Abstract
Purpose
The purpose of this study was to evaluate electrophysiologic study (EPS) in risk stratification of relative indications for pacemaker implantation (PMI) after transcatheter aortic valve implantation (TAVI).
Methods
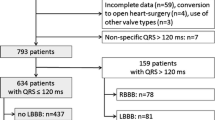
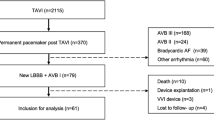
We reviewed files of all patients who had a left bundle branch block (LBBB) and underwent EPS after TAVI between 3/2009 and 5/2015. The indications for EPS were new-onset LBBB and the presence of an old or a new-onset LBBB associated with either PR prolongation after TAVI (∆PR >20 ms) or with “slow” atrial fibrillation (<100/min). Pacemakers were implanted when significant infranodal disease was demonstrated. The control group comprised of 55 consecutive patients who underwent TAVI and had an indication for an EPS per our definitions. These patients were discharged without further intervention. All patients were followed during 1 year for the composite endpoint of mortality or PMI after hospital discharge.
Results
Indications for EPS were new LBBB (n = 8, 30.8%), new LBBB + ∆PR >20 ms (n = 9, 34.6%), baseline LBBB + ∆PR >20 ms (n = 7, 26.9%) and new LBBB + slow AF <100 bpm (n = 2, 7.7%). Multilevel conduction disturbances involving the AV node (n = 19, 73.1%), the His (n = 3, 11.5%), and the infra-His system (n = 4, 15.4%) were found. Post discharge, there were 5 (9%) deaths and 3 (5.5%) PMI in the control group compared to none in the EPS group corresponding to event-free survival of 85 and 100%, respectively (p = 0.04).
Conclusions
Patients with LBBB with or without ∆PR >20 ms are at a higher risk of mortality and late PMI at 1-year follow-up. EPS can be used to safely identify patients in whom a PMI is needed.






Similar content being viewed by others
References
Cribier A et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description, (in eng). Circulation. 2002;106(24):3006–8.
van der Boon RM et al. New conduction abnormalities after TAVI—frequency and causes, (in eng). Nat Rev Cardiol. 2012;9(8):454–63.
van der Boon RM et al. Pacemaker dependency after transcatheter aortic valve implantation with the self-expanding Medtronic CoreValve System, (in eng). Int J Cardiol. 2013;168(2):1269–73.
Urena M et al. Predictive factors and long-term clinical consequences of persistent left bundle branch block following transcatheter aortic valve implantation with a balloon-expandable valve, (in eng). J Am Coll Cardiol. 2012;60(18):1743–52.
Bjerre Thygesen J, Loh PH, Cholteesupachai J, Franzen O, Sondergaard L. Reevaluation of the indications for permanent pacemaker implantation after transcatheter aortic valve implantation, (in eng). J Invasive Cardiol. 2014;26(2):94–9.
Urena M et al. Impact of new-onset persistent left bundle branch block on late clinical outcomes in patients undergoing transcatheter aortic valve implantation with a balloon-expandable valve, (in eng). JACC Cardiovasc Interv. 2014;7(2):128–36.
Salizzoni S et al. One-year follow-up of conduction disturbances following transcatheter aortic valve implantation, (in eng). J Cardiovasc Med (Hagerstown). 2015;16(4):296–302.
Brignole M et al. 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA), (in eng). Europace. 2013;15(8):1070–118.
Leon MB et al. Standardized endpoint definitions for transcatheter aortic valve implantation clinical trials: a consensus report from the Valve Academic Research Consortium, (in eng). Eur Heart J. 2011;32(2):205–17.
Akin I et al. Predictive factors for pacemaker requirement after transcatheter aortic valve implantation, (in eng). BMC Cardiovasc Disord. 2012;12:87.
Ramazzina C et al. Pacemaker implantation and need for ventricular pacing during follow-up after transcatheter aortic valve implantation, (in eng). Pacing Clin Electrophysiol. 2014;37(12):1592–601.
Surawicz B et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology, (in eng). J Am Coll Cardiol. 2009;53(11):976–81.
Kappetein AP et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document, (in eng). J Am Coll Cardiol. 2012;60(15):1438–54.
O. Tovia-Brodie, Y. Michowitz, M. Rahkovich, and B. Belhassen, QRS normalization during atrial pacing in a patient with complete left bundle branch block: What is your diagnosis?, HeartRhythm Case Reports, vol. 1, no. 5, pp. 320–322.
Kostopoulou A et al. Permanent pacing after transcatheter aortic valve implantation of a CoreValve prosthesis as determined by electrocardiographic and electrophysiological predictors: a single-centre experience, (in eng). Europace. 2016;18(1):131–7.
Rivard L et al. Electrocardiographic and electrophysiological predictors of atrioventricular block after transcatheter aortic valve replacement, (in eng). Heart Rhythm. 2015;12(2):321–9.
R. Moreno et al., Cause of complete atrioventricular block after percutaneous aortic valve implantation: insights from a necropsy study, in Circulation, vol. 120no. 5) United States, 2009, pp. e29-30.
Kawashima T, Sato F. Visualizing anatomical evidences on atrioventricular conduction system for TAVI, (in eng). Int J Cardiol. 2014;174(1):1–6.
Piazza N et al. Early and persistent intraventricular conduction abnormalities and requirements for pacemaking after percutaneous replacement of the aortic valve, (in eng). JACC Cardiovasc Interv. 2008;1(3):310–6.
Sovari AA, Shehata M. Heart block following transcatheter aortic valve implantation: a matter of right bundle branch integrity? (in eng). Expert Rev Cardiovasc Ther. 2016;14(6):663–5.
ME Josephson. Clinical Cardiac Electrophysiology. Techniques and Interpretations. Third Edition. Lippincot Williams $ Wilkins, 2002, p 132.
Haworth P et al. Predictors for permanent pacing after transcatheter aortic valve implantation, (in eng). Catheter Cardiovasc Interv. 2010;76(5):751–6.
De Torres-Alba F et al. Changes in the pacemaker rate after transition from Edwards SAPIEN XT to SAPIEN 3 Transcatheter Aortic Valve Implantation: the critical role of valve implantation height, (in eng). JACC Cardiovasc Interv. 2016;9(8):805–13.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent was obtained from all individual participants included in the study, and the study was approved by the Institutional Ethics Committee.
Funding
There was no funding for this study.
Conflict of interest
Dr. Finkelstein acts as a TAVI proctor and receives consultation fees from Medtronic cardiovascular (Minneapolis, Minnesota) and Edwards Lifesciences (Irvine, California). All other authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Tovia-Brodie, O., Ben-Haim, Y., Joffe, E. et al. The value of electrophysiologic study in decision-making regarding the need for pacemaker implantation after TAVI. J Interv Card Electrophysiol 48, 121–130 (2017). https://doi.org/10.1007/s10840-016-0218-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-016-0218-2