Abstract
Purpose
This study sought to identify risk factors for permanent pacemaker implantation (PPMI) after Transcatheter aortic valve implantation (TAVI) and explain their trends over the last decade. TAVI is performed nowadays for severe aortic stenosis in more patients with lower surgical risk. While most TAVI complications have been reduced, PPMI remains common.
Methods
In this observational, retrospective cohort analysis, 338 TAVI patients treated between 2008 and 2017 were reviewed. Risk factors were compared between the early (2008–2013) and late years (2014–2017), and a multivariable logistic regression model was used.
Results
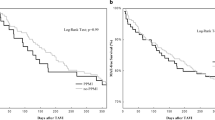
A decreasing trend in PPMI over time was observed (p for trend = 0.008), as was a lower rate of PPMI in the late period (19.3% vs. 31.7%, p = 0.009). Three variables were identified as independent risk factors for PPMI that also decreased significantly in the late period: valve implantation depth ≥ 8 mm (OR = 4.3, 95% CI 2.3–8.2, p < 0.001), use of self-expandable valves (OR = 2.8, 95% CI 1.4–5.5, p = 0.004), and patient risk assessed by EuroSCORE II (OR = 1.07, 95% CI 1.0–1.1, p = 0.034). Indications for PPMI were also shown to change over time, with an increase in the prevalence of complete AVB as the main indication for PPMI (p = 0.048), and a trend towards a decrease in LBBB alone (p = 0.061).
Conclusions
The decrease in post-TAVI PPMI over the past decade is multifactorial and can be explained by (1) lower baseline patient surgical risk, (2) modified procedural variables including decreased implantation depth and increased use of balloon-expandable valves, and (3) refined indications for PPMI.





Similar content being viewed by others
Abbreviations
- AVR:
-
Aortic valve replacement
- AVB:
-
Atrioventricular block
- COPD:
-
Chronic obstructive pulmonary disease
- EF:
-
Ejection fraction
- LAHB:
-
Left anterior hemiblock
- LBBB:
-
Left bundle branch block
- LVOT:
-
Left ventricular outlet tract
- NYHA:
-
New York Heart Association
- PPMI:
-
Permanent pacemaker implantation
- RBBB:
-
Right bundle branch block
- STS:
-
Society of Thoracic Surgeons
- TAVI:
-
Transcatheter aortic valve implantation
- VARC2:
-
Valve Academic Research Consortium-2
References
Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364(23):2187–98.
Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363(17):1597–607.
Leon MB, Smith CR, Mack MJ, Makkar RR, Svensson LG, Kodali SK, et al. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2016;374(17):1609–20.
Reardon MJ, Van Mieghem NM, Popma JJ. Surgical or transcatheter aortic-valve replacement. N Engl J Med. 2017;377(2):197–8.
Siontis GC, Praz F, Pilgrim T, Mavridis D, Verma S, Salanti G, et al. Transcatheter aortic valve implantation vs. surgical aortic valve replacement for treatment of severe aortic stenosis: a meta-analysis of randomized trials. Eur Heart J. 2016;37(47):3503–12.
Thourani VH, Kodali S, Makkar RR, Herrmann HC, Williams M, Babaliaros V, et al. Transcatheter aortic valve replacement versus surgical valve replacement in intermediate-risk patients: a propensity score analysis. Lancet. 2016;387(10034):2218–25.
Falk V, Baumgartner H, Bax JJ, De Bonis M, Hamm C, Holm PJ, et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur J Cardiothorac Surg. 2017;52(4):616–64.
Anantha-Narayanan M, Kandasamy VV, Reddy YN, Megaly M, Baskaran J, Pershad A, et al. Low-risk transcatheter versus surgical aortic valve replacement-an updated meta-analysis of randomized controlled trials. Cardiovasc Revasc Med. 2019.
Kolte D, Vlahakes GJ, Palacios IF, Sakhuja R, Passeri JJ, Inglessis I, et al. Transcatheter versus surgical aortic valve replacement in low-risk patients. J Am Coll Cardiol. 2019;74(12):1532–40.
Giannini C, De Carlo M, Tamburino C, Ettori F, Latib AM, Bedogni F, et al. Transcathether aortic valve implantation with the new repositionable self-expandable Evolut R versus CoreValve system: a case-matched comparison. Int J Cardiol. 2017;243:126–31.
Thyregod HG, Steinbruchel DA, Ihlemann N, Nissen H, Kjeldsen BJ, Petursson P, et al. Transcatheter versus surgical aortic valve replacement in patients with severe aortic valve stenosis: 1-year results from the all-comers NOTION randomized clinical trial. J Am Coll Cardiol. 2015;65(20):2184–94.
Rodes-Cabau J, Ellenbogen KA, Krahn AD, Latib A, Mack M, Mittal S, et al. Management of conduction disturbances associated with transcatheter aortic valve replacement: JACC scientific expert panel. J Am Coll Cardiol. 2019;74(8):1086–106.
Barbanti M, Buccheri S, Rodes-Cabau J, Gulino S, Genereux P, Pilato G, et al. Transcatheter aortic valve replacement with new-generation devices: a systematic review and meta-analysis. Int J Cardiol. 2017;245:83–9.
Al-Ogaili A, Fugar S, Okoh A, Kolkailah AA, Al Hashemi N, Ayoub A, et al. Trends in complete heart block after transcatheter aortic valve replacement: a population based analysis. Catheter Cardiovasc Interv. 2019;94:773–80.
Auffret V, Puri R, Urena M, Chamandi C, Rodriguez-Gabella T, Philippon F, et al. Conduction disturbances after transcatheter aortic valve replacement: current status and future perspectives. Circulation. 2017;136(11):1049–69.
Auffret V, Lefevre T, Van Belle E, Eltchaninoff H, Iung B, Koning R, et al. Temporal trends in transcatheter aortic valve replacement in France: FRANCE 2 to FRANCE TAVI. J Am Coll Cardiol. 2017;70(1):42–55.
Landes U, Barsheshet A, Finkelstein A, Guetta V, Assali A, Halkin A, et al. Temporal trends in transcatheter aortic valve implantation, 2008-2014: patient characteristics, procedural issues, and clinical outcome. Clin Cardiol. 2017;40(2):82–8.
Mauri V, Reimann A, Stern D, Scherner M, Kuhn E, Rudolph V, et al. Predictors of permanent pacemaker implantation after transcatheter aortic valve replacement with the SAPIEN 3. JACC Cardiovasc Interv. 2016;9(21):2200–9.
Becker M, Blangy H, Folliguet T, Villemin T, Freysz L, Luc A, et al. Incidence, indications and predicting factors of permanent pacemaker implantation after transcatheter aortic valve implantation: a retrospective study. Arch Cardiovasc Diseases. 2017;110(10):508–16.
Naveh S, Perlman GY, Elitsur Y, Planer D, Gilon D, Leibowitz D, et al. Electrocardiographic predictors of long-term cardiac pacing dependency following transcatheter aortic valve implantation. J Cardiovasc Electrophysiol. 2017;28(2):216–23.
Siontis GC, Juni P, Pilgrim T, Stortecky S, Bullesfeld L, Meier B, et al. Predictors of permanent pacemaker implantation in patients with severe aortic stenosis undergoing TAVR: a meta-analysis. J Am Coll Cardiol. 2014;64(2):129–40.
Al-Abdouh A, Upadhrasta S, Fashanu O, Elias H, Zhao D, Hasan RK, et al. Transcatheter aortic valve replacement in low-risk patients: a meta-analysis of randomized controlled trials. Cardiovasc Revasc Med 2019.
Adams DH, Popma JJ, Reardon MJ. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med. 2014;371(10):967–8.
Mack MJ, Leon MB, Thourani VH, Makkar R, Kodali SK, Russo M, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med. 2019;380(18):1695–705.
Nashef SA, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR, et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012;41(4):734–44 discussion 44-5.
Rosa VE, Lopes AS, Accorsi TA, Fernandes JR, Spina GS, Sampaio RO, et al. EuroSCORE II and STS as mortality predictors in patients undergoing TAVI. Rev Assoc Med Bras (1992). 2016;62(1):32–7.
Kappetein AP, Head SJ, Genereux P, Piazza N, van Mieghem NM, Blackstone EH, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. J Am Coll Cardiol. 2012;60(15):1438–54.
Popma JJ, Adams DH, Reardon MJ, Yakubov SJ, Kleiman NS, Heimansohn D, et al. Transcatheter aortic valve replacement using a self-expanding bioprosthesis in patients with severe aortic stenosis at extreme risk for surgery. J Am Coll Cardiol. 2014;63(19):1972–81.
Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O’Hair D, et al. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med. 2019;380(18):1706–15.
Ojeda S, Hidalgo F, Romero M, Mazuelos F, Suarez de Lezo J, Martin E, et al. Impact of the repositionable Evolut R CoreValve system on the need for a permanent pacemaker after transcatheter aortic valve implantation in patients with severe aortic stenosis. Catheter Cardiovasc Interv. 2019.
Kowalewski M, Gozdek M, Raffa GM, Slomka A, Zielinski K, Kubica J, et al. Transcathether aortic valve implantation with the new repositionable self-expandable Medtronic Evolut R vs. CoreValve system: evidence on the benefit of a meta-analytical approach. J Cardiovasc Med (Hagerstown). 2019;20(4):226–36.
Manoharan G, Van Mieghem NM, Windecker S, Bosmans J, Bleiziffer S, Modine T, et al. 1-year outcomes with the Evolut R self-expanding transcatheter aortic valve: from the international FORWARD study. JACC Cardiovasc Interv. 2018;11(22):2326–34.
Abdel-Wahab M, Mehilli J, Frerker C, Neumann FJ, Kurz T, Tolg R, et al. Comparison of balloon-expandable vs self-expandable valves in patients undergoing transcatheter aortic valve replacement: the CHOICE randomized clinical trial. JAMA. 2014;311(15):1503–14.
Makkar RR, Jilaihawi H, Chakravarty T, Fontana GP, Kapadia S, Babaliaros V, et al. Determinants and outcomes of acute transcatheter valve-in-valve therapy or embolization: a study of multiple valve implants in the U.S. PARTNER trial (Placement of AoRTic TraNscathetER Valve Trial Edwards SAPIEN Transcatheter Heart Valve). J Am Coll Cardiol. 2013;62(5):418–30.
Khawaja MZ, Rajani R, Cook A, Khavandi A, Moynagh A, Chowdhary S, et al. Permanent pacemaker insertion after CoreValve transcatheter aortic valve implantation: incidence and contributing factors (the UK CoreValve Collaborative). Circulation. 2011;123(9):951–60.
Sager SJ, Damluji AA, Cohen JA, Shah S, O’Neill BP, Alfonso CE, et al. Transient and persistent conduction abnormalities following transcatheter aortic valve replacement with the Edwards-Sapien prosthesis: a comparison between antegrade vs. retrograde approaches. J Interv Card Electrophysiol. 2016;47(2):143–51.
van der Boon RM, Van Mieghem NM, Theuns DA, Nuis RJ, Nauta ST, Serruys PW, et al. Pacemaker dependency after transcatheter aortic valve implantation with the self-expanding Medtronic CoreValve System. Int J Cardiol. 2013;168(2):1269–73.
Urena M, Mok M, Serra V, Dumont E, Nombela-Franco L, DeLarochelliere R, et al. Predictive factors and long-term clinical consequences of persistent left bundle branch block following transcatheter aortic valve implantation with a balloon-expandable valve. J Am Coll Cardiol. 2012;60(18):1743–52.
Houthuizen P, Van Garsse LA, Poels TT, de Jaegere P, van der Boon RM, Swinkels BM, et al. Left bundle-branch block induced by transcatheter aortic valve implantation increases risk of death. Circulation. 2012;126(6):720–8.
Nazif TM, Chen S, George I, Dizon JM, Hahn RT, Crowley A, et al. New-onset left bundle branch block after transcatheter aortic valve replacement is associated with adverse long-term clinical outcomes in intermediate-risk patients: an analysis from the PARTNER II trial. Eur Heart J. 2019;40(27):2218–27.
Alqarawi W, Sadek MM, Golian M, Hibbert B, Redpath CJ, Nair GM, Nery PB, Davis DR, Klein A, Birnie DH, Green MS A new electrocardiographic definition of left bundle branch block (LBBB) in patients after transcatheter aortic valve replacement (TAVR). J Electrocardiol 2019.
Tovia-Brodie O, Ben-Haim Y, Joffe E, Finkelstein A, Glick A, Rosso R, et al. The value of electrophysiologic study in decision-making regarding the need for pacemaker implantation after TAVI. J Interv Card Electrophysiol. 2017;48(2):121–30.
Schernthaner C, Kraus J, Danmayr F, Hammerer M, Schneider J, Hoppe UC, et al. Short-term pacemaker dependency after transcatheter aortic valve implantation. Wien Klin Wochenschr. 2016;128(5–6):198–203.
Mirolo A, Viart G, Durand E, Savoure A, Godin B, Auquier N, et al. Pacemaker memory in post-TAVI patients: who should benefit from permanent pacemaker implantation? Pacing Clin Electrophysiol. 2018;41(9):1178–84.
Rodes-Cabau J, Urena M, Nombela-Franco L, Amat-Santos I, Kleiman N, Munoz-Garcia A, et al. Arrhythmic burden as determined by ambulatory continuous cardiac monitoring in patients with new-onset persistent left bundle branch block following transcatheter aortic valve replacement: the MARE study. JACC Cardiovasc Interv. 2018;11(15):1495–505.
Faroux L, Chen S, Muntane-Carol G, Regueiro A, Philippon F, Sondergaard L, et al. Clinical impact of conduction disturbances in transcatheter aortic valve replacement recipients: a systematic review and meta-analysis. Eur Heart J. 2020;41:2771–81.
Author information
Authors and Affiliations
Contributions
Rotem Eliav: conceptualization, methodology, writing—original draft; Yair Elitzur: investigation; David Planer: investigation; Ronen Beeri: investigation; Dan Gilon: investigation; Mony Shuvy: investigation; David Luria: investigation; Haim Danenberg: investigation, writing—review and editing; Gidon Y. Perlman: conceptualization, supervision, investigation, writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics approval
All patients gave written informed consent for treatment and data collection, and the study was approved by the Hadassah Medical Center Institutional Review Board. The procedures used in this study adhere to the tenets of the declaration of Helsinki.
Consent to participate
Informed consent was obtained from all induvial participants included in the study.
Consent for publication
Informed consent was obtained from all induvial participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Eliav, R., Elitzur, Y., Planer, D. et al. Predictors for permanent pacemaker implantation following transcatheter aortic valve implantation: trends over the past decade. J Interv Card Electrophysiol 62, 299–307 (2021). https://doi.org/10.1007/s10840-020-00902-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-020-00902-y