Abstract
Purpose
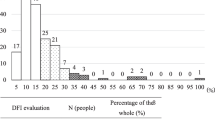
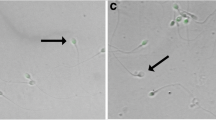
The sperm DNA fragmentation index (DFI) was quantitatively measured and its relationship with age, semen quality, and infertility conditions was investigated.
Methods
Semen routine test and sperm DFI were performed in 2760 infertile male and 2354 male whose spouse experienced at least one unexplained miscarriage to analyze the correlation between sperm DNA damage, semen routine parameters, and age.
Results
Sperm DFI was significantly lower from patients whose wife experienced unexplained miscarriage compared to infertility males (p = 0.000). An inverse correlation between sperm DFI and sperm progressive motility was observed (rs = − 0.465, p = 0.000) and sperm DFI was positively correlated with age (rs = 0.255, p = 0.000). However, the correlation between sperm DFI and sperm concentration, semen volume, total sperm count, and motile sperm count were not proved.
Conclusions
Sperm DFI is an important indicator for evaluating the quality of semen. Sperm DNA integrity testing is preferentially recommended to those who have decreased sperm progressive motility, especially older men. An integrative analysis of sperm DFI, sperm progressive motility, age, and infertility conditions can provide a more comprehensive assessment of male fertility.
Similar content being viewed by others
References
Pasqualotto FF, Sobreiro BP, Hallak J, Athayde KS, Pasqualotto EB, Lucon AM. High percentage of abnormal semen parameters in a prevasectomy population. Fertil Steril. 2006;85(4):954–60. https://doi.org/10.1016/j.fertnstert.2005.09.032.
Practice Committee of the American Society for Reproductive M. Diagnostic evaluation of the infertile male: a committee opinion. Fertil Steril. 2015;103(3):e18–25. https://doi.org/10.1016/j.fertnstert.2014.12.103.
Cooper TG, Noonan E, von Eckardstein S, Auger J, Baker HW, Behre HM, et al. World Health Organization reference values for human semen characteristics. Hum Reprod Update. 2010;16(3):231–45. https://doi.org/10.1093/humupd/dmp048.
Andersen AG, Ziebe S, Jorgensen N, Petersen JH, Skakkebaek NE, Andersen AN. Time to pregnancy in relation to semen quality assessed by CASA before and after sperm separation. Hum Reprod. 2002;17(1):173–7. https://doi.org/10.1093/humrep/17.1.173.
Buck Louis GM, Sundaram R, Schisterman EF, Sweeney A, Lynch CD, Kim S, et al. Semen quality and time to pregnancy: the Longitudinal Investigation of Fertility and the Environment Study. Fertil Steril. 2014;101(2):453–62. https://doi.org/10.1016/j.fertnstert.2013.10.022.
Santi D, Spaggiari G, Simoni M. Sperm DNA fragmentation index as a promising predictive tool for male infertility diagnosis and treatment management - meta-analyses. Reprod BioMed Online. 2018;37(3):315–26. https://doi.org/10.1016/j.rbmo.2018.06.023.
Panner Selvam MK, Agarwal A. A systematic review on sperm DNA fragmentation in male factor infertility: Laboratory assessment. Arab J Urol. 2018;16(1):65–76. https://doi.org/10.1016/j.aju.2017.12.001.
Agarwal A, Cho CL, Majzoub A, Esteves SC. The Society for Translational Medicine: clinical practice guidelines for sperm DNA fragmentation testing in male infertility. Transl Androl Urol. 2017;6(Suppl 4):S720–S33. https://doi.org/10.21037/tau.2017.08.06.
Oliva R. Protamines and male infertility. Hum Reprod Update. 2006;12(4):417–35. https://doi.org/10.1093/humupd/dml009.
Sakkas D, Alvarez JG. Sperm DNA fragmentation: mechanisms of origin, impact on reproductive outcome, and analysis. Fertil Steril. 2010;93(4):1027–36. https://doi.org/10.1016/j.fertnstert.2009.10.046.
Lu JC, Jing J, Chen L, Ge YF, Feng RX, Liang YJ, et al. Analysis of human sperm DNA fragmentation index (DFI) related factors: a report of 1010 subfertile men in China. Reprod Biol Endocrinol. 2018;16(1):23. https://doi.org/10.1186/s12958-018-0345-y.
Sergerie M, Laforest G, Bujan L, Bissonnette F, Bleau G. Sperm DNA fragmentation: threshold value in male fertility. Hum Reprod. 2005;20(12):3446–51. https://doi.org/10.1093/humrep/dei231.
Schulte RT, Ohl DA, Sigman M, Smith GD. Sperm DNA damage in male infertility: etiologies, assays, and outcomes. J Assist Reprod Genet. 2010;27(1):3–12. https://doi.org/10.1007/s10815-009-9359-x.
Agarwal A, Said TM. Role of sperm chromatin abnormalities and DNA damage in male infertility. Hum Reprod Update. 2003;9(4):331–45. https://doi.org/10.1093/humupd/dmg027.
Robinson L, Gallos ID, Conner SJ, Rajkhowa M, Miller D, Lewis S, et al. The effect of sperm DNA fragmentation on miscarriage rates: a systematic review and meta-analysis. Hum Reprod. 2012;27(10):2908–17. https://doi.org/10.1093/humrep/des261.
Tesarik J, Greco E, Mendoza C. Late, but not early, paternal effect on human embryo development is related to sperm DNA fragmentation. Hum Reprod. 2004;19(3):611–5. https://doi.org/10.1093/humrep/deh127.
Qiu Y, Yang H, Li C, Xu C. Progress in research on sperm DNA fragmentation. Med Sci Monit. 2020;26:e918746. https://doi.org/10.12659/MSM.918746.
Evenson DP, Darzynkiewicz Z, Melamed MR. Relation of mammalian sperm chromatin heterogeneity to fertility. Science. 1980;210(4474):1131–3. https://doi.org/10.1126/science.7444440.
Giwercman A, Lindstedt L, Larsson M, Bungum M, Spano M, Levine RJ, et al. Sperm chromatin structure assay as an independent predictor of fertility in vivo: a case–control study. Int J Androl. 2010;33(1):e221–e7. https://doi.org/10.1111/j.1365-2605.2009.00995.x.
Oleszczuk K, Augustinsson L, Bayat N, Giwercman A, Bungum M. Prevalence of high DNA fragmentation index in male partners of unexplained infertile couples. Andrology. 2013;1(3):357–60. https://doi.org/10.1111/j.2047-2927.2012.00041.x.
Winkle T, Rosenbusch B, Gagsteiger F, Paiss T, Zoller N. The correlation between male age, sperm quality and sperm DNA fragmentation in 320 men attending a fertility center. J Assist Reprod Genet. 2009;26(1):41–6. https://doi.org/10.1007/s10815-008-9277-3.
Colin A, Barroso G, Gomez-Lopez N, Duran EH, Oehninger S. The effect of age on the expression of apoptosis biomarkers in human spermatozoa. Fertil Steril. 2010;94(7):2609–14. https://doi.org/10.1016/j.fertnstert.2010.04.043.
Brahem S, Mehdi M, Elghezal H, Saad A. The effects of male aging on semen quality, sperm DNA fragmentation and chromosomal abnormalities in an infertile population. J Assist Reprod Genet. 2011;28(5):425–32. https://doi.org/10.1007/s10815-011-9537-5.
Sloter ED, Marchetti F, Eskenazi B, Weldon RH, Nath J, Cabreros D, et al. Frequency of human sperm carrying structural aberrations of chromosome 1 increases with advancing age. Fertil Steril. 2007;87(5):1077–86. https://doi.org/10.1016/j.fertnstert.2006.08.112.
Bojar I, Witczak M, Wdowiak A. Biological and environmental conditionings for a sperm DNA fragmentation. Ann Agric Environ Med. 2013;20(4):865–8.
Das M, Al-Hathal N, San-Gabriel M, Phillips S, Kadoch IJ, Bissonnette F, et al. High prevalence of isolated sperm DNA damage in infertile men with advanced paternal age. J Assist Reprod Genet. 2013;30(6):843–8. https://doi.org/10.1007/s10815-013-0015-0.
Pino V, Sanz A, Valdes N, Crosby J, Mackenna A. The effects of aging on semen parameters and sperm DNA fragmentation. JBRA Assist Reprod. 2020;24(1):82–6. https://doi.org/10.5935/1518-0557.20190058.
Plastira K, Msaouel P, Angelopoulou R, Zanioti K, Plastiras A, Pothos A, et al. The effects of age on DNA fragmentation, chromatin packaging and conventional semen parameters in spermatozoa of oligoasthenoteratozoospermic patients. J Assist Reprod Genet. 2007;24(10):437–43. https://doi.org/10.1007/s10815-007-9162-5.
Potts RJ, Notarianni LJ, Jefferies TM. Seminal plasma reduces exogenous oxidative damage to human sperm, determined by the measurement of DNA strand breaks and lipid peroxidation. Mutat Res. 2000;447(2):249–56. https://doi.org/10.1016/s0027-5107(99)00215-8.
Baumber J, Ball BA, Linfor JJ, Meyers SA. Reactive oxygen species and cryopreservation promote DNA fragmentation in equine spermatozoa. J Androl. 2003;24(4):621–8. https://doi.org/10.1002/j.1939-4640.2003.tb02714.x.
Guthrie HD, Welch GR. Effects of reactive oxygen species on sperm function. Theriogenology. 2012;78(8):1700–8. https://doi.org/10.1016/j.theriogenology.2012.05.002.
Andolz P, Bielsa MA, Vila J. Evolution of semen quality in North-eastern Spain: a study in 22 759 infertile men over a 36 year period. Hum Reprod. 1999;14(3):731–5. https://doi.org/10.1093/humrep/14.3.731.
Fisch H, Goluboff ET, Olson JH, Feldshuh J, Broder SJ, Barad DH. Semen analyses in 1,283 men from the United States over a 25-year period: no decline in quality. Fertil Steril. 1996;65(5):1009–14. https://doi.org/10.1016/s0015-0282(16)58278-8.
Levitas E, Lunenfeld E, Weisz N, Friger M, Potashnik G. Relationship between age and semen parameters in men with normal sperm concentration: analysis of 6022 semen samples. Andrologia. 2007;39(2):45–50. https://doi.org/10.1111/j.1439-0272.2007.00761.x.
Gu XL, Li HG, Xiong CL. [Correlation of sperm DNA fragmentation index with age and semen parameters in infertile men]. Zhonghua nan ke xue =. Natl J Androl. 2018;24(7):608–12.
Spano M, Kolstad AH, Larsen SB, Cordelli E, Leter G, Giwercman A, et al. The applicability of the flow cytometric sperm chromatin structure assay in epidemiological studies. Asclepios. Hum Reprod. 1998;13(9):2495–505. https://doi.org/10.1093/humrep/13.9.2495.
Zhang LH, Qiu Y, Wang KH, Wang Q, Tao G, Wang LG. Measurement of sperm DNA fragmentation using bright-field microscopy: comparison between sperm chromatin dispersion test and terminal uridine nick-end labeling assay. Fertil Steril. 2010;94(3):1027–32. https://doi.org/10.1016/j.fertnstert.2009.04.034.
Gandini L, Lombardo F, Paoli D, Caruso F, Eleuteri P, Leter G, et al. Full-term pregnancies achieved with ICSI despite high levels of sperm chromatin damage. Hum Reprod. 2004;19(6):1409–17. https://doi.org/10.1093/humrep/deh233.
Zini A, Boman JM, Belzile E, Ciampi A. Sperm DNA damage is associated with an increased risk of pregnancy loss after IVF and ICSI: systematic review and meta-analysis. Hum Reprod. 2008;23(12):2663–8. https://doi.org/10.1093/humrep/den321.
Bungum M, Humaidan P, Axmon A, Spano M, Bungum L, Erenpreiss J, et al. Sperm DNA integrity assessment in prediction of assisted reproduction technology outcome. Hum Reprod. 2007;22(1):174–9. https://doi.org/10.1093/humrep/del326.
Giwercman A, Richthoff J, Hjøllund H, Bonde JP, Jepson K, Frohm B, et al. Correlation between sperm motility and sperm chromatin structure assay parameters. Fertil Steril. 2003;80(6):1404–12. https://doi.org/10.1016/s0015-0282(03)02212-x.
McQueen DB, Zhang J, Robins JC. Sperm DNA fragmentation and recurrent pregnancy loss: a systematic review and meta-analysis. Fertil Steril. 2019;112(1):54–60 e3. https://doi.org/10.1016/j.fertnstert.2019.03.003.
Tan J, Taskin O, Albert A, Bedaiwy MA. Association between sperm DNA fragmentation and idiopathic recurrent pregnancy loss: a systematic review and meta-analysis. Reprod BioMed Online. 2019;38(6):951–60. https://doi.org/10.1016/j.rbmo.2018.12.029.
Simon L, Murphy K, Shamsi MB, Liu L, Emery B, Aston KI, et al. Paternal influence of sperm DNA integrity on early embryonic development. Hum Reprod. 2014;29(11):2402–12. https://doi.org/10.1093/humrep/deu228.
Katib AA, Al-Hawsawi K, Motair W, Bawa AM. Secondary infertility and the aging male, overview. Cent Eur J Urol. 2014;67(2):184–8. https://doi.org/10.5173/ceju.2014.02.art13.
Singh NP, Muller CH, Berger RE. Effects of age on DNA double-strand breaks and apoptosis in human sperm. Fertil Steril. 2003;80(6):1420–30. https://doi.org/10.1016/j.fertnstert.2003.04.002.
Acknowledgments
The authors would like to thank their grant sponsors, National Key R&D Program of China(2018YFC1004302), Open Project of the Key Laboratory of Male Reproductive Medicine and Genetics, National Health Commission of the People’s Republic of China (grant no: KF201708), and National Natural Science Foundation (grant nos. 81471495).
Author information
Authors and Affiliations
Contributions
Yonghong Tian and Fan Jin conceived the idea and designed the study. Fengbin Zhang and Jinggen Wu collected the retrospective clinical data; Jingping Li and Zhongyan Liang analyzed data and conducted the statistical analysis. Fengbin Zhang and Chong Chen wrote the manuscript. Yonghong Tian and Lejun Li reviewed and assessed the manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study received ethical approval from the Institutional Review Boards of our facility (IRB-20200152-R).
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, F., Li, J., Liang, Z. et al. Sperm DNA fragmentation and male fertility: a retrospective study of 5114 men attending a reproductive center. J Assist Reprod Genet 38, 1133–1141 (2021). https://doi.org/10.1007/s10815-021-02120-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02120-5