gelation process due to ionic crosslink formation with bivalent ions. Furthermore, alginate can be processed under physiological conditions [48, 228]. Although extraordinarily tough alginate-based hydrogels—which offer outstanding durability and are excellent candidates for soft TE, cell encapsulation, and extracellular matrix mimics—have been reported [229], pure hydrogels do not usually offer the required tensile strength and fracture toughness mandatory for load-bearing applications like bone TE [6, 26, 32]. Synthetic hydrogels such as poly(ethylene glycol) (PEG) offer higher mechanical strength but often lack the required biocompatibility or cell-interactive properties [26].
By incorporating inorganic fillers into 3D natural or synthetic hydrogel scaffolds, several groups have tried to impart strength and to enhance bio-instructive properties like cell adhesion or bioactivity while maintaining the characteristic properties of polymeric systems like flexibility and deformability, which will be described in the following sections [23]. It has to be stated that the incorporation of inorganic fillers into hydrogel networks significantly alters the properties of the final printed scaffolds but does not necessarily enhance the pre-gel material’s properties. The addition of inorganic particles to the printing solution can result in an increase in the pre-gel material’s viscosity which can be beneficial for the manufacturing process. However, as it will be discussed below, this viscosity increase can also be disadvantageous. High viscosities can complicate the printing process thus limiting the applicable content of inorganic material in the composite [230]. Furthermore, printing of dispersed particle systems can cause clogging issues of the printing nozzle due to unsuitable particles dimensions or their aggregation [231]. Consequently, the amount, size and aggregation behavior of the inorganic particles needs to be considered and must be compatible with the bioprinting setup.
In the following section, we will first discuss bioprinted hydrogel composites for bone TE ("Examples of bioprinted hydrogel composites in bone tissue engineering" section). In the second part, examples of bioprinted hydrogels for bone and chondral TE will be reviewed ("Examples of bioprinted hydrogel composites in bone and chondral tissue engineering" section) before debating bioprinted materials for applications in general hard and soft TE approaches ("Examples of bioprinted hydrogel composites in hard and soft tissue engineering" section).
Composites for bioprinting
Examples of bioprinted hydrogel composites in bone tissue engineering
Luo et al. incorporated mesoporous bioactive glass (MBG) into alginate scaffolds aiming to enhance the mechanical strength, induce bioactivity, and improve alginate’s drug delivery capacity for bone TE applications [228]. The composite was prepared by homogenous mixing of alginate and 40 µm mesoporous bioactive glass particles. The scaffolds were printed and subsequently crosslinked using a CaCl2 solution. The scaffolds were characterized with respect to their mechanical strength, degradation, biological and drug delivery properties. The introduction of MBG to the alginate scaffolds resulted in a decreased porosity, enhanced compressive strength and modulus compared to scaffolds consisting of pure alginate. Furthermore, the scaffolds exhibited an enhanced pH stability and attachment of human bone marrow-derived mesenchymal stem cells (hBMSC). The authors hypothesize that the ion release from MBG stabilizes the pH of the surrounding solution and might stimulate the proliferation and attachment of cells due to the release of Si ions. The increased surface area and roughness resulting from the incorporation of MBG particles are being considered as alternative explanation for the enhancement of cellular attachment. In order to investigate the drug delivery capacity of the composite, Dextran was incorporated as a model drug. While pure alginate scaffolds showed a burst release within 0–120 h, alginate/MBG scaffolds released dextran in a much slower and more sustained manner. The authors suggest that the formation of an apatite layer on the surface of the scaffolds hinders the release of the model drug resulting in a slower and more controlled release profile.
Wang et al. [232] investigated the effect of bioactive glass addition on the mineralization behavior of bone-related SaOS-2 cells incorporated in alginate/gelatin scaffolds. Cell-containing alginate/gelatin scaffolds were printed and subsequently supplemented with 55 nm bioactive glass particles. Although no significant effect on the proliferation was observed, the mineralization of the SaOS-2 cells was enhanced by bioactive glass addition.
As discussed above, alginate lacks the necessary integrin-binding sites to support cellular attachment which can be overcome by chemical modification or composite formation. Lee et al. [233] investigated a composite consisting of alginate and collagen mixed with silica particles. The alginate–collagen composite showed enhanced mechanical properties compared to the pure components. Silicated alginate/collagen scaffolds were prepared from the mixed solutions and subsequently dip coated with a silica solution. The coated scaffolds showed improved resistance to degradation, increased compressive modulus, higher protein adsorption as well as increased proliferation and ALP activity of seeded mouse pre-osteoblast cells (MC3T3-E1) as shown in Fig. 4. All these characteristics are probably based on the Si-induced mineralization of the scaffold. The formation of an apatite layer on top of the structure impedes degradation. A synergetic effect of the apatite layer and released silica ions on the osteoblastic activity of the cells is a possible explanation for the observed enhanced ALP activity of the MC3T3-E1 cells [101, 233–236].
Surface and cross-sectional SEM images of alginate–collagen composites without (a) and with (b–d) incorporated silica particles after 21 days in cell culture. e The ALP activity of seeded pre-osteoblast cells shows a strong dependence on the amount of silica ions present in the scaffolds. Synergetic effects of resulting from the apatite layer formed on the silicated scaffolds surface, and the release of silica ions are a potential explanation for the enhanced ALP activity. Reprinted from Ref. [233] with permission of RSC Publishing
Examples of bioprinted hydrogel composites in bone and chondral tissue engineering
Luo and colleagues investigates the incorporation of calcium phosphate cement (CPC) into alginate scaffolds for applications in bone and chondral TE [237]. The composites were prepared by either mixing of CPC and alginate solutions or by multi-channel plotting of alternating alginate and CPC strands. The biphasic CPC/alginate scaffolds showed a denser structure and enhanced mechanical properties compared to pure alginate, pure CPC and mixed CPC/alginate scaffolds. The direct contact between the CPC particles in the biphasic scaffolds was considered to be the reason for a further enhancement of the mechanical properties, as compared to CPC particle embedded in an alginate matrix.
Another publication by the same group investigated gelatin/alginate composite scaffolds for bone and chondral TE [238]. Gelatin/alginate composite scaffolds with or without incorporation of micron-sized hydroxyapatite particles were generated by 3D bioplotting and analyzed with respect to mechanical properties, surface morphology, cell adhesion, and proliferation. In contrast to the alginate/gelatin systems discussed above, the authors used a dual crosslinking procedure: ionic crosslinking of alginate was induced by addition of CaCl2 to the fabricated scaffolds followed by the carbodiimide-mediated covalent crosslinking of the gelatin chains resulting in scaffolds with superior mechanical properties. The mechanical properties, compressive strength, and modulus, could be further increased by the addition of HAp particles. Furthermore, the incorporation of HAp particles resulted in an increase of the scaffold’s surface roughness as illustrated in Fig. 5. However, the inorganic particles had little effect on the attachment and growth of hBMSCs seeded on top of the scaffolds. By contrast, gelatin/alginate scaffolds without HAp showed better cellular attachment and growth than HAp-containing composites. Potentially negative effects of the enhanced surface roughness on cell migration as well as influences of the HAp particles’ negative charge on cell attachment and the reduced accessibility of cell-binding sites present in the gelatin chains in the presence of HAp particles are discussed as possible explanation. Nevertheless, a uniform distribution of viable cells is observed for all scaffolds. The authors emphasize the high porosity of the 3D plotted structures and suggest the generation of biphasic scaffolds consisting of a bone-like part formed by the gelatin/alginate/HAp composite and a chondral part by HAp-free gelatin/alginate.
Microscopic images of gelatin/alginate scaffolds without (a) and with (b) addition of hydroxyapatite microparticles. The addition of HAp particles results in a dramatic increase of the scaffolds’ surface roughness as can be seen from the SEM images (gelatin/alginate: c, d; gelatin/alginate/HAp: e, f). Reprinted from Ref. [238] with permission of RSC publishing
Examples of bioprinted hydrogel composites in hard and soft tissue engineering
Alginate/gelatin scaffolds combined with hydroxyapatite (HAp) particles were reported by Wüst et al. [230]. They observed a drastic increase in viscosity which made the composite difficult to print. The HAp content was therefore limited to 8 % which was not sufficient for a significant enhancement of the mechanical properties. However, an influence of the HAp content on the temperature-dependent gelation behavior of gelatin was observed. Gelation temperatures of the composites including HAp particles were higher than those of the pure hydrogel mixtures. Cells were successfully incorporated into the printing process and no reduction of cell viability after printing was observed.
Gao et al. [239] compared the biological effects of hydroxyapatite (HAp) and bioactive glass (BG) particles on bone marrow-derived hMSCs) in bioprinted poly(ethylene glycol)dimethacrylate (PEGDMA) composite scaffolds. In analogy to the results obtained by Patel et al. [209], Gao. et al. [239] observed high cell viability, increased ALP activity, and osteogenesis in the presence of HAp particles. By contrast, cells cultured in the presence of BG particles showed decreased cell viability and significantly slower osteogenetic differentiation than cells cultured in HAp-containing composites. By combining HAp and BG particles in one PEGDMA hydrogel composite an intermediate cellular response with values in between the ones determined for HAp/PEGDMA and BG/PEGDMA composites was observed. However, it has to be noted that in this study nano-sized HAp particles were compared to micron-sized BG particles. The determined effects could thus result from the different particle sizes and the accordingly higher surface reactivity of the nano-sized HAp particles compared to the larger BG microparticles. In addition, a decrease in the hydrogels compressive strength was found after addition of the inorganic fillers. This result conflicts with observations reported by Killion et al. [186] who found an increase in the compressive strength of PEGDMA hydrogels with increasing BG content using similar particle sizes and concentrations as reported by Gao et al. [239].
Table 5 summarizes the discussed composite systems and highlights the properties resulting from the incorporation of inorganic fillers into the hydrogel matrices. It is apparent that, in comparison to cell encapsulation strategies discussed above, the design of hydrogel–inorganic phase composites for bioprinting (biofabrication) methods for advanced scaffolding systems is much less developed. In most cases so far, bioactive glasses or CaP ceramics have been considered as fillers. Given the ability of bioactive glasses to release specific ions to activate specific cell responses, e.g., proliferation or collagen production, the field is currently going to expand to include applications beyond bone regeneration for example in the field of soft tissue regeneration or wound healing [123, 240].
Injectable materials
The significance of injectable materials for clinical use lies in the minimal invasive nature of their administration. The classical implantation of engineered tissues or fillers requires surgery which is accompanied by additional stress for the patient. Injectable materials eliminate the need for an operation [241, 242]. The material is simply injected into the area of interest, typically bone fractures and defects, where it will self-organize into the required structure in a minimal invasive procedure. Mechanical stability and integrity are achieved by subsequent crosslinking of the material by light-induced or thermal gelation, for example [243]. Other systems have been reported to gel spontaneously relying on click-chemistry [244, 245] or physiological pH and ion concentrations which trigger the crosslinking reaction [246, 247]. Furthermore, irregular shaped defects which are difficult to treat with preformed scaffolds can easily be filled with injectable materials [248]. One very well-known and investigated material in that respect is calcium phosphate cement (CPC). Calcium phosphate cement is self-setting due to the interaction between acidic and basic calcium phosphate compounds [248]. The injectable material can be administered in form of a paste, solution, emulsion or dispersion allowing the co-injection of a cellular suspension creating a 3D cell-infused structure [248]. Poor injectability due to liquid–solid phase-separation (filter-pressing), brittleness and unintentional material distribution into the surrounding tissue and blood are some of the disadvantages of injectable CPCs [248, 249]. Besides inorganic cements, a broad range of polymeric materials has been investigated as injectable scaffolds. In contrast to inorganic materials, injectable polymers are often capable of handling high mechanical stresses but lack the important factors for bone regeneration like bioactivity or osteoconductivity. An overview about injectable materials for TE applications has been published by Hou et al. [248].
The design of injectable composite materials aims to combine the elastic properties of polymeric systems with the bioactive and osteoconductive properties of bioactive glasses and ceramic which will be reviewed in "Examples of injectable hydrogel composites in bone tissue engineering" section. As discussed in "Bioprinting" section for bioprinting of hydrogel composites, the addition of inorganic particles to the polymeric solution mainly alters the properties of the resulting hydrogel rather than the properties of the pre-gel material. However, the size and amount of inorganic particles added to a polymeric solution do certainly influence the rheological properties and thus the injectability of the system [250] as will be discussed below. Typically, polymeric solutions exhibit good injectability while inorganic materials can be difficult to inject [248, 249]. Consequently, the injectability of the material needs to be investigated for each composite and material combination in order to find the most suitable system. Besides conventional injectable materials, additional functionalities like magnetic properties for magnetically triggered drug release, bactericidal effects or the ability to generate heat via IR-absorption can be introduced via incorporation of additional moieties as discussed in "Examples of injectable hydrogel composites with additional functionalities" section.
Composites as injectable materials
Examples of injectable hydrogel composites in bone tissue engineering
The incorporation of fillers provides advantages in terms of mechanical properties and bioactivity. For example, addition of 20–70 nm hydroxyapatite nanoparticles (HAp) to PEG hydrogels results in an increased Young’s and tensile modulus [251]. The resulting composites are extremely tough and extensible, as illustrated in Fig. 6a. The addition of HAp nanoparticles significantly increases Young’s modulus, fracture stress, ultimate strain, and toughness of the polymeric composite (Fig. 6b, c). These enhanced physical properties can be attributed to physical interactions between the polymer chains and the HAp nanoparticles. The particles act as physical crosslinking points which reinforce the photochemically crosslinked hydrogel as schematically illustrated in Fig. 6d. In addition, the cell adhesion of pure PEG hydrogels can be overcome by HAp addition since HAp is known for its high protein adsorption which induces cellular attachment.
The tensile properties (a, b) and mechanical properties (c) of PEG hydrogels are significantly improved by the addition of HAp nanoparticles. The mechanical improvement results from strong physical interactions between the polymeric chains and the incorporated nanoparticles as schematically illustrated (d). Reprinted from Ref. [253] with permission of ACS Publications
Song et al. [252] compared the influence of porous aggregates of HAp nanocrystals (ComHA) to compact micrometer-sized calcined HAp particles (CalHA) on the mechanical properties of an injectable poly(2-hydroxyethylmethacrylate) (pHEMA) hydrogel. They observed an enhancement of the mechanical properties for both systems. However, the composites containing aggregates of HAp nanocrystals were significantly stiffer and showed an enhanced resistance to crack formation compared to composites containing micron-sized HAp particles. The larger surface area and the resulting higher absorbance capacity of the smaller particles were given as possible explanations for the observed size-dependent reinforcement. The enhanced absorption of prepolymer chains to the nanocrystals during hydrogel formation might improve the interaction and structural integrity of the two components. In addition, SEM images revealed that the hydrogel-infused nano-sized HAp aggregates flattened into plywood-like structures upon compression which might provide an energy-dissipation mechanism, thus leading to an enhanced resistance to crack formation. Subcutaneous injection of the composite system (pHEMA-ComHA) proved its nondegradable nature. However, a slight increase in surface roughness was observed which might be the result of the dissociation of the inorganic filler. In vivo experiments with cell-seeded composites showed that attachment and osteogenic differentiation of bone marrow stromal cells (BMSCs) were supported by the material.
The reinforcement of PEG-based hydrogels by anisotropic hydroxyapatite was also investigated by Fu et al. [253]. In this case, a thermosensitive co-polymer consisting of poly(ethylene glycol)–poly(ε-caprolactone)–poly(ethylene glycol) (PEG–PCL–PEG, PECE) was tested. Gelation, melting, and crystallization temperature of the composite could be adjusted by the content of HAp particles. Due to hydrogen-bond formation between the polymer and the inorganic particles, the melting temperature of the composite was increased while crystallization and gelation temperatures were decreased compared to the pure polymer. This effect was also reported by Fan et al. as a result of the incorporation of tricalcium phosphate (β-TCP) and tetracalcium phosphate (TTCP) into PEG–PCL–PEG hydrogels [254]. The incorporation of hydroxyapatite in form of acellular bone matrix (ABM) granules into PEG–PCL–PEG hydrogels also resulted in a thermosensitive injectable hydrogel with thermal transition temperatures around 37 °C and an enhanced resistance toward degradation due to hydrogen-bond formation between the polymeric chains and the inorganic particles [255].
Injectability, bone ingrowth, and cell-material interaction of PEG–PCL–PEG composites could further be enhanced by the addition of collagen to the PEG–PCL–PEG/HAP composites [256].
Similar effects were shown by Savestani et al. [257]. They found that polar interactions and hydrogen bonding between uncrosslinked poly(lactide ethylene oxide fumarate) (PLEOF) and anisotropic hydroxyapatite nanoparticles cause an increase in viscosity and storage modulus.
A distinct influence on the degradation behavior of injectable, thermosensitive poly(ethylene glycol)-poly(lactic acid-co-glycolic acid)-poly(ethylene glycol) (PEG–PLGA–PEG, PELGA) hydrogels by the incorporation of hydroxyapatite particles (HAp) was reported by Lai et al. [258]. PELGA hydrogels containing HAp nanoparticles showed a higher pH value than pristine PELGA hydrogels due to the alkaline dissolution products of the HAp particles. This increase in pH caused a neutralization of acidic degradation products resulting from PLGA degradation. The degradation of PLGA is known to be an auto-catalyzed process, meaning that the release of acidic degradation products accelerates the degradation process due to the decrease in the pH value [98, 99, 259, 260]. In the presented study, it was shown that the resistance to auto-catalyzed degradation can be significantly enhanced by the addition of HAp particles. The slight increase in the pH value enhances the hydrogel’s stability resulting in a significant prolonging of the degradation rate: while the pure PELGA hydrogel showed a weight loss of 85 % after 70 days of incubation, the PELGA/HAp composite exhibited a loss of 25 % after the same amount of time as shown in Fig. 7.
a pH stabilization and b weight variation of PELGA and PELGA/HAp hydrogels during 70 days of incubation. The addition of HAp nanoparticles causes a slight increase of the pH value which has a significant effect on the weight loss of the hydrogel material. The pH stabilization hinders the auto-catalyzed degradation of the PELGA hydrogel leading to a major prolongation of the degradation time of the polymer as can be seen by the drastically reduced weight loss of the PELGA/HAp composite compared to the pristine hydrogel after 70 days of incubation. Reprinted from Ref. [258] with permission (© IOP Publishing, Reproduced with permission. All rights reserved)
In an early effort, Daculsi et al. reported a novel injectable polymer composite [261]. The so-called injectable bone substitute (IBS) consisted of a biphasic calcium phosphate/hydroxypropylmethylcellulose (HPMC) composite. Upon implantation in trabecular bone the composite resorbed rapidly while the colonization of the transplanted site by osteogenic cells and bone ingrowth was observed. The concept of HPMC as carrier for calcium phosphate ceramics and cements has continuously been improved. In a later study, the same group investigated the effect of particle size on injectability and bone ingrowth [250, 262]. The comparison of IBS consisting of BCP granules with diameters in the range of 40–80 µm and 80–200 µm and HPMC led to the conclusion that ceramic degradation, resorption, and bone colonization were higher in case of smaller particles. Bioactivities and bone-filling abilities were similar for both particle sizes. In an in vivo study, good injectability and effective bone filling was also demonstrated for particle sizes between 200 and 500 µm [263].
In order to further improve the mechanical properties of HPMC/calcium phosphate composites, a silane-functionalized HPMC (Si-HPMC) was developed [264]. Under appropriate pH conditions, the silane groups of the silane-functionalized HPMC will be transformed into silanol groups, which react with each other via condensation forming a 3D network structure. This self-hardening property increases the mechanical stability of Si-HPMC/calcium phosphate materials after injection [265]. Bone marrow stromal cells (BMSCs) can directly be injected with the composite material. The cells exhibit high cell viability (95 %). The composites show promising results with respect to osteoblast invasion and bone formation upon percutaneous injection into mice. By contrast on the other hand, in case of cell-free or pure Si-HPMC, no bone formation was observed.
A similar work was published by Sohier et al. [266]. Instead of using 40–80 µm BCP particles, larger particles with diameters between 80 and 200 µm were used. In contrast to the observations of Trojani et al. [265], no cell attachment and proliferation were observed although the investigated particle size was reported to enable cellular attachment. It was reported that the discrepancy between the two studies lies in the difference between in vitro and in vivo experiments. Due to a lack of enzymatic degradability, Si-HPMC can only be degraded via phagocytosis by macrophages [267, 268]. In vivo, the presence of inflammatory cells enables Si-HPMC degradation, and thus, migration of encapsulated cells through the polymeric network to the inorganic particles where cellular attachment takes place [265]. The issue of limited degradation and consequently limited adhesion to the inorganic particles in vitro could be circumvented by seeding cells onto BCP particles prior to composite formation or by addition of collagen to the Si-HPMC hydrogel [266]. In this case, both cellular attachment and suitable proliferation were observed.
In a more recent study, Si-HPMC was investigated in combination with CPCs [269]. The composites proved to be easily injectable, fast setting, and exhibited enhanced fracture toughness [269].
The combination of natural polymers with bioactive glasses and ceramics has also been reported in the context of injectable scaffolds. Moreau et al. demonstrated that chitosan/CPC composites show enhanced mechanical properties compared to pure cements [270]. Furthermore, the stability of chitosan was significantly improved. Upon mixing with CPC, the pH value of the chitosan solution was increased. Since chitosan is only soluble in acidic solution an enhanced resistance to degradation resulted.
Nguyen et al. reported the generation of chitosan/BCP composites [271]. The composite material’s mechanical compressive strength increased with the amount of BCP nanoparticles added due to the adhesion of the polymeric chains onto the BCP particles surface causing a reinforcement of the hydrogel matrix. In addition, the attachment and proliferation of mesenchymal stem cells (MSCs) seeded onto the surface of the materials could be enhanced by incorporation of BCP particles. These effects are probably a result of the increased surface roughness after BCP addition to the polymeric matrix as well as the high serum protein adsorption to the CBP nanoparticles which are known to show a positive effect on cellular behavior like adhesion and proliferation [272].
Similar results were obtained using GG/bioglass composites [273]. The influence of sol–gel versus melt-derived bioactive glasses on the mechanical properties, degradation behavior, microbial and cellular response of the composites was investigated. In case of sol–gel-derived glasses, an increased resistance to degradation and enhanced mechanical properties were observed. Antibacterial activity was increased while MG63 cells seeded onto the scaffolds showed limited adhesion. The opposite behavior was found for melt-derived glasses: Increased degradation, decreased Young’s modulus and good cell adhesion were found. The different observations are attributed to the different chemical stabilities of sol–gel and melt-derived glasses. Enhanced ion release from sol–gel derived glasses, especially Ca2+, are considered as origin for the higher resistance to degradation and increased mechanical strength. Released Ca2+ ions could be incorporated into the GG network reinforcing its structure and thus mechanical stability and resistance to degradation. Similarly, dissolution of the sol–gel-derived glasses can contribute to antibacterial effects resulting from increased pH, ion release and ionic strength [274–276]. However, these high ion release profiles may also have cytotoxic effects causing low cellular attachment [277]. By contrast, the melt-derived glass investigated showed enhanced release of magnesium ions which are known for their positive influence on cell adhesion and proliferation [101].
Fedorovich et al. [278] reported similar observations in in vivo experiments using composites of Matrigel and BCP microparticles or apatitic (CaP) nanoparticles. Apatitic nanoparticles showed osteoinductive properties and induced osteoclast activation of encapsulated multipotent stromal cells (MSCs). However, no bone formation was observed. In contrast, bone formation was observed in case of BCP microparticles-containing composites. Injection of pure Matrigel showed no osteogenesis. The lack of bone formation capacity of small particles was reported to be related to the close particle packing which impedes vascularization. Another explanation for the different biological response of the two systems was found in the particle’s chemical stability. While the BCP particles had been sintered at elevated temperatures resulting in an enhanced crystallinity and chemical stability, the CaP particles were synthesized by a wet-chemical procedure without further sintering treatment. Consequently, the CaP particles were less resistant to degradation causing osteoclast activation and reducing osteogenesis.
Examples of injectable hydrogel composites with additional functionalities
pNIPAAm hydrogels are also interesting as injectable materials due to their thermo-responsive behavior. Growth factors or proteins like recombinant human bone morphogenic proteins (BMPs) can be incorporated into the polymeric matrix, directly be delivered to the injection site and subsequently be released. The incorporation of BCP and superparamagnetic iron oxide nanoparticles (SPIONs) into pNIPAAm hydrogels has been shown to increase the resistance to degradation and enhance the mechanical properties of pNIPAAm block-co-polymers [279]. These reinforcing effects were attributed to hydrogen bonds forming additional physical crosslinking points in the polymeric networks. In addition, enhanced ALP activity of mesenchymal stem cells (MSCs) and human fetal osteoblastic cells (hFOBs) was observed in pNIPAAm/bioactive glass composites [249, 280]. Furthermore, the incorporation of magnetic moieties into the polymeric network structure may allow for a magnetically controlled on-demand release of encapsulated drugs.
The combination of antibacterial effects and bioactive properties of injectable materials based on dextran/carboxymethyl cellulose (CMC) hydrogels supplemented with silver nanoparticle coated bioactive glass particles (Ag-BG) was demonstrated by Wren et al. [281]. The control systems, pure dextran/CMC hydrogel and BG-doped dextan/CMC hydrogel showed no bactericidal effect, distinct antibacterial properties were observed for Ag-BG-doped hydrogels. Among the tested bacteria species, E. coli cultures showed the most pronounce effects while other species, S. aureus and S. epidermidis, revealed a higher resistance to the antimicrobial compound which is probably a result of their higher cell wall complexity compared to E. coli [282].
A multifunctional PEG-based hydrogel system was investigated by Sahu et al. [283] who introduced graphene oxide (GO) nanosheets as physical crosslinking points for poly(ethylene glycol)–poly(propylene oxide)–poly(ethylene glycol) (PEG–PPO–PEG, Pluronic) hydrogels. Under appropriate conditions (e.g., 0.4 wt% GO, 0.25–1 wt% Pluronic, 37 °C), the mixture formed a hydrogel due to hydrophobic association between the inorganic sheets and the polymer chains which increased with increasing temperature due to the increased hydrophobicity of PPO at elevated temperature. In addition, hydrogen bonding between the GO surface and the PEG chains occurred. No gel formation was observed for high Pluronic concentrations which might be a result of an extensive adsorption of PPO chains onto the GO surface preventing hydrogen-bond formation between GO and PEG and thus, stable crosslinking. The gelation process was not only concentration but also pH dependent due to protonation–deprotonation of carboxylic groups (–COOH) which interfered with the formation of hydrogen bonds. Furthermore, the near-IR absorption of GO particles could be used to generate heat and thus, to induce gelation resulting in a light-sensitive system. In vivo, no noticeable degradation was observed during the 8 weeks post-injection.
The different discussed hydrogel–inorganic filler composites are summarized in Table 6, where the systems investigated, key findings, and applications are collected enabling a rapid comparison.
Conclusion and outlook
The combination of hydrogels with inorganic fillers leads to materials with superior properties for applications in the biomedical field. Synergetic effects occur which influence the mechanical behavior, degradation profiles and interactions with biological species. Hydrogel networks can be reinforced and the processability of inorganic materials like glasses and cements can be significantly improved by the combination of inorganic and organic materials. It is of crucial importance to choose the two components wisely. Particle size, preparation technique, dissolution effects and physical properties like UV-absorption need to be considered to ensure the successful and beneficial incorporation of inorganic materials into hydrogel networks. If all criteria are fulfilled, highly biologically active materials with tailored degradation profiles and mechanical properties result. As discussed in this review article based on published work, these materials are particularly interesting for TE applications using modern additive manufacturing techniques, as injectable materials or for the encapsulation of cells in 3D network structures to study the effect of the extracellular environment and architecture on cellular behavior.
The addition of inorganic fillers to polymeric matrices is especially useful to enhance the mechanical stability of the system. The introduction of additional physical crosslinking points enables increased tensile strength, shape recovery, and energy dissipation under compression or shear stress which is of great benefit for TE applications. Furthermore, inorganic fillers can help to stimulate the behavior of cells encapsulated inside the hydrogel matrix. The effects which influence cellular behavior like proliferation and differentiation are complex, especially in three dimensions. The general biological processes in three dimensional environments need to be more comprehensively investigated in order to draw incontrovertible conclusions about the cellular behavior in composite materials. Besides the great progress made in these fields, many effects arising from the combination of inorganic and organic materials are still poorly understood and it can only be hypothesized about their origins. One reason for this lack of a fundamental understanding is the complexity of the evolving systems. Many combinatorial effects need to be considered which is often challenging since the behavior of the individual components is not in all cases well understood. For example, the biological effects of ions released from bioactive glasses are still not comprehensively uncovered. By combining bioactive glasses with polymeric materials new questions arise. The released ions can have a significant influence on the polymeric material, especially in case of ionically crosslinked gels like alginate. The released ions can thus be scavenged by the polymeric chains which will alter the ion release profile and consequently, the cellular response to these materials. Thus, these complex interactions need to be considered and carefully investigated further. Although basic requirements, such as biocompatibility and biodegradability, are valid for all discussed applications, each application makes additional demands on the materials properties. In addition, for cell encapsulation experiments the appropriate cell population needs to be identified for a given hydrogel/inorganic filler system in order to stimulate the anticipated cellular response. To tackle all these requirements the composites need to be specifically designed or able to adapt for a given application. While most applications have focused on bone tissue given the bioactive character of the fillers used, e.g., bioactive glasses, CaP, new research areas for soft tissue regeneration like wound healing are started to be explored [123]. The introduction of additional functionalities by incorporation of carbonaceous fillers (CNTs, GO) or magnetic nanoparticles remains a viable field for further research enabling the control of cellular growth and behavior by anisotropic structural elements, electrical or magnetic stimulation [284, 285]. Furthermore, the incorporation of magnetic or fluorescent particles as well as inorganic elements can be used for simultaneous in vivo imaging of the administered materials. This strategy would allow for the detection or monitoring of the implanted materials via fluorescent methods or magnetic resonant imaging techniques enabling a direct observation of the material’s position, integrity, and fate during and after implantation [18, 285]. The introduction of specific functionalities, microstructures, molecular adsorption, and mechanical properties are also of significant importance for the active recruitment of cells in vivo. Of course, the migration and invasion of cells to and into the implant are important considerations for the design of successfully engineered artificial tissues and implants. Many strategies have been proposed and are currently being explored to enable the active recruitment of cells to the implantation site. Advanced materials which recruit cells via chemical, mechanical or electrical cues can be envisioned. To this effect, lessons can be learned from natural recruitment strategies like the active recruitment of stem cells by tumors or sites of injury [286, 287].
The applications of the discussed composite systems are not solely limited to regenerative medicine. They are also valuable model systems for the investigation of cell-material interaction, cellular behavior in three-dimensions, migration behavior, and tumor growth or as more complex tissue models in drug testing and disease treatment. The huge variety and diversity of available materials and applications result in an immense scope which needs to be examined in order to find the most suitable system for a given application. Various interesting and promising results have been gained already, and materials with enhanced processibility and mechanical properties which display the anticipated cellular behavior have been designed. Nevertheless, more studies are inevitable to gain a comprehensive understanding of the governing process and to widen the application fields of this class of composite systems.
Abbreviations
- ALP:
-
Alkaline phosphatase
- ABM:
-
Acellular bone matrix
- Ag-NPs:
-
Silver nanoparticles
- BCP:
-
Biphasic calcium phosphate
- BG:
-
Bioactive glass
- BMP-2:
-
Morphogenetic protein-2
- BMPs:
-
Recombinant human bone morphogenic proteins
- BMSC:
-
Bone marrow stromal cells
- CA:
-
Collagen–alginate
- CaP:
-
Calcium phosphate (apatite)
- CaP:
-
Apatitic nanoparticles
- CNSC:
-
Carbon nanotube chain
- CNT:
-
Carbon nanotube
- CONP:
-
Cerium oxide nanoparticle
- CPC:
-
Calcium phosphate cement
- DPSC:
-
Dental pulp stem cell
- ECM:
-
Extracellular matrix
- EHS:
-
Engelbreth–Holm–Swarm mouse sarcoma
- ELP:
-
Elastin-like polypeptide
- EPO:
-
Erythropoietin
- FBS:
-
Fetal bovine serum
- Gel:
-
Gelatin
- GelMA:
-
Gelatin methacrylate
- GG:
-
Gellan gum
- GO:
-
Graphene oxide
- HA:
-
Hyaluronic acid
- HA-CPN:
-
Hyaluronic acid-g-chitosan-g-poly(N-isopropylacrylamide)
- HAp:
-
Hydroxyapatite
- hBMSC:
-
Human bone marrow-derived mesenchymal stem cells
- HCA:
-
Carbonated hydroxyapatite
- hFOBs:
-
Human fetal osteoblastic cells
- HPMC:
-
Hydroxypropylmethylcellulose
- IBS:
-
Injectable bone substitute
- IEP:
-
Isoelectric point
- LCST:
-
Lower critical solution temperature
- MBG:
-
Mesoporous bioactive glass
- nBG:
-
Nano-bioglass
- nHAp:
-
Nano-hydroxyapatite
- OC:
-
Osteocalcin
- OPF:
-
Oligo(poly(ethylene glycol) fumarate
- PAAc or PAA:
-
Poly(acrylic acid)
- PCL:
-
Poly(ε-caprolactone)
- PEG:
-
Poly(ethylene glycol)
- PEGDA:
-
PEG diacrylate
- PEGDMA:
-
PEG dimethacrylate
- PELGA:
-
Poly(ethylene glycol)-poly(lactic acid-co-glycolic acid)-poly(ethylene glycol)
- pHEMA:
-
Poly(2-hydroxyethyl methacrylate)
- PLEOF:
-
Poly(lactide ethylene oxide fumarate)
- PLGA:
-
Poly(lactic acid-co-glycolic acid)
- pNIPAAm:
-
Poly(N-isopropylacrylamide)
- polyp:
-
Polyphosphate
- PPO:
-
Poly(propylene oxide)
- Si-HPMC:
-
Silated hydroxypropylmethylcellulose
- SPIONS:
-
Superparamagnetic iron oxide nanoparticles
- TCP:
-
Tricalcium phosphate
- TE:
-
Tissue engineering
- TTCP:
-
Tetracalcium phosphate
References
Lodish H, Berk A, Zipursky LS, Matsudaira P, Baltimore D, Darnell JE (2002) Molecular cell biology. W.H. Freemann and Company, New York
Lee J, Cuddihy MJ, Kotov NA (2008) Three-dimensional cell culture matrices: state of the art. Tissue Eng Part B Rev 14:61–86
Huh D, Hamilton GA, Ingber DE (2011) From 3D cell culture to organs-on-chips. Trends Cell Biol 21:745–754
Haycock JW (2011) 3D cell culture. Springer Science and Business Media, New York
Gaharwar AK, Peppas NA, Khademhosseini A (2014) Nanocomposite hydrogels for biomedical applications. Biotechnol Bioeng 111:441–453
Rezwan K, Chen QZ, Blaker JJ, Boccaccini AR (2006) Biodegradable and bioactive porous polymer/inorganic composite scaffolds for bone tissue engineering. Biomaterials 27:3413–3431
Carrow JK, Gaharwar AK (2015) Bioinspired polymeric nanocomposites for regenerative medicine. Macromol Chem Phys 216:248–264
Vashist A, Ahmad S (2015) Hydrogels in tissue engineering: scope and applications. Curr Pharm Biotechnol 16:606–620
Orive G, Hernández RM, Gascón AR, Calafiore R, Chang TMS, de Vos P, Hortelano G, Hunkeler D, Lacík I, Shapiro AMJ, Pedraz JL (2003) Cell encapsulation: promise and progress. Nat Med 9:104–107
Uludag H, de Vos P, Tresco PA (2000) Technology of mammalian cell encapsulation. Adv Drug Deliv Rev 42:29–64
Hunt NC, Grover LM (2010) Cell encapsulation using biopolymer gels for regenerative medicine. Biotechnol Lett 32:733–742
Zhao X, Kim J, Cezar CA, Huebsch N, Lee K, Bouhadir K, Mooney DJ (2011) Active scaffolds for on-demand drug and cell delivery. Proc Natl Acad Sci USA 108:67–72
Cezar CA, Kennedy SM, Mehta M, Weaver JC, Gu L, Vandenburgh H, Mooney DJ (2014) Biphasic ferrogels for triggered drug and cell delivery. Adv Healthc Mater 3:1869–1876
Ferris CJ, Gilmore KG, Wallace GG, In Het Panhuis M (2013) Biofabrication: an overview of the approaches used for printing of living cells. Appl Microbiol Biotechnol 97:4243–4258
Ivanova O, Williams C, Campbell T (2013) Additive manufacturing (AM) and nanotechnology: promises and challenges. Rapid Prototyp J 19:353–364
Liu Y, Kim E, Ghodssi R, Rubloff GW, Culver JN, Bentley WE, Payne GF (2010) Biofabrication to build the biology-device interface. Biofabrication 2:022002
Billiet T, Vandenhaute M, Schelfhout J, vanVlierberghe S, Dubruel P (2012) A review of trends and limitations in hydrogel-rapid prototyping for tissue engineering. Biomaterials 33:6020–6041
Schexnailder P, Schmidt G (2009) Nanocomposite polymer hydrogels. Colloid Polym Sci 287:1–11
Thoniyot P, Tan MJ, Karim AA, Young DJ, Loh XJ (2015) Nanoparticle-hydrogel composites: concept, design, and applications of these promising, multi-functional materials. Adv Sci. doi:10.1002/advs.201400010
Kretlow JD, Mikos AG (2007) Review: mineralization of synthetic polymer scaffolds for bone tissue engineering. Tissue Eng 13:927–938
Sanchez C, Julián B, Belleville P, Popall M (2015) Applications of hybrid organic-inorganic nanocomposites. J Mater Chem 15:3559–3592
Hule RA, Pochan DJ (2007) Polymer nanocomposites for biomedical applications. MRS Bull 32:354–358
Boccaccini AR, Erol M, Stark WJ, Mohn D, Hong Z, Mano JF (2010) Polymer/bioactive glass nanocomposites for biomedical applications: a review. Compos Sci Technol 70:1764–1776
Peppas NA, Hilt JZ, Khademhosseini A, Langer R (2006) Hydrogels in biology and medicine: from molecular principles to bionanotechnology. Adv Mater 18:1345–1360
Hoffman AS (2002) Hydrogels for biomedical applications. Adv Drug Deliv Rev 54:3–12
Annabi N, Tamayol A, Uquillas JA, Akbari M, Bertassoni LE, Cha C, Camci-Unal G, Dokmeci MR, Peppas NA, Khademhosseini A (2014) 25th anniversary article: rational design and applications of hydrogels in regenerative medicine. Adv Mater 26:85–124
de las Heras Alarcón C, Pennadam S, Alexander C (2005) Stimuli responsive polymers for biomedical applications. Chem Soc Rev 34:276–285
Jeong B, Gutowska A (2002) Lessons from nature: stimuli-responsive polymers and their biomedical applications. Trends Biotechnol 20:305–311
Huebsch N, Kearney CJ, Zhao X, Kim J, Cezar CA, Suo Z, Mooney DJ (2014) Ultrasound-triggered disruption and self-healing of reversibly cross-linked hydrogels for drug delivery and enhanced chemotherapy. Proc Natl Acad Sci USA 111:9762–9767
Kennedy S, Bencherif S, Norton D, Weinstock L, Mehta M, Mooney DJ (2014) Rapid and extensive collapse from electrically responsive macroporous hydrogels. Adv Healthc Mater 3:500–507
Kearney CJ, Skaat H, Kennedy SM, Hu J, Darnell M, Raimondo TM, Mooney DJ (2015) Switchable release of entrapped nanoparticles from alginate hydrogels. Adv Healthc Mater 4:1634–1639
Drury JL, Mooney DJ (2003) Hydrogels for tissue engineering: scaffold design variables and applications. Biomaterials 24:4337–4351
Kim JK, Kim HJ, Chung JY, Lee JH, Young SB, Kim YH (2014) Natural and synthetic biomaterials for controlled drug delivery. Arch Pharm Res 37:60–68
Seliktar D (2012) Designing cell-compatible hydrogels for biomedical applications. Science 336:1124–1128
Engel J, Bächinger HP (2005) Structure, stability and folding of the collagen triple helix. Top Curr Chem 247:7–33
Walters BD, Stegemann JP (2014) Strategies for directing the structure and function of three-dimensional collagen biomaterials across length scales. Acta Biomater 10:1488–1501
Fratzl P, Misof K, Zizak I, Rapp G, Amenitsch H, Bernstorff S (1997) Fibrillar structure and mechanical properties of collagen. J Struct Biol 122:119–122
White DJ, Puranen S, Johnson MS, Heino J (2004) The collagen receptor subfamily of the integrins. Inter J Biochem Cell Biol 36:1405–1410
Heino J (2000) The collagen receptor integrins have distinct ligand recognition and signaling functions. Matrix Biol 19:319–323
Brown RA, Wiseman M, Chuo CB, Cheema U, Nazhat SN (2005) Ultrarapid engineering of biomimetic materials and tissues: fabrication of nano- and microstructures by plastic compression. Adv Funct Mater 15:1762–1770
Bitar M, Salih V, Brown RA, Nazhat SN (2007) Effect of multiple unconfined compression on cellular dense collagen scaffolds for bone tissue engineering. J Mater Sci Mater Med 18:237–244
Hu X, Cebe P, Weiss AS, Omenetto F, Kaplan DL (2012) Protein-based composite materials. Mater Today 15:208–215
Sarker B, Lyer S, Arkudas A, Boccaccini AR (2013) Collagen/silica nanocomposites and hybrids for bone tissue engineering. Nanotechnol Rev 2:427–447
Allison DD, Grande-Allen KJ (2006) Hyaluronan: a powerful tissue engineering tool. Tissue Eng 12:2131–2140
Burdick JA, Prestwich GD (2011) Hyaluronic acid hydrogels for biomedical applications. Adv Healtc Mater 23:H41–H56
Burdick JA, Chung C, Jia X, Randolph MA, Langer R (2005) Controlled degradation and mechanical behavior of photopolymerized hyaluronic acid networks. Biomacromolecules 6:386–391
Kuo JW, Prestwich GD (2010) Hyaluronic acid. In: Materials of biological origin—materials analysis and implant uses, comprehensive biomaterials. Elsevier
Augst AD, Kong HJ, Mooney DJ (2006) Alginate hydrogels as biomaterials. Macromol Biosci 6:623–633
Draget KI, Skjåk-Bræk G, Smidsrød O (1997) Alginate based new materials. Int J Biol Macromol 21:47–55
Kong HJ, Kaigler D, Kim K, Mooney DJ (2004) Controlling rigidity and degradation of alginate hydrogels via molecular weight distribution. Biomacromolecules 5:1720–1727
Bouhadir KH, Lee KY, Alsberg E, Damm KL, Anderson KW, Mooney DJ (2001) Degradation of partially oxidized alginate and its potential application for tissue engineering. Biotechnol Prog 17:945–950
Sarker B, Papageorgiou DG, Silva R, Zehnder T, Gul-E-Noor F, Bertmer M, Kaschta J, Chrissafis K, Detsch R, Boccaccini AR (2014) Fabrication of alginate-gelatin crosslinked hydrogel microcapsules and evaluation of the microstructure and physic-chemical properties. J Mater Chem B 2:1470–1482
Venkatesan J, Bhatnagar I, Manivasagan P, Kang KH, Kim SK (2015) Alginate composites for bone tissue engineering: a review. Int J Biol Macromol 72:269–281
Balakrishnan B, Jayakrishnan A (2005) Self-cross-linking biopolymers as injectable in situ forming biodegradable scaffolds. Biomaterials 26:3941–3951
Liao H, Zhang H, Chen W (2009) Differential physical, rheological, and biological properties of rapid in situ gelable hydrogels composed of oxidized alginate and gelatin derived from marine or porcine sources. J Mater Sci Mater Med 20:1263–1271
Sarker B, Singh R, Silva R, Roether JA, Kaschta J, Detsch R, Schubert DW, Cicha I, Boccaccini AR (2014) Evalulation of fibroblasts adhesion and proliferation on alginate-gelatin crosslinked hydrogels. PLoS One 9:e107952
Grigore A, Sarker B, Fabry B, Boccaccini AR, Detsch R (2014) Behavior of encapsulated MG-63 cells in RGD and gelatine-modified alginate hydrogels. Tissue Eng Part A 20:2140–2150
Rowley JA, Madlambayan G, Mooney DJ (1999) Alginate hydrogels as synthetic extracellular matrix material. Biomaterials 20:45–53
Hill SE, Ledward DA, Mitchell JR (1998) Functional properties of food macromolecules. Springer, Berlin
Park H, Park K, Shalaby WSW (2011) Biodegradable hydrogels for drug delivery. CRC Press, Boca Raton
Atala A, Mooney DJ (2013) Synthetic biodegradable polymer scaffolds. Springer, New York
Pluen A, Netti PA, Jain RK, Berk DA (1999) Diffusion of macromolecules in agarose gels: comparison of linear and globular configuarations. Biophys J 77:542–552
Pernodet N, Maaloum M, Tinland B (1997) Pore size of agarose gels by atomic force microscopy. Electrophoresis 18:55–58
Wang H, Hansen MB, Löwik DWPM, van Hest JCM, Li Y, Jansen JA, Leeuwenburgh SCG (2011) Oppositely charged gelatin nanospheres as building blocks for injectable and biodegradable gels. Adv Healthc Mater 23:H119–H124
Boanini E, Bigi A (2011) Biomimetic gelatin–octacalcium phosphate core–shell microspheres. J Colloid Interface Sci 362:594–599
Bigi A, Panzavolta S, Rubini K (2004) Relationship between triple-helix content and mechanical properties of gelatin films. Biomaterials 25:5675–5680
Ross-Murphy SB (1992) Structure and rheology of gelatin gels: recent progress. Polymer 33:2622–2627
Pezron I, Djabourov M, Leblond J (1991) Conformation of gelatin chains in aqueous solutions: 1. A light and small-angle neutron scattering study. Polymer 32:3201–3210
Fialho AM, Moreira LM, Granja AT, Popescu AO, Hoffmann K, Sá-Correia I (2008) Occurrence, production, and application of gellan: current state and perspectives. Appl Microbiol Biotechnol 79:889–900
Giavasis I, Harvey LM, McNeil B (2000) Gellan gum. Crit Rev Biotechnol 20:177–211
Madihally SV, Matthew HWT (1999) Porous chitosan scaffolds for tissue engineering. Biomaterials 20:1133–1142
Suh JKF, Matthew HWT (2000) Application of chitosan-based polysaccharide biomaterials in cartilage tissue engineering: a review. Biomaterials 21:2589–2598
Chandy T, Sharma CP (1990) Chitosan-as a biomaterial. Biomater Artif Cells Artif Organs 18:1–24
Kleinman HK, Martin GR (2005) Matrigel: basement membrane matrix with biological activity. Semin Cancer Biol 15:378–386
Hughes CS, Postovit LM, Lajoie GA (2010) Matrigel: a complex protein mixture required for optimal growth of cell culture. Proteomics 10:1886–1890
Daamen WF, Veerkamp JH, van Hest JC, van Kuppevelt TH (2007) Elastin as a biomaterial for tissue engineering. Biomaterials 28:4378–4398
Kundu S (2014) Silk biomaterials for tissue engineering and regenerative medicine. Woodhead Publishing, Cambridge
Chang C, Zhang L (2011) Cellulose-based hydrogels: present status and application prospects. Carbohydr Polym 84:40–53
Chien KB, Chung EJ, Shah RN (2014) Investigation of soy protein hydrogels for biomedical applications: materials characterization, drug release, and biocompatibility. J Biomater Appl 28:1085–1096
Paliwal R, Palakurthi S (2014) Zein in controlled drug delivery and tissue engineering. J Control Release 189:108–122
Bailey FE, Koleske JV (2012) Poly(ethylene oxide). Elsevier, London
Ulery BD, Nair LS, Laurencin CT (2011) Biomedical applications of biodegradable polymers. J Polym Sci Part B 49:832–864
Helmy R (2012) Biotechnology—molecular studies and novel applications for improved quality of human life. InTech
Lin CC, Anseth KS (2008) PEG hydrogels for the controlled release of biomolecules in regenerative medicine. Pharm Res 26:631–643
Falco EE, Patel M, Fisher JP (2008) Recent developments in cyclic acetal biomaterials for tissue engineering applications. Pharm Res 25:2348–2356
Betz MW, Modi PC, Caccamese JF, Coletti DP, Sauk JJ, Fisher JP (2008) Cyclic acetal hydrogel system for bone marrow stromal cell encapsulation and osteodifferentiation. J Biomed Mater Res A 86:662–670
Lee KY, Mooney DJ (2001) Hydrogels for tissue engineering. Chem Rev 101:1869–1879
Lu S, Anseth KS (1999) Photopolymerization of multilaminated poly(HEMA) hydrogels for controlled release. J Control Release 57:291–300
Meyvis TKL, De Smedt SC, Demester J (2000) Influence of the degradation mechanism of hydrogels on their elastic and swelling properties during degradation. Macromolecules 33:4717–4725
Schild HG (1992) Poly(N-isopropylacrylamide): experiment, theory and application. Prog Polym Sci 17:163–249
Seiffert S, Weitz DA (2010) Microfluidic fabrication of smart microgels from macromolecular precursors. Polymer 51:5883–5889
Galaec IY, Mattiasson B (1999) “Smart” polymers and what they could do in biotechnology and medicine. Trends Biotechnol 17:335–340
Cooper SL, Bamford CH, Tsuruta T (1995) Polymer biomaterials in solution, as interfaces and as solids. Springer, New York
Nichol JW, Koshy ST, Bae H, Hwang CM, Yamanlar S, Khademhosseini A (2010) Cell-laden microengineered gelatin methacrylate hydrogels. Biomaterials 31:5536–5544
Van Vlierberghe S, Dubruel P, Schacht E (2011) Biopolymer-based hydrogels as scaffolds for tissue engineering applications: a review. Biomacromolecules 12:1387–1408
Yoshida T, Lai TC, Kwon GS, Sako K (2013) pH- and ion-sensitive polymers for drug delivery. Expert Opin Drug Deliv 10:1497–1513
Bourges X, Weiss P, Daculsi G, Legeay G (2002) Synthesis and general properties of silated-hydroxypropyl methylcellulose in prospect of biomedical use. Adv Colloid Interface Sci 99:215–228
Engineer C, Parikh J, Raval A (2011) Review on hydrolytic degradation behavior of biodegradable polymers from controlled drug delivery system. Trends Biomater Artif Organs 25:79–85
Lyu SP, Untereker D (2009) Degradability of polymers from implantable biomedical devices. Int J Mol Sci 10:4033–4065
Kilpadi KL, Chang PL, Bellis SL (2001) Hydroxylapatite binds more serum proteins, purified integrins, and osteoblast precursor cells than titanium or steel. J Biomed Mater Res 57:258–267
Hoppe A, Güldal NS, Boccaccini AR (2011) A review of the biological response to ionic dissolution products from bioactive glasses and glass-ceramics. Biomaterials 32:2757–2774
Lutolf MP, Hubbell JA (2005) Synthetic biomaterials as instructive extracellular microenvironments for morphogenesis in tissue engineering. Nat Biotechnol 23:47–55
Mooney E, Mackle JN, Blond DJ, O’Cearbhaill E, Shaw G, Blau WJ, Barry FP, Barron V, Murphy JM (2012) The electrical stimulation of carbon nanotubes to provide a cardiomimetic cue to MSCs. Biomaterials 33:6132–6139
Sahithi K, Swetha M, Ramasamy K, Srinivasan N, Selvamurugan N (2010) Polymeric composites containing carbon nanotubes for bone tissue engineering. Int J Biol Macromol 46:281–283
Stevens MM (2008) Biomaterials for bone tissue engineering. Mater Today 11:18–25
Suchanek W, Yoshimura M (1998) Processing and properties of hydroxyapatite-based biomaterials for use as hard tissue replacement implants. J Mater Res 13:94–117
LeGeros RZ, LeGeros JP (2003) Calcium phosphate ceramics: past, present and future. Key Eng Mater 240–242:3–10
LeGeros RZ (1993) Biodegradation and bioresorption of calcium phosphate ceramics. Clin Mater 14:65–88
Song W, Tian M, Chen F, Tian Y, Wan C, Yu X (2009) The study on the degradation and mineralization mechanism of ion-doped calcium polyphosphate in vitro. J Biomed Mater Res B 89:430–438
Bodhak S, Bose S, Badyopadhyay A (2011) Bone cell-materials interactions on metal-ion doped polarized hydroxyapatite. Mater Sci Eng, C 31:755–761
Rodríguez-Valencia C, López-Álvarez M, Cochón-Cores B, Pereiro I, Serra J, González P (2013) Novel selenium-doped hydroxyapatite coatings for biomedical applications. J Biomed Mater Res A 101:853–861
Hench LL (2015) Opening paper 2015-Some comments on Bioglass: Four Eras of Discovery and Development, Biomed. Glasses 1:1–11
Hench LL (1998) Biocermics. J Am Ceram Soc 81:1705–1728
Rahaman MN, Day DE, Bal BS, Fu Q, Jung SB, Bonewald LF, Tomsia AP (2011) Bioactive glass in tissue engineering. Acta Biomater 7:2355–2373
Jell G, Stevens MM (2006) Gene activation by bioactive glasses. J Mater Sci Mater Med 17:997–1002
Day RM (2005) Bioactive glass stimulates the secretion of angiogenic growth factors and angiogenesis in vitro. Tissue Eng 11:768–777
Gorustovich AA, Roether JA, Boccaccini AR (2010) Effect of bioactive glasses on angiogenesis: a review of in vitro and in vivo evidences. Tissue Eng Part B Rev 16:199–207
Uo M, Mizuno M, Kuboki Y, Makishima A, Watari F (1998) Properties and cytotoxicity of water soluble Na2O–CaO–P2O5 glasses. Biomaterials 19:2277–2284
Hu Q, Li Y, Miao G, Zhao N, Chen X (2014) Size control and biological properties of monodispersed mesoporous bioactive glass sub-micron spheres. RSC Adv 4:22678–22687
Luz GM, Mano JF (2013) Nanoengineering of bioactive glasses: hollow and dense nanospheres. J Nanopart Res 15:1457–1468
Tsigkou O, Labbaf S, Stevens MM, Porter AE, Jones JR (2014) Monodispersed bioactive glass submicron particles and their effect on bone marrow and adipose tissue-derived stem cells. Adv Healthc Mater 3:115–125
Lukowiak A, Lao J, Lacroix J, Nedelec JM (2013) Bioactive glass nanoparticles obtained through sol-gel chemistry. Chem Comm 49:6620–6622
Miguez-Pacheco V, Hench LL, Boccaccini AR (2015) Bioactive glasses beyond bone and teeth: emerging applications in contact with soft tissue. Acta Biomater 13:1–15
Saranti A, Koutselas I, Karakassides MA (2006) Bioactive glasses in the system CaO–B2O3–P2O5: preparation, structural study and in vitro evaluation. J Non-Cryst Solids 352:390–398
Liang W, Rahaman MN, Day DE, Marion NW, Riley GC, Mao JJ (2008) Bioactive borate glass scaffold for bone tissue engineering. J Non-Cryst Solids 354:1690–1696
Sepulveda P, Jones JR, Hench LL (2002) Bioactive sol-gel foams for tissue repair. J Biomed Mater Res 59:340–348
Vallet-Regí M (2006) Ordered mesoporous materials in the context of drug delivery systems and bone tissue engineering. Chemistry 12:5934–5943
Vallet-Regí M, Balas F, Arcos D (2007) Mesoporous materials for drug delivery. Angew Chem Int Ed 46:7548–7558
Manzano M, Vallet-Regí M (2010) New developments in ordered mesoporous materials for drug delivery. J Mater Chem 20:5593–5604
Bellantone M, Williams HD, Hench LL (2002) Broad-spectrum bactericidal activity of Ag2O-doped bioactive glass. Antimicrob Agents Chemother 46:1940–1945
Blaker JJ, Nazhat SN, Boccaccini AR (2004) Development and characterization of silver-doped bioactive glass-coated sutures for tissue engineering and wound healing applications. Biomaterials 25:1319–1329
Bergaya F, Theng BKG, Lagaly G (2006) Handbook of clay science. Elsevier, Amsterdam
Dawson JI, Oreffo ROC (2013) Clay: new opportunites for tissue regeneration and biomaterial design. Adv Mater 25:4069–4086
Dawson JI, Kanczler JM, Yang XB, Attard GS, Oreffo ROC (2011) Clay gels for the delivery of regenerative microenvironments. Adv Mater 23:3304–3308
Wang Q, Mynar JL, Yoshida M, Lee E, Lee M, Okuro K, Kinbara K, Aida T (2010) High-water-content mouldable hydrogels by mixing clay and a dendritic molecular binder. Nature 463:339–343
Mieszawska AJ, Llamas JG, Vaiana CA, Kadakia MP, Naik RR, Kaplan DL (2011) Clay-enriched silk biomaterials for bone formation. Acta Biomater 7:3036–3041
Maisanaba S, Pichardo S, Puerto M, Gutiérrez-Praene D, Cameán AM, Jos A (2015) Toxicological evaluation of clay minerals and derived nanocomposites: a review. Environ Res 138:233–254
Harrison BS, Atala A (2007) Carbon nanotube applications for tissue engineering. Biomaterials 28:344–353
Bianco A, Kostarelos K, Partidos CD, Prato M (2005) Biomedical applications of functionalized carbon nanotubes. Chem Comm 7:571–577
Dreyer DR, Park S, Bielawski CW, Ruoff RS (2010) The chemistry of graphene oxide. Chem Soc Rev 39:228–240
Liu K, Zhang JJ, Cheng FF, Zheng TT, Wang C, Zhu JJ (2011) Green and facile synthesis of highly biocompatible graphene nanosheets and its application for cellular imaging and drug delivery. J Mater Chem 21:12034–12040
Lu CH, Yang HH, Zhu CL, Chen X, Chen GN (2009) A graphene platform for sensing biomolecules. Angew Chem Int Ed 48:4785–4787
Gao J, Gu H, Xu B (2009) Multifunctional magnetic nanoparticles: design, synthesis, and biomedical applications. Acc Chem Res 42:1097–1107
Tan MC, Chow GM, Ren L (2009) Nanostructured materials for biomedical applications. Transworld Research Network, Trivandrum
Gupta AK, Gupta M (2005) Synthesis and surface engineering of iron oxide nanoparticles for biomedical applications. Biomaterials 26:3995–4021
Pagé M (2002) Tumor targeting in cancer therapy. Springer, New York
Wahajuddin Arora S (2012) Superparamagnetic iron oxide nanoparticles: magnetic nanoplatforms as drug carriers. Int J Nanomed 7:3445–3471
Schubert D, Dargusch R, Raitano J, Chang SW (2006) Cerium and yttrium oxide nanoparticles are neuroprotective. Biochem Biophys Res Commun 342:86–91
Tiedge M, Lortz S, Drinkgern J, Lenzen S (1997) Complementary action of antioxidant gene expression and antioxidative defense status of insulin-producing cells. Diabetes 46:1733–1742
Tsai YY, Oca-Cossio J, Agering K, Simpson NE, Atkinson MA, Wasserfall CH, Constantinidis I, Sigmung W (2007) Novel synthesis of cerium oxide nanoparticles for free radical scavenging. Nanomedicine 2:325–332
Celardo I, Pedersen JZ, Traversa E, Ghibelli L (2011) Pharmacological potential of cerium oxide nanoparticles. Nanoscale 3:1411–1420
Dröge W (2002) Free radicals in the physiological control of cell function. Physiol Rev 82:47–95
Strong LE, Dahotre SN, West JL (2014) Hydrogel-nanoparticle composites for optically modulated cancer therapeutic delivery. J Control Release 178:63–68
Boccaccini AR, Blaker JJ (2005) Bioactive composite materials for tissue engineering scaffolds. Expert Rev Med Devices 2:303–317
García-Astrain C, Chen C, Burón M, Palomares T, Eceiza A, Fruk L, Corcuera MA, Gabilondo N (2015) Biocompatible hydrogel nanocomposites with covalently embedded silver nanoparticles. Biomacromolecules 16:1301–1310
Alvarez GS, Hélary C, Mebert AM, Wang X, Coradin T, Desimone MF (2014) Antibiotic-loaded silica nanoparticles-collagen composite hydrogels with prolonged antimicrobial activity for wound infection prevention. J Mater Chem B 2:4660–4670
Zeng R, Dietzel W, Witte F, Hort N, Blawert C (2008) Progress and challenge for magnesium alloys as biomaterials. Adv Eng Mater 10:B3–B14
Gutwein LG, Webster TK (2002) Osteoblast and chrondrocyte proliferation in the presence of alumina and titania nanoparticles. J Nanopart Res 4:231–238
Piconi C, Maccauro G (1999) Zirconia as a ceramic biomaterial. Biomaterials 20:1–25
Dewi AH, Ana ID, Wolke J, Jansen J (2015) Behavior of POP-calcium carbonate hydrogel as bone substitute with controlled release capability: a study in rat. J Biomed Mater Res A. doi:10.1002/jbm.a.35460
Liu K, Li Y, Xu F, Zuo Y, Zhang L, Wang H, Liao J (2009) Graphite/poly(vinyl alcohol) hydrogel composite as porous ringy skirt for artificial cornea. Mater Sci Eng, C 29:261–266
Lu N, Liu J, Li J, Zhang Z, Weng Y, Yuan B, Yang K, Ma Y (2014) Tunable dual-stimuli response of microgel composite consisting of reduced graphene oxide nanoparticles and poly(N-isopropylacrylamide) hydrogel microspheres. J Mater Chem B 2:3791–3798
Gross KA, Rodríguez-Lorenzo LM (2004) Biodegradable composite scaffolds with an interconnected spherical network for bone tissue engineering. Biomaterials 25:4955–4962
Sambudi NS, Sathyamurthy M, Lee GM, Park SB (2015) Electrospun chitosan/poly(vinyl alcohol) reinforced with CaCO3 nanoparticles with enhanced mechanical properties and biocompatibility for cartilage tissue engineering. Compos Sci Technol 106:76–84
Müller WEG, Tolba E, Schröder HC, Neufurth M, Wang S, Link T, Al-Nawas B, Wang X (2015) A new printable and durable N, O-carboxymethyl chitosan-Ca2+-polyphosphate complex with morphogenetic activity. J Mater Chem B 3:1722–1730
Murphy WL, Dennis RG, Kileny JL, Mooney DJ (2002) Salt fusion: an approach to improve pore interconnectivity within tissue engineering scaffolds. Tissue Eng 8:43–52
Legeros RZ, Lin S, Rohanizadeh R, Mijares D, Legeros JP (2003) Biphasic calcium phosphate biocermics: preparation, properties and applications. J Mater Sci Mater Med 14:201–209
Boccaccini AR, Ma PX (2014) Tissue engineering using ceramics and polymers. Elsevier, Burlington
Boccaccini AR, Maquet V (2003) Bioresorbable and bioactive polymer/bioglass composites with tailored pore structure for tissue engineering applications. Compos Sci Technol 63:2417–2429
Gkioni K, Leeuwenburgh SCG, Douglas TEL, Mikos AG, Jansen JA (2010) Mineralization of hydrogels for bone regeneration. Tissue Eng Part B Rev 16:577–585
Huang T, Xu H, Jiao K, Zhu L, Brown HR, Wang H (2007) A novel hydrogel with high mechanical strength: a macromolecular microsphere composite hydrogel. Adv Mater 19:1622–1626
Zhao F, Qin X, Feng S (2015) Microstructure, mechanical and swelling properties of microgel composite hydrogels with high microgel content and a microgel cluster crosslinker. RSC Adv 5(56):45113–45121. doi:10.1039/C5RA05969K
Sun Y, Liu S, Du G, Gao G, Fu J (2015) Multi-responsive and tough hydrogels based on triblock copolymer micelles as multi-functional macro-crosslinkers. Chem Commun 51:8512–8515
Zheng C, Huang Z (2015) Microgel reinforced composite hydrogels with pH-responsive, self-healing properties. Colloids Surf A 468:327–332
Ajayan PM, Schadler LS, Braun PV (2006) Nanocomposite science and technology. Wiley, New York
Ylänen H (2011) Bioactive glasses: materials, properties and applications. Elsevier, Oxford
Tilocca A, Cormack AN (2011) The initial stages of bioglass dissolution: a Car-Parrinello molecular-dynamics study of the glass-water interface. Proc R Soc A 467:2102–2111
Wang H, Zhao S, Zhou J, Shen Y, Huang W, Zhang C, Rahaman MN, Wang D (2014) Evaulation of borate bioactive glass scaffolds as a controlled delivery system for copper ions in stimulating osteogenesis and angiogenesis in bone healing. J Mater Chem B 2:8547–8557
Jones J, Clare A (2012) Bio-glasses: an introduction. Wiley, Chichester
Bernards MT, Qin C, Jiang S (2008) MC3T3-E1 cell adhesion to hydroxyapatite with adsorbed bone sialoprotein, bone osteopontin and bovine serum albumin. Colloids Surf B 64:236–247
del Pino P, Pelaz B, Zhang Q, Maffre P, Nienhaus GU, Parak WJ (2014) Protein corona formation around nanoparticles—from the past to the future. Mater Horiz 1:301–313
Stevens MM, George JH (2005) Exploring and engineering the cell surface interface. Science 310:1135–1138
Vroman L (1988) The life of an artificial device in contact with blood: initial events and their effect on its final state. Bull NY Acad Med 64:352–357
Franz S, Rammelt S, Scharnweber D, Simon JC (2011) Immune response to implants—a review of the implications for the design of immunomodulatory biomaterials. Biomaterials 32:6692–6709
Lynch I, Salvati A, Dawson KA (2009) Protein-nanoparticle interactions: what does the cell see? Nat Nanotechnol 4:546–547
Killion JA, Kehoe S, Geever LM, Devine DM, Sheehan E, Boyd D, Higginbotham CL (2013) Hydrogel/bioactive glass composites for bone regeneration applications: synthesis and characterization. Mater Sci Eng, C 33:4203–4212
Skardal A, Zhang J, McCoard L, Xu X, Oottamasathien S, Prestwich GD (2010) Photocorsslinkable hyaluronan-gelatin hydrogels for two-step bioprinting. Tissue Eng Part A 16:2675–2685
Pfister A, Landers R, Laib A, Hübner U, Schmelzeisen R, Mülhaupt R (2004) Biofunctional rapid prototyping for tissue-engineering applications: 3D bioplotting versus 3D printing. J Polym Sci A 42:624–638
Nakamura M, Iwanaga S, Henmi C, Arai K, Nishiyama Y (2010) Biomatrices and biomaterials for future developments of bioprinting and biofabrication. Biofabrication 2:014110
Hurtley S (2009) Location, location, location. Science 326:1205
Hollister SJ (2005) Porous scaffold design for tissue engineering. Nat Mater 4:518–524
Lee J, Cuddihy MJ, Kotov NA (2008) Three-dimensional cell culture matrices: state of the art. Tissue Eng Part B 14:61–86
Chaudhuri O, Koshy ST, Branco da Cunha C, Shin JW, Verbeke CS, Allison KH, Mooney DJ (2014) Extracellular matrix stiffness and composition jointly regulate the induction of malignant phenotypes in mammary epithelium. Nat Mater 13:970–978
Chaudhuri O, Gu L, Darnell M, Klumpers D, Bencherif SA, Weaver JC, Huebsch N, Mooney DJ (2015) Substrate stress relaxation regulates cell spreading. Nat Commun. doi:10.1038/ncomms7365
Velasco D, Tumarkin E, Kumacheva E (2012) Microfluidic encapsulation of cells in polymer microgels. Small 8:1633–1642
Schmidt JJ, Rowley J, Kong HJ (2008) Hydrogels used for cell-based drug delivery. J Biomed Mater Res A 87:1113–1122
Melchels FPW, Domingos MAN, Klein TJ, Malda J, Bartolo PJ, Hutmacher DW (2012) Additive manufacturing of tissues and organs. Prog Polym Sci 37:1079–1104
Griffith LG, Swartz MA (2006) Capturing complex 3D tissue physiology in vitro. Nat Rev Mol Cell Biol 7:211–224
Hutmacher DW, Loessner D, Rizzi S, Kaplan DL, Mooney DJ, Clements JA (2010) Can tissue engineering concepts advance tumor biology research? Trends Biotechnol 28:125–133
Hutmacher DW (2010) Biomaterials offer cancer research the third dimension. Nat Mater 9:90–93
Nyga A, Cheema U, Loizidou M (2011) 3D tumour models: novel in vitro approaches to cancer studies. J Cell Commun Signal 5:239–248
Xu X, Farach-Carson MC, Jia X (2014) Three-dimensional in vitro tumor models for cancer research and drug evaluation. Biotechnol Adv 32:1256–1268
Song HHG, Park KM, Gerecht S (2014) Hydrogels to model 3D in vitro microenvironment of tumor vascularization. Adv Drug Deliv Rev 79–80:19–29
Hutmacher DW, Horch RE, Loessner D, Rizzi S, Sieh S, Reichert JC, Clements JA, Beier JP, Arkudas A, Bleiziffer O, Kneser U (2009) Translating tissue engineering technology platforms into cancer research. J Cell Mol Med 13:1417–1427
Horch RE, Boos AM, Quan Y, Bleiziffer O, Detsch R, Boccaccini AR, Alexiou C, Sun J, Beier JP, Arkudas A (2013) Cancer research by means of tissue engineering—is there a rationale? J Cell Mol Med 17:1197–1206
Costa P (2015) Biofabricated constructs as tissue models: a short review. J Mater Sci Mater Med 26(4):156. doi:10.1007/s10856-015-5502-7
Chang CW, van Spreeuwel A, Zhang C, Varghese S (2010) PEG/clay nanocomposite hydrogel: a mechanically robust tissue engineering scaffold. Soft Matter 6:5157–5164
Bongio M, van den Beucken JJJP, Nejadnik MR, Leeuwenburgh SCG, Kinard LA, Kasper FK, Mikos AG, Jansen JA (2011) Biomimetic modification of synthetic hydrogels by incorporation of adhesive peptides and calcium phosphate nanoparticles: in vivo evaluation of cell behavior. Eur Cell Mater 22:359–376
Patel M, Patel KJ, Caccamese JF, Coletti DP, Sauk JJ, Fisher JP (2010) Characterization of cyclic acetal hydroxyapatite nanocomposites for craniofacial tissue engineering. J Biomed Mater Res A 94:408–418
Zeng Q, Han Y, Li H, Chang J (2014) Bioglass/alginate composite hydrogel beads as cell carriers for bone regeneration. J Biomed Mater Res B Appl Biomater 102:42–51
Sadat-Shojai M, Khorasani MT, Jamshidi A (2015) 3-Dimensional cell-laden nano-hydroxyapatite/protein hydrogels for bone regeneration applications. Mater Sci Eng C Mater Biol Appl 49:835–843
Wheeler TS, Sbravati ND, Janorkar AV (2013) Mechanical & cell culture properties of elastin-like polypeptide, collagen, bioglass, and carbon nanosphere composites. Ann Biomed Eng 41:2042–2055
Khanarian NT, Haney NM, Burga RA, Lu HH (2012) A functional agarose-hydroxyapatite scaffold for osteochondral interface regeneration. Biomaterials 33:5247–5258
Wu LN, Ishikawa Y, Sauer GR, Genge BR, Mwale F, Mishima H, Wuthier RE (1995) Morphological and biochemical characterization of mineralizing primary cultures of avian growth plate chondrocytes: evidence for cellular processing of Ca2+ and Pi prior to matrix mineralization. J Cell Biochem 57:218–237
Mwale F, Tchetina E, Wu CW, Poole AR (2002) The assembly and remodeling of the extracellular matrix in growth plate in relationship to mineral deposition and cellular hypertrophy: an in situ study of collagens II and IX and proteoglycan. J Bone Miner Res 17:275–283
Khanarian NT, Jiang J, Wan LQ, Mow VC, Lu HH (2012) A hydrogel-mineral composite scaffold for osteochondral interface tissue engineering. Tissue Eng Part A 18:533–545
Linsenmayer TF, Long F, Nurminskaya M, Chen Q, Schmid TM (1998) Type X collagen and other up-regulated components of the avian hypertrophic cartilage program. Prog Nucleic Acid Res Mol Biol 60:79–109
Zizak I, Roschger P, Paris O, Misof BM, Berzlanovich A, Bernstorff S, Amenitsch H, Klaushofer K, Fratzl P (2003) Characteristics of mineral particles in the human bone/cartilage interface. J Struct Biol 141:208–217
Chatzistavrou X, Rao RR, Caldwell DJ, Peterson AW, McAlpin B, Wang YY, Zheng L, Fenno JC, Stegemann JP, Papagerakis P (2015) Collagen/fibrin microbeads as a delivery system for Ag-doped bioactive glass and DPSCs for potential applications in dentistry. J Non-Cryst Solids. doi:10.1016/j.jnoncrysol.2015.03.024
Shin SR, Aghaei-Ghareh-Bolagh B, Dang TT, Topkaya SN, Gao X, Yang SY, Jung SM, Oh JH, Dokmeci MR, Tang X, Khademhosseini A (2013) Cell-laden microengineered and mechanically tunable hybrid hydrogels of gelatin and graphene oxide. Adv Mater 25:6385–6391
Shin SR, Bae H, Cha JM, Mun JY, Chen YC, Tekin H, Shin H, Farshchi S, Dokmeci MR, Tang S, Khademhosseini A (2012) Carbon nanotube reinforced hybrid microgels as scaffold materials for cell encapsulation. ACS Nano 6:362–372
Shin SR, Jung SM, Zalabany M, Kim K, Zorlutuna P, Kim SB, Nikkah M, Khabiry M, Azize M, Kong J, Wan KT, Palacios T, Dokmeci MR, Bae H, Tang X, Khademhosseini A (2013) Carbon-nanotube-embedded hydrogel sheets for engineering cardiac constructs and bioactuators. ACS Nano 7:2369–2380
Weaver JD, Stabler CL (2015) Antioxidant cerium oxide nanoparticle hydrogels for cellular encapsulation. Acta Biomater 16:136–144
Ciriza J, del Burgo S, Virumbrales-Muñoz LM, Ochoa I, Fernandez LJ, Orive G, Hernandez MR, Pedraz JL (2015) Graphene oxide increases the viability of C2C12 myoblasts microencapsulated in alginate. Int J Pharm 493:260–270
Derby B (2012) Printing and prototyping of tissues and scaffolds. Science 338:921–926
Fedorovich NE, Schuurman W, Wijnberg HM, Prins HJ, van Weeren PR, Malda J, Alblas J, Dhert WJA (2012) Biofabrication of osteochondral tissue equivalents by printing topologically defined, cell-laden hydrogel scaffolds. Tissue Eng Part C Methods 18:33–44
Kolesky DB, Truby RL, Gladman AS, Busbee TA, Homan KA, Lewis JA (2014) 3D bioprinting of vascularized, heterogeneous cell-laden tissue constructs. Adv Mater 26:3124–3130
Luo Y, Wu C, Lode A, Gelinsky M (2013) Hierarchical mesoporous bioactive glass/alginate composite scaffolds fabricated by three-dimensional plotting for bone tissue engineering. Biofabrication 5:015005
Sun JY, Zhao X, Illeperuma WRK, Chaudhuri O, Oh KH, Mooney DJ, Vlassak JJ, Suo Z (2012) Highly stretchable and tough hydrogels. Nature 489:133–136
Wüst S, Godla ME, Müller R, Hofmann S (2014) Tunable hydrogel composite with two-step processing in combination with innovative hardware upgrade for cell-based three-dimensional bioprinting. Acta Biomater 10:630–640
Lewis JA (2008) Novel inks for direct-write assembly of 3-D periodic structures. Mater Matters 3:4–7
Wang X, Tolba E, Schröder HC, Neufurth M, Feng Q, Diehl-Seifert B, Müller WEG (2014) Effect of bioglass on growth and biomineralization of SaOS-2 cells in hydrogel after 3D cell bioprinting. PLoS One 9:e112497
Lee HJ, Kim YB, Kim SH, Kim GH (2014) Mineralized biomimetic collagen/alginate/silica composite scaffolds fabricated by a low-temperature bio-plotting process for hard tissue regeneration: fabrication, characterisation and in vitro cellular activities. J Mater Chem B 2:5785–5798
Hench LL, Jones J (2005) Biomaterials. Woodhead Publishing, Artificial Organs and Tissue Engineering
Lee EJ, Shin DS, Kim HE, Kim HW, Koh YH, Jang JH (2009) Membrane of hybrid chitosan–silica xerogel for guided bone regeneration. Biomaterials 30:743–750
Ozawa S, Kasugai S (1996) Evaluation of implant materials (hydroxyapatite, glass-ceramics, titanium) in rat bone marrow stromal cell culture. Biomaterials 17:23–29
Luo Y, Lode A, Sonntag F, Nies B, Gelinsky M (2013) Well-ordered biphasic calcium phosphate-alginate scaffolds fabricated by multi-channel 3D plotting under mild conditions. J Mater Chem B 1:4088–4098
Luo Y, Lode A, Akkineni AR, Gelinsky M (2015) Concentrated gelatin/alginate composites for fabrication of predesigned scaffolds with a favorable cell response by 3D plotting. RSC Adv 5:43480–43488
Gao G, Schilling AF, Yonezawa T, Wang J, Dai G, Cui X (2014) Bioactive nanoparticles stimulate bone tissue formation in bioprinted three-dimensional scaffold and human mesenchymal stem cells. Biotechnol J 9:1304–1311
Wilson J, Pigott GH, Schoen FJ, Hench LL (1981) Toxicology and biocompatibility of bioglasses. J Biomed Mater Res 15:805–817
Stevens B, Yang Y, Mohandas A, Stucker B, Nguyen KT (2008) A review of materials, fabrication methods, and strategies used to enhance bone regeneration in engineered bone tissue. J Biomed Mater Res B 85:573–582
Kretlow JD, Klouda L, Mikos AG (2007) Injectable matrices and scaffolds for drug delivery in tissue engineering. Adv Drug Deliv Rev 59:263–273
Mano JF, Sousa RA, Boesel LF, Neves NM, Reis RL (2004) Bioinert, biodegradable and injectable polymeric matrix composites for hard tissue replacement: state of the art and recent developments. Compos Sci Technol 64:789–817
Sun F, Zhang WB, Mahdavi A, Arnold FH, Tirrell DA (2014) Synthesis of bioactive protein hydrogels by genetically encoded SpyTag-SpyCatcher chemistry. Proc Natl Acad Sci USA 5:11269–11274
Desai RM, Koshy ST, Hilderbrand SA, Mooney DJ, Joshi NS (2015) Versatile click alginate hydrogels crosslinked via tetrazine-norbornene chemistry. Biomaterials 50:30–37
Elisseeff J (2004) Injectable cartilage tissue engineering. Expert Opin Biol Ther 4:1849–1859
Haines-Butterick L, Rajagopal K, Branco M, Salick D, Rughani R, Pilarz M, Lamm MS, Pochan DJ, Schneider JP (2007) Controlling hydrogelation kinetics by peptide design for three-diemensional encapsulation and injectable delivery of cells. Proc Natl Acad Sci USA 104:7791–7796
Hou Q, De Bank PA, Shakesheff KM (2004) Injectable scaffolds for tissue engineering. J Mater Chem 14:1915–1923
Chen JP, Tsaia MJ, Liao HT (2013) Incorporation of biphasic calcium phosphate microparticles in injectable thermoresponsive hydrogel modulates bone cell proliferation and differentiation. Colloids Surf B 110:120–129
Gauthier O, Khairoun I, Bosco J, Obadia L, Bourges X, Rau C, Magne D, Bouler JM, Aguado E, Daculsi G, Weiss P (2003) Noninvasive bone replacement with a new injectable calcium phosphate biomaterial. J Biomed Mater Res A 66:47–54
Gaharwar AK, Dammu SA, Canter JM, Wu CJ, Schmidt G (2011) Highly extensible, tough, and elastomeric nanocomposite hydrogels from poly(ethylene glycol) and hydroxyapatite nanoparticles. Biomacromolecules 12:1641–1650
Song J, Xu J, Filion T, Saiz E, Tomsia AP, Lian JB, Stein GS, Ayers DC, Bertozzi CR (2009) Elastomeric high-mineral content hydrogel-hydroxyapatite composites for orthopedic applications. J Biomed Mater Res A 15:1098–1107
Fu SZ, Guo G, Gong CY, Zeng S, Liang H, Luo F, Zhang XN, Zhao X, Wei YQ, Qian ZY (2009) Injectable biodegradable thermosensitive hydrogel composite for orthopedic tissue engineering. 1. Preparation and characterization of nanohydroxyapatite/poly(ethylene glycol)-poly(ε-caprolactone)-poly(ethylene glycol) hydrogel nanocomposites. J Phys Chem B 113:16518–16525
Fan RR, Deng XH, Zhou LX, Gao X, Fan M, Wang YL, Guo G (2014) Injectable thermosensitve hydrogel composite with surface-functionalized calcium phosphate as raw materials. Int J Nanomed 9:615–626
Ni PY, Fan M, Qian ZY, Luo JC, Gong CY, Fu SZ, Shi S, Luo F, Yang ZM (2012) Synthesis and characterization of injectable, thermosensitive, and biocompatible acellular bone matrix/poly(ethylene glycol)-poly(ε-caprolactone)-poly(ethylene glycol) hydrogel composite. J Biomed Mater Res A 100:171–179
Fu SZ, Ni PY, Wang BY, Chu BY, Zheng L, Luo F, Luo JC, Qian ZY (2012) Injectable and thermo-sensitive PEG-PCL-PEG copolymer/collagen/n-HA hydrogel composite for guided bone regeneration. Biomaterials 33:4801–4809
Sarvestani AS, Jabbari E (2006) Modeling and experimental investigation of rheological properties of injectable poly(lactide ethylene oxide fumarate)/hydroxyapatite nanocomposites. Biomacromolecules 7:1573–1580
Lai MC, Chang KC, Hsu SC, Chou MC, Hung WI, Hsiao YR, Lee HM, Hsieh MF, Yeh JM (2014) In situ gelation of PEG-PLGA-PEG hydrogels containing high loading of hydroxyapatite: in vitro and in vivo characterization. Biomed Mater 9:015011
Miller RA, Brady JM, Cutright ED (1977) Degradation rates of oral resorbable implants (polylactates and polyglycolates): rate modification with changes in PLA/PGA copolymer ratios. J Biomed Mater Res 11:711–719
Li SM, Garreau H, Vert M (1990) Structure-property relationship in the case of the degradation of massive poly(α-hydroxy acids) in aqueous media. J Mater Sci 3:131–139. doi:10.1007/BF00700871
Daculsi G, Weiss P, Bouler JM, Gauthier O, Millot F, Aguado E (1999) Biphasic calcium phosphate/hydrosoluble polymer composites: a new concept for bone and dental substitution biomaterials. Bone 25:59S–61S
Gauthier O, Bouler JM, Weiss P, Bosco J, Aguado E, Daculsi G (1999) Short-term effect of mineral particle size on cellular degradation activity after implantation of injectable calcium phosphate biomaterials and the consequences for bone substitution. Bone 25:71S–74S
Gauthier O, Boix D, Grimandi G, Aguado E, Bouler JM, Weiss P, Daculsi G (1999) A new injectable calcium phosphate biomaterial for immediate bone filling of extraction sockets: a preliminary study in dogs. J Peridontol 70:375–383
Weiss P, Vinatier C, Guicheux J, Grimandi G, Daculsi G (2004) A self setting hydrogel as an extracellular synthetic matrix for tissue engineering. Key Eng Mater 254–256:1107–1110
Trojani C, Boukhechba F, Scimeca JC, Vandenbos F, Michiels JF, Daculsi G, Boileau P, Weiss P, Carle GF, Rochet N (2006) Ectopic bone formation using an injectable biphasic calcium phosphate/Si-HPMC hydrogel composite loaded with undifferentiated bone marrow stromal cells. Biomaterials 27:3256–3264
Sohier J, Corre P, Weiss P, Layrolle P (2010) Hydrogel/calcium phosphate composites require specific properties for three-dimensional culture of human bone mesenchymal cells. Acta Biomater 6:2932–2939
Weiss P, Vinatier C, Sohier J, Fatimi A, Layrolle P, Demais V, Atmani H, Basle MF, Guicheux J (2008) Self-hardening hydrogel for bone tissue engineering. Macromol Symp 1:30–35
Laib S, Fellah BH, Fatimi A, Quillard S, Vinatier S, Gauthier O, Janvier P, Petit M, Bujoli B, Bohic S, Weiss P (2009) The in vivo degradation of a ruthenium labelled polysaccharide-based hydrogel for bone tissue engineering. Biomaterials 8:1568–1577
Liu W, Zhang J, Rethore G, Khairoun K, Pilet P, Tancret F, Bouler JM, Weiss P (2014) A novel injectable, cohesive and toughened Si-HPMC (silanized-hydroxypropyl methylcellulose) composite calcium phosphate cement for bone substitution. Acta Biomater 10:3335–3345
Moreau JL, Xu HHK (2009) Mesenchymal stem cell proliferation and differentiation on an injectable calcium phosphate–chitosan composite scaffold. Biomaterials 30:2675–2682
Nguyen TP, Doan BHP, Dang DV, Nguyen CK, Tran NQ (2014) Enzyme-mediated in situ preparation of biocompatible hydrogel composites from chitosan derivative and biphasic calcium phosphate nanoparticles for bone regeneration. Adv Nat Sci: Nanosci Nanotechnol 5:015012
Anselme K (2000) Osteoblast adhesion on biomaterials. Biomaterials 21:667–681
Douglas TEL, Piwowarczyk W, Pamula E, Liskova J, Schaubroeck D, Leeuwenburgh SCG, Brackman G, Balcaen L, Detsch R, Declercq H, Cholewa-Kowalska K, Dokupil A, Cuijpers VMJI, Vanhaecke F, Cornelissen R, Coenye T, Boccaccini AR, Dubruel P (2014) Injectable self-gelling composites for bone tissue engineering based on gellan gum hydrogel enriched with different bioglasses. Biomed Mater 9:045014
Gorriti MF, Lopez JMP, Boccaccini AR, Audisio C, Gorustovich AA (2009) In vitro study of the antibacterial activity of bioactive glass-ceramic scaffolds. Adv Eng Mater 11:B67–B70
Hu S, Chang J, Liu MQ, Ning CQ (2009) Study on antibacterial effect of 45S5 bioglass. J Mater Sci Mater Med 20:281–286
Hum J, Boccaccini AR (2012) J Mater Sci Mater Med 23:2317–2333
Maeno S, Niki Y, Matsumoto H, Morioka H, Yatabe T, Funayama A, Toyama Y, Taguchi T, Tanaka J (2005) The effect of calcium ion concentration on osteoblast viability, proliferation and differentiation in monolayer and 3D culture. Biomaterials 26:4847–4855
Fedorovich NE, Leeuwenburgh SC, van der Helm YJM, Alblas J, Dhert WJA (2012) The osteoinductive potential of printable, cell-laden hydrogel-ceramic composites. J Biomed Mater Res A 100:2412–2420
Campbell SB, Patenaude M, Hoare T (2013) Injectable superparamagnets: highly elastic and degradable poly(N-isopropylacrylamide)–superparamagnetic iron oxide nanoparticle (SPION) composite hydrogels. Biomacromolecules 14:644–653
Na K, Kim SW, Sun BK, Woo DG, Yang HN, Chung HM, Park KH (2007) Osteogenic differentiation of rabbit mesenchymal stem cells in thermo-reversible hydrogel constructs containing hydroxyapatite and bone morphogenic protein-2 (BMP-2). Biomaterials 28:2631–2637
Wren AW, Hassanzadeh P, Placek LM, Keenan TJ, Coughlan A, Boutelle LR, Towler MR (2015) Silver nanoparticle coated bioactive glasses – composites with dex/CMC hydrogels: characterization, solubility and in vitro biological studies. Macromol Biosci 15:1146–1158
Yang X, Yang W, Wang Q, Li H, Wang K, Yang L, Liu W (2010) Atomic force microscopy investigation of the characteristic effects of silver ions on Escherichia coli and Staphylococcus epidermidis. Talanta 81:1508–1512
Sahu A, Choi WI, Tae G (2012) A stimuli-sensitive injectable graphene oxide composite hydrogel. Chem Commun 48:5820–5822
Satarkar NS, Biswal D, Hilt JZ (2010) Hydrogel nanocomposites: a review of applications as remote controlled biomaterials. Soft Matter 6:2364–2371
Gil S, Mano JF (2014) Magnetic composite biomaterials for tissue engineering. Biomater Sci 2:812–818
Jung Y, Kim JK, Shiozawa Y, Wang J, Mishra A, Joseph J, Berry JE, McGee S, Lee E, Sun H, Wang J, Jin T, Zhang H, Dai J, Krebsbach PH, Keller ET, Pienta KJ, Taichman RS (2013) Recruitment of mesenchymal stem cells into prostate tumours promotes metastasis. Nat Commun 4:1795
Tajiri N, Kaneko Y, Shinozuka K, Ishikawa H, Yankee E, McGrogan M, Case C, Borlongan CV (2013) Stem cell recruitment of newly formed host cells via a successful seduction? Filling the gap between neurogenic niche and injured brain site. PLoS One 8:e74857
Galano A (2008) Carbon nanotubes as free-radical scavengers. J Phys Chem C 112:8922–8927
Kafi MA, El-Said WA, Kim TH, Choi JW (2011) Cell adhesion, spreading, and proliferation on surface functionalized with RGD nanopillar arrays. Biomaterials 33:731–739
Baik KY, Park SY, Heo K, Lee KB, Hong S (2011) Carbon nanotube monolayer cues for osteogenesis of mesenchymal stem cells. Small 7:741–745
Namgung S, Kim T, Baik KY, Lee M, Nam JM, Hong S (2011) Fibronectin carbon nanotube hybrid nanostructures for controlled cell growth. Small 7:56–61
Boanini E, Torricelli P, Fini M, Sima F, Serban N, Mihailescu IN, Bigi A (2012) Magnesium and strontium doped octacalcium phosphate thin films by matrix assisted pulsed laser evaporation. J Inorg Biochem 107:65–72
Bracci B, Torricelli P, Panzavolta S, Boanini E, Giardino R, Bigi A (2009) Effect of Mg2+, Sr2+, and Mn2+ on the chemico-physical and in vitro biological properties of calcium phosphate biomimetic coatings. J Inorg Biochem 103:1666–1674
Sader MS, Legeros RZ, Soares GA (2009) Human osteoblasts adhesion and proliferation on magnesium-substituted tricalcium phosphate dense tablets. J Mater Sci Mater Med 20:521–527
Acknowledgements
S.U. would like to thank the Deutsche Forschungsgemeinschaft (DFG) for their financial support. The authors thank B. Sarker and T. Zehnder (the Institute of Biomaterials, The University of Erlangen-Nuremberg) for stimulating discussions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Utech, S., Boccaccini, A.R. A review of hydrogel-based composites for biomedical applications: enhancement of hydrogel properties by addition of rigid inorganic fillers. J Mater Sci 51, 271–310 (2016). https://doi.org/10.1007/s10853-015-9382-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10853-015-9382-5